uring the past decade, the fi eld of refractive surgery has been fl ooded with dramatic advances introduced by new technologies. Aside from new applications of the femtosecond laser, further improvements were achieved with the development of new excimer laser platforms with higher repetition rates, faster eye trackers, and customized ablation profi les. Along with this rapid development, the pri-mary goal of refractive surgery has evolved and today aims to provide “super vision” in terms of visual performance.
The quest for “super vision” has generated a surge of inter-est, leading to the development of new algorithms of treat-ment and numerous technological improvetreat-ments in the new-er gennew-erations of excimnew-er lasnew-ers. A large numbnew-er of studies comparing different ablation profi les and different excimer laser platforms have been published. However, has an ideal algorithm of treatment emerged from these studies? Does one ablation profi le clearly demonstrate superiority compared to the other in regards to visual acuity, contrast sensitivity, or night symptoms?
After describing the technical properties of the various treat-ment algorithms using wavefront technology, we attempted to provide an overview of the clinical results available among several comparative studies. The factors tending to limit the success of these new procedures were also discussed along with future perspectives in the fi eld. Studies reporting results of such profi les for retreatments, highly aberrated eyes, kera-toconus, or transplant as well as results of topography-guided treatments were not included in this review.
TECHNICAL CONSIDERATIONS OF ABLATION PROFILES The technical aspects of excimer laser ablation have evolved considerably since the introduction of the formula for standard
D
ABSTRACT
PURPOSE: To provide an overview of the clinical results of different ablation profi les based on wavefront tech-nology and discuss their characteristics and limitations.
METHODS: Literature review of studies reporting results of ablation profi les based on wavefront technology in virgin healthy eyes.
RESULTS: Over the past 10 years, a large number of studies comparing different treatment algorithms and newer excimer laser platforms have been published. Thirty-six clinical studies including 3637 eyes analyz-ing the clinical results obtained after wavefront-guided, wavefront-optimized, and Q-factor profi les have been reviewed. Although wavefront-driven profi les allowed re-duction of the amount of induced optical aberrations with conventional ablations, thereby improving the qual-ity of vision, it appears that no algorithm of treatment or excimer laser platform has demonstrated a clear supe-riority over another. Wound healing and unexpected bio-mechanical response to surgery affect the accuracy of customized treatments and produce variable results. In addition, it is diffi cult to rigorously analyze and compare fi ndings among different studies because of the diverse variety in which the data are reported.
CONCLUSIONS: Despite several technological improve-ments over the years, wavefront ablation profi les have not consistently demonstrated superiority in terms of vi-sual acuity and lower order aberrations compared to the standard procedure, although the induction of higher order aberrations has been reduced. The concept of an individualized eye model has emerged recently, based on the optical ray tracing algorithm, and could theo-retically provide a higher level of customization, thus fulfi lling the promise of “super vision.” [J Refract Surg. 2012;28(3):xxx-xxx.]
doi:10.3928/1081597X
From the Refractive Surgery Department, Cole Eye Institute, Cleveland Clinic Foundation, Cleveland, Ohio.
Dr Krueger receives consulting and research funds from Alcon Laboratories Inc, Ft Worth, Texas. The remaining authors have no financial interest in the materials presented herein.
Correspondence: David Smadja, MD, 1701 E 12th, W22Q, Cleveland, OH 44114. Tel: 216.501.3340; E-mail: davidsmadj@hotmail.fr
Received: April 9, 2011; Accepted: December 6, 2011
Wavefront Ablation Profi les in Refractive
Surgery: Description, Results, and
Limitations
David Smadja, MD; Glauco Reggiani-Mello, MD; Marcony R. Santhiago, MD;
Ronald R. Krueger, MD, MSE
sphere-cylindrical correction described by Munnerlyn
in 1988.1 Over the years, and with the surge of
inter-est generated by wavefront technology, advanced laser treatment algorithms based on different concepts have been developed, aiming to correct not only lower but also higher order wavefront aberration errors.
WAVEFRONT-GUIDED TREATMENT REQUIREMENTS
Towards the end of the past decade, a new era began with the introduction of ablation profi les guided by the wavefront map to sculpt the cornea in a way to correct preexisting aberrations and reduce surgically induced aberrations. To achieve the precision required for this profi le, advancements in excimer laser technology were needed.
