Y0046_LT44441EB Approved LT44441EB No changes made since 09/2014
│
Value
│
Drugs That Require Prior Authorization (PA)
Before Being Approved for Coverage
You will need authorization by your Express Scripts Medicare
®(PDP) before
filling prescriptions for the drugs shown in the chart below. The Express Scripts
Medicare (PDP) will only provide coverage after it determines that the drug is
being prescribed according to the criteria specified in the chart. You, your
appointed representative, or your prescriber can request prior authorization by
calling Express Scripts toll-free at 1.800.935.6103, 24 hours 7 days a week,
including Thanksgiving and Christmas. Customer Service is available in English
and other languages. TTY/TDD users should call 1.800.716.3231.
Express Scripts Medicare (PDP) is a prescription drug plan with a Medicare contract. Enrollment in Express Scripts Medicare depends on contract renewal.
A
CTEMRA
Products Affected
Actemra INJ 200MG/10MLPA Criteria
Criteria Details
Covered Uses All FDA-approved indications not otherwise excluded from Part D. Plus patients already started on tocilizumab for a Covered Use.
Exclusion Criteria
Tocilizumab should not be given in combination with tumor necrosis factor (TNF) antagonists (adalimumab, certolizumab pegol, etanercept, golimumab, infliximab), abatacept, anakinra, rituximab, or tofacitinib.
Required Medical Information
N/A
Age Restrictions For rheumatoid arthritis (RA), approve for adults.
Prescriber Restrictions
Prescribed by or in consultation with a rheumatologist.
Coverage Duration
Authorization will be for 12 months.
Other Criteria Adults with RA, approve for patients who have tried for at least 3 months or who were intolerant to adalimumab, or etanercept. Systemic-onset JIA, approve for patients who have tried a systemic corticosteroid or MTX, leflunomide, or sulfasalazine or another DMARD such as etanercept, adalimumab, infliximab, or anakinra OR have systemic arthritis with active systemic features and features of poor prognosis (eg, arthritis of the hip, radiographic damage).
3
A
CTEMRA
S
Q
Products Affected
Actemra INJ 162MG/0.9MLPA Criteria
Criteria Details
Covered Uses All FDA-approved indications not otherwise excluded from Part D. Plus patients already started on tocilizumab for a Covered Use.
Exclusion Criteria
Concurrent use with another biologic therapy (e.g., certolizumab, etanercept, adalimumab, anakinra, abatacept, infliximab, rituximab, golimumab) or with tofacitinib.
Required Medical Information
N/A
Age Restrictions RA - adults
Prescriber Restrictions
Prescribed by or in consultation with a rheumatologist.
Coverage Duration
12 months
Other Criteria RA - The pt had a 3 month trial with tofacitinib or one of the following biologic DMARDs, unless intolerant: Actemra (IV), abatacept,
rituximab, or a tumor necrosis factor (TNF) antagonist (e.g., etanercept, adalimumab, certolizumab, infliximab, or golimumab
A
CTHAR
Products Affected
H.p. ActharPA Criteria
Criteria Details
Covered Uses All FDA-approved indications not otherwise excluded from Part D.
Exclusion Criteria
Use in patients with multiple sclerosis (MS) as pulse therapy on a monthly basis.
Required Medical Information
MS exacerbation, history of corticosteroid use.
Age Restrictions N/A
Prescriber Restrictions
Infantile spasms, prescribed by or in consultation with a neurologist or an epileptologist. MS exacerbation, prescribed by or in consultation with a neurologist or physician that specializes in the treatment of MS.
Coverage Duration
Infantile spasms, 12 months. MS exacerbation, approve 1 month.
Other Criteria For MS exacerbation, approve if the patient cannot use high-dose IV corticosteroids because IV access is not possible or if the patient has tried high-dose corticosteroids administered IV for an acute MS exacerbation and has experienced a severe or limiting adverse effect.
5
A
DEMPAS
Products Affected
AdempasPA Criteria
Criteria Details
Covered Uses All FDA-approved indications not otherwise excluded from Part D.
Exclusion Criteria N/A Required Medical Information N/A
Age Restrictions N/A
Prescriber Restrictions
PAH and CTEPH- must be precribed by or in consultation with a cardiologist or a pulmonologist.
Coverage Duration
12 months
Other Criteria For PAH - must have PAH (WHO Group 1) and had a right heart
catheterization to confirm the diagnosis of PAH (WHO Group 1). Right heart cathererization is not required in pts who are currently receiving Adempas or another agent indicated for WHO group 1.
A
DHD
N
ON
-
STIMULANT
M
EDICATIONS
Products Affected
IntunivStrattera
PA Criteria
Criteria Details
Covered Uses All medically accepted indications not otherwise excluded from Part D.
Exclusion Criteria N/A Required Medical Information N/A
Age Restrictions N/A
Prescriber Restrictions
N/A
Coverage Duration
Authorization will be for 12 months.
7
A
FINITOR
Products Affected
AfinitorAfinitor Disperz
PA Criteria
Criteria Details
Covered Uses All FDA-approved indications not otherwise excluded from Part D. Plus patients already taking Afinitor for a Covered Use. Advanced,
unresectable neuroendocrine tumors. Perivascular Epitheloid Cell Tumors (PEComa), Recurrent Angiomyolipoma,
Lymphangioleiomyomatosis. Exclusion Criteria N/A Required Medical Information
HER2 status. Advanced HER2-negative breast cancer, hormone receptor (HR) status.
Age Restrictions N/A
Prescriber Restrictions
N/A
Coverage Duration
Authorization will be for 12 months.
Other Criteria Advanced HER2-negative breast cancer, approve if the patient is a
postmenopausal woman and has HR+ disease and Afinitor will be used in combination with exemestane or tamoxifen and the patient has tried letrozole or anastrozole. Renal cell carcinoma (RCC), approve if patient meets one of the following: 1) patient has advanced RCC with
predominant clear cell histology AND the patient has tried Inlyta, Votrient, has tried Sutent or Nexavar OR 2) patient has relapsed or medically unresectable RCC with non-clear cell histology.Tuberous sclerosis complex (TSC) for the treatment of subependymal giant cell astrocytoma (SEGA), approve if the patient requires therapeutic intervention but cannot be curatively resected.
A
LPHA
-1
P
ROTEINASE
I
NHIBITORS
Products Affected
Aralast Np INJ 400MGProlastin-c
PA Criteria
Criteria Details
Covered Uses All FDA-approved indications not otherwise excluded from Part D. Alpha-1 antitrypsin (AAT) deficiency-associated panniculitis.
Exclusion Criteria N/A Required Medical Information
For AAT deficiency with emphysema (or COPD), approve in patients with baseline (pretreatment) alpha1-antitrypsin serum concentration less than 11 microM (11 micromol/L) or 80 mg/dL.
Age Restrictions N/A
Prescriber Restrictions
N/A
Coverage Duration
Authorization will be for 12 months, unless otherwise specified.
Other Criteria For all covered uses, the patient is required to try Aralast NP first line. For AAT deficiency with emphysema (or COPD), approve in patients with baseline (pretreatment) alpha1-antitrypsin serum concentration less than 11 microM (11 micromol/L) or 80 mg/dL.
9
A
MPYRA
Products Affected
AmpyraPA Criteria
Criteria Details
Covered Uses All FDA-approved indications not otherwise excluded from Part D. Plus patient already started on dalfampridine extended-release for Multiple Sclerosis (MS). Exclusion Criteria N/A Required Medical Information N/A
Age Restrictions N/A
Prescriber Restrictions
MS. If prescribed by, or in consultation with, a neurologist or MS specialist.
Coverage Duration
Authorization will be for 12 mos.
