ASSESSING THE KNOWLEDGE ON SELF-MEDICATION AMONG
MEDICAL STUDENTS OF BANGLADESH
Mahmudul Hasan Tushar1, Munira Tasnim Karim1, Omer Fayshal Pavel*1
1
Department of Pharmacy, East West University, Dhaka, Bangladesh.
ABSTRACT
Self medication is one of the most practiced worldwide issues and can
cause both benefit also with harmful effect at a time, when if it is not
properly mentored by experts of drugs. Bangladesh is a south Asian
developing country, where self medication is highly practiced. The aim
of the study was to examine the knowledge and practice of self
medication among the medical students in Bangladesh. The study was
done among 731 medical students of both public and private medicals
in Bangladesh. 92% of the medical students of both government and
non- government medical colleges self-medicate and they get the drugs
from local pharmacies, family, friends and neighbors. More than 60%
of the population suffered from mismanagement of self medication and more than 30% know
about the harmful effect of self medication but till they are practicing self medication.
KEYWORDS: Self medication, Medical Students, Harmful effect, Prescription, Bangladesh.
INTRODUCTION
Self medication is a pattern obtaining and consumption of drugs without the proper guideline
of physicians by diagnostic or other medical procedures.[1] Self medication is widely
practiced worldwide and can cause both benefit and harm at a time if it is not properly
mentored by experts of drugs.[2] As the result of harm self medication can bring many
unexpected and health hazardous states like adverse drug reactions, resistance of pathogens,
physical dependence, misdiagnosis, abuse of drug resources etc.[3] About the self medication
World Health Organization (WHO) has pointed out the accurate and responsible self
medication can help to prevent or treat diseases only which don’t require physicians’
consultation or can be used as over the counter drugs.[4] This self prescribing practice is
predominant in the developing countries like south Asian countries as it allows the low cost
Volume 6, Issue 10, 27-33. Research Article ISSN 2277– 7105
Article Received on 06 July 2017,
Revised on 27 July 2017, Accepted on 16 Aug. 2017
DOI: 10.20959/wjpr201710-8914
*Corresponding Author
Omer Fayshal Pavel
Department of Pharmacy,
East West University,
alternative for those people who are not financially stable enough to access the doctors for
proper consultancy.[5]
Self medication is well practiced in medical students as they have very good idea and practice
of handling different drugs and disease. Besides that they are the future councilors of drugs
and medicine thus need rapid knowledge enhancing on drugs in their academic study.[6]
Without this there is a specific culture among doctors that they don’t expect to get sick or to
be a patient of others thus self-diagnosis, self-referral or self-treatment among physicians is
highly significant.[7] Now days the most commonly accessible (Over the Counter) OTC
medications are pain-killers, cold remedies, anti-allergy medicines and vitamins. Though
these medications are considered as risk free and useful for the treatment of common health
hazards but their excessive use can also lead to serious side-effects, unfavorable reactions or
adverse drug reaction with concomitant use with other drugs.[8]
The study was done to assess knowledge of the self-medication and practice of self treatment
behavior of medical students. There have been several reports addressing the extent of
self-medication practices among university students in South Asian countries as well as developed
countries of the worlds. The current study was undertaken to describe self-medication
practices among medical college students as well as to identify potential factors that are
associated with self-medication practices and to identify reasons for self-medication practices
in Bangladesh.
METHOD AND MATERIALS
Study design
This was a cross-sectional, questionnaire-based study. There were 9 major questions, under
these questions there were 20 sub questions.
Study setting
This cross-sectional descriptive study was carried out at 9 different medical colleges of
Bangladesh situated in 3 different districts. 4 of the medical colleges are government medical
college and other 5 were private medical colleges
Study time and Population
Questionnaires were completed in January to April 2016. Approximately 900 students
them 731 people were taken as population where remaining were not included for their
ambiguous response. In the population the age range was 20 to 30 and 61% was male and
39% of the population was female. All the students from 1st to 5th year were included in the
study. Among the people 33% were form rural area and 67% were from urban area. In the
population 52% were form families earning more than 35,000 BDT monthly.