The broad beam cannot treat small irregularities in the cornea and most current devices use fl ying-spot technology, in which smaller beams (0.5 to 1.0 mm) are used for better and more accurate results in custom ablations and the correction of irregular astigmatism.
Spot sizes ⬍1 mm are required to adequately correct
up to the fourth order terms whereas 0.6-mm beams
are needed to treat up to the sixth order terms.2 Some
devices have a variable spot size (eg, VISX S4; Abbott Medical Optics Inc, Santa Ana, California).
The shape of the beam is also important to produce a smoother surface, which is best achieved with an
optimized spot overlap.3 The energy is delivered in a
Gaussian profi le (greater energy density in the center of the beam than the periphery) with the Allegretto Wave Eye-Q laser (Alcon Laboratories Inc, Ft Worth, Texas), MEL 80 (Carl Zeiss Meditec AG, Jena, Germany), and
NIDEK NAVEX (NIDEK Co Ltd, Gamagori, Japan).4
The fl ying-spot laser must be delivered precisely for an accurate wavefront correction and requires high-speed eye-tracking systems because of the smaller spot size and risk of individual pulse decentration and mis-placement compared to broad-beam lasers. Centration
needs to be accurate,5 as minimal misalignment or
cy-clotorsion that would normally cause only a small un-dercorrection in the spherical-cylindrical profi le can induce a completely different aberration pattern.
The-oretical modeling indicates that a decentration ⬎0.10
mm can induce rather than reduce aberrations during
myopic wavefront-guided treatments.6
The repetition rate of laser pulses is another feature that varies among excimer lasers. Repetition rate cor-relates directly with treatment time. Longer periods cause drying of the corneal stroma and loss of fi xation, which are unacceptable with customized profi les. In the fi rst broad-beam lasers, the repetition rate was low (6 to 10 Hz). With scanning-spot technology, the rate needed to increase; otherwise, treatment times would
be longer because more pulses would be needed for the same ablation.
The scanning-spot frequency must not exceed a rate
that can be followed by the tracking system.6 In
addi-tion, excessive thermal damage in adjacent tissue can occur with repetition rates higher than 60 Hz. Modern devices, such as the Amaris excimer laser (SCHWIND eye-tech-solutions GmbH & Co KG, Kleinostheim, Ger-many), use higher repetition rates up to 500 Hz for fast-er treatments with scanning spots. In these devices, a repetition rate in a determined locale does not exceed 40 Hz because the pulses are being applied sequentially in different locations of the cornea to prevent thermal
damage.7
WAVEFRONT-OPTIMIZED PROFILE
Controversy remains concerning the proper defi
ni-tion of the optimal ablani-tion profi le. Artal et al8 found
that eyes with smaller wavefront aberrations did not achieve the best visual quality. In 2004, Mrochen et
al9 designed an optimized aspheric profi le to
compen-sate only for the spherical aberration induced with the conventional treatment, preserving the preexisting optical aberration pattern of the eye. Since then, this algorithm of treatment has been introduced in sev-eral modern excimer laser platforms and is in theory less dependent on technical aspects that are critical in wavefront-guided treatment. This profi le has been de-veloped considering the loss in ablation effi cacy due to the angle of incidence of the excimer laser pulses in the midperiphery (ie, the cosine effect, leading to an oval beam of reduced energy on the peripherally sloping cornea), which can lead to a decrease in the intended ablation depth in this region and an increase in spherical aberration. The optimized profi les com-pensate for this effect by increasing the pulse energy in the periphery.