A
NABOLIC
S
TEROIDS
Products Affected
Oxandrolone ORAL TABSPA Criteria
Criteria Details
Covered Uses All FDA-approved indications not otherwise excluded from Part D. Girls w/Turner's Syndrome or Ullrich-Turner Syndrome, management of protein catabolism w/burns or burn injury, AIDS wasting and cachexia.
Exclusion Criteria N/A Required Medical Information N/A
Age Restrictions N/A
Prescriber Restrictions
N/A
Coverage Duration
Authorization will be for 12 months, unless otherwise specified.
11
A
RCALYST
Products Affected
ArcalystPA Criteria
Criteria Details
Covered Uses All FDA-approved indications not otherwise excluded from Part D. Plus patient already started on rilonacept for Muckle Wells Syndrome (MWS) or Familial Cold Autoinflammatory Syndrome (FCAS).
Exclusion Criteria
Rilonacept should not be given in combination with tumor necrosis factor (TNF) blocking agents (eg, adalimumab, certolizumab pegol, etanercept, golimumab, infliximab), anakinra, or canakinumab.
Required Medical Information
N/A
Age Restrictions Greater than or equal to 12 years of age.
Prescriber Restrictions
Prescribed by, or in consultation with, a rheumatologist, geneticist, or dermatologist.
Coverage Duration
Initial approval of MWS/FCAS, 2 mos. Subsequent authorization for 12 mos if patient had a response.
Other Criteria Patients already started on rilonacept for MWS/FCAS may receive authorization if they have had a response and are continuing therapy to maintain response/remission.
B
OSULIF
Products Affected
BosulifPA Criteria
Criteria Details
Covered Uses All FDA approved indications not otherwise excluded from Part D. Plus patients already started on Bosulif for a Covered Use.
Exclusion Criteria N/A Required Medical Information
Diagnosis for which Bosulif is being used. For chronic myelogenous leukemia (CML), the Philadelphia chromosome (Ph) status of the leukemia must be reported. For CML, prior therapies tried must be reported to confirm resistance or intolerance.
Age Restrictions N/A
Prescriber Restrictions
N/A
Coverage Duration
Authorization will be for 12 months.
Other Criteria For CML, patient must have Ph-positive CML and must have resistance or intolerance to prior therapy for approval.
13
B
OTOX
Products Affected
Botox INJ 100UNITPA Criteria
Criteria Details
Covered Uses All FDA-approved indications not otherwise excluded from Part D. Plus Achalasia. Anal Fissure. BPH. Chronic facial pain/pain associated with TMJ dysfunction. Chronic low back pain. Headache (migraine, chronic tension HA, whiplash, chronic daily HA). Palmar/plantar and facial hyperhidrosis. Myofascial pain. Salivary hypersecretion. Spasticity (eg, due to cerebral palsy, stroke, brain injury, spinal cord injury, MS, hemifacial spasm). Essential tremor. Dystonia other than cervical (eg, focal dystonias, tardive dystonia, anismus). Frey's syndrome (gustatory sweating). Ophthalmic disorders (eg, esotropia, exotropia, nystagmus, facial nerve paresis). Speech/voice disorders (eg, dysphonias). Tourette's syndrome. Additional indications will be evaluated by a pharmacist and/or a physician on a case-by-case basis.
Exclusion Criteria
Use in the management of cosmetic uses (eg, facial rhytides, frown lines, glabellar wrinkling, horizontal neck rhytides, mid and lower face and neck rejuvenation, platsymal bands, rejuvenation of the peri-orbital region), allergic rhinitis, gait freezing in Parkinsons disease, vaginismus, interstitial cystitis, trigeminal neuralgia, or Crocodile tears syndrome.
Required Medical Information
N/A
Age Restrictions N/A
Prescriber Restrictions
Headache if prescribed by, or after consultation with, a neurologist or HA specialist.
Coverage Duration
Other Criteria Primary axillary hyperhydrosis after trial with at least 1 topical agent (eg, aluminum chloride). BPH after trial with at least 2 other therapies (eg, alpha1-blocker, 5 alpha-reductase inhibitor, TURP, transurethral microwave heat treatment, TUNA, interstitial laser therapy, stents,
various forms of surgery). Chronic low back pain after trial with at least 2 other pharmacologic therapies (eg, NSAID, antispasmodics, muscle relaxants, opioids, antidepressants) and if being used as part of a multimodal therapeutic pain management program. Headache (eg, migraine, chronic tension headache, whiplash, chronic daily headache) after a trial with at least 2 other pharmacologic therapies (eg,
anticonvulsants, antidepressants, beta-blockers, calcium channel blockers, non-steroidal anti-inflammatory drugs). Palmar/plantar and facial
hyperhidrosis after a trial with at least 1 topical agent (eg, aluminum chloride). Essential tremor after a trial with at least 1 other pharmacologic therapy (eg, primidone, propranolol, benzodiazepines, gabapentin,
topiramate). Urinary incontinence after a trial with at least 1 other pharmacologic therapy (eg, oral antimuscarinic agents). Tourette’s syndrome if after a trial with at least 1 more commonly used pharmacologic therapy (eg, neuroleptics, clonidine, SSRIs, psychostimulants).
15
C
HENODAL
Products Affected
ChenodalPA Criteria
Criteria Details
Covered Uses All FDA-approved indications not otherwise excluded from Part D.
Exclusion Criteria N/A Required Medical Information N/A
Age Restrictions N/A
Prescriber Restrictions
N/A
Coverage Duration
Authorization will be for 12 months.
Other Criteria For the treatment of gallstones, approve if the patient has tried or is currently using an ursodiol product.
C
HORIONIC
G
ONADOTROPINS
(
HCG
)
Products Affected
Chorionic Gonadotropin INJPA Criteria
Criteria Details
Covered Uses All FDA-approved indications not otherwise excluded from Part D.
Exclusion Criteria N/A Required Medical Information N/A
Age Restrictions Prepubertal cryptorchidism, 4 years or older.
Prescriber Restrictions
N/A
Coverage Duration
Authorization will be for 12 months, unless noted otherwise.
17
C
IALIS
Products Affected
Cialis ORAL TABS 2.5MG, 5MGPA Criteria
Criteria Details
Covered Uses All FDA-approved indications not otherwise excluded from Part D.
Exclusion Criteria N/A Required Medical Information
Indication for which tadalafil is being prescribed.
Age Restrictions N/A
Prescriber Restrictions
N/A
Coverage Duration
Authorization will be for 12 mos.
Other Criteria Benign prostatic hyperplasia (BPH), after confirmation that tadalafil is being prescribed to treat the signs and symptoms of BPH and not for the treatment of erectile dysfunction (ED) and after a trial of an alpha-1 blocker (eg, doxazosin [Cardura XL], terazosin, tamsulosin [Flomax], alfuzosin extended-release [UroXatral]) or 5 alpha reductase inhibitor (eg, finasteride, dutasteride [Avodart]).
C
IMZIA
Products Affected
CimziaPA Criteria
Criteria Details
Covered Uses All FDA-approved indications not otherwise excluded from Part D plus patients already started on certolizumab pegol for Covered use.
Exclusion Criteria
Concurrent use with tumor necrosis factor (TNF) alpha antagonists (eg, adalimumab, etanercept, golimumab, and infliximab), or anakinra, rituximab, abatacept, natalizumab, tocilizumab.
Required Medical Information
N/A
Age Restrictions Adults.
Prescriber Restrictions
RA, prescribed by or in consultation with a rheumatologist. Crohn’s disease, prescribed by or in consultation with a gastroenterologist.
Coverage Duration
Authorization will be for 12 months.
