LUNG ULTRASOUND IN DIAGNOSIS OF PNEUMONIA IN
EMERGENCY DEPARTMENT: A SYSTEMATIC REVIEW AND
META-ANALYSIS
1
Ayman Ahmad Heikal, 2Yousef Mohammed Abozinadah, 3Turki Faiz Khawaji, 4Faisal Mohammed Altumaihi, 5hamed Marzoog Alharthi, 6Abdullah Saleh Alghamdi, 7Zead Ibrahim A. Alhussain, 8*Banan Ali Najmi, 9Zakaria Abdullah Alsaileek, 10Mohammad
Tariq Almasri
1
Associate Professor of Critical Care Medicine, Cairo University, Critical Care Consultant at King Fahad hospital, Jeddah Saudi Arabia.
2,5,6
Critical Care Resident, King, Abdulaziz University Hospital, Jeddah Saudi Arabia.
3
Critical Care Resident, King Fahad General Hospital, Jeddah, Saudi Arabia.
4
Critical Care Resident, Critical Care Residency Program King Fahad General Hospital, Jeddah, Saudi Arabia.
7
Emergency Resident at King Khalid Hospital Al-Kharj, Riyadh, Saudi Arabia.
8
Medical intern - College of Medicine, King Khalid University, Abha. Saudi Arabia.
9
General Physician, King Fahad Hospital Hofuf, Alahsa, Saudi Arabia.
10
Emergency Resident at Ajyad Emergency Hospital, Makkah, Saudi Arabia.
ABSTRACT
Background & Purpose: Acute community-acquired pneumonia needs to be identified early to keep away from most complications. The
common diagnostic tools had been represented by means of blood
exams and chest X- ray with CT test coming as a 2nd-line exploration.
The presence of air in the pulmonary parenchyma has long been
thought of as no longer explorable by ultrasound. The Aim of this work
is to provide cumulative data about the diagnostic efficacy of Lung
Ultrasound (LUS) in diagnosis of Community-acquired pneumonia
(CAP) in emergency setting. Methods: A systematic search was performed of PubMed, Cochrane library Ovid, Scopus & Google
scholar to identify Emergency medicine RCTs, clinical trials, and comparative studies, which
studied the Sensitivity and Specificity of LUS in pneumonia patients. A meta-analysis was
done using fixed and random-effect methods. The primary outcome was Sensitivity for
diagnostic odds ratio (DOR). Secondary outcome was Specificity for diagnostic odds ratio
(DOR). The assessment of DOR was assessed by pooled Area under ROC curve for each *Corresponding Author
Banan Ali Najmi
Medical intern - College of
Medicine, King Khalid
University, Abha. Saudi
Arabia.
Article Received on 21 Oct. 2019,
Revised on 11 Nov. 2019, Accepted on 01 Dec. 2019,
DOI: 10.20959/wjpr201913-16495
parameter. Results: A total of 7 studies were identified involving 3380 patients. Regarding Sensitivity measure, the fixed- effects model of the meta-analysis study showed highly
significant increase in pooled sensitivity (90%) of LUS in pneumonia patients (p < 0.01).
Regarding Specificity measure, the fixed-effects model of the meta-analysis study showed
highly significant increase in pooled specificity (92%) of LUS in pneumonia patients (p <
0.01). Conclusion: To conclude, the LUS proved to be a sufficiently useful and accurate tool to diagnose CAP in an adult population in the ED.
KEYWORDS: Lung ultrasound, Diagnosis of Pneumonia, Emergency Department.
INTRODUCTION
Pneumonia has been documented as a forgotten killer for human health. in keeping with the
information launched via world health organization, lower respiratory tract contamination is
the leading reason of infectious disorder related mortality worldwide and refers back to the
top rating death reason in be based on swift and accurate recognition. The symptoms and
signs localizing to the respiratory system, usually referring as dyspnea, cough and fever.[1]
The yearly incidence of community-acquired pneumonia (CAP) degrees from to four million,
resulting in about 1 million hospitalizations and 60,000 deaths yearly within the USA.