CUSTOM-Q FACTOR PROFILE
Based on the concept that an ideal asphericity of the cornea could lead to a better visual performance, the “Q-factor adjusted” profi le was developed to manipu-late the asphericity by selecting the desired target of Q-value. Based on an aspheric eye model, Manns et
al10 suggested that a minimum of spherical aberration
would be obtained at a target Q-factor of approximately
⫺0.4. Some excimer laser platforms are equipped with
this profi le such as the Allegretto Wave Eye-Q laser with the adjustable “Q software mode,” allowing the surgeon to target the Q-value independently from the preexisting spherical aberration and the NAVEX sys-tem with the “Optimized Prolate Ablation (OPA).” The OPA profi le uses both corneal topography and ocular
aberrometry to either maintain the natural corneal shape of the cornea after surgery or to target a specifi c
corneal asphericity to improve the visual quality.11 The
MEL 80 platform is equipped with the CRS-MASTER La-ser Blended Vision module, which allows manipula-tion of the corneal asphericity to increase the depth of focus to overcome presbyopia. This module has been used to create a non-linear aspheric ablation to provide
micro-monovision.12
CONVENTIONAL TREATMENT AND DEVELOPMENT OF CUSTOMIZED ABLATION PROFILES
The main complaints reported by patients after con-ventional excimer laser refractive surgery are blurred vision under low light conditions, halos, and glare,
which lead to decreased visual quality.13 These
com-plaints could occur despite achieving 20/20 visual acuity on the Snellen chart and are believed to be due to the surgically induced increase in high order
aberra-tions (HOAs) after laser treatment.14 By reshaping the
cornea, the lasers modify the curvature and aspheric-ity in a way that induces an increase in HOAs, espe-cially spherical aberration, due to the optical effect of the transition zone between the treated and untreated cornea. The amount of induced optical aberrations is correlated with the level of attempted refractive
cor-rection.15 It is well known that the effects of signifi cant
HOAs degrade the quality of the optical image on the fovea. Although some controversy exists, it has been suggested that the correction of HOAs could lead to an improvement in contrast sensitivity and visual acu-ity.16,17 Therefore, the introduction of a customized correction based on the wavefront pattern of the eye was promising to overcome the main issues found in the conventional treatment.
OVERVIEW OF THE CLINICAL RESULTS
Over the past 10 years, a large number of studies comparing the different treatment algorithms and newer excimer laser platforms have been published. Despite efforts to show the superiority of wavefront-guided correction over the standard treatment, or a customized profi le over another, it remains unclear whether an ablation profi le has demonstrated its supe-riority over another in terms of visual performance and patient satisfaction.
For clarity, and despite the lack of standardization concerning patient selection and treatment parameters surrounding the majority of these studies, we attempt-ed to summarize the main results reportattempt-ed in the lit-erature using the different available wavefront ablation profi les (wavefront-guided, wavefront-optimized, and custom-Q) in virgin healthy eyes.
Potential advantages of using these ablation profi les in highly aberrated eyes such as retreatment for decen-tered ablation, small optical zone, irregular astigma-tism, keratoconus, or transplant are not discussed in this review.
INTRODUCTIONOF WAVEFRONT ABLATION PROFILES
Wavefront-guided Treatment. To avoid induction and reduce preexisting aberrations of the eye, the wavefront-guided profi le was developed. The fi rst
re-sults reported by Seiler et al18 in 2000 after performing
wavefront-guided LASIK on 35 eyes were encourag-ing. After 3 months, 93.5% of eyes had uncorrected distance visual acuity (UDVA) of 20/20 or better, and supernormal vision, defi ned as 20/10 or better, was achieved in 16%. Postoperative HOAs decreased in 22.5% of eyes. However, optical aberrations increased on average by a factor 1.44 with a 5-mm pupil. More re-cently, studies using different wavefront-guided plat-forms have supported these primary results, reporting improvements in visual acuity and contrast sensitivity
postoperatively.19-21
Although this ablation profi le was developed with the goal of avoiding both induction of optical aberra-tions and reduction of preexisting aberraaberra-tions, recent studies reported the limitations of such customized
treatments. Bottos et al22 retrospectively analyzed 177
myopic eyes and 32 hyperopic eyes that underwent wavefront-guided LASIK for correction ranging from
⫺9.87 to ⫹6.25 diopters (D). They reported a high
cor-relation between the amount of preoperative refractive
error and asphericity changes (r2=0.81, P⬍.001) and
in-duced corneal spherical aberrations (r2=0.34, P⬍.001)
and thus concluded that changes depended on the magnitude of the refractive correction. Additionally, they highlighted the tendency for the postoperative Q-value and spherical aberration to be more positive after myopic ablation and more negative after
hyper-opic ablation. Keir et al23 reported similar results in a
prospective study analyzing the impact of hyperopic wavefront-guided LASIK on HOAs and contrast sensi-tivity. A signifi cant change was noted in postoperative spherical aberration, which had a reverse sign (became negative) and a high correlation was found between low contrast visual acuity and induced spherical
aber-ration (r2=0.62, P⬍.001).