Other Criteria Adult RA, approve if the patient has tried Enbrel or Humira for at least 3 months OR the patient is concurrently receiving MTX OR the patient has a contraindication or intolerance to MTX and leflunomide OR the patient has early RA (defined as disease duration of less than 6 months) with at least one of the following features of poor prognosis: functional limitation (eg, based on HAQ-DI score), extraarticular disease such as rheumatoid nodules, RA vasculitis, or Felty’s syndrome, positive rheumatoid factor or anti-CCP antibodies, or bony erosions by radiograph. Adult CD, approve if patient has previously tried Humira OR the patient has tried or is currently taking corticosteroids, unless contraindicated.
19
C
INRYZE
Products Affected
CinryzePA Criteria
Criteria Details
Covered Uses All FDA-approved indications not otherwise excluded from Part D. Plus for the acute treatment of Hereditary Angioedema (HAE).
Exclusion Criteria N/A Required Medical Information N/A
Age Restrictions N/A
Prescriber Restrictions
Must be prescribed by, or in consultation with, an allergist/immunologist or a physician that specializes in the treatment of HAE or related
disorders.
Coverage Duration
Authorization will be for 12 months.
C
OMETRIQ
Products Affected
CometriqPA Criteria
Criteria Details
Covered Uses All FDA approved indications not otherwise excluded from Part D. Plus patients already started on Cometriq for a Covered Use.
Exclusion Criteria N/A Required Medical Information
Diagnosis of progressive, metastatic medullary thyroid cancer.
Age Restrictions N/A
Prescriber Restrictions
N/A
Coverage Duration
Authorization will be for 12 months.
21
C
OPAXONE
Products Affected
Copaxone INJ 20MG/MLPA Criteria
Criteria Details
Covered Uses All FDA-approved indications not otherwise excluded from Part D.
Exclusion Criteria
Concurrent use with other disease-modifying agent used for multiple scelorosis (ie, interferon beta-1a, interferon beta-1b, natalizumab, fingolimod).
Required Medical Information
Multiple Sclerosis (MS) diagnosis worded or described as patients with a diagnosis of MS or have experienced an attack and who are at risk of MS.
Age Restrictions N/A
Prescriber Restrictions
Prescribed by or after consultation with a neurologist or an MS specialist.
Coverage Duration
Authorization will be for 12 months, unless otherwise specified.
C
RINONE
G
EL
Products Affected
Crinone GEL 8%PA Criteria
Criteria Details
Covered Uses All FDA-approved indications not otherwise excluded from Part D. Plus, secondary amenorrhea, support of an established pregnancy.
Exclusion Criteria
Use in patients to supplement or replace progesterone in the management of infertility.
Required Medical Information
N/A
Age Restrictions N/A
Prescriber Restrictions
N/A
Coverage Duration
Secondary amenorrhea, 12 months.Support of an established pregnancy, 9 months.
23
D
ALIRESP
Products Affected
DalirespPA Criteria
Criteria Details
Covered Uses All FDA-approved indications not otherwise excluded from Part D
Exclusion Criteria N/A Required Medical Information
Chronic Obstructive Pulmonary Disease (COPD), FEV1 results to confirm severity, medications tried.
Age Restrictions N/A
Prescriber Restrictions
N/A
Coverage Duration
Authorization will be for 12 months.
Other Criteria COPD, approve in patients who meet all of the following conditions: Patients has severe COPD (defined as an FEV1 less than 50% predicted) or very severe COPD (defined as FEV1 less than 30% predicted), AND Patient has chronic bronchitis, AND Patient has a history of
exacerbations, AND Patient has tried a medication from two of the three following drug categories: long-acting beta2-agonist (LABA) [eg, salmeterol, formoterol], long-acting anticholinergic (eg, tiotropium), inhaled corticosteroid (eg, fluticasone).
E
NBREL
Products Affected
EnbrelPA Criteria
Criteria Details
Covered Uses All FDA-approved indications not otherwise excluded from Part D plus patient already on etanercept for a Covered Use.Graft versus host disease (GVHD). Behcet's disease. Autoimmune mucocutaneous blistering diseases (pemphigus vulgaris, mucous membrane pemphigoid [cicatricial pemphigoid]) (AMBD) . Uveitis
Exclusion Criteria
Concurrent use with adalimumab, anakinra, abatacept, certolizumab pegol, ustekinumab, infliximab, rituximab, golimumab, or tocilizumab.
Required Medical Information
N/A
Age Restrictions For use in rheumatoid arthritis (RA), approve for adults. For juvenile idiopathic arthritis (JIA) approve for children aged 2 years and older.
Prescriber Restrictions
RA/Ankylosing spondylitis/JIA/JRA,prescribed by or in consult w/ rheumatologist. Psoriatic arthritis, prescribed by or in consultation w/ rheumatologist or dermatologist.Plaque psoriasis (PP)/AMBD, prescribed by or in consult w/ dermatologist.GVHD,prescribed by or in consult w/ oncologist,hematologist,or physician affiliated w/ transplant
center.Behcet’s disease,prescribed by or in consult w/
rheumatologist,dermatologist,ophthalmologist,gastroenterologist,or neurologist. Uveitis- ophthalmol
Coverage Duration
25
Other Criteria RA, Tried 1 DMARD for 3 mos or is also receiving MTX, has a
contraindication or intolerance to MTX and leflunomide, or has early RA (defined as disease duration of less than 6 months) with at least one of the following features of poor prognosis: functional limitation, extraarticular disease such as rheumatoid nodules, RA vasculitis, or Felty’s syndrome, positive rheumatoid factor or anti-CCP antibodies, or bony erosions by radiograph. JIA/JRA, approve if the pt has aggressive disease or the pt has tried one other agent for this condition (eg, MTX, sulfasalazine,
leflunomide, NSAID, biologic DMARD or the pt will be started on Enbrel concurrently with MTX, sulfasalazine, or leflunomide or the pt has an absolute contraindication to MTX (eg, pregnancy, breast feeding, alcoholic liver disease, immunodeficiency syndrome, blood dyscrasias), sulfasalazine, or leflunomide.Plaque psoriasis (PP). Approve if the patient has tried at least one of the following agents for at least 3 months for plaque psoriasis: an oral therapy for psoriasis (eg, MTX, cyclosporine, Soriatane), oral methoxsalen plus PUVA, or a biologic agent OR the patient had intolerance to a trial of at least one oral or biologic therapy for plaque psoriasis OR the patient has a contraindication to one oral agent for psoriasis such as MTX. GVHD. Tried or currently is receiving with etanercept 1 conventional GVHD tx (high-dose SC, CSA, tacrolimus, MM, thalidomide, antithymocyte globulin, etc.). Behcet's. Have not responded to at least 1 conventional tx (eg, CS, immunosuppressant, interferon alfa, MM, etc) or adalimumab or infliximab. AMBD. Tried 2 conventional txs (eg, systemic corticosteroids, azathioprine,
cyclophosphamide, dapsone, MTX, cyclosporine, mycophenolate mofetil). Uveitis, tried 1 of the following periocular, intraocular, or systemic CS, immunosuppressives, Humira or Remicade
E
POETIN
/
PROCRIT
Products Affected
ProcritPA Criteria
Criteria Details
Covered Uses All FDA-approved indications not otherwise excluded from Part D worded as anemia associated with chronic renal failure (CRF), including patients on dialysis and not on dialysis, and worded as anemia secondary to myelosuppressive anticancer chemotherapy in solid tumors, multiple myeloma, lymphoma, and lymphocytic leukemia. Plus anemia in patients with HIV who are receiving zidovudine. Anemic patients (Hb of 13.0 g/dL or less) at high risk for perioperative transfusions (secondary to significant, anticipated blood loss and are scheduled to undergo elective, noncardiac, nonvascular surgery to reduce the need for allogeneic blood transfusions). Anemia due to myelodysplastic syndrome (MDS). Anemia associated with use of ribavirin therapy for hepatitis C (in combination with interferon or pegylated interferon alfa 2a/2b products with or without the direct-acting antiviral agents Victrelis or Incivek). Anemia in HIV-infected patients. Exclusion Criteria N/A Required Medical Information
Confirmation of adequate iron stores (eg, prescribing information recommends supplemental iron therapy when serum ferritin is less than 100 mcg/L or when serum transferrin saturation is less than 20%).CRF anemia in patients on dialysis.Hemoglobin (Hb) of less than 10.0 g/dL for adults or less than or equal to 11 g/dL for children to start.Hb less than or equal to 11.5 g/dL for adults or 12 g/dL or less for children if previously on epoetin alfa or Aranesp.CRF anemia in patients not on dialysis.