Ethical issues
Prior permission was taken from the authority of the institution for conducting the study. The
purpose of the study was explained clearly to the participating students and confidentiality
was ensured. Informed consent was obtained from population before filling the questionnaire.
Study procedure
The questionnaire was distributed to all students attending randomly selected classes,
cafeteria, student halls, and common rooms. After obtaining informed consent, they were
asked to fill up a printed, questionnaire.
Statistical analysis
The data were coded, entered, and analyzed using the Microsoft Excel 2010. Descriptive
results were expressed as percentage and plotted with table, pie chart and bar diagrams. The
variables of the study are government and non-government institution, age, gender and year
of study.
RESULT
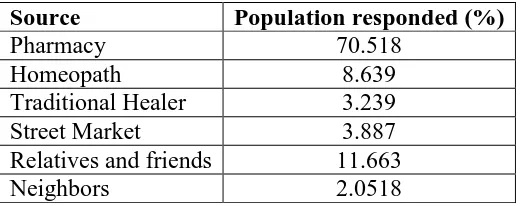
In the response of the source of medication without prescriptions the population mentioned
[image:3.595.169.429.595.698.2]mainly five sources, shown in the table 1.
Table 1: Source of medication without prescription.
Source Population responded (%)
Pharmacy 70.518
Homeopath 8.639
Traditional Healer 3.239
Street Market 3.887
Relatives and friends 11.663
Neighbors 2.0518
When the population were asked the factor associated with the self medication with 8
questions they were given to choose 3 options agree, disagree or don’t know. The response is
Table 2: Factor Associated With Self Medication.
Factors Yes (%) No (%) Confused (%)
Self Medicate in the Past Year 74 18 08
Avoidance of burden my physician 26.34 32.70 40.94
No Physicians Advice 24 33 43
Active Role about Personal Health 38 19 43
Influence of Relatives, Friends and Media 18 33 49
Long Waiting Time in doctors chamber 25 31 44
Prescribed Treatment was Unsuccessful 13 44 43
They don't have Trust in Physician 17 47 36
In the study it was found that the pattern of using different medication like sedative,
painkillers, antibiotics and other non OTC drug as self medication in last month, shown is the
[image:4.595.141.456.311.490.2]figure 1.
Figure 1: Use of Certain Drugs for Self medication.
And when asked in different physical hazards like weight loss, mild to moderate injury,
toothache and others what is the steps they took in last month shown in Graph 1.
[image:4.595.143.457.575.742.2]From population different adverse or side effect were collected and shown in the table 3.
Table 3: Different unexpected effect after self medication.
Effect Yes (%) No (%) No response (%)
Duration of Symptoms 67 21 12
Worsening Symptoms 66 22 12
Presence of Severe Pain 62 28 10
Irregular Side Effects 43 39 18
Serious Problems 58 24 18
Psychological Problems 23 60 17
At the end of the survey the knowledge on self medication and its hazardous effect was asked
through different questions. The result is shown in the table 4.
Table 4: Knowledge on Self Medication and Its Hazardous Effect.
Questions Agree
(%)
Disagree (%)
Not Sure (%)
All drugs have side effects 33 30 37
Simultaneous use of drugs can be potentially dangerous 46 14 40
Increasing Drug Dose can be dangerous 49 41 10
Lowering drug dose can be dangerous 32 22 46
Physicians help must sought in case of side effects 50.6 8.3 40.9
Using drugs with unknown substances in patients with
liver and kidney diseases is very dangerous 60.7 7.8 31.33
No drugs can be used during pregnancy 32 28 40
Mild medical problems don’t need drug treatment 31 21 48
Self treatment can mask signs and symptoms 43 14 43
DISCUSSION
From the study it is evident that self-medication is very common among Bangladeshi medical
students. About 92% of the medical students of both government and non- government
medical colleges self-medicate in the past years which matches with the study of southern
India[9] and Students at University of Ljubljana, Slovenia.[10] It does mean the self medication
is not only an issue of Bangladesh rather a global issue that needs to get the concern of global
regulatory author with proper implementation. In the study it was found that the most
available source to get drugs for self-medication for Bangladeshi medical students is mainly
the local pharmacies and others factors like friends and neighbors are also included. It is also
evident that medical students not only influenced by friends, family rather by social
marketing of the drugs.[11] As a result some dugs are so available to get in Bangladesh like the
