http://www.sciencepublishinggroup.com/j/ijacm doi: 10.11648/j.ijacm.20190702.12
ISSN: 2376-7766 (Print); ISSN: 2376-7774(Online)
A Clinical Study of Comparison of Dexmedetomidine and
Ketamine Versus Propofol and Ketamine for Procedural
Sedation in Children Undergoing Device Closure
Sowmya Sree, Somita Christopher
*, Thota Venkata Sanjeev Gopal
Department of Anesthesiology, Care Hospitals, Hyderabad, India
Email address:
*
Corresponding author
To cite this article:
Sowmya Sree, Somita Christopher, Thota Venkata Sanjeev Gopal. A Clinical Study of Comparison of Dexmedetomidine and Ketamine Versus Propofol and Ketamine for Procedural Sedation in Children Undergoing Device Closure. International Journal of Anesthesia and Clinical Medicine. Vol. 7, No. 2, 2019, pp. 37-42. doi: 10.11648/j.ijacm.20190702.12
Received: August 13, 2019; Accepted: September 4, 2019; Published: September 23, 2019
Abstract:
This prospective, randomized trial was done to compare the effects of Dexmedetomidine-Ketamine and Propofol-Ketamine combinations on hemodynamics, sedation level, and the recovery period in paediatric patients undergoing device closure in cardiac catheterization laboratory. Sixty children undergoing device closure were divided into two groups of thirty each. The Dexmedetomidine-Ketamine group (group I, n=31) received an infusion of 1microgram/kg of Inj Dexmedetomidine over 10 minutes and 1 mg/kg of Inj Ketamine IV as a bolus for induction. The patients then received an infusion of 0.5 microgram/kg/hour of Inj Dexmedetomidine. The Propofol - Ketamine group (group II, n=29) received 1 mg/kg of Inj Propofol and 1 mg/kg of Inj Ketamine as a bolus for induction. These patients then received an infusion of100 micorgram/kg/ min of Inj Propofol. Additional doses of Inj Ketamine, 0.5 mg/kg, were administered when a patient showed discomfort in both groups. Both groups had similar additional Ketamine consumption to maintain deep sedation. The recovery time was longer in group 1 than in group 2 (13 vs 5 minutes, respectively; p <0.01). So it was concluded that both Dexmedetomidine-Ketamine and Propofol-Ketamine combinations are safe and acceptable for sedation without any hemodynamic or respiratory effects for device closure in the cardiac catheterization laboratory in children.Keywords:
Dexmedetomidine, Ketamine, Propofol, Ventricular Septal Defect, Atrial Septal Defect1. Introduction
Congenital heart disease (CHD) is a structural and functional heart disease, which is present at birth. The prevalence of CHD in India is around 2.5-5.2/1000 live births, and common lesions are ventricular septal defect (VSD), patent ductus arteriosus (PDA), transposition of great arteries (TGA), atrial septal defect (ASD) and pulmonary atresia.[1] Percutaneous closure and surgical repair are the effective interventions in the management of CHD. Transcatheter device closure is increasingly used in selected patients in the current era, in a effort to postpone or replace surgical intervention. [2]
Cardiac catheterization procedures require sedation to keep the child immobile, facilitating the procedure. Unlike adults, children need moderate to severe sedation to maintain immobility. The requirement for sedation has increased along
with increase in number and complexity of paediatric cardiac interventions. Deep sedation is preferred by interventional cardiologists as compared to general anaesthesia as it provides better cardiovascular stability, allowing spontaneous ventilation via a natural airway with quick recovery. However there is always a difficulty in deep sedation to balance the perfect level of sedation, especially during the procedure. [3]. It is also shown that conducting these procedures under deep sedation is safe with minimal anaesthetic complications. [4]
2. Material and Methods
2.1. Study Population
All paediatric patients of age group 1 month to 12 years who underwent elective cardiac catheterization for device closure procedures (Atrial septal defect, Ventricular septal defect, and Patent ductus arteriosus) in catheterization suite were included in the study.