Pneumonia can be life-threatening, most usually in older patients with comorbidities or
immunocompromised sufferers. Mortality reaches 28% in admitted sufferers, even though it
is closer to 5–7% in admitted sufferers with CAP.[2]
Community-acquired pneumonia (CAP) is a common and critical infectious disorder related
to high morbidity and mortality. It is the 6th main reason of dying and the maximum common
infectious cause of death worldwide. But CAP is frequently misdiagnosed even now. Early
and powerful antibiotic treatment is important. An adequate treatment is therefore reliant on
an early diagnosis of pneumonia, but the diagnosis isn't always constantly clear at
presentation to the emergency department (ED).[3]
Acute community-acquired pneumonia needs to be identified early to keep away from most
complications. The common diagnostic tools had been represented by means of blood exams
and chest X-ray with CT test coming as a 2nd-line exploration. The presence of air in the
pulmonary parenchyma has long been thought of as no longer explorable by ultrasound.
pulmonary illnesses. Moreover, the safety of the technique and the development of mobile
and ultra-portable devices have provided it as a first-line examination by means of a
non-radiologist doctor.[4]
Lung ultrasonography has increasingly more emerged as a beneficial point-of-care (POC)
tool in comparing these patients due to its rapid, non-invasive, repeatable and non-ionizing
traits. Latest research have additionally proven its high sensitivity and specificity within the
diagnosis of decompensated heart failure, pneumonia, pneumothorax, pulmonary embolism,
and pleural effusion.[5]
Aim of the study: The Aim of this work is to provide cumulative data about the diagnostic efficacy of Lung Ultrasound (LUS) in diagnosis of Community-acquired pneumonia (CAP)
in emergency setting.
METHODS
This review was carried out using the standard methods mentioned within the Cochrane
handbook and in accordance with the (PRISMA) statement guidelines.[6]
Identification of Studies
An initial search carried out throughout the PubMed, Cochrane library Ovid, Scopus &
Google scholar using the following keywords: Lung ultrasound, diagnosis of pneumonia,
emergency department.
We will consider published, full text studies in English only. Moreover, no attempts were
made to locate any unpublished studies nor non-English studies.
Criteria of Accepted Studies Types of Studies
The review will be restricted to RCTs, clinical trials, and comparative studies, either
prospective or retrospective, which studied the outcome of Sensitivity versus Specificity of
LUS in pneumonia patients.
Types of Participants
Participants with suspected pneumonia in emergency department.
Types of Outcome Measures
2. Specificity (2ry outcome)
Inclusion Criteria English literature. Journal articles.
Between 2014 until 2018.
Describing Sensitivity or Specificity of LUS in pneumonia patients. Human studies.
Exclusion Criteria
Articles describing other diagnostic methods of pneumonia (e.g. CT or CXR). Articles describing pneumonia in outpatient setting.
Irrelevance to our study.
METHODS OF THE REVIEW Locating Studies
Abstracts of articles identified using the above search strategy will be viewed, and articles
that appear of fulfill our inclusion criteria will be retrieved in full, when there is a doubt, a
second reviewer will assess the article and consensus will be reached.
Data Extraction
Using the following keywords: Lung ultrasound, diagnosis of pneumonia, emergency
department, data will be independently extracted by two reviewers and cross-checked.
Statistical Analysis
Statistical analysis done using MedCalc ver. 18.11.3 (MedCalc, Ostend, Belgium). Data were
pooled and odds ratios (ORs) as well as standard mean differences (SMD), were calculated
with their 95 per cent confidence intervals (CI). A meta-analysis was performed to calculate
direct estimates of each treatment, technique or outcome. According to heterogeneity across
trials using the I2-statistics; a fixed- effect model (P ≥ 0.1) or random-effects model (P < 0.1)
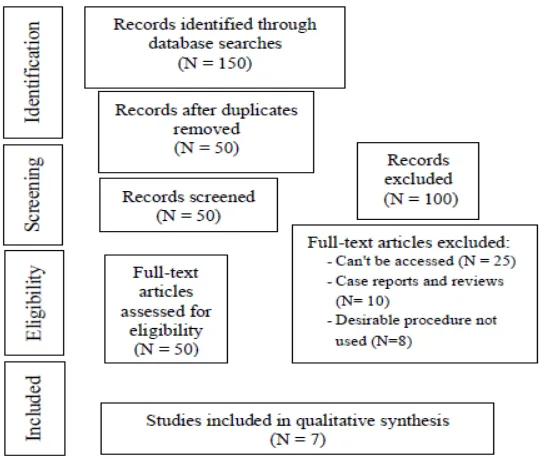
Study Selection
Figure 1: Flow Chart For Study Selection.