LIMITATION
1. The study was based on self-reported data about self-medication in four month duration.
2. Though the students were encouraged to complete the survey independently, mutual
influence between the students could not be entirely ruled out.
3. The results of the study would have been more generalized if it could involve students of
all the medical colleges in Bangladesh
CONCLUSION
This study has found that self-medication is very common among medical students,
facilitated by the easy availability of drugs, and high self-care orientation. A significant
number of students are unaware of the adverse effects of the medication that they themselves
take and suggest to others. Since inappropriate self-medication has the potential to cause
serious harm, not only to the students themselves but also to those whom they suggest
medication, potential problems of self-medication should be emphasized to the students to
minimize this risk. Restriction of sale of drugs with potentially harmful effects should be
implemented effectively with monitoring systems between the physicians and pharmacists.
REFERENCE
1. Montastruc, J.L., Bagheri, H., Geraud, T. and Lapeyre-Mestre, M., Pharmacovigilance of
self-medication. Europe PMC, 1996; 52(2): 105-110.
2. Hughes, C.M., McElnay, J.C. and Fleming, G.F.,. Benefits and risks of self
medication. Drug safety, 2001; 24(14): 1027-1037.
3. Badiger, S., Kundapur, R., Jain, A., Kumar, A., Pattanshetty, S., Thakolkaran, N., Bhat,
N. and Ullal, N., Self-medication patterns among medical students in South India. The
Australasian medical journal, 2012; 5(4): 217.
4. World Health Organization, The Role of the pharmacist in self-care and self-medication:
report of the 4th WHO Consultative Group on the Role of the Pharmacist, The Hague,
The Netherlands, 26-28 August 1998.
5. Hussain, S., Malik, F., Hameed, A., Ahmad, S. and Riaz, H., Exploring health seeking
behavior, medicine use and self medication in urban and rural Pakistan. Southern Med
Review, 2010; 3(2): 32-35.
6. Banerjee, I. and Bhadury, T., Self-medication practices among undergraduate medical
students in a tertiary care medical college, West Bengal. Journal of postgraduate
7. Montgomery, A.J., Bradley, C., Rochfort, A. and Panagopoulou, E., A review of
self-medication in physicians and medical students. Occupational medicine, 2011; 61(7):
490-497.
8. Hussain, A. and Khanum, A., Self medication among university students of Islamabad,
Pakistan-a preliminary study. Southern Medcal Review, 2008; 1(1): 14.
9. Badiger, S., Kundapur, R., Jain, A., Kumar, A., Pattanshetty, S., Thakolkaran, N., Bhat,
N. and Ullal, N., Self-medication patterns among medical students in South India. The
Australasian medical journal, 2012; 5(4): 217.
10.Klemenc-Ketis, Z., Hladnik, Z. and Kersnik, J., Self-medication among healthcare and
non-healthcare students at University of Ljubljana, Slovenia. Medical Principles and
practice, 2010; 19(5): 395-401.
11.Kamat, V.R. and Nichter, M., Pharmacies, self-medication and pharmaceutical marketing
in Bombay, India. Social science & medicine, 1998; 47(6): 779-794.
12.James, H., Handu, S.S., Al Khaja, K.A., Otoom, S. and Sequeira, R.P., Evaluation of the
knowledge, attitude and practice of self-medication among first-year medical