Hemoglobin (Hb) of less than 10.0 g/dL for adults or less than or equal to 11 g/dL in children to start or Hb less than or equal to 11.5 g/dL in adults or 12 g/dL or less in children.Anemia w/myelosuppressive chemotx.Hb 10.0 g/dL or less to start.Hb less than or equal to 12.0 g/dL if previously on epoetin alfa or Aranesp.MDS, approve if Hb is 10 g/dL or less or serum erythropoietin level is 500 mU/mL or less to start.Previously receiving Aranesp or EA, approve if Hb is 12.0 g/dL or less. Anemia in HIV (with or without zidovudine), Hb is 10.0 g/dL or less or endogenous erythropoetin levels are 500 munits/mL or less at tx start.Previously on EA approve if Hb is 12.0 g/dL or less.Anemia due to ribavirin for Hep C, Hb is 10.0 g/dL or less at tx start. Previously on EA or Aranesp approve if Hb is 12.0 g/dL or less.
27
Prescriber Restrictions
MDS anemia, prescribed by or in consultation with, a hematologist or oncologist. Hep C anemia, prescribed by or in consultation with hepatologist, gastroenterologist or infectious disease physician who specializes in the management of hepatitis C.
Coverage Duration
Anemia w/myelosuppressive = 4 mos.MDS=6mo.Transfus=1 mo.Other=6mo. HIV + zidovudine = 4 mo
Other Criteria Part B versus Part D determination will be made at time of prior
authorization review per CMS guidance to establish if the drug prescribed is to be used for an end-stage renal disease (ESRD)-related condition.
E
RIVEDGE
Products Affected
ErivedgePA Criteria
Criteria Details
Covered Uses All FDA-approved indications not otherwise excluded from Part D. Plus, patient already started on Erivedge for a covered use.
Exclusion Criteria N/A Required Medical Information N/A
Age Restrictions N/A
Prescriber Restrictions
N/A
Coverage Duration
Authorization will be for 12 months
Other Criteria Locally advanced basal cell carcinoma (LABCC), approve if the patient’s BCC has recurred following surgery or the patient is not a candidate for surgery or radiation therapy.
29
F
IRAZYR
Products Affected
FirazyrPA Criteria
Criteria Details
Covered Uses All FDA-approved indications not otherwise excluded from Part D.
Exclusion Criteria N/A Required Medical Information N/A
Age Restrictions N/A
Prescriber Restrictions
Prescribed by, or in consultation with, an allergist/immunologist or a physican that specializes in the treatment of HAE or related disorders.
Coverage Duration
Authorization will be for 12 mos.
F
ORTEO
Products Affected
ForteoPA Criteria
Criteria Details
Covered Uses All FDA-approved indications not otherwise excluded from Part D.
Exclusion Criteria
Concomitant use with other medications for osteoporosis (eg, denosumab [Prolia], bisphosphonates, raloxifene, calcitonin nasal spray [Miacalcin, Fortical]), except calcium and Vitamin D.
Required Medical Information
N/A
Age Restrictions N/A
Prescriber Restrictions
N/A
Coverage Duration
Authorization will be for up to 2 years in a patient’s lifetime.
Other Criteria Treatment of PMO, approve if pt has tried one oral bisphosphonate OR pt cannot take an oral bisphosphonate because the pt cannot swallow or has difficulty swallowing or the pt cannot remain in an upright position post oral bisphosphonate administration or pt has a pre-existing GI medical condition (eg, patient with esophageal lesions, esophageal ulcers, or abnormalities of the esophagus that delay esophageal emptying [stricture, achalasia]), OR pt has tried an IV bisphosphonate (ibandronate or
zoledronic acid), OR pt has severe renal impairment (creatinine clearance less than 35 mL/min) or CKD or pt has had multiple osteoporotic
fractures. Increase bone mass in men with primary or hypogondal
osteoporosis/Treatment of men and women with GIO, approve if pt tried one oral bisphosphonate OR pt cannot take an oral bisphosphonate because the patient cannot swallow or has difficulty swallowing or the patient cannot remain in an upright position post oral bisphosphonate administration or has a pre-existing GI medical condition (eg, patient with esophageal lesions, esophageal ulcers, or abnormalities of the esophagus that delay esophageal emptying [stricture, achalasia]), OR pt has tried zoledronic acid (Reclast), OR pt has severe renal impairment (CrCL less than 35 mL/min) or has CKD or has had multiple osteoporotic fractures.
31
G
ILENYA
Products Affected
GilenyaPA Criteria
Criteria Details
Covered Uses All FDA-approved indications not otherwise excluded from Part D.
Exclusion Criteria
Concurrent use of Gilenya with other disease-modifying agents used for multiple sclerosis (MS).
Required Medical Information
For use in MS, patient has a relapsing form of MS.
Age Restrictions N/A
Prescriber Restrictions
Prescribed by, or in consultation with, a neurologist or an MS specialist.
Coverage Duration
Authorization will be for 12 months.
Other Criteria For use in MS, patient has a relapsing form of MS and is not currently taking Gilenya, approve if the patient has tried interferon beta-1a intramuscular (Avonex), interferon beta-1a subcutaneous (Rebif),
interferon beta-1b (Betaseron or Extavia), glatiramer acetate (Copaxone), teriflunomide (Aubagio), or natalizumab (Tysabri) or if the patient is unable to administer injections due to dexterity issues or visual
impairment. Patient has a relapsing form of MS and is currently receiving Gilenya, approve without a trial of a disease modifying injectable for MS.
G
ILOTRIF
Products Affected
GilotrifPA Criteria
Criteria Details
Covered Uses All FDA-approved indications not otherwise excluded from Part D.
Exclusion Criteria N/A Required Medical Information
For NSCLC - EGFR exon deletions or mutations
Age Restrictions N/A
Prescriber Restrictions
N/A
Coverage Duration
Authorization will be for 12 months.
Other Criteria For the treatment of metastatic non small cell lung cancer (NSCLC) must be used in tumors with epidermal growth factor receptor (EGFR) exon 19 deletions or exon 21 (L858R) substitution mutations
33
G
LEEVEC
Products Affected
GleevecPA Criteria
Criteria Details
Covered Uses All medically-accepted indications not otherwise excluded from Part D. Plus patients already started on Gleevec for a Covered Use.
Exclusion Criteria N/A Required Medical Information
Diagnosis for which Gleevec is being used. For indications of CML and ALL, the Philadelphia chromosome (Ph) status of the leukemia must be reported. New patients with CML and ALL which is Ph-positive may receive authorization for Gleevec.
Age Restrictions N/A
Prescriber Restrictions
N/A
Coverage Duration
Authorization will be for 12 months.
Other Criteria For CML, new patient must have Ph-positive CML for approval of Gleevec. For ALL, new patient must have Ph-positive ALL for approval of Gleevec.
G
ROWTH
H
ORMONES
Products Affected
Norditropin FlexproNorditropin Nordiflex Pen INJ 30MG/3ML
Omnitrope INJ 5MG/1.5ML
PA Criteria
Criteria Details
Covered Uses All FDA-approved indications not otherwise excluded from Part D. Growth hormone (GH) deficiency (DF). Non-GH deficient short stature (idiopathic short stature, ISS). Turner’s syndrome (TS). SHOX (short stature homeobox-containing gene) deficiency. Chronic kidney disease (CKD). Prader-Willi syndrome (PW). Noonan syndrome (NS). Short bowel syndrome (SBS).
Exclusion Criteria
Use in the management of acute critical illness due to complications of surgery, trauma, or with acute respiratory failure, as antiaging therapy, to improve functional status in elderly, somatopause, enhancement of athletic ability, bone marrow transplant (BMT) without total body irradiation, bony dysplasias, burn injury, cardiac transplantation, central precocius puberty, chronic fatigue syndrome, congenital adrenal
hyperplasia, constitutional delay of growth and puberty, corticosteroid-induced short stature including a variety of chronic glucocorticoid-dependent conditions, such as asthma, juvenile rheumatoid arthritis, after renal, heart, liver, or BMT, Crohn's disease, cystic fibrosis, dilated cardiomyopathy/heart failure, end-stage renal disease in adults undergoing hemodialysis, Down's syndrome, familial dysautonomia, fibromyalgia, HIV-infected patients with alterations in body fat distribution, infertility, kidney transplant patients (children) with a functional renal allograft, liver transplantation, multiple system atrophy, myelomeningocele, obesity, osteogenesis imperfecta, osteoporosis
(postmenopausal, idiopathic in men, glucocorticoid-induced), thalassemia, and X-linked hypophosphatemic rickets (familial hypophosphatemia, hypophosphatemic rickets).
35
Required Medical Information
Child/adol GH DF initial tx, eval by an endocrin, documented GH stim test w/GH response less than 10 ng/mL AND base Ht less than the 10th pct for gender/age + pretx Ht growth rate (GR) child less than 3 yrs of less than 7 cm/yr and child greater than or equal to 3 yrs of less than 4 cm/yr OR child/adol less than 18 yrs of age GR less than the 10th pct for
age/gender based on min 6 mo data.Child w/brain radiation does not have to meet bas Ht crit.Congenital hypopituit does not have to meet Ht or GR crit.Child w/hypophysectomy,approve.Child/adol GH DF cont tx, GR increased by 4 cm/yr or more in most recent yr (MRY) + epiphyses open (between 12 and 18 yrs),both crit exclude adol w/hypopituit.Review GR annually.Adoles/yng adult w/completed linear growth (GR less than 2 cm/yr), review for adult GH DF.Greater than 18 yrs,GR increased by 4 cm/yr or more in MRY AND epiphyses open, auth not allowed if midparental ht attained.ISS child w/open epiphyses,6 mo trial if base Ht less than 5th pct + pretx GR child greater than or equal to 7 yrs of less than 4 cm/yr and child 3 or more yrs of less than 4 cm/yr OR child any age GR less than the 10th pct for age/gender based on min 6 mo of data and has condition which GH effective + endocrinol certifies via bone-age x-ray, + the pt doesn’t have constitutional delay of growth and puberty (CDGP).Auth after initial tx based on adequate clinical response
(annualized GR doubles).Cont tx, at least 7 yrs and received somatropin on 6 mo trial, if GR has doubled in comparison to previous yr. At least 7 and less than 12 yrs, GR increased by 4 cm/yr or more in MRY. At least 12 and less than or equal to 18 yrs), GR increased by 4 cm/yr or more in MRY AND epiphyses open).Greater than 18 yrs, GR increased by 4 cm/yr or more in MRY,+ epiphyses open auth not allowed if midparental ht attained.Adult GH DF or PW/trans adoles, eval by endocrinol (start and annually).NS/SHOX/child PW, eval by an endocrinol, CKD, eval by an endocrinol or nephrologist.
Age Restrictions Child/adolesc w/GH DF (initial tx), adolescent is less than or equal to 18 years of age.TS, children. SHOX/CRI/NS, children/adolescents.HIV infection w/wasting or cachexia, less than or equal to 18 years of age.SBS/HIV cachexia/wasting, adults.
Prescriber Restrictions
For adults, the endocrinologist must certify that the somatropin is not being prescribed for anti-aging therapy or to enhance athletic ability.
Coverage Duration
GH DF 12 mos.SBS 4-8wks/yr.Non-GH DF ISS 6 mos.HIV wast/cach 24 wks.
Other Criteria Adult GH DF (start), document diagnosis of GH DF due to adult-onset (GH alone or multiple hormone deficiencies/hypopituitarism from
pituitary dz, hypothalamic dz, surgery, cranial radiation tx, tumor txment, traumatic brain injury, or subarachnoid hemorrhage) or due to childhood-onset (GH not rec in adults who had GH tx as child for uses not due to GH DF) AND negative response to 1 GH stim test (insulin tolerance [peak less than 5 mcg/L], or glucagon [peak less than 3 mcg/L]) [GHRH plus arginine may be used if available] (exclude stim test for childhood-onset due to mutations, lesions, congenital defects), transition adoles off somatropin 1 mo before retesting, OR 3 or more pituitary hormone deficiencies (TSH, ACTH, LH/FSH, or AVP) AND serum IGF-1 84 microg/L or less using the Esoterix ECB RIA or age/gender adjusted serum IGF-1 SDS below the lower limits of the normal reference range for the reporting laboratory.TS start, female and has short stature (SS).SHOX start, open epiphyses AND baseline Ht less than the 3rd percentile for gender/age.CRI w/growth failure (GF), start, approve.Child PW w/GF or adult PW, approve.NS start, baseline ht less than 5th
percentile.TS/SHOX/CKD/child PW/NS, cont tx, GR increased by 2.5 cm/yr or more in most recent yr (MRY) AND epiphyses open.PW, Cont tx in Adult OR adolescent, GR increased by 2.5 cm/yr or more in most recent yr.HIV w/wasting or cachexia, HIV-positive AND have 1 of the following, documented unintentional wt loss of greater than or equal to 10% from baseline OR wt less than 90% of the lower limit of ideal body wt OR BMI less than or equal to 20 kg/m2 AND wasting or cachexia that is due to malabsorption, poor diet, opportunistic infection, depression, and other causes have been addressed prior to starting somatropin AND on antiretroviral tx greater than or equal to 30 days prior to beginning GH tx and will continue antiretroviral tx throughout GH txment. Repeat 12 or 24-wk courses of GH may be authorized after initial 12 or 24-wk GH course for HIV infection w/wasting or cachexia provided that they are off GH for at least 1 mo and meet all of previous HIV criteria.HIV-assoc failure to thrive.Able to consume or be fed via parenteral or enteral feedings 75% or more of maintenance energy requirements based on current body wt AND on antiretroviral tx for greater than or equal to 30 days prior to beginning GH tx and will continue antiretroviral tx.SBS, receiving specialized nutritional support.SBS pts approve for a second 4-wk course if adult responded to somatropin therapy w/ a decrease in requirement for specialized nutritional support according to prescribing physician.
37
H
IGH
R
ISK
M
EDICATIONS
-
B
ENZODIAZEPINES
Products Affected
Clonazepam ORAL TABS Clonazepam Odt
Clorazepate Dipotassium ORAL TABS 15MG
Diazepam RECTAL GEL
Lorazepam ORAL TABS 0.5MG Onfi ORAL TABS 10MG, 20MG Onfi SUSP
Oxazepam Temazepam
PA Criteria
Criteria Details
Covered Uses All medically accepted indications not otherwise excluded from Part D.
Exclusion Criteria N/A Required Medical Information N/A
Age Restrictions Patients aged less than 65 years, approve. Patients aged 65 years and older, other criteria apply.
Prescriber Restrictions
N/A
Coverage Duration
Procedure-related sedation = 1mo. All other conditions = 12 months.
Other Criteria All medically accepted indications other than Restless Leg Syndrome and insomnia, authorize use. Restless Leg Syndrome, approve clonazepam or temazepam if the patient has tried one other agent for this condition (eg, ropinirole, pramipexole, carbidopa-levodopa [immediate-release or extended-release]). Insomnia, approve lorazepam, oxazepam, or temazepam if the patient has had a trial with two of the following: ramelteon, trazodone, doxepin 3mg or 6 mg, eszopiclone, zolpidem, or zaleplon.
H
IGH
R
ISK
M
EDICATIONS
-
F
IRST
G
ENERATION
A
NTIHISTAMINES
Products Affected
Hydroxyzine Hcl ORAL SOLN Hydroxyzine Hcl ORAL TABS
Promethazine Hcl ORAL TABS Promethazine Hcl SYRP
PA Criteria
Criteria Details
Covered Uses All FDA-approved indications not otherwise excluded from Part D.
Exclusion Criteria N/A Required Medical Information N/A
Age Restrictions Patients aged less than 65 years, approve. Patients aged 65 years and older, other criteria apply.
Prescriber Restrictions
N/A
Coverage Duration
Authorization will be for 12 months.
Other Criteria For promethazine tablets/syrup, authorize use without a previous drug trial for all FDA-approved indications other than emesis, including cancer/chemo-related emesis. For diphenhydramine capsules/elixir, authorize use without a previous drug trial for all FDA-approved indications other than insomnia. For hydroxyzine hydrochloride tablets/syrup, authorize use without a previous drug trial for all FDA-approved indications other than anxiety. For the treatment of
non-cancer/chemo related emesis, approve promethazine hydrochloride tablets or syrup if the patient has tried a prescription oral anti-emetic agent (ondansetron, granisetron, dolasetron, palonosetron, aprepitant) for the current condition. Approve diphenhydramine (capsules or elixir) if the patient has tried at least two other FDA-approved products for the management of insomnia. Approve hydroxyzine hydrochloride (tablets and syrup) or hydroxyzine pamoate (capsules) if the patient has tried at least two other FDA-approved products for the management of anxiety.
39
H
IGH
R
ISK
M
EDICATIONS
-
T
ERTIARY
T
RICYCLIC
A
NTIDEPRESSANTS
Products Affected
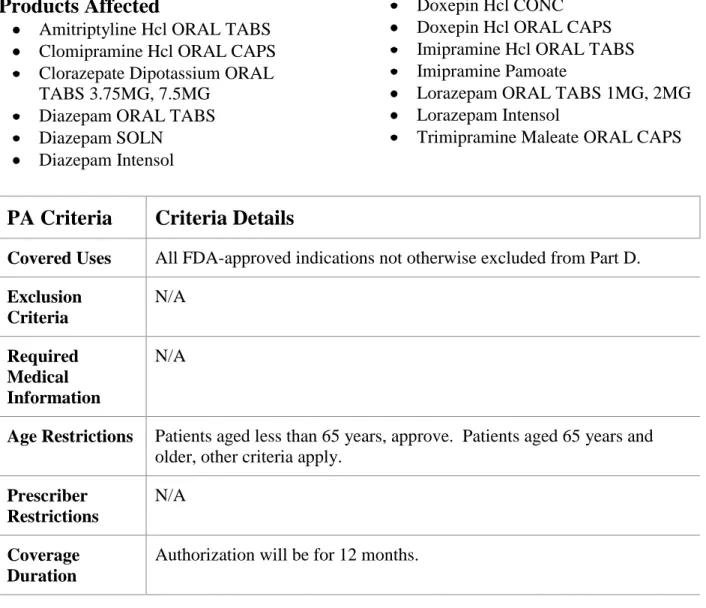
Amitriptyline Hcl ORAL TABS Clomipramine Hcl ORAL CAPS Clorazepate Dipotassium ORAL TABS 3.75MG, 7.5MG
Diazepam ORAL TABS Diazepam SOLN
Diazepam Intensol
Doxepin Hcl CONC Doxepin Hcl ORAL CAPS Imipramine Hcl ORAL TABS Imipramine Pamoate
Lorazepam ORAL TABS 1MG, 2MG Lorazepam Intensol
Trimipramine Maleate ORAL CAPS
PA Criteria
Criteria Details
Covered Uses All FDA-approved indications not otherwise excluded from Part D.
Exclusion Criteria N/A Required Medical Information N/A
Age Restrictions Patients aged less than 65 years, approve. Patients aged 65 years and older, other criteria apply.
Prescriber Restrictions
N/A
Coverage Duration
Other Criteria For the treatment of depression, approve if the patient has tried at least two of the following agents (brand or generic): citalopram, escitalopram, fluoxetine, paroxetine, sertraline, venlafaxine, desvenlafaxine, duloxetine, bupropion, mirtazapine, nortriptyline, desipramine, or trazodone. For the treatment of pain, may approve amitriptyline (single-entity only, not amitriptyline combination products) or imipramine (brand or generic) if the patient has tried at least two of the following agents: duloxetine, pregabalin, gabapentin, venlafaxine, venlafaxine Er, desipramine, or notriptyline. For the mangement of insomnia, may approve amitriptyline (single-entity only, not amitriptyline combination products), doxepin greater than 6 mg, or imipramine (brand or generic) if the patient has tried at least two of the following medications: ramelteon, trazodone, or
doxepin 3 mg or 6 mg. For the treatment of obessessive compulsive disorder (OCD), may approve clomipramine (brand or generic) if the patient has tried at least two of the following medications: fluoxetine, fluvoxamine, paroxetine, sertraline, citalopram, escitalopram, or venlafaxine.
41
H
UMIRA
Products Affected
HumiraHumira Pen-crohns Diseasestarter
PA Criteria
Criteria Details
Covered Uses All FDA-approved indications not otherwise excluded from Part D plus patients already started on adalimumab for a Covered Use.
Exclusion Criteria
Concurrent use with anakinra, abatacept, rituximab, ustekinumab, certolizumab pegol, etanercept, infliximab, or golimumab.
Required Medical Information
N/A
Age Restrictions RA, adults. Crohn's disease (CD), 6 or older.Ulcerative colitis (UC), adults.
Prescriber Restrictions
RA/JIA/JRA/Ankylosing spondylitis, prescribed by or in consultation with rheumatologist. Psoriatic arthritis (PsA), prescribed by or in consultation with a rheumatologist or dermatologist. Plaque psoriasis (PP), prescribed by or in consultation with a dermatologist. UC/ CD, prescribed by or in consultation with a gastroenterologist.
Coverage Duration
Other Criteria RA, Tried 1 DMARD (brand or generic, oral or injectable) for 3 mos (this includes patients who have tried other biologic DMARDs for 3 mos), or pt is concurrently receiving methotrexate (MTX), or pt has a
contraindication or inolerance to MTX and leflunomide, as determined by prescribing physician, or pt has early RA (defined as disease duration of less than 6 months) with at least one of the following features of poor prognosis: functional limitation, extraarticular disease such as rheumatoid nodules, RA vasculitis, or Felty’s syndrome, positive rheumatoid factor or anti-cyclic citrullinated protein antibodies, or bony erosions by
radiograph. JIA/JRA. Tried another agent (e.g MTX, sulfasalazine, leflunomide, NSAID, or biologic DMARD (eg, etanercept, abatacept, infliximab, anakinra, tocilizumab) or will be starting on adalimumab concurrently with MTX, sulfasalazine, or leflunomide. Approve without trying another agent if pt has absolute contraindication to MTX,
sulfasalazine, or leflunomide or if pt has aggressive disease. Plaque psoriasis (PP). Pt has tried a systemic therapy (eg, MTX, CSA, acritretin, etanercept, infliximab, or ustekinumab) for 3 mos or PUVA) for 3 months , or pt experienced an intolerance to a trial of at least one systemic therapy (oral or biologic therapy), or pt has a contraindication to one oral agent for psoriasis such as MTX, as determined by the prescribing physician. CD. Tried corticosteroids (CSs) or if CSs are contraindicated or if pt currently on CSs or patient has tried one other agent for CD (eg,
azathioprine, 6-mercaptopurine, MTX, certolizumab, infliximab) OR pt had ilecolonic resection. UC. Pt has tried a systemic therapy (eg, 6-mercaptopurine, azathioprine, CSA, tacrolimus, infliximab, or a
corticosteroid such as prednisone or methylprednisolone) for 3 2 months or was intolerant to one of these agents, or the pt has pouchitis and has tried therapy with an antibiotic, probiotic, corticosteroid enema, or mesalamine (Rowasa) enema.
43
I
LARIS
Products Affected
IlarisPA Criteria
Criteria Details
Covered Uses All FDA-approved indications not otherwise excluded from Part D. Plus patients already started on canakinumab (Ilaris) for a Covered Use.
Exclusion Criteria
When used in combination with tumor necrosis factor (TNF) blocking agents (e.g., etanercept, adalimumab, certolizumab pegol, golimumab, infliximab), anakinra, or rilonacept.
Required Medical Information
N/A
Age Restrictions N/A
Prescriber Restrictions
CAPS/MWS/FCAS intial tx- Prescribed by or in consultation with a rheumatologist, geneticist, or dermatologist. SJIA initial tx - prescribed by or in consultation with a rheumatologist
Coverage Duration
Initial approval for MWS or FCAS, one dose, subsequent auth 12 mo if response. SJIA, 12 mos.
Other Criteria For initial approval for MWS or FCAS, authorize one dose. After up to 8 weeks of therapy if the patient has had a response to therapy as
determined by prescribing physician an additional 12 months authorization is allowed. For treatment of SJIA, approve.
I
NCIVEK
Products Affected
IncivekPA Criteria
Criteria Details
Covered Uses All FDA-approved indications not otherwise excluded from Part D. Plus patients current taking Incivek for a Covered Use.
Exclusion Criteria
Patients who have failed therapy with Incivek or another NS3/4A protease inhibitor (e.g., Victrelis) for HCV.
Required Medical Information
N/A
Age Restrictions Adults.
Prescriber Restrictions
Must be prescribed by or in consultation with a gastroenterologist, hepatologist, infectious disease physician, or a liver transplant physician.
Coverage Duration
Authorization will be for 3 months.
45
I
NLYTA
Products Affected
InlytaPA Criteria
Criteria Details
Covered Uses All FDA-approved indications not otherwise excluded from Part D. Plus, patients already started on Inlyta for a Covered Use.
Exclusion Criteria N/A Required Medical Information N/A
Age Restrictions N/A
Prescriber Restrictions
N/A
Coverage Duration
Authorization will be for 12 months
Other Criteria Advanced renal cell carcinoma, approve the patient has failed at least one prior systemic therapy (eg, Torisel, Avastin, Sutent, IFN-alpha, IL-2, Votrient, Nexavar).
I
VIG
Products Affected
Privigen INJ 20GM/200MLPA Criteria
Criteria Details
Covered Uses All FDA-approved indications not otherwise excluded from Part D. Idiopathic thrombocytopenic purpura (ITP) or immune thrombocytopenia, acute and chronic treatment. Kawasaki disease (KD). B-cell CLL in patients with hypogammaglobulinemia and previous history of a serious bacterial infection. Chronic inflammatory demyelinating polyneuropathy (CIDP). Allogeneic bone marrow transplant (BMT) or hematopoietic stem cell transplantation (HSCT). HIV-infected infants and children less than 13 yrs old - prevention of recurrent bacterial infections (PRB) or passive immunization of varicella (chickenpox) [PIV]. Autoimmune hemolytic anemia (AIHA). Autoimmune mucocutaneous blistering diseases (AMBD). CMV interstitial pneumonia in allogeneic BMT or HSCT patients. Dermatomyositis and polymyositis (DaP). End stage heart failure, ESRD, end stage liver or lung disease, or small bowel transplant awaiting transplant or post-transplant, to lower allosensitization.
Desensitization therapy prior to and immediately after solid organ (kidney, heart, lung, liver, intestinal) transplantation. Evans syndrome (EvS). Guillan-Barre syndrome (GBS). HIV-associated thrombocytopenia (HAT). Multifocal acquired demyelinating sensory and motor neuropathy or Lewis-Sumner syndrome. Multifocal motor neuropathy (MMN),
treatment. Multiple myeloma (MM). Multiple sclerosis (MS), acute severe exacerbations (MSase). MS, post-partum to prevent relapses (MSppr). Myasthenia gravis (MG). Pure red blood cell aplasia (PRCA) secondary to chronic parvovirus B19 infection (infxn). PRCA, immunologic subtype. Stiff-person syndrome (SPS). Thrombocytopenia, fetal
alloimmune (TFA). Varicella, postexposure prophylaxis (VPP). Vasculitic syndromes, systemic (VSS). Lambert-Eaton Myasthenic syndrome
(LEMS)
Exclusion Criteria
47
Required Medical Information
ITP acute bleed, tried systemic corticosteroid (CS), or has a CI to tx w/ a CS according to prescribing physician or before surgery/procedure if PC less than 75,000 for majory surgery or less than 50,000 for other. Chronic ITP if patient (pt) tried a systemic CS, or has a CI to tx w/ a CS according to prescribing physician OR there is an urgent need to increase the plt count quickly AND IVIG will be started with a systemic CS. BMT/HSCT in previous yr, AND according to prescribing physician, pt has a
significant risk of having frequent and/or severe bacterial infections despite antibiotic therapy, 6 mos if IgG is less than 500 mg/dL (not applicable to MM, malignant macroglobulinemia). HIV-infected kids PRB, on highly active antiretroviral therapy (HAART), IgG less than 400 mg/dL or functional antibody deficiency (2 or more serious bacterial infections (SBis) in 1 yr-period of HAART and antibiotic prophylaxis or absence of detectable antibody response). HIV-infected kids (PIV), 1 dose if VariZIG unavailable and no history of varicella infection, or seronegative for varicella-zoster virus, or has not received 2 varicella vaccine doses, or is immunized but is moderately/severely
immunocompromised, and no IVIG dose within 2-3 wks of varicella exposure.EvS, refer to ITP or AIHA criteria depending on predominant symptoms.GBS, approve if IVIG started within 2 wks and no longer than 4 wks of neuropathic symptoms onset or initial response to IVIG now having a relapse.HAT, approve 1 mo if significant bleeding or on
antiretroviral therapy (ART)/HAART. MM stable disease, recurrent SBis. LEMS - has paraneoplastic LEMS, tried one CS, AZA, or other
immunosuppressive (CSA, MM), OR has contraind to BOTH CS AND AZA or immunosuppressive.
Age Restrictions HIV-infected infants and children less than 13 yrs old - prevention of recurrent bacterial infxns or passive immunization of varicella
(chickenpox). Still's disease, adult. Retractable epilepsy, children. ITP acute bleed or chronic ITP less than 17 yrs old and adults greater than 17 yrs old.
Prescriber Restrictions
PID,allergist/immunol,immuno,otolaryng,pulmon,or
ID.ITP/AIHA,hematol.KD,ped cardio or ped ID.B-cell CLL/ BMT/HSCT/CMV interstit pneumonia HCT/MM,oncol,hematol,or ID.CIDP/MMN/MG/SPS,neurol.HIV-kids/VPP,ID or immunol.HIV-infected,ID.DaP,neurol or rheuma.GBS,neurol or GBS special.HAT,ID or HIV special.MS exac,MSppr,MS special/neuro.PRCA infxn/PRCA, ID,immunol, hematol, transplant MD.Scleromyxedema,dermatol or rheumatol.TCP,fetal alloimmune,hematol or OB.Vasculitic
syndromes,rheum or nephrol.
Coverage Duration
Acute or surgery ITP,1 mo.CMV/PRCA,2 mo.GBS,1 mo. Fetal allo thrombo,6 mo.Preg ITP,3 mo.Others 12 mo
Other Criteria Part B versus D determination per CMS guidance to establish if drug used for PID in pt’s home. KD, 2nd dose if failed to respond to initial therapy (tx). AIHA, tried systemic CS,or Rituxan (rituximab), OR has a CI to tx w/ a CS or Rituxan (rituximab) according to prescribing physician, or had splenectomy. AMBD, tried conventional txs (eg, systemic CS and
immunosuppresive) OR has a CI to tx w/ a CS according to prescribing physician, or disease rapidly progressive/extensive/debilitating, or inadequate time for tx to have rapid effect. DaP, tried conventional tx of systemic CS and immunosuppressive, OR has a CI to tx w/ a CS or according to prescribing physician. Retractable epilepsy, tried an anticonvulsant and CS. MSase, 1 5-day course if not responded to or significant AE from 2 of following: oral/IV CS tx (if possible), plasma exchange, or adrencorticotropic hormone and continuing to deteriorate. MSppr, 6 mo in women not currently receiving disease-modifying tx. MG, 1 5-day course if MG exacerbation, requires stabilization before surgery, has been started on immunosuppressive drug or responded to previous IVIG course but weakens/relapses and no response to other drugs. PRCA from B19 infxn, 3 mos if chronic immunodeficient condition and clinically significant anemia or transfusion dependent. PRCA immunologic, tried prednisone and CPA or cyclosporine (CSA). VPP, 1 dose if VariZIG not available AND pt does not have evidence of immunity to varicella (i.e. pt has no history of the disease or
age-appropriate vaccination) or pt immunocompromised, or pregnant woman. VSS, patient has anti-neutrophil antibody-associated vasculitis, tried a systemic CS and either CPA, methotrexate (MTX), Rituxan, or AZA.
49
J
AKAFI
Products Affected
JakafiPA Criteria
Criteria Details
Covered Uses All FDA-approved indications not otherwise excluded from Part D. Plus, patients already started on Jakafi for a Covered Use.
Exclusion Criteria N/A Required Medical Information N/A
Age Restrictions N/A
Prescriber Restrictions
N/A
Coverage Duration
Authorization will be for 12 months.
L
ETAIRIS
/
TRACLEER
Products Affected
LetairisTracleer
PA Criteria
Criteria Details
Covered Uses All FDA-approved indications not otherwise excluded from Part D. Patients currently on Letairis or Tracleer for a Covered Use. Chronic thromboembolic pulmonary hypertension (CTEPH) (Tracleer).
Exclusion Criteria N/A Required Medical Information
Pulmonary arterial hypertension (PAH) WHO Group 1patients not currently on Letairis or Tracleer or another agent indicated for WHO Group 1 PAH are required to have had a right-heart catheterization to confirm the diagnosis of PAH to ensure appropriate medical assessment. PAH WHO Group 1 patients currently on Letairis or Tracleer or another agent indicated for WHO Group 1 PAH may continue therapy without confirmation of a right-heart catheterization.
Age Restrictions N/A
Prescriber Restrictions
For treatment of pulmonary arterial hypertension, Letairis or Tracleer must be prescribed by or in consultation with a cardiologist or a pulmonologist.
Coverage Duration
Authorization will be for 12 months, unless otherwise specified.
51
L
EUPROLIDE
(
LONG
A
CTING
)
Products Affected
Lupron Depot INJ 22.5MG, 3.75MG, 30MG, 45MG
Lupron Depot-ped
PA Criteria
Criteria Details
Covered Uses All FDA-approved indications not otherwise excluded from Part D but specific to the following drugs as follows: Prostate cancer (Lupron Depot), Endometriosis (Lupon Depot), Uterine leiomyomata (Lupon Depot), Treatment of central precocious puberty (Lupron Depot Ped). Ovarian cancer (Lupron Depot, Lupron Depot Ped). Breast cancer (Lupron Depot, Lupron Depot Ped). Induce amenorrhea during bone marrow transplant (Lupron Depot, Lupron Depot Ped). Premenstral syndrome (Lupron Depot, Lupron Depot Ped). Catamenial pneumothorax (Lupron Depot, Lupron Depot Ped). Paraphilias or other inappropriate sexual behaviors or disorders (Lupron Depot, Lupron Depot Ped). Dysfunctional uterine bleeding (Lupron Depot, Lupron Depot Ped).
Exclusion Criteria N/A Required Medical Information N/A
Age Restrictions N/A
Prescriber Restrictions
N/A
Coverage Duration
For dysfunctional uterine bleeding approve for up to 6 months and all other indications x 12 mos.
Other Criteria Premenstrual syndrome (PMS) for patients that have tried two other therapies (e.g., selective serotonin reuptake inhibitors [SSRIs], oral contraceptives [OCs]).
L
IDODERM
Products Affected
Lidocaine PTCHLidoderm
PA Criteria
Criteria Details
Covered Uses All FDA-approved indications not otherwise excluded from Part D. Plus diabetic neuropathic pain.
Exclusion Criteria N/A Required Medical Information N/A
Age Restrictions N/A
Prescriber Restrictions
N/A
Coverage Duration
Authorization will be for 12 months, unless otherwise specified.
53
M
EKINIST
Products Affected
MekinistPA Criteria
Criteria Details
Covered Uses All FDA-approved indications not otherwise excluded from Part D. Plus patients already started on Mekinist for a Covered Use.
Exclusion Criteria N/A Required Medical Information
Diagnosis for which Mekinist is being used. For unresectable or metastatic melanoma must have documentation of BRAF V600E or V600K mutations
Age Restrictions N/A
Prescriber Restrictions
N/A
Coverage Duration
Authorization will be for 12 months.
Other Criteria For unresectable or metastatic melanoma must be used in patients with BRAF V600E or V600K mutations
N
EULASTA
Products Affected
NeulastaPA Criteria
Criteria Details
Covered Uses All FDA-approved indications not otherwise excluded from Part D but worded more broadly as cancer patients receiving myelosuppressive chemotherapy. Plus patients undergoing PBPC collection and therapy
Exclusion Criteria N/A Required Medical Information N/A
Age Restrictions N/A
Prescriber Restrictions
Cancer patients receiving chemotherapy, if prescribed by or in consultation with an oncologist or hematologist.
Coverage Duration
Authorization will be for 6months.
Other Criteria Cancer patients receiving chemotherapy, approve if the patient is receiving myelosuppressive anti-cancer medications that are associated with a high risk of febrile neutropenia (the risk is at least 20% based on the chemotherapy regimen), OR the patient is receiving myelosuppressive anti-cancer medications that are associated with a risk of febrile
neutropenia but the risk is less than 20% based on the chemotherapy regimen and the patient has one or more risk factors for febrile
neutropenia (eg, older patient [aged greater than or equal to 65 years]), history of previous chemotherapy or radiation therapy, pre-existing neutropenia, open wounds or active infection, poor performance status, OR the patient has had a neutropenic complication from prior
chemotherapy and did not receive prophylaxis with a colony stimulating factor and a reduced dose or frequency of chemotherapy may compromise treatment.