RESULTS
Descriptive analysis of all studies included (Tables 1, 2). Table 1: Patients and Study Characteristics.
N Author Type of study Sample size Age (average years)
1 Laursen et al., 2014 Prospective 158 73
2 Pagano et al., 2015 Prospective 105 58
3 Mantuani et al., 2016 Prospective 57 58
4 Papanagnou et al., 2017 Prospective 115 61
5 Zanobetti et al., 2017 Prospective 2683 71
6 Amatya et al., 2018 Prospective 62 60
7 Samson et al., 2018 Prospective 200 29.5
#Studies were arranged according to publication year.
Table 2: Summary of Outcome Measures In All Studies.
N Author
Primary outcome Primary outcome
Sensitivity (95% CI) Specificity (95% CI) Sensitivity Lower
limit
Upper
limit Specificity
Lower limit
Upper limit
1 Laursen et al., 2014 0.92 0.82 0.97 1.00 0.96 1.00
2 Pagano et al., 2015 0.98 0.91 0.99 0.64 0.49 0.78
3 Mantuani et al., 2016 0.82 0.61 0.93 0.83 0.69 0.92
4 Papanagnou et al., 2017 0.92 0.52 0.99 0.97 0.92 0.99
5 Zanobetti et al., 2017 0.88 0.86 0.90 0.91 0.90 0.92
6 Amatya et al., 2018 0.91 0.78 0.97 0.61 0.36 0.83
[image:5.595.62.539.598.759.2]The included studies published between 2014 and 2018. Regarding the type of included
studies, all 7 studies were prospective.
Regarding patients’ characteristics, the total number of patients in all the included studies was
3380 patients, while their average age of all patients was (58.5 years).
Meta-analysis of Outcome Measures
Data were divided into two parameters:
1) Sensitivity
2) Specificity
Meta-analysis study was done on 7 studies which described sensitivity and specificity of LUS
in pneumonia patients; with overall number of patients (N=3380).
Patients who achieved outcome measures were pooled:
Each outcome was measured by
Area under ROC curve. For pooled sensitivity (%). For pooled specificity (%).
Regarding primary outcome measure,
We found 7 studies reported sensitivity with total number of patients (N=3380).
I2 (inconsistency) was 0% with non-significant Q test for heterogeneity (p > 0.05), so
fixed-effects model was carried out; with overall AROC= 90% (95% CI 83 to 96).
The fixed-effects model of the meta-analysis study showed highly significant increase in
Figure 2: Forest plot of (pooled sensitivity) – Area under ROC curve.
Regarding secondary outcome measure,
We found 7 studies reported specificity with total number of patients (N=3380).
I2 (inconsistency) was 0% with non-significant Q test for heterogeneity (p > 0.05), so
fixed-effects model was carried out; with overall AROC= 92% (95% CI 89 to 96).
The fixed-effects model of the meta-analysis study showed highly significant increase in
pooled specificity (92%) of LUS in pneumonia patients (p < 0.01).
[image:7.595.143.456.524.733.2]DISCUSSION
The Aim of this work is to provide cumulative data about the diagnostic efficacy of Lung
Ultrasound (LUS) in diagnosis of Community-acquired pneumonia (CAP) in emergency
setting.
The included studies published between 2014 and 2018. Regarding the type of included
studies, all 7 studies were prospective.
Regarding patients’ characteristics, the total number of patients in all the included studies was
3380 patients, while their average age of all patients was (58.5 years).
Meta-analysis of outcome measures: data were divided into two parameters: (Sensitivity and
Specificity).
Meta-analysis study was done on 7 studies which described sensitivity and specificity of LUS
in pneumonia patients; with overall number of patients (N=3380).
Regarding primary outcome measure, we found 7 studies reported sensitivity with total
number of patients (N=3380).
The fixed-effects model of the meta-analysis study showed highly significant increase in
pooled sensitivity (90%) of LUS in pneumonia patients (p < 0.01).
Which came in agreement with, Liu et al. 2015[3], Bourcier, Braga, and Garnier 2016[4] and
with Xia et al. 2016.[1]
Liu et al. 2015[3] reported that, their study found that, by combining four patterns of
ultrasonographic findings, bedside ultrasonography had a high sensitivity (94.6%) for
diagnosing CAP.
Bourcier, Braga, and Garnier 2016[4] reported that, from the studies evaluating the ability of
US to detect alveolar consolidation, the sensitivity of the test was about 90%. In these studies,
US was carried out after radiographic confirmation of a lung image, which introduced a bias
for US examination.
Xia et al. 2016[1] Reported that, the study contained participants met all inclusion criteria and
On other hand, in disagreement with our study Koh et al. 2018[5] reported that, results had
lower sensitivities compared to other studies, with sensitivity 65.3%. This discrepancy may
be expected since ultrasonography is operator dependent, despite ensuring adequate
ultrasonographical training. Moreover, patient factors such as body habitus and inability to
cooperate with evaluation may also be prevailing reasons for suboptimal ultrasonographic
image sorted.
Regarding secondary outcome measure, we found 7 studies reported specificity with total
number of patients (N=3380).
The fixed-effects model of the meta-analysis study showed highly significant increase in
pooled specificity (92%) of LUS in pneumonia patients (p < 0.01). which came in agreement
with Liu et al. 2015[3], Llamas-Alvarez, Tenza-Lozano, and Latour-Perez 2017[7], Staub et al. 2019[8] and with Long, and Koyfman 2017.[2]
Llamas-Alvarez, Tenza-Lozano, and Latour-Perez 2017[7] reported that, sixteen studies
(2359 participants) were included. There was significant heterogeneity of both sensitivity and
specificity according to Q test, without clear evidence of threshold effect. The area under the
SROC curve was 93%, with a DOR at the optimal cut-point of 50%. A tendency towards a
higher area under the SROC curve in high quality studies was detected, however these
differences were not significant. The overall effect indicates a sensitivity of approximately
80% to 90% and a specificity of 70% to 90%.
Liu et al. 2015[3] reported that, their study found that by combining four patterns of
ultrasonographic findings, bedside ultrasonography had a high sensitivity (94.6%) for
diagnosing CAP.
Staub et al. 2019[8] reported that, 25 studies involving 4241 patients were included. Fourteen
studies assessed pneumonia (n = 1867 patients), four studies assessed exacerbation of COPD
or asthma (n = 527 patients). The overall diagnostic accuracy of LUS for pneumonia had an
AUC of 0.948. The 95% CI of the overall effects estimates a specificity of approximately of
75% – 90%.
Long, and Koyfman 2017[2] reported that, US has demonstrated utility in differentiating
pneumonia from other conditions. A comparison of US and chest radiograph for the diagnosis
radiography, and specificity over 94%.
On other hand, in disagreement with our study Sen et al. 2017[9] reported that, the sensitivity
and specificity for the most common conditions in the study were lower than that reported by
others, with specificity 78% and sensitivity 88%. There are several reasons for the relatively
low diagnostic accuracy in our study compared to previous reports. Lung ultrasonography has
been shown to be accurate in differentiating alveolar processes (pulmonary edema or
pneumonia), obstructive disease (asthma and COPD), and PE. However, other conditions
causing respiratory distress may not be easily diagnosed using lung ultrasonography
protocols.
CONCLUSION
To conclude, the LUS proved to be a sufficiently useful and accurate tool to diagnose CAP in
an adult population in the ED.
ACKNOWLEDGMENTS Conflict of interest
None.
Authorship
All the listed authors contributed significantly to conception and design of study, acquisition,
analysis and interpretation of data and drafting of manuscript, to justify authorship.
Funding
Self-funding.
REFERENCES
1. Xia, Y.; Ying, Y.; Wang, S.; Li, W.; Shen, H. Effectiveness of Lung Ultrasonography for
Diagnosis of Pneumonia in Adults: A Systematic Review and Meta-Analysis. Journal of
thoracic disease, 2016; 8(10): 2822.
2. Long, B.; Long, D.; Koyfman, A. Emergency Medicine Evaluation of
Community-Acquired Pneumonia: History, Examination, Imaging and Laboratory Assessment, and
Risk Scores. The Journal of emergency medicine, 2017; 53(5): 642–652.