2.2. Study Design: A Randomized Clinical Trial
2.2.1. Method of Randomization: Simple Randomization
All the included subjects were randomized by computer generated random numbers using web based software. Sealed opaque envelopes were used to conceal the allocation of the subject. The envelope was opened after the entry of subject into the trial in the catheterization suite. They were randomized to receive Dexmedetomidine-Ketamine or Propofol- Ketamine combination for deep sedation during the procedure.
2.2.2. Sample Size Calculation
A total number of approximately 60 patients were determined through power analysis using a sample size calculation formula. The effect size was calculated based upon a previous study done by Joshi et al [5]which compared anaesthetic drug combinations on paediatric sedation. The outcome variable taken for calculation was mean recovery time, which is 40.88 minutes in group 1, and 22.28 minutes in group II.
The formula for the sample size for comparison of 2 means (2-sided) is as follows:
n = 2[Zα+Z1-β]2×σ2/∆2 (1)
n = the sample size required in each group,
∆ = size of difference of clinical importance, which is 18.6, σ = standard deviation of the outcome variable, which is 8.19, Zα is 1.96, Z1-β is 0.8416 (Constants for a power of 80%
and 5% level of significance).
3. Methodology
According to hospital policy, all children were kept fasting for at least 6 hours before procedure. All the patients underwent pre-anesthetic assessment a day before the procedure after admission into the hospital ward. The patients were premedicated with Inj Midazolam (50 µg/kg) intravenously (IV) 10 min before taking the child inside the catheterization laboratory where appropriate measures to prevent hypothermia were undertaken.
Standard monitors including electrocardiogram and pulse-oximeter were attached after entry into the suite.[6] The sealed envelope was opened after entry into the lab and the child was randomized to receive either Dexmedetomidine-Ketamine or Propofol-Dexmedetomidine-Ketamine for sedation during the procedure. Group Dexmedetomidine-Ketamine (DK) received: Inj Dexmedetomidine IV infusion 1 µg/kg over 10 min along with Inj Ketamine 1 mg/kg IV bolus for induction and then maintenance by IV infusion of 0.5 µg/kg/h of Inj Dexmedetomidine. Group Propofol –Ketamine (PK)
received: Inj Propofol 1mg/kg IV bolus and Inj Ketamine 1 mg/kg IV for induction and then maintenance by IV infusion of 100 µg/kg/min of Inj Propofol. We administered additional boluses of Inj Ketamine 0.5 mg/kg IV bolus when any child showed discomfort (cried or moved) in either of the groups.
Heart rate (HR), blood pressure (BP), peripheral oxygen saturation (SPO2), end tidal CO2 (EtCO2), respiratory rate
(RR), and sedation scores were recorded at baseline and every 5 min during the procedure. Sedation level was assessed using Ramsay sedation scale [7] along with monitoring of vital parameters throughout the procedure. All patients breathed room air and were supplemented with 3 to 4 L/min oxygen via nasal cannula in case of change of saturation. The anesthetic drug infusion was stopped when the groin bandage was applied and the total dose was calculated. The number of extra boluses and doses of Inj Ketamine given in both the groups was recorded. Adverse events occurring during the procedure and the total duration of the procedure were noted. If the deep sedation was not effective, general anesthesia (GA) was initiated with endotracheal intubation and that particular patient was excluded from the study.
Table 1. Ramsay Sedation Score.
Score Level of sedation achieved
1 Patient anxious, agitated or restless. 2 Patient co-operative oriented and tranquil. 3 Patient responds to commands.
4 Asleep but with brisk response to light glabeller tap or loud auditory stimulus.
5 Asleep, sluggish response to light glabeller tap or loud auditory stimulus.
6 Asleep, no response.
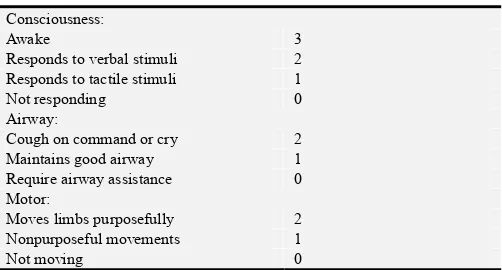
The child was shifted to post-anaesthesia recovery room after completion of the procedure for monitoring. Recovery score were assigned on admission to post anesthesia room where the routine vital signs were measured. Repeated scoring was performed every 10 minutes till the patient recovered up to score of 6 according to the Stewards Simplified Post anesthetic Recovery Score.[8] This score was determined by an independent blinded observer till discharge from the recovery room. After a minimum of 2 hours on the floor, a final interview was conducted and feeding was allowed without restriction. Any difficulty with feeding or voiding after the procedure was documented.