With the surge of interest generated by the wave-front-guided treatment, the need to improve outcomes to meet expectations led the current generation of la-sers to undergo many technological improvements over the past 10 years. Following the company-driven technological developments, several studies compar-ing different wavefront-guided laser platforms have
been published despite the bias introduced such as the familiarization to the use of a new platform and the need for nomogram adjustment that is surgeon-depen-dent. Despite the introduction of different technologi-cal advancements in all platforms, superiority of one system over another has yet to be established in the
peer-reviewed literature.24-26
Wavefront-optimized Treatment. Good visual out-comes have also been reported with the
wavefront-optimized profi le. George et al,27 using the Allegretto
Wave Eye-Q laser, found that 92% of myopes and 63% of hyperopes achieved UDVA of 20/20 after 3 months, and no statistically signifi cant surgically induced spherical aberration was noted among myopic eyes.
Using the AMARIS platform, Arbelaez et al28 found
similar results, with 84% of 50 myopic eyes achieving UDVA of 20/20 or better and 40% achieving UDVA of 20/16 or better after 6 months. No signifi cant chang-es in aberration metrics were found postoperatively.
Vongthongsri et al29 also reported good results after
myopic treatment using the optimized aspheric treat-ment zone (OATz) profi le, which is available with the NIDEK NAVEX system. In their study, 94.2% of eyes were within 0.50 D of the intended refraction and 75% of eyes achieved UDVA of 20/20 or better after a mean follow-up of 3 months.
RESULTSOF COMPARATIVE STUDIES BETWEEN CONVENTIONALAND WAVEFRONT PROFILES
Conventional vs Wavefront-guided Treatment. Nu-merous studies published in the literature have failed to demonstrate a clear advantage of wavefront-guided over conventional treatment for low to moderate
my-opia and myopic astigmatism.30,31 In a contralateral
study comparing 10 eyes treated with conventional LASIK and 10 eyes with wavefront-guided LASIK,
Phusitphoykai et al30 did not fi nd any statistically
signifi cant differences regarding visual outcomes and optical aberrations postoperatively. More recently,
Dougherty and Bains,31 in a series of 290 eyes,
com-pared the results of conventional LASIK using the NI-DEK EC-5000 (NINI-DEK Co Ltd, Gamagori, Japan) with those obtained after using 2 different wavefront-guided laser platforms, the VISX S4 CustomVue (VISX, Santa Clara, California) and CustomCornea (Alcon Laborato-ries Inc). No statistically signifi cant differences were observed regarding safety, effi cacy, or predictability among groups.
Other studies concluded that wavefront-guided ab-lation induces fewer aberrations than conventional
treatment, but still increases total HOAs.32,33 Kim et
al,32 in a contralateral eye comparative study including
24 patients treated with LASIK using the Technolas
217z excimer laser (Bausch & Lomb Surgical, Roches-ter, New York), reported a reduction in induced HOAs following wavefront-guided treatment. However, no clinical differences in terms of visual acuity, patient preference, and mesopic contrast sensitivity were ob-served between the two treatments.
Another group of studies reported a signifi cant su-periority of wavefront-guided compared to conven-tional treatment in terms of night visual performance
and glare symptoms.20,34 Schallhorn et al20 observed a
signifi cant improvement of night driving visual perfor-mance after wavefront-guided correction compared to conventional treatment.
Conventional Treatment vs Optimized Profi le. Al-though several authors reported good visual outcomes and only a small increment in surgically induced HOAs
after treatment with aspheric profi les,27,28 few
compar-ative studies with conventional treatment are available
in the peer-reviewed literature. Mastropasqua et al35
compared the visual outcomes and wavefront errors of 50 myopic eyes treated with photorefractive keratecto-my (PRK) using an aspheric profi le with the MEL 80 la-ser platform to 24 myopic eyes treated with a standard treatment using the MEL 70 laser platform. They found that both treatments caused an increase in HOAs. Nev-ertheless, the total wavefront error and spherical aber-ration were signifi cantly lower with the aspheric pro-fi le compared to conventional treatment. de Ortueta
et al36 compared 70 myopic eyes with conventional
treatment with 70 eyes treated with an aspheric profi le using the ESIRIS laser platform (SCHWIND eye-tech-solutions GmbH & Co KG). Their results were similar
to those reported by Mastropasqua et al,35 with an
in-crease of HOAs and spherical aberrations after ablation in both groups, but a smaller induction of HOAs after aspheric ablation than standard ablation.
When analyzing these data, despite showing a small reduction in the induction of HOAs with the wave-front-optimized profi le, it is not possible to conclude that it leads to superior visual performance compared to the standard treatment.
RESULTSOF COMPARATIVE STUDIES BETWEEN DIFFERENT WAVEFRONT ABLATION PROFILES
Wavefront-guided vs Wavefront-optimized. Both of these profi les have suggested a smaller increase in HOAs postoperatively compared to the conventional treatment. The wavefront-optimized profi le was in-troduced to preserve the natural prolate shape of the cornea and to compensate for the so-called “cosine ef-fect.” The idea is also to reduce the variables that can infl uence the fi nal outcome, resulting in a more simple procedure. In wavefront-guided treatments, as an
ex-ample, the quality of the wavefront map and correct axis alignment tend to be more crucial than in wave-front-optimized treatments.
To determine the place of this new algorithm in the
strategy of treatment, Stonecipher and Kezirian,37 in
a United States Food and Drug Administration trial, compared 374 myopic eyes randomized to receive either the optimized profi le or wavefront-guided profi le (which was approved for use in the United States in 2003) using the Allegretto Wave Eye-Q. Regarding the visual outcomes after 3 months, most of the results analyzed did not show any statistically signifi cant differences between groups, except for the percentage of eyes that achieved uncorrected distance visual acuity of 20/16, which was slightly higher in the wavefront-optimized group (76% vs 64%). Regard-ing postoperative wavefront errors, no difference was
found between groups in 83% of eyes that had ⬍0.30
μm of preoperative HOA root-mean-square (RMS). In
eyes that had ⬎0.30 μm of preoperative HOA RMS,
the wavefront-guided profi le resulted in less HOAs postoperatively than the wavefront-optimized profi le. In terms of these results, the authors concluded that wavefront-guided treatment did not have an advantage over wavefront-optimized treatment in the majority of cases. They suggested wavefront-guided treatment be considered if the magnitude of preoperative HOA
RMS is ⬎0.35 μm, which represents approximately
20% to 25% of eyes in the overall general popula-tion. Other recent studies have supported these fi
nd-ings.38,39 Hantera39 reported similar results with the
NAVEX, comparing the OATz algorithm (equivalent to the wavefront-optimized profi le) to the optimized path difference custom aspheric treatment (equivalent to the wavefront-guided profi le). The author found a greater tendency for increasing HOAs in eyes with
⬍0.30 μm HOA RMS preoperatively in the
wavefront-guided group. The reverse tendency was observed in the wavefront-optimized group. Therefore, the author recommended using the wavefront-optimized profi le
for eyes with preoperative HOA RMS ⬍0.30 μm.
Re-cently, Feng et al40 supported these fi ndings in a
meta-analysis including 7 studies and 930 eyes comparing wavefront-guided to wavefront-optimized LASIK for myopia. They reported no difference between profi les in terms of UDVA, corrected distance visual acuity (CDVA), and induction of HOAs for patients with
pre-operative HOA RMS ⬍0.30 μm. However, in eyes with
preoperative HOA RMS ⬎0.30 μm, the
wavefront-guided profi le induced less postoperative HOAs than the wavefront-optimized profi le.
In a prospective, randomized, double-masked study of 200 eyes that underwent LASIK for myopia and
astigmatism, Yu et al41 found no statistically signifi
-cant difference between treatments after 6 months. The variables analyzed included visual acuity, total HOAs, and contrast sensitivity in dim light conditions. An interesting fi nding in this study was the absence of a signifi cant difference in patient satisfaction level after both treatments, evaluating night driving symptoms; visual symptoms such glare, halos, or ghost images; fl uctuation of vision; and dryness. Perez-Straziota et
al,42 comparing 66 eyes receiving either
wavefront-guided or wavefront-optimized LASIK, respective-ly, found similar results with no difference between groups in terms of UDVA, CDVA, manifest refraction spherical equivalent, and HOAs after 3 months. An-other interesting fi nding in this study was that 14 eyes initially scheduled for wavefront-guided treatment had to be converted to wavefront-optimized for poor limbal ring alignment (8 eyes), a Wavescan that was inconsistent with the manifest refraction (5 eyes), and no iris registration (1 eye), indicating the high level of requirements for wavefront-guided compared to wave-front-optimized treatment.
George et al27 retrospectively evaluated the results
of 285 eyes treated with the wavefront-optimized pro-fi le using the WaveLight Allegretto laser and found excellent visual outcomes with a low postoperative
increase in HOAs of ⫹0.03 μm for myopic LASIK and
0.00⫾0.07 μm spherical aberration induced after 3
months. Comparing these results to former outcomes obtained with the wavefront-guided treatment using the LADAR CustomCornea, they reported a greater in-crease in surgically induced spherical aberration with the wavefront-guided compared to the wavefront-opti-mized profi le after myopic LASIK.
These results, although in contrast with previous studies comparing both ablation profi les, are consis-tent with the primary aim of the wavefront-optimized profi le, which is to preserve the natural shape of the cornea without inducing ocular aberrations.
Custom-Q Profi le. Koller et al43 compared this treat-ment algorithm to wavefront-guided ablation in a con-tralateral eye study of 35 patients treated with LASIK for myopia and astigmatism. They reported equal safe-ty and effi cacy using both treatments. Although the corneal asphericity was less impaired in the Q-factor
profi le up to ⫺5.00 D, no statistically signifi cant
dif-ference was noted regarding visual or optical
param-eters up to ⫺9.00 D, except after 1 month when the
wavefront-guided group had signifi cantly lower coma-like aberration. The unexpected result was the similar induced spherical aberration in both groups. Ghoreishi
et al,44 in a contralateral eye study comprising 56
with custom-Q PRK targeted to a Q-value of ⫺0.2 and the fellow eye treated with wavefront-guided PRK. They found no differences in terms of safety and visual outcomes and a similar increase in spherical
aberra-tions postoperatively. Stojanovic et al45 compared this
same algorithm of treatment with a target Q-value set
to ⫺0.5 or ⫺0.6, depending on the patient’s
preopera-tive asphericity and age, to the wavefront-optimized profi le. All eyes showed a tendency towards an oblate shift postoperatively; however, less shift was noted in the Custom-Q group than in the wavefront-optimized group. No differences were found regarding safety, refractive outcomes, low contrast visual acuity, and wavefront errors.
Of the few studies available in the peer-reviewed lit-erature comparing the custom-Q profi le to other abla-tion profi les, most failed to demonstrate any superior-ity of this algorithm of treatment over another. These fi ndings also suggest that the custom-Q profi le was not able to deliver exactly the attempted asphericity with the current technology, probably affected also by an unexpected wound-healing response.
In a multivariate regression analysis of 160 eyes that underwent wavefront-guided treatment, Tuan and
Chernyak46 found no signifi cant correlation between
the change in corneal shape and visual performance. The authors concluded that no standard optimal asphericity exists and the ideal shape needs to be
cus-tomized on an individual basis.37
LIMITING FACTORS PATIENT-RELATED LIMITATIONS
Despite all technological improvements, fi nal out-come is limited by patient-specifi c factors, such as wound healing and biomechanical response. Current excimer lasers are precise and can sculpt a plastic model with submicron precision. However, corneal wound-healing response tends to smooth features ap-plied to the corneal stroma and potentially avoid the effect of the intended ablation to correct HOAs. As
mentioned by Netto and Wilson,47 hyperplasia of the
epithelium within the ablated zone by even a single cell is likely to have a major affect on a customized cor-neal treatment, given that the diameter of an epithelial cell is larger than the ablation volume to correct 1 μm RMS of wavefront irregularity in a single point.
Furthermore, regarding the biomechanical response,
Dupps and Roberts48 suggested that a central ablation,
by releasing tension in the periphery, can lead to ex-pansion and thickening in the midperiphery causing a secondary fl attening of the center and thus a change in curvature. These postoperative issues are known
to hinder the accuracy of customized treatments and produce variable results because the majority of these profi les do not take into account these unexpected re-sponses.
Wavefront-guided treatment aims to correct the preexisting aberrations and avoid the induction of sig-nifi cant amounts of aberrations to improve visual per-formance, but questions have been raised with recent publications showing that the total RMS of HOAs is not a reliable predictor of visual performance. It has been shown that visual acuity varied signifi cantly de-pending on the combination of Zernike modes and
the relative contribution of each mode.49 From these
fi ndings, it remains to be seen whether the treatment of all HOAs is more benefi cial for visual performance and if not, which specifi c combinations of aberrations must be treated or, on the contrary, maintained or un-changed. Technology, such as adaptive optics, might be a useful tool to combine with wavefront technol-ogy to reach a higher level of customization. Preopera-tive patient simulations with different combinations of aberrations might help in determining the specifi c amount and Zernike mode of aberration to target with the treatment.
TECHNOLOGY-RELATED LIMITATIONS
Wavefront sensors are precise and reproducible when dealing with low to moderate magnitudes of higher order aberrations. However, because the mea-surement of ocular aberrations is based on the posi-tion of a collecposi-tion of spot images, if the eye is highly aberrated (decentered ablations, small optical zone, or irregular astigmatism), the spots overlap and the computer cannot determine the origin of an individ-ual spot, reducing the precision of the measurement. In addition, data analysis by a wavefront sensor does not take into account the quality of individual spots formed by the lenslet array, which can cause false readings in opacities and disruption of the tear fi lm. Furthermore, differences in the technology used by the different wavefront sensing devices such as Hartmann-Shack, Tscherning (position-based aberrometers), or dynamic skiascopy (time-based aberrometers) lead to different wavefront measurements, thereby further
in-creasing the discrepancy in results.50
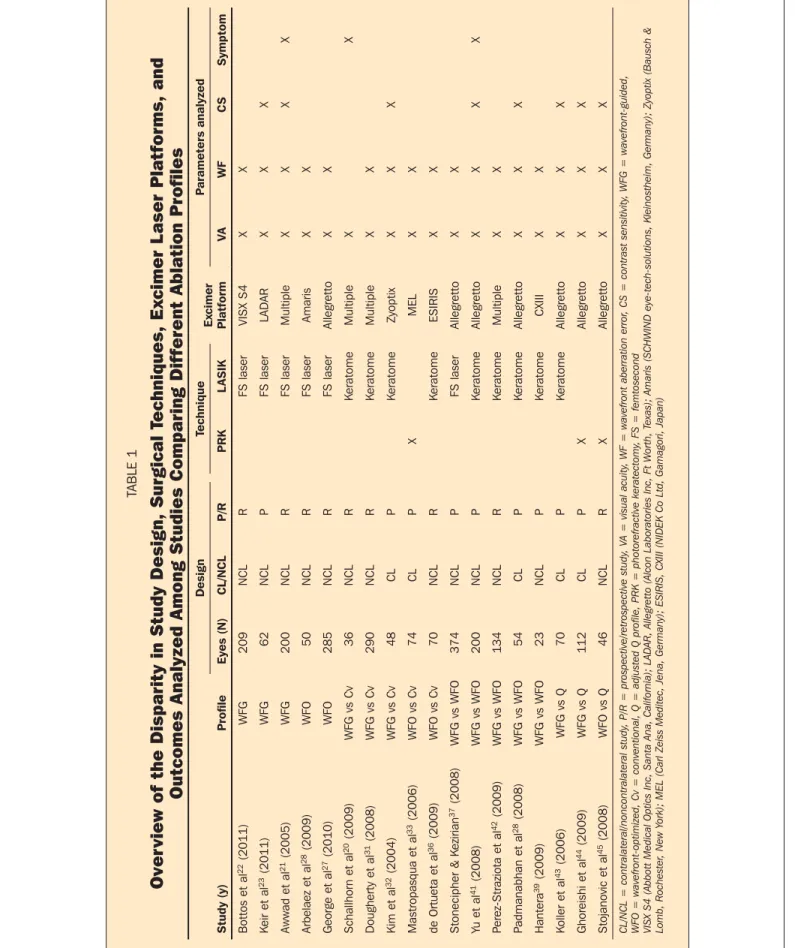
FACTORS LIMITING INTERPRETATIONAND ANALYSISOFTHE AVAILABLE RESULTS
Due to the disparity in results among the different comparative studies, and although customized abla-tion seems to provide better outcomes than conven-tional ablation in terms of induced aberrations, it ap-pears that no algorithm of treatment or excimer laser
TABLE 1
Over
view of the Disparity in Study Design, Surgical T
echniques, Ex
cimer L
aser Platforms, and
Outcomes Analyzed Among Studies Comparing Different Ablation Profiles
Design Technique Ex cimer Platform P arameters analyzed Study (y) Profi le Eyes (N) CL/NCL P/R PRK L ASIK V A WF C S Symptom Bottos et al 22 (2011) WFG 209 NCL R FS laser VISX S4 X X K eir et al 23 (2011) WFG 62 NCL P FS laser LADAR X X X Awwad et al 21 (2005) WFG 200 NCL R FS laser Multiple X X X X Arbelaez et al 28 (2009) WFO 50 NCL R FS laser Amaris X X George et al 27 (2010) WFO 285 NCL R FS laser Allegretto X X Schallhorn et al 20 (2009) WFG vs Cv 36 NCL R K eratome Multiple X X Dougherty et al 31 (2008) WFG vs Cv 290 NCL R K eratome Multiple X X Kim et al 32 (2004) WFG vs Cv 48 CL P K eratome Zyoptix X X X Mastropasqua et al 33 (2006) WFO vs Cv 74 CL P X MEL X X de Ortueta et al 36 (2009) WFO vs Cv 70 NCL R K eratome ESIRIS X X Stonecipher & K ezirian 37 (2008) WFG vs WFO 374 NCL P FS laser Allegretto X X Yu et al 41 (2008) WFG vs WFO 200 NCL P K eratome Allegretto X X X X P erez-Straziota et al 42 (2009) WFG vs WFO 134 NCL R K eratome Multiple X X P admanabhan et al 28 (2008) WFG vs WFO 54 CL P K eratome Allegretto X X X Hantera 39 (2009) WFG vs WFO 23 NCL P K eratome CXIII X X K oller et al 43 (2006) WFG vs Q 70 CL P K eratome Allegretto X X X Ghoreishi et al 44 (2009) WFG vs Q 112 CL P X Allegretto X X X Stojanovic et al 45 (2008) WFO vs Q 46 NCL R X Allegretto X X X CL/NCL = contralateral/noncontralateral study , P/R = prospective/retrospective study , V A = visual acuity , WF = wavefront aberra tion error , C S = contrast sensitivity , WFG = wavefront-guided,
WFO = wavefront-optimized, Cv = conventional, Q = adjusted Q profile, PRK = photorefractive keratectomy
, FS = femtosecond
VISX S4 (Abbott Medical Optics Inc, Santa Ana, California); LADAR, Allegretto (Alcon Laboratories Inc, Ft Worth, T
exas); Amaris
(SCHWIND eye-tech-solutions, Kleinostheim, Germany); Zyoptix (Bausch &
Lomb, Rochester
, New Y
platform has demonstrated a clear superiority over another. The main reason lies in the diffi culties in ana-lyzing and comparing fi ndings among those different studies. The Table summarizes the disparities in study design and parameters analyzed among several com-parative studies. The lack of standardization in patient selection, range of attempted correction, excimer laser platform and ablation algorithm used, nomogram ad-justments, and visual function tested (visual acuity, contrast sensitivity, wavefront errors, or subjective pa-tient satisfaction and visual symptoms) lead to a high degree of bias and signifi cant discrepancies in the re-sults. Furthermore, over the past 10 years, numerous improvements in excimer laser platforms such as fast-er repetition rates, fastfast-er eye trackfast-ers, and wavefront analyzers (providing more accurate measurements), may have led to superior outcomes, inducing more variables and thus further confusing the critical analy-sis of the results.
PERSPECTIVES
Despite the technological improvements and im-provements in refractive outcomes in terms of induc-tion of higher order aberrainduc-tions and reducinduc-tion of night vision symptoms compared to the standard
proce-dure,17-19 it is now a well known fact that
wavefront-guided ablation profi les are not as effective as original-ly promised. It was demonstrated that wavefront-based ablation profi les could lead to incomplete correction of HOAs or induction of additional aberrations, espe-cially when higher refractive corrections are required. The reason is believed to be due to an inaccurate trans-fer of a theoretically calculated ablation profi le to the cornea by simplifying the effect of the multi-lens
sys-tem of the eye. As suggested by Mrochen et al51 only
an individualized eye model, based on an optical ray tracing algorithm, can provide an ideal ablation profi le by achieving the highest degree of customization.
This eye model is obtained by taking into account the following parameters: wavefront of the entire eye, shape and curvature of the anterior and posterior sur-face of the cornea, corneal and lens thicknesses, an-terