ARTICLE
Effects of the Accreditation Council for Graduate
Medical Education Duty Hour Limits on Sleep, Work
Hours, and Safety
Christopher P. Landrigan, MD, MPHa,b, Amy M. Fahrenkopf, MD, MPHb, Daniel Lewin, PhDc, Paul J. Sharek, MD, MPHd, Laura K. Barger, PhDa,
Melanie Eisner, BSc, Sarah Edwards, BSa,b, Vincent W. Chiang, MDb, Bernhard L. Wiedermann, MDc, Theodore C. Sectish, MDb,d
aDivision of Sleep Medicine, Department of Medicine, Brigham and Women’s Hospital, andbDepartment of Medicine, Children’s Hospital Boston, Harvard Medical
School, Boston, Massachusetts;cDepartment of Pediatrics, Children’s National Medical Center, George Washington University, Washington, DC;dDivision of General
Pediatrics, Department of Pediatrics, Lucile Packard Children’s Hospital, Stanford Medical School, Palo Alto, California
Financial Disclosure: Dr Landrigan is a paid employee of Brigham and Women’s Hospital and Children’s Hospital Boston, both of which employ interns and residents. He has served as a paid consultant to the District Health Boards of New Zealand and has received research prizes with monetary awards and/or honoraria for delivering lectures on sleep and safety from the National Sleep Foundation, the Sleep Research Society, the Society of Hospital Medicine, and multiple academic medical centers and professional organizations. Drs Fahrenkopf and Chiang are paid employees of Children’s Hospital Boston. Dr Barger is a paid employee of Brigham and Women’s Hospital. Dr Sharek is a paid employee of the Stanford University School of Medicine and Lucile Packard Children’s Hospital, both of which employ interns and residents; in addition, he has served as a paid consultant to the Ohio Children’s Hospital Association and has received honoraria for delivering lectures on quality and safety from multiple academic institutions and organizations. Drs Wiedermann and Lewin are paid employees of Children’s National Medical Center (Washington, DC), which employs interns and residents. Dr Wiedermann is director of medical education at that institution and, at the time of the study, was director of the pediatric residency training program. Dr Sectish currently is director of the pediatric resident training program and a paid employee of Children’s Hospital Boston; at the time of the study, he was director of the pediatric resident training program and a paid employee of Lucile Packard Children’s Hospital.
What’s Known on This Subject
Traditional 24-hour shifts for physicians-in-training are associated with high rates of medical errors and occupational injuries. It has remained unclear whether the ACGME work hour limits, which continue to endorse 24-hour shifts, have reduced this risk.
What This Study Adds
In 3 pediatric centers, implementation of the ACGME duty hour standards did not change total work or sleep hours, medical error rates, occupational injury rates, or resi-dent educational experiences. More-effective policies are needed to reduce fatigue-related injuries and errors.
ABSTRACT
OBJECTIVE.To mitigate the risks of fatigue-related medical errors, the Accreditation Council for Graduate Medical Education introduced work hour limits for resident physicians in 2003. Our goal was to determine whether work hours, sleep, and safety changed after implementation of the Accreditation Council for Graduate Medical Education standards.
METHODS.We conducted a prospective cohort study in which residents from 3 large pediatric training programs provided daily reports of work hours and sleep. In addition, they completed reports of near-miss and actual motor vehicle crashes, occupational exposures, self-reported medical errors, and ratings of educational experience. They were screened for depression and burnout. Concurrently, at 2 of the centers, data on medication errors were collected prospectively by using an established active surveillance method.
RESULTS.A total of 220 residents provided 6007 daily reports of their work hours and sleep, and 16 158 medication orders were reviewed. Although scheduling changes were made in each program to accommodate the standards, 24- to 30-hour shifts remained common, and the frequency of residents’ call remained largely unchanged. There was no change in residents’ measured total work hours or sleep hours. There was no change in the overall rate of medication errors, and there was a borderline increase in the rate of resident physician ordering errors, from 1.06 to 1.38 errors per 100 patient-days. Rates of motor vehicle crashes, occupational exposures, depres-sion, and self-reported medical errors and overall ratings of work and educational
experiences did not change. The mean length of extended-duration (on-call) shifts decreased 2.7% to 28.5 hours, and rates of resident burnout decreased significantly (from 75.4% to 57.0%).
CONCLUSIONS.Total hours of work and sleep did not change after implementation of the duty hour standards. Although fewer residents were burned out, rates of medication errors, resident depression, and resident injuries and educa-tional ratings did not improve.Pediatrics2008;122:250–258
R
ESIDENT PHYSICIANS’ TRADITIONALextended duty shifts of 24 to 30 consecutive hours have been found to pose significant hazards to patients1,2and to the physicians-in-training themselves.3,4To address the risks of long work hours, the Accreditation Council for Graduate Medical Education (ACGME) implemented work hour limits for allwww.pediatrics.org/cgi/doi/10.1542/ peds.2007-2306
doi:10.1542/peds.2007-2306
Key Words
patient safet, medical errors, sleep deprivation, work hours, Accreditation Council for Graduate Medical Education, motor vehicle crashes
Abbreviations
ACGME—Accreditation Council for Graduate Medical Education CI— confidence interval MVC—motor vehicle crash
Accepted for publication Nov 26, 2007
Address correspondence to Christopher P. Landrigan, MD, MPH, Division of Sleep Medicine, Department of Medicine, Brigham and Women’s Hospital, 221 Longwood Ave, Boston, MA 02115. E-mail: clandrigan@ partners.org
resident physicians in the United States in July 2003. Under these regulations, residents can work no more than 30 consecutive hours and no more than 80 to 88 hours/week, averaged over 4 weeks.5Although surveys of health care providers regarding the duty hour stan-dards abound,6–12 rigorously conducted studies of their objectively measured effects are lacking.13
In the European Union, data on sleep deprivation and performance have prompted laws limiting all workers, including physicians and nurses, to 13 consecutive hours and 48 to 56 hours/week.14The ACGME standards pro-hibit shifts of⬎30 consecutive hours but, because 24- to 30-hour shifts continue to be permitted, it is unclear whether the standards are sufficient to reduce rates of fatigue-related errors and injuries substantially. More-over, compliance with the ACGME duty hour standards has been suboptimal,15 which may further limit their potential to effect measurable improvements in safety.
The ACGME Duty Hours Study was initiated in the year before implementation of the standards, in an effort to measure their effects prospectively. Our specific aim was to conduct a comprehensive tricenter study to com-pare residents’ work and sleep hours, medication error rates, health and safety, and work and educational ex-periences before and after implementation of the ACGME duty hour standards.
METHODS
Study Population
In the spring before and the spring after implementation of the ACGME duty hour standards, we advertised a study of work hours, sleep, and safety to all pediatric residents (postgraduate years 1–3) in 3 major pediatric residency programs, namely, the Boston Combined Res-idency Program, the program at the Lucile Packard dren’s Hospital at Stanford, and the program at the Chil-dren’s National Medical Center. Pediatric residents’ work hours are typical of those in most specialties,15,16 but rates of serious medication errors in pediatrics have been found to be relatively high.17Therefore, we antic-ipated sufficient power to measure differences in medi-cation error rates before versus after implementation of the duty hour standards. All categorical and pediatric residents, as well as medicine-pediatric residents, on all pediatric rotations (including inpatient, outpatient, elec-tive, and vacation) were potentially eligible to participate in the study (246 eligible residents in 2003 and 252 eligible residents in 2004). Only residents on extended leave and medicine-pediatric residents working exclu-sively in internal medicine settings during the study period were excluded from consideration. Subjects were informed that, unless an immediate risk to themselves or others was identified (eg, a subject expressed suicidal or homicidal ideation), all individually identifiable data would be coded and kept confidential. Because the Agency for Healthcare Research and Quality supported this research, the data are protected by federal statute (Public Health Service Act 42 USC). Institutional review board approval was obtained at all 3 hospitals.
Study Setting and Interventions
Before implementation of the ACGME duty hour stan-dards, residents were frequently working⬎30 hours in a row and ⬎80 hours/week on many rotations in the study hospitals. Consequently, numerous policies and changes were implemented in July 2003, in an effort to bring the programs into full compliance with the stan-dards. These policies and changes included the imple-mentation of frequent reminders and surveillance by program officials to enforce residents’ on-time departure after call; development of requirements for housestaff members to sign out by noon after call; creation of new associate senior resident positions on some teams, to facilitate the on-time departure of the senior resident after call; rescheduling of continuity clinics; rescheduling of educational conferences; designation of some patients as “uncovered,” meaning that residents were removed from involvement in their care; and hiring of additional residents and nurse practitioners to supplement the res-ident workforce. Of note, however, shifts of 24 to 30 hours remained common and the frequency of those shifts remained unchanged on most rotations, because 24- to 30-hour shifts up to every other shift (a “q3” schedule) continue to be permitted under the ACGME standards.
Subject Data
After providing written informed consent and baseline demographic data, subjects were asked to complete daily logs of their work hours and sleep from the day of their enrollment (late May to early June) through the end of their last rotation of the academic year (on or about June 30 of that year). The precise number of possible log days completed differed among subjects, depending on their day of enrollment and whether the academic year ended precisely on June 30 for that individual in that program (eg, interns in one program finished on June 26 in 2003). Key questions in the log asked what time the subject tried to fall asleep the previous night, how long it took the subject to fall asleep, how many times the subject awakened (with details of the timing and reasons for awakening provided), what time the subject finally woke up, and whether the subject napped the previous day (with details of the timing of naps provided); a recording of all hours actually worked in the previous 24 hours also was provided. We found in a previous study that work hours recorded by interns using a structured daily log instrument correlated very highly with those recorded by third-party observers (r⫽0.98).18Similarly, as reported previously, sleep hours correlated highly with those documented objectively by using polysom-nography (r⫽0.94).18Small cash incentives were pro-vided to subjects to complete all study materials.
(with the health care worker-specific version of the Maslach Burnout Inventory20–22).
The Harvard Department of Psychiatry/National De-pression Screening Day Scale is a 10-item, validated instrument demonstrated to be 94% specific and 95% sensitive in detecting major depression. Subjects in this study were defined as depressed if they scoredⱖ9 on the scale, which indicates a high risk for major depression.19 The Maslach Burnout Inventory is a 22-item, validated instrument considered the standard for determining burnout, a syndrome of mental exhaustion and personal detachment that develops in response to chronic occu-pational stress. The Maslach Burnout Inventory mea-sures emotional exhaustion, depersonalization, and per-sonal achievement; subjects were considered “burned out” if they had either a high score for emotional ex-haustion (score of⬎27) or a high score for depersonal-ization (score of⬎10).20–22
Medication Errors
Concurrent with our collection of data from subjects, objective data on medication errors were collected on the inpatient wards at 2 of the 3 study sites (Boston Combined Residency Program and Lucile Packard Chil-dren’s Hospital) by using an established, comprehensive, surveillance method17,23that included daily chart review and medication order review, as well as collection of voluntary and solicited error reports from clinical staff members. These methods have been used for collection of objective data on medication errors and adverse events in numerous studies and have been shown to have much higher sensitivity than traditional incident-reporting systems,24,25 with moderate to high reliabil-ity.17,26,27Prospective data on medication errors could not be collected at the third site (Children’s National Medical Center); therefore, the site was excluded from this facet of the study.
A team of 6 nurse and physician data extractors trained in medical error detection methods reviewed the care of all patients treated by residents on select inpa-tient wards 5 days/week; reviews on Monday included a review of all data from the weekend. The wards studied were chosen by the investigators as typical, busy, inpa-tient services on which all painpa-tients are cared for by
residents. Residents wrote all medication orders studied, but errors detected anywhere in the medication delivery process (ordering, transcription, pharmacy dispensation, administration, or monitoring) were included in the study. All medication orders, physician notes, nursing notes, and nursing flow sheets were reviewed 5 days/ week; in addition, data extractors asked clinical staff members to report any suspected errors or adverse events to them, and formal incident reports were re-viewed. For all suspected errors or adverse events iden-tified through any of these mechanisms, detailed clinical and demographic data were recorded. After completion of year 2 data collection efforts (after work hour stan-dards implementation), each suspected error was classi-fied independently by 2 physician investigators (Drs Fahrenkopf and Landrigan), who were blinded to whether the incident was captured before or after im-plementation of the duty hour standards. Definitions used to classify all incidents (with examples of incidents captured in the study) are provided in Table 1. In addi-tion to classifying each incident according to category, reviewers rated independently the preventability of ad-verse events by using a 5-point Likert scale (prevented, definitely preventable, probably preventable, probably not preventable, or definitely not preventable); the scale was dichotomized to preventable (prevented, definitely preventable, or probably preventable) and nonable (probably not preventnonable or definitely not prevent-able) for analysis. Disagreements in ratings were re-solved through discussion. Prediscussion inter-rater reliability was calculated by using the statistic. The was 0.89 for reviewers’ judgments regarding event clas-sification, and thewas 1.00 for ratings of the prevent-ability of adverse events.
Analyses
Mean ranks of hours of work and sleep before and after implementation of the ACGME duty hour standards were compared by using the nonparametric Wilcoxon rank sum test, because values were nonnormally distrib-uted. Rates of medication errors per 100 orders were compared by using Fisher’s exact tests. The proportions of subjects experiencing MVCs, needle stick injuries,
TABLE 1 Definitions and Examples of Medication Errors Identified in the Study
Error Type Definition Example
Medication error with little potential for harm Medication error (ie, an error in medication ordering, transcription, administration, or monitoring) with little potential to cause harm
Order written for Tylenol with no route provided
Intercepted potential adverse drug event Medication error with significant potential to cause harm but does not because it is intercepted before reaching the patient
Order for 30 mg of prednisone for wrong patient written by resident but intercepted by nurse
Nonintercepted potential adverse drug event Medication error with significant potential to cause harm but does not because the patient has sufficient physiologic reserves to buffer the error without apparent injury
Order written and drug administered for 10-fold overdose of enalapril, which was not discovered for several hours but caused no apparent harm
depression, burnout, and educational/job dissatisfaction also were compared by using Fisher’s exact tests.
During the periods of data collection, comprehensive data on medication errors were captured on study units through active surveillance; missing survey responses and log entries were excluded from analysis. Our pri-mary analysis of medication errors included errors at all stages in the medication delivery process, but a second-ary analysis of resident ordering errors also was con-ducted. All reportedPvalues are 2-sided, withPvalues of ⬍.05 being considered statistically significant. SPSS 14.0 (SPSS, Chicago, IL) and SAS 9.1 (SAS Institute, Cary, NC) were used for statistical analyses.
Power
We determined a priori that we would have ⬎99% power to detect a 10% change in work hours or sleep, with a 2-sided ␣error of .05. We had⬎80% power to detect a 25% change in rates of medication errors. We had ⬃80% power to detect a 50% change in the pro-portions of residents reporting occupational injuries, near-miss MVCs, and symptoms of depression. Analysis of actual MVC rates was considered exploratory, because we had only 40% power to detect a 50% reduction in MVCs.
RESULTS
Study Group
Of the 246 potential resident subjects to whom the study was advertised in 2003, 144 (58.5%) volunteered to participate, providing written informed consent and baseline demographic data; of the 252 to whom the study was advertised in 2004, 124 (49.2%) agreed to participate. Of those who agreed to participate, 220 (82.1%) returned their daily logs of work hours and sleep, providing a total of 6007 (91.0%) of a possible 6604 daily reports of their work and sleep; 209 (95.0%) of 220 subjects who returned their logs provided data regarding⬎50% of their eligible days of study. A total of 213 participants returned all remaining study materials, including detailed reports of any near-miss or actual MVCs, reports of occupational exposures, the Harvard Department of Psychiatry/National Depression Screen-ing Day Scale, the Maslach Burnout Inventory, and rat-ings of educational and job experiences. There were no statistically significant differences in participants’ demo-graphic characteristics before versus after implementa-tion of the ACGME duty hour standards (Table 2).
Hours of Work and Sleep
Residents’ mean daily sleep did not change after imple-mentation of the ACGME duty hour standards, and nei-ther did total work hours (Table 3). The mean duration of extended work shifts decreased 2.7%, from 29.3⫾3.2 hours to 28.5⫾2.4 hours (P⬍.001). A total of 80.8% (95% confidence interval [CI]: 73.0%– 86.7%) of resi-dents reported working shifts exceeding 30 consecutive hours before implementation of the standards, com-pared with 55.8% (95% CI: 45.2%– 65.9%) after imple-mentation (P⬍.001).
Medication Error and Adverse Event Surveillance
During the 2 study periods, data extractors reviewed 16 158 medication orders written over the course of 2324 patient-days. Total medication error rates did not change significantly after implementation of the duty hour standards (before implementation: 1.29 errors per 100 orders; 95% CI: 1.06-1.56 errors per 100 orders; after implementation: 1.50 errors per 100 orders; 95% CI: 1.26-1.79 errors per 100 orders; P⫽.25), and total rates of adverse events did not change (before imple-mentation: 0.16 adverse events per 100 orders; 95% CI: 0.10-0.27 adverse events per 100 orders; after imple-mentation: 0.17 adverse events per 100 orders; 95% CI: 0.10-0.29 adverse events per 100 orders;P⬎.99). There was, however, a borderline significant increase in the occurrence of resident physician ordering errors (ie, those errors most directly attributable to resident physi-cians), from 1.06 errors per 100 patient-days (95% CI: 0.86-1.31 errors per 100 patient-days) to 1.38 errors per 100 patient-days (95% CI: 1.15-1.66 errors per 100 pa-tient-days;P⫽.08). Data on changes in subcategories of medication errors (preventable adverse events, inter-cepted and noninterinter-cepted potential adverse events, and medication errors with little potential for harm) are pre-sented in Table 4. Examples of medication errors de-tected are presented in Table 1.
Reported Safety and Performance
During the study, 18 respondents (8.5%; 95% CI: 5.4%– 13.0%) reported having been in an actual MVC, and 72 participants (33.8%; 95% CI: 27.8%– 40.4%) reported having had a near-miss MVC. A total of 46 respondents (21.6%; 95% CI: 16.6%–27.6%) reported having per-sonally experienced an occupational exposure to blood or another bodily fluid, and 7 (3.3%; 95% CI: 1.6%–
TABLE 2 Subject Demographic Data, Before and After Implementation of the ACGME Duty Hour Standards
Before Implementation
After Implementation
P
Enrolled participants,n 144 124
Female, % 70.7 68.3 .69
White, % 75.9 63.6 .60
Married, % 41.5 34.8 .08
In pediatric level-1 year, % 35.4 39.1 .51
Age, mean, y 30.2 29.1 .32
TABLE 3 Residents’ Reported Work Hours and Sleep, Before and After Implementation of the ACGME Duty Hour Standards
Duration, Mean⫾SD, h Change, %
P
Before Implementation
After Implementation
Daily work durationa 8.6⫾7.5 8.6⫾7.4 0 .94
Duration of extended work shifts
29.3⫾3.2 28.5⫾2.4 ⫺2.7 ⬍.001
Daily sleep duration 7.4⫾2.7 7.5⫾2.7 ⫹1.4 .49
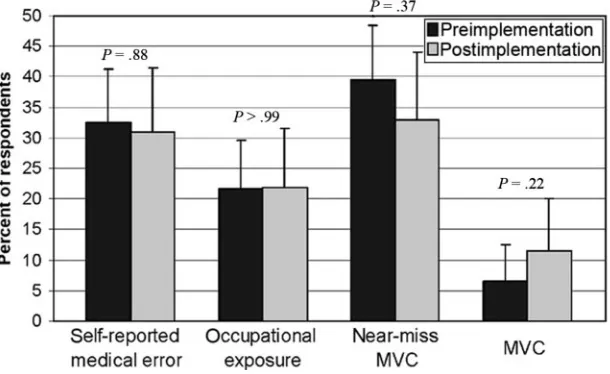
6.6%) reported having caused an exposure to another provider. Sixty-eight residents (31.9%; 95% CI: 26.0%– 38.4%) acknowledged having made a medical error. Rates of near-miss MVCs, actual MVCs, occupational exposures, and self-reported medical errors did not change significantly after implementation of the stan-dards (Fig 1).
Mental Health
A total of 41 residents (19.6%; 95% CI: 14.8%–25.5%) screened positive for depression, and 141 (67.8%; 95% CI: 61.1%–73.8%) met criteria for burnout. Rates of depression did not change significantly after mentation of the ACGME standards (before imple-mentation: 19.5%; 95% CI: 13.5%–27.4%; after im-plementation: 19.8%; 95% CI: 12.7%–29.4%; P ⬎ .99), but rates of burnout decreased from 75.4% (95% CI: 67.0%– 82.2%) to 57.0% (95% CI: 46.4%– 66.9%; P⫽ .007).
Educational and Job Dissatisfaction
Before implementation of the standards, 22.4% (95% CI: 16.0%–30.5%) of residents characterized their over-all educational experience as poor or fair, compared with
23.5% (95% CI: 15.8%–33.6%) after implementation (P ⫽ .87). A total of 7.9% (95% CI: 4.4%–14.0%) of residents before implementation, compared with 12.9% (95% CI: 7.4%–21.7%) after implementation, reported the quality of their residency program to be poor or fair (P⫽.25); 23.0% (95% CI: 16.5%–31.1%) of residents reported being dissatisfied with their job before imple-mentation of the standards, and 14.1% (95% CI: 8.3%– 23.1%) reported dissatisfaction after implementation (P⫽.12). When asked whether they would take this job again, 62.1% (95% CI: 53.2%–71.2%) before imple-mentation, compared with 62.4% (95% CI: 51.7%– 71.9%) after implementation, would have some second thoughts or would definitely decide not to take it (P⬎ .99); 78.4% (95% CI: 70.4%– 84.7%) and 73.8% (95% CI: 63.5%– 82.0%) of residents, respectively, would have doubts about recommending the job to a friend interested in becoming a resident or would advise against it (P⫽.51).
DISCUSSION
In a tricenter, prospective, cohort study, we found that total work hours, sleep hours, and rates of medication errors, resident depression, occupational exposures, MVCs,
TABLE 4 Medication Error Rates, Before and After Implementation of the ACGME Duty Hour Standards
Before Implementation After Implementation Pa
No. Error Rate, Estimate (95% CI), Cases per
100 Orders
No. Error Rate, Estimate (95% CI), Cases per
100 Orders
No. of orders 8003 8115
No. of errors
Total 103 1.29 (1.06–1.56) 122 1.50 (1.26–1.79) .25
Preventable adverse events 5 0.06 (0.03–0.15) 5 0.06 (0.03–0.14) ⬎.99 Potential adverse events 60 0.75 (0.58–0.96) 56 0.69 (0.53–0.90) .71 Intercepted potential adverse events 38 0.47 (0.35–0.65) 32 0.39 (0.28–0.56) .47 Nonintercepted potential adverse events 22 0.27 (0.18–0.42) 24 0.30 (0.20–0.44) .88 Medication errors with little potential for harm 38 0.47 (0.35–0.65) 61 0.75 (0.59–0.96) .03 No. of resident physician ordering errors 85 1.06 (0.86–1.31) 112 1.38 (1.15–1.66) .08
aFisher’s exact test.
FIGURE 1
and adverse educational experiences were unchanged af-ter implementation of the ACGME duty hour standards. There was a significant decrease in resident burnout, as well as a 2.7% reduction in the mean duration of pedi-atric residents’ extended shifts, but the reductions in the duration of extended shifts and burnout were not ac-companied by improvements in any of the measured outcomes regarding patient or resident safety.
Europe, New Zealand, and the United States have addressed the hazards of long work hours in widely disparate ways. In New Zealand, junior doctors have been limited by contract to 16 consecutive hours of work and 72 hours/week since 1985.28 Europe has limited physicians to 13 consecutive hours and 48 to 56 hours/ week by law.14The United States, in contrast, has relied on professional self-regulation both to set work hour limits and to enforce them; 30 consecutive hours and 80 to 88 hours/week are allowed.5Limited objective data have been collected to assess the effectiveness of any of these regulatory efforts, and considerable controversy about the effectiveness of each has remained.13,28,29 High-quality data on the effectiveness of resident work hour policies are important for both developed and develop-ing nations as they evaluate current work hour practices and seek to improve care.30
Our study is the first of which we are aware that has evaluated directly the effect of governmental or profes-sional work hour regulations across medical centers by using (1) state-of-the-art methods for the collection of validated data on sleep and work hours, (2) rigorous surveillance for medication errors, (3) assessment of res-ident safety, and (4) measurement of resres-ident educa-tional and work experiences. The fact that implementation of the ACGME standards did not lead to improvements in either total work hours or error rates in the centers studied is of considerable concern, given the established conse-quences of long work hours for the safety of both pro-viders and patients. Physicians-in-training working 24-hour shifts experience performance decrements similar to those induced by blood alcohol levels of 0.05% to 0.10%,31,32with a doubling of intrusive attentional fail-ures at night.18 This impairment leads to 1.5- to 2-SD deterioration in their performance on a range of clinical and nonclinical tasks.33Physicians-in-training have been found to suffer 61% more percutaneous injuries4 and twice as many MVCs after 24-hour shifts3and to make many more serious medical errors, including those that harm their patients.1,2
We found previously that a schedule that was built on sleep and circadian principles and that limited interns’ scheduled work to 16 consecutive hours improved in-terns’ alertness and patient safety substantially.2,18 Sim-ilarly, in a single medical center that eliminated resi-dents’ overnight call, Horwitz et al34 found that ICU transfers decreased and pharmacist interventions to pre-vent medication errors decreased by 1.92 interpre-ventions per 100 patient-days. Although these data are encour-aging, elimination of all overnight calls for residents is an approach that very few residency programs in the United States have taken,15 and one that goes well beyond the requirements of the ACGME standards. In this study, we
found that, in 3 centers where residents continue to be scheduled for ACGME-endorsed 24- to 30-hour shifts, implementation of the standards did not lead to im-provements in safety or resident experiences.
Our study follows a host of published studies regard-ing trainees’ and program directors’ subjective impres-sions of the ACGME standards. Some studies concluded that safety and resident experiences generally remained stable or improved after implementation of the stan-dards,6,10 whereas others concluded that the standards affected safety or resident education adversely.7–9,11,12 More recently, Shetty and Bhattacharya35 conducted a large administrative database evaluation, in which they found a 0.25% reduction in the mortality rate among medical patients but no change among surgical patients after implementation of the duty hour standards. Al-though that study added important objective data re-garding the duty hour standards, it could not directly measure residents’ actual work hours or determine whether individual patients were cared for by resident physicians. In addition, it could not differentiate effects attributable to implementation of work hour limits from other global effects that might have been occurring con-currently in teaching hospitals, especially implementa-tion of other ongoing naimplementa-tional efforts to improve safety. Our study, which directly assessed work hours and eval-uated outcomes closely linked to resident performance, found no improvements in resident or patient safety.
Inherent limitations in the nature of the ACGME standards may explain the lack of improvement we ob-served. Despite a number of studies conducted in the past several years demonstrating the hazards of 24-hour work shifts,1–4,32,33 the ACGME continues to endorse shifts of up to 30 consecutive hours. Seeking to comply with the ACGME’s 30-hour shift limit and 80-hour weekly work limit impelled considerable rearrangement in the structure of residents’ schedules in the 3 programs studied (as described above) but did not lead to elimina-tion of 24-hour shifts. The mean duraelimina-tion of extended shifts decreased only 3% to 28.5 hours, and even this modest improvement was counterbalanced by slight in-creases in the duration of other work days, such that total work hours remained unchanged.
Noncompliance with laws or regulations that limit work hours also may attenuate their effects. We found that⬎80% of interns were working shifts exceeding the ACGME’s 30-hour limit at baseline; after implementa-tion of the standards, nearly 60% continued to work shifts of ⬎30 hours. These data are comparable to na-tional compliance data in the United States. In a previ-ous nationwide cohort study, we found that 67.4% of interns were noncompliant with the ACGME’s 30-hour shift limit in the year after their implementation.15Even with perfect compliance, however, the continued pres-ence of 24- to 30-hour shifts in most programs would pose an ongoing safety risk.1–4,32,33
pediatric residents or residents in other specialties. The demographic distribution of the residents participating in the study was typical of the overall distribution of the 3 residency programs, as well as the nationwide demo-graphic distribution of pediatric residents,36,37 but it is possible that our subjects differed from the broader pop-ulation of residents in unmeasured ways. The work hours of the pediatric trainees studied here are fairly typical of the work hours of pediatric trainees and train-ees in other specialties in the United States,16however, and we demonstrated previously that work hour changes after implementation of the ACGME duty hour standards were fairly small across specialties, including pediatrics.15Because noncompliance with the duty hour standards occurred with similar frequencies in this co-hort and in the national coco-hort of residents,15it is prob-able that changes in safety and residency experiences attributable to the ACGME standards, the focus of this study, are similarly small in other residency programs where limited changes in work hours have occurred. In the minority of programs where mosubstantive re-ductions in work hours occurred after implementation of the ACGME standards, there may be measurable im-provements in safety, as found by Horwitz et al.34 Ob-jectively differentiating effective from ineffective work hour reforms by using rigorous study designs is of critical importance in making evidence-based scheduling im-provements and should be a focus of future research efforts throughout the world as new work hour limits and schedules are introduced.
Second, the study was underpowered to detect dif-ferences in certain uncommon but important safety outcomes, such as adverse drug events and MVCs. Although we collected data from ⬎200 residents and reviewed ⬎15 000 medication orders, larger studies would be needed to detect changes in those inci-dences. Because we found no changes in sleep depri-vation or work hours, however, or in rates of more-sensitive key indicator outcomes (medication errors and near-miss MVCs), it is unlikely that even a much larger study would have identified changes in resident or patient harm associated with implementation of the standards.
Third, because it was not possible to blind either subjects or data extractors to the implementation of the ACGME duty hour standards, biases in data reporting might have occurred. To minimize this effect with re-spect to the measurement of medication errors, all final classification of events was conducted after the conclu-sion of the study, with investigators blinded to when the error was detected. In addition, we used a well-validated instrument to collect data on work and sleep hours and validated instruments to measure depression and burn-out. Despite these precautions, we cannot exclude the possibility of reporting biases, although the consistent lack of major differences in findings obtained before versus after implementation in all of our major data sources (medication error reports from data extractors, daily resident work logs, and resident reports of injuries and errors) suggest that reporting bias is unlikely to be responsible for the lack of measured effects.
Fourth, we cannot determine definitively the reasons for the lack of change in medication error rates. Previous work showed profoundly increased rates of serious med-ical errors among sleep-deprived trainees, compared with rested trainees (36% increase overall; 136.0 and 100.1 errors per 1000 patient-days, respectively; P ⬍ .001), and a fivefold increase in serious diagnostic errors (18.6 and 3.3 errors per 1000 patient-days, respectively; P⬍.001).2Therefore, we would expect that a policy that reduced resident fatigue effectively would lead to readily measured decreases in medication errors, as long as handoffs of care are managed appropriately.38,39Instead, we found no statistically significant change in overall error rates, a statistically significant increase in errors with little potential for harm, and an increase in physi-cian ordering errors of borderline significance, which suggests that systemic disruptions and increased hand-offs (unaccompanied by any improvement in work hours or sleep) might have led to marginal worsening of system performance. Our study was not designed to evaluate the quality of teamwork, sign-out processes, team structure, or resident workload objectively, how-ever, and other unmeasured factors might have influ-enced the rates of medication errors detected before and after intervention. Similarly, we did not seek to correlate errors with the timing of work and sleep experienced by residents before error occurrence; therefore, we have not attempted to quantify the relative contributions of circadian factors, acute sleep deprivation, chronic sleep deprivation, sleep inertia, and other sleep and schedul-ing variables to error occurrence. Because this was a between-groups comparison, rather than a within-sub-jects study, we could not evaluate the manner in which individual-level error rates might have changed after implementation of the ACGME standards. Each of these topics should be the subject of future inquiries.
Fifth, although data on work hours and medication errors were collected on a daily basis, other data, such as self-reports of medical errors and MVCs, were provided by residents after the occurrence of those events, and recall bias might have affected the reporting of those outcomes. Lastly, our study measured the effects of the ACGME duty hour standards in their first year only (2003–2004). If work hours decreased substantially after this initial year, it is possible that such reductions were accompanied by measurable improvements in safety. In the 3 programs studied, however, there has not been any major restructuring of resident work hours since 2003. To date, very few programs in the United States have taken major steps to reduce fatigue-related injury (such as the elimination of 24-hour shifts) that go sig-nificantly beyond the work hour limits required by the ACGME.
work hours or on patient and provider safety. The grow-ing literature demonstratgrow-ing the risks of residents’ tradi-tional 24-hour shifts1,2,4,18,32,33suggests that the incidence of fatigue-related errors in academic medical centers will continue to be high as long as these shifts remain com-mon. Unfortunately, 24- to 30-hour shifts continue to be endorsed by professional regulatory organizations in the United States, and only a few progressive hospital lead-ers and residency programs, such as the surgical resi-dency program at Brigham and Women’s Hospital40and the medical residency program at Yale-New Haven Hos-pital,34have gone significantly beyond what is required by the ACGME and eliminated 24-hour shifts in some settings. Without more-widespread actions by policy-makers, professional organizations, hospital leaders, and program directors to implement such evidence-based work hour limits, the ACGME’s laudable goal of reduc-ing “the negative effects of sleep loss on resident educa-tion and on the safety and well-being of patients and residents”41is likely to remain out of reach.
ACKNOWLEDGMENTS
This work was supported by the US Agency for Health-care Research and Quality (grant K08 HS13333), Brigham and Women’s Hospital, Lucile Packard Chil-dren’s Hospital Department of Pediatrics, ChilChil-dren’s Na-tional Medical Center Department of Pediatrics, and Children’s Hospital Boston Department of Medicine. The Agency for Healthcare Research and Quality support afforded data confidentiality protection through federal statute (Public Health Service Act 42 USC). The funding agencies had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Our thanks go to the members of the Harvard Work Hours, Health, and Safety Group and the Center of Ex-cellence in Patient Safety at Brigham and Women’s Hos-pital, especially Charles A. Czeisler, PhD, MD, Steven W. Lockley, PhD, Najib T. Ayas, MD, MPH, David W. Bates, MD, MSc, and Jeffrey M. Rothschild, MD, MPH, for their contributions to the development of data collection in-struments used in this study. Our thanks also go to Frederick Lovejoy, MD, Gary Fleisher, MD, Joseph Loscalzo, MD, PhD, Gary L. Gottlieb, MD, MBA, and Anthony D. Whittemore, MD, for their leadership in creating an environment in which the study of quality of care and patient safety is a high priority. Special thanks go to our data extractors and research assistants, espe-cially Christopher O’Rourke-Friel, RN, Sridhar Goli, MBBS, Doris Hanna, RN, Louise Hitchko, RN, Suzanne Moser, RN, Jennifer Quinby, Bernadette Rkiouak, RN, and Pirouz Shamszad, who were compensated for their work by the Agency for Healthcare Research and Quality and departmental funds designated for this project. Thanks go to the Harvard Department of Psychiatry and Screening for Mental Health for permission to use the Harvard Department of Psychiatry/National Depression Screening Day Scale and to CPP, Inc, for permission to use the Maslach Burnout Inventory.
REFERENCES
1. Barger LK, Ayas NT, Cade BE, et al. Impact of extended-duration shifts on medical errors, adverse events, and atten-tional failures.PLoS Med.2006;3(12):e497
2. Landrigan CP, Rothschild JM, Cronin JW, et al. Effect of reducing interns’ work hours on serious medical errors in intensive care units.N Engl J Med.2004;351(18):1838 –1848
3. Barger LK, Cade BE, Ayas NT, et al. Extended work shifts and the risk of motor vehicle crashes among interns.N Engl J Med. 2005;352(2):125–134
4. Ayas NT, Barger LK, Cade BE, et al. Extended work duration and the risk of self-reported percutaneous injuries in interns. JAMA.2006;296(9):1055–1062
5. Accrediation Council for Graduate Medical Education. Com-mon program requirements: duty hour requirements, 2003. Available at: www.acgme.org/acWebsite/dutyHours/ dh㛭dutyHoursCommonPR.pdf. Accessed July 13, 2007 6. Jagsi R, Shapiro J, Weissman JS, Dorer DJ, Weinstein DF. The
educational impact of ACGME limits on resident and fellow duty hours: a pre-post survey study. Acad Med.2006;81(12): 1059 –1068
7. Brunworth JD, Sindwani R. Impact of duty hour restrictions on otolaryngology training: divergent resident and faculty per-spectives.Laryngoscope.2006;116(7):1127–1130
8. Karamanoukian RL, Ku JK, DeLaRosa J, Karamanoukian HL, Evans GR. The effects of restricted work hours on clinical training.Am Surg.2006;72(1):19 –21
9. Mathis BR, Diers T, Hornung R, Ho M, Rouan GW. Implement-ing duty-hour restrictions without diminishImplement-ing patient care or education: can it be done?Acad Med.2006;81(1):68 –75 10. Lieberman JD, Olenwine JA, Finley W, Nicholas GG.
Resi-dency reform: anticipated effects of ACGME guidelines on general surgery and internal medicine residency programs. Curr Surg.2005;62(2):231–236
11. Myers JS, Bellini LM, Morris JB, et al. Internal medicine and general surgery residents’ attitudes about the ACGME duty hours regulations: a multicenter study.Acad Med.2006;81(12): 1052–1058
12. Whang EE, Perez A, Ito H, Mello MM, Ashley SW, Zinner MJ. Work hours reform: perceptions and desires of contemporary surgical residents.J Am Coll Surg.2003;197(4):624 – 630 13. Okie S. An elusive balance: residents’ work hours and the
continuity of care.N Engl J Med.2007;356(26):2665–2667 14. British Medical Association.Time’s Up: A Guide on the EWTD for
Junior Doctors. London, England: British Medical Association; 2005. Available at: www.bma.org.uk/ap.nsf/AttachmentsByTitle/ PDFtimesup2/$FILE/TimesUp2.pdf. Accessed July 13, 2007 15. Landrigan CP, Barger LK, Cade BE, Ayas NT, Czeisler CA.
Interns’ compliance with Accreditation Council for Graduate Medical Education work-hour limits. JAMA. 2006;296(9): 1063–1070
16. Baldwin DC Jr, Daugherty SR, Tsai R, Scotti MJ Jr. A national survey of residents’ self-reported work hours: thinking beyond specialty.Acad Med.2003;78(11):1154 –1163
17. Kaushal R, Bates DW, Landrigan C, et al. Medication errors and adverse drug events in pediatric inpatients.JAMA.2001; 285(16):2114 –2120
18. Lockley SW, Cronin JW, Evans EE, et al. Effect of reducing interns’ weekly work hours on sleep and attentional failures. N Engl J Med.2004;351(18):1829 –1837
19. Baer L, Jacobs DG, Meszler-Reizes J, et al. Development of a brief screening instrument: the HANDS.Psychother Psychosom. 2000;69(1):35– 41
20. Maslach C, Jackson SE, Leiter MP.Maslach Burnout Inventory Manual. 3rd ed. Palo Alto, CA: Consulting Psychologists Press; 1996
self-reported patient care in an internal medicine residency program.Ann Intern Med.2002;136(5):358 –367
22. West CP, Huschka MM, Novotny PJ, et al. Association of perceived medical errors with resident distress and empathy: a prospective longitudinal study.JAMA.2006;296(9):1071–1078 23. Bates DW, Leape LL, Cullen DJ, et al. Effect of computerized physician order entry and a team intervention on prevention of serious medication errors.JAMA.1998;280(15):1311–1316 24. Cullen DJ, Bates DW, Small SD, Cooper JB, Nemeskal AR, Leape LL. The incident reporting system does not detect ad-verse drug events: a problem for quality improvement.Jt Comm J Qual Improv.1995;21(10):541–548
25. O’Neil AC, Petersen LA, Cook EF, Bates DW, Lee TH, Brennan TA. Physician reporting compared with medical-record review to identify adverse medical events. Ann Intern Med. 1993; 119(5):370 –376
26. Bates DW, Cullen D, Laird N, et al. Incidence of adverse drug events and potential adverse drug events: implications for prevention.JAMA.1995;274(1):29 –34
27. McBride SC, Chiang VW, Goldmann DA, Landrigan CP. Pre-ventable adverse events in infants hospitalized with bronchi-olitis.Pediatrics.2005;116(3):603– 608
28. Gander PH, Purnell HM, Garden A, Woodward A. Work pat-terns and fatigue-related risk among junior doctors. Occup Environ Med.2007;64(11):733–738
29. MacDonald R. How protective is the working time directive? BMJ.2004;329(7461):301–302
30. Ferna´ndez Taylor KR. Excessive work hours of physicians in training in El Salvador: putting patients at risk. PLoS Med. 2007;4(7):e205
31. Dawson D, Reid K. Fatigue, alcohol and performance impair-ment.Nature.1997;388(6639):235
32. Arnedt JT, Owens J, Crouch M, Stahl J, Carskadon MA. Neu-robehavioral performance of residents after heavy night call vs after alcohol ingestion.JAMA.2005;294(9):1025–1033
33. Philibert I. Sleep loss and performance in residents and nonphysicians: a meta-analytic examination. Sleep. 2005; 28(11):1392–1402
34. Horwitz LI, Kosiborod M, Lin Z, Krumholz HM. Changes in outcomes for internal medicine inpatients after work-hour regulations.Ann Intern Med.2007;147(2):97–103
35. Shetty KD, Bhattacharya J. Changes in hospital mortality as-sociated with residency work-hour regulations.Ann Intern Med. 2007;147(2):73– 80
36. Sectish TC, Zalneraitis EL, Carraccio C, Behrman RE. The state of pediatrics residency training: a period of transformation of graduate medical education.Pediatrics.2004;114(3):832– 841 37. Cull WL, Yudkowsky BK, Shipman SA, Pan RJ. Pediatric
train-ing and job market trends: results from the American Academy of Pediatrics third-year resident survey, 1997–2002.Pediatrics. 2003;112(4):787–792
38. Petersen LA, Brennan TA, O’Neil AC, Cook EF, Lee TH. Does housestaff discontinuity of care increase the risk for prevent-able adverse events? Ann Intern Med. 1994;121(11):866 – 872
39. Petersen LA, Orav EJ, Teich JM, O’Neil AC. Using a comput-erized sign-out program to improve continuity of inpatient care and prevent adverse events.Jt Comm J Qual Improv.1998; 24(2):77– 87
40. Knox R. Work rules fail to end danger from tired doctors.Morning Edition. National Public Radio. December 12, 2006. Available at: www.npr.org/templates/story/story.php?storyId⫽6612904& sc⫽emaf. Accessed November 5, 2007
41. Accreditation Council for Graduate Medical Education. The ACGME’s approach to limit resident duty hours 2005– 06: a summary of achievements for the third year under the com-mon requirements, 2007. Available at: www.acgme.org/ acWebsite/dutyHours/dh㛭achieveSum05-06.pdf. Accessed July 13, 2007
YELLOW BUSES PUT SCHOOLS IN THE RED
“The pain at the pump is hitting those too young to drive. In Nebraska, Bellevue School District is budgeting $600,000 to cover fuel costs for school buses next school year, compared with $250,000 a year ago. Kentucky’s Bowling Green Independent Schools is budgeting 36% more for fuel com-pared with last year. The Durham, NC, public schools budgeted $3.3 million for fuel, more than twice what was budgeted a year ago. ‘I’ve never seen anything escalate this quick,’ says Hank Hurd, the Durham district’s chief operating officer. ‘There’s no way for a school district to absorb those kinds of increases.’ Some 475 000 school buses transport 25 million children—more than half of the country’s schoolchildren— each day, and cover 4.3 billion miles a year, says the American School Bus Council.”
Chaker AM.Wall Street Journal. June 19, 2008
DOI: 10.1542/peds.2007-2306
2008;122;250
Pediatrics
Wiedermann and Theodore C. Sectish
K. Barger, Melanie Eisner, Sarah Edwards, Vincent W. Chiang, Bernhard L.
Christopher P. Landrigan, Amy M. Fahrenkopf, Daniel Lewin, Paul J. Sharek, Laura
Limits on Sleep, Work Hours, and Safety
Effects of the Accreditation Council for Graduate Medical Education Duty Hour
Services
Updated Information &
http://pediatrics.aappublications.org/content/122/2/250
including high resolution figures, can be found at:
References
http://pediatrics.aappublications.org/content/122/2/250#BIBL
This article cites 36 articles, 5 of which you can access for free at:
Subspecialty Collections
http://www.aappublications.org/cgi/collection/safety_sub
Safety
_management_sub
http://www.aappublications.org/cgi/collection/administration:practice
Administration/Practice Management following collection(s):
This article, along with others on similar topics, appears in the
Permissions & Licensing
http://www.aappublications.org/site/misc/Permissions.xhtml
in its entirety can be found online at:
Information about reproducing this article in parts (figures, tables) or
Reprints
http://www.aappublications.org/site/misc/reprints.xhtml
DOI: 10.1542/peds.2007-2306
2008;122;250
Pediatrics
Wiedermann and Theodore C. Sectish
K. Barger, Melanie Eisner, Sarah Edwards, Vincent W. Chiang, Bernhard L.
Christopher P. Landrigan, Amy M. Fahrenkopf, Daniel Lewin, Paul J. Sharek, Laura
Limits on Sleep, Work Hours, and Safety
Effects of the Accreditation Council for Graduate Medical Education Duty Hour
http://pediatrics.aappublications.org/content/122/2/250
located on the World Wide Web at:
The online version of this article, along with updated information and services, is
by the American Academy of Pediatrics. All rights reserved. Print ISSN: 1073-0397.