Table 2. Recovery Scoring System.
Consciousness:
Awake 3
Responds to verbal stimuli 2 Responds to tactile stimuli 1
Not responding 0
Airway:
Cough on command or cry 2
Maintains good airway 1
Require airway assistance 0
Motor:
Moves limbs purposefully 2
Nonpurposeful movements 1
4. Statistical Methods
The data was analyzed using statistical software package (IBM SPSS for windows, version 23.0; Chicago IL). The data was described using counts and proportions for categorical data like gender, frequency of bolus ketamine administration, and type of CHD. Mean and standard deviation (or median with interquartile range if non parametric distribution) was used as appropriate for continuous data. Normality of data was assessed using Q-Q plot and Kolmogorov Smirinov test.
Categorical data was analyzed using chi-square test or
Fishers exact test (if expected number is less than 5). The sedation score was analyzed with a Mann-Whitney U test. A
p value 0.05 was considered statistically significant.
5. Results
The baseline characteristics (age, gender, type of CHD, vital parameters, and laboratory data) were comparable among both the groups (Group I, DK and group II, PK). The subjects in both the groups did not differ from each other at baseline. The data comparison among them was shown in table 3.
Table 3. Comparison of baseline characteristics among both the study groups.
Group I (n =31) Group II (n =29) P
Age in months 36 (12, 72) 42 (19, 90) 0.24
Male gender, n (%) 12 (39) 17 (59) 0.12*
Weight in kg 16 (9, 25) 18 (12, 25) 0.32
Clinical disease
ASD, n (%) 10 (32) 16 (55) 0.18*
VSD, n (%) 10 (32) 5 (17)
PDA, n (%) 11 (36) 8 (28)
Pulse rate (per minute) 103 (96, 110) 97 (92, 104) 0.13
Respiratory rate (per minute) 30 (26, 32) 28 (25, 33) 0.98
Systolic blood pressure (mm Hg) 96 (90, 110) 98 (93, 110) 0.68
Diastolic blood pressure (mm Hg) 68 (62, 72) 68 (68, 72) 0.55
In Group I, the median induction dose of Inj Dexmedetomidine was 16µg and Inj Ketamine was 16mg while the median maintenance dose of Inj Dexmedetomidine was 10µg. The total median amount of Inj Dexmedetomidine received was 28µg ranging from 8.5µg to 96µg.
In Group II, the median induction dose of Inj Propofol was 18 mg and Inj Ketamine was 18mg while the median maintenance dose of Inj Propofol was 144 mg. The total median amount of Inj Propofol received was 156 mg ranging from 42mg to 460mg.
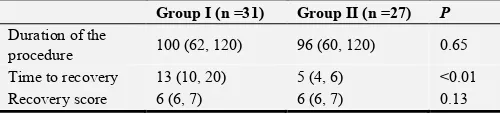
The duration of the procedure and recovery score did not differ among both the groups. The time to recovery differed significantly among both the groups (13 min, group I vs 5 min, group II; p <0.01). Two subjects of group II (PK) had
developed adverse events during the procedure. They developed respiratory depression manifested as bradypnoea and hypoxia, for which endotracheal intubation was done and the procedure was converted to GA. These adverse events occurred at 20 minutes in one patient and at 30 minutes in another patient after initiation of the sedation protocol.