3. Liu, X.; Lian, R.; Tao, Y.; Gu, C.; Zhang, G. Lung Ultrasonography: An Effective Way to
Diagnose Community-Acquired Pneumonia. Emerg Med J., 2015; 32(6): 433–438.
Radiography in the Diagnosis of Acute Community-Acquired Pneumonia. Current
infectious disease reports, 2016; 18(12): 43.
5. Koh, Y.; Chua, M. T.; Ho, W. H.; Lee, C.; Chan, G. W. H.; Kuan, W. S. Assessment of
Dyspneic Patients in the Emergency Department Using Point-of-Care Lung and Cardiac
Ultrasonography—a Prospective Observational Study. Journal of thoracic disease, 2018;
10(11): 6221.
6. Liberati, A.; Altman, D.; Tetzlaff, J.; Mulrow, C.; Gøtzsche, P.; Ioannidis, J.; Clarke, M.;
Devereaux, P.; Kleijnen, J.; Moher, D. The PRISMA Statement for Reporting Systematic
Reviews and Meta-Analyses of Studies That Evaluate Healthcare Interventions. Bmj,
2009; 339.
7. Llamas-Alvarez, A. M.; Tenza-Lozano, E. M.; Latour-Perez, J. Accuracy of Lung
Ultrasonography in the Diagnosis of Pneumonia in Adults: Systematic Review and
Meta-Analysis. Chest, 2017; 151(2): 374–382.
8. Staub, L. J.; Biscaro, R. R. M.; Kaszubowski, E.; Maurici, R. Lung Ultrasound for the
Emergency Diagnosis of Pneumonia, Acute Heart Failure, and Exacerbations of Chronic
Obstructive Pulmonary Disease/Asthma in Adults: A Systematic Review and
Meta-Analysis. The Journal of emergency medicine, 2019; 56(1): 53–69.
9. Sen, S.; Acash, G.; Sarwar, A.; Lei, Y.; Dargin, J. M. Utility and Diagnostic Accuracy of
Bedside Lung Ultrasonography during Medical Emergency Team (MET) Activations for
Respiratory Deterioration. Journal of critical care, 2017; 40: 58–62.
Papers included in our meta-analysis
Laursen, C.B., Sloth, E., Lassen, A.T., Christensen, R.D., Lambrechtsen, J., Madsen, P.H.,
Henriksen, D.P., Davidsen, J.R. and Rasmussen, F., Point-of-care ultrasonography in
patients admitted with respiratory symptoms: a single-blind, randomised controlled trial.
The Lancet Respiratory medicine, 2014; 2(8): 638-646.
Pagano, A., Numis, F.G., Visone, G., Pirozzi, C., Masarone, M., Olibet, M., Nasti, R.,
Schiraldi, F. and Paladino, F., Lung ultrasound for diagnosis of pneumonia in emergency
department. Internal and emergency medicine, 2015; 10(7): 851-854.
Mantuani, D., Frazee, B.W., Fahimi, J. and Nagdev, A., Point-of-care multi-organ
ultrasound improves diagnostic accuracy in adults presenting to the emergency
department with acute dyspnea. Western Journal of Emergency Medicine, 2016; 17(1): 46.
Papanagnou, D., Secko, M., Gullett, J., Stone, M. and Zehtabchi, S., Clinician-Performed
with Acute Dyspnea. Western Journal of Emergency Medicine, 2017; 18(3): 382.
Zanobetti, M., Scorpiniti, M., Gigli, C., Nazerian, P., Vanni, S., Innocenti, F., Stefanone, V.T., Savinelli, C., Coppa, A., Bigiarini, S. and Caldi, F., Point-of-care ultrasonography
for evaluation of acute dyspnea in the ED. Chest, 2017; 151(6): 1295-1301.
Amatya, Y., Rupp, J., Russell, F.M., Saunders, J., Bales, B. and House, D.R., Diagnostic
use of lung ultrasound compared to chest radiograph for suspected pneumonia in a
resource-limited setting. International journal of emergency medicine, 2018; 11(1): 8.
Samson, F., Gorostiza, I., González, A., Landa, M., Ruiz, L. and Grau, M., Prospective evaluation of clinical lung ultrasonography in the diagnosis of community-acquired
pneumonia in a pediatric emergency department. European Journal of Emergency