The top up boluses of Inj Ketamine were used in both the groups to maintain sedation without altering the rate of maintenance drug infusions. Subjects in group I received median 2 boluses with median dose of 12 mg while subjects in group II received median 2 boluses with median dose of 11 mg. The requirement of Inj Ketamine did not differ statistically among the groups both in terms of boluses and dose of drug received as shown in figure 1
Figure 1. Bar graph comparing Ketamine consumption among the groups.
We found no statistical or clinical difference in depth of sedation between both the groups. No difference was found
after 10 minutes of induction as compared to PK group 85.26 vs 96.34. p=0.01) as shown in figure 2.
Figure 2. Line diagram comparing mean heart rates among the groups.
Respiratory rate (RR) was similar among both the groups (Figure 3) at all intervals except at 120 minutes where we found statistical difference between both the groups. Subjects
of group II (PK, n =9) had lower mean RR than group I (DK, n=13) subjects [23.6 vs 30; p<0.01]. However this difference in RR did not have any clinical significance.
Figure 3. Line diagram comparing respiratory rates among the groups.
The median duration of procedure in the 58 children was 99 minutes ranging from 25 to 120 minutes. The median time to recovery from the sedation was 7.5 minutes ranging from 2 to 35 minutes. The duration of the procedure and recovery score did not differ among both the groups. The time to recovery differed significantly among both the groups (13 min, group I vs 5 min, group II; p <0.01) as depicted in Table 4.
Table 4. Comparison of duration and recovery scores among both the groups.
Group I (n =31) Group II (n =27) P Duration of the
procedure 100 (62, 120) 96 (60, 120) 0.65 Time to recovery 13 (10, 20) 5 (4, 6) <0.01
Recovery score 6 (6, 7) 6 (6, 7) 0.13
All values are expressed in median, IQR unless specified P value from, Mann-Whitney U test
6. Discussion
We enrolled 60 children who underwent device closure procedures for acyanotic congenital heart disease (ASD, VSD and PDA). Among the 60 patients, 31 had received DK combination and 29 received PK combination for deep sedation.
due to difference in intrinsic sensitivity to Dexmedetomidine/Propofol in our group of subjects. Equal amounts of additional Inj Ketamine between the groups were noted in study by Ali NP et al[10] similar to our study. However our study did not use any narcotic infusions for maintaining deep sedation.
The median time for recovery from sedation was different among both the groups [13 min (10,20) in group I vs 5 min (4,6) in group II; p <0.01). The patients receiving Dexmedetomidine-Ketamine had prolonged recovery as compared to subjects receiving Propofol-Ketamine. The elimination half life of Inj Dexmedetomidine (100-150 min) is approximately 3 times longer than Inj Propofol (30-60 min).[11] We did not use Inj Ketamine infusion for maintanence which may explain the speedy recovery of the children after the procedure in our study. The similar drug combinations were compared for paediatric sedation in burn subjects [12] and in children undergoing upper gastrointestinal endoscopy. [13] In pediatric burns patients both combinations were found to be effective in providing sedation and analgesia. The DK group had prolonged recovery (p< 0.05) and the PK group had significantly high incidence of respiratory depression. In the study done by Mogahed et al [12] DK group had higher ketamine consumption then PK group (p=0.001).
We did not find any significant clinical difference with regard to hemodynamic and respiratory variables among the groups. We hypothesized Inj Propofol to have more cardiovascular depressant action than Inj Dexmedetomidine, but contrary the effect of both the drugs was similar in our study. This may be due to use of Inj Ketamine in addition which led to better hemodynamic stability. [14]. Heart rate (HR) was found to be lower in group DK as compared to propofol group after 10 min in our study. This bradycardic effect could be explained due to decrease in norepinephrine release as a result of presynaptic alpha 2 receptors activation in the peripheral nervous system. This finding is similar to the study done by Sharkawy et al [15] in which decreased heart rate was recorded in D-K group, 2 min and 5 min after the tracheal intubation (p=0.017).
We noticed adverse events in two subjects in PK group; they developed respiratory depression resulting in conversion to general anesthesia. We did not notice any other side effects like laryngospasm, shivering or convulsions as also noted in study by Tosun Z et al. [8]
7. Limitations of the Study
We restricted our study cohort to a selective group of CHD. Sedation depth was assessed objectively in our group. Use of BIS monitoring could have had a better assessment. There was lack of double blinding of our cases.
8. Conclusion
Our study compared the efficacy of both Dexmedetomidine-Ketamine and Propofol-Ketamine
combinations for device closure in children in the cardiac catheterization laboratory. We conclude that acceptable level of sedation can be achieved with both the drug combinations, however Dexmedetomidine-Ketamine combinations tend to prolong the recovery in a few cases. We also observed no difference in trend of hemodynamic and respiratory parameters among both the combinations except for lower heart rates seen with Inj Dexmedetomidine. The lack of narcotic usage in this study has simplified post procedure monitoring of these children, thereby allowing the children to be shifted after 4 to 6 hours of observation to a less monitored facility. This also has economic benefits.
References
[1] Saxena A. Congenital Heart Disease in India: a Status Report. Indian J Pediatr 2005; 72: 595-598.
[2] Spies C, Cao Q-L, Hijazi ZM. Transcatheter Closure of Congenital and Acquired Septal Defects. European Heart Journal Supplements 2010; 12: E24-E34.
[3] Lam JE, Lin EP, Alexy R, Aronson LA. Anesthesia and the Pediatric Cardiac Catheterization Suite: A Review. Paediatr Anaesth 2015; 25: 127-134.
[4] Hanslik A, Moysich A, Laser KT, Mlczoch E, Kececioglu D, Haas NA. Percutaneous Closure of Atrial Septal Defects in Spontaneously Breathing Children under Deep Sedation: A Feasible and Safe Concept. Pediatr Cardiol 2014; 35: 215-222. [5] Joshi VS, Kollu SS, Sharma RM. Comparison of Dexmedetomidine and Ketamine versus Propofol and Ketamine for Procedural Sedation in Children undergoing Minor Cardiac Procedures in Cardiac Catheterization Laboratory. Ann Card Anaesth 2017; 20: 422-426.
[6] Cote CJ, Wilson S. AMERICAN ACADEMY OF PEDIATRICS, AMERICAN ACADEMY OF PEDIATRIC DENTISTRY. Guidelines for Monitoring and Management of Pediatric Patients Before, During and After Sedation for Diagnostic and Therapeutic Procedures Pediatrics 2019; 143. [7] Ramsay MA, Savege TM, Simpson BR, Goodwin R.
Controlled Sedation with alphaxalone-alphadolone. Br Med J 1974; 2: 656-659.
[8] Steward DJ. A Simplified Scoring System for the Post-operative Recovery Room. Can Anaesth Soc J 1975; 22: 111-113. [9] Tosun Z, Akin A, Guler G, Esmaoglu A, Boyaci A.
Dexmedetomidine-ketamine and Propofol-ketamine Combinations for Anesthesia in Spontaneously Breathing Pediatric patients undergoing Cardiac Catheterization. J Cardiothorac Vasc Anesth 2006; 20: 515-519.
[10] Parvez Ali N, Kanchi M, Singh S, Prasad A, Kanase N. Dexmedetomedine-Ketamine versus Propofol-Ketamine as anaesthetic agents in Paediatric Cardiac Catheterization, JAFMC Bangladesh 2004; 1: 19-24.
[12] Canpolat DG, Esmaoglu A, Tosun Z, Akn A, Boyaci A, Coruh A. Ketamine-propofol vs ketamine-dexmedetomidine combinations in pediatric patients undergoing burn dressing changes. J Burn Care and Res 2012; 33 (6): 718-722.
[13] Mogahed MM, Salama ER. A Comparison of Ketamine-Dexmedetomidine versus Ketamine-Propofol for Sedation in Children during Upper Gastrointestinal Endoscopy. Journal of Anesthesia & Clinical Research 2017; 8 (11): 785.
[14] Friesen RH, Twite MD, Nichols CS, Cardwell KA, Pan Z, Darst JR, et al. Hemodynamic response to ketamine in children with pulmonary hypertension. Paediatr Anaesth 2016; 26: 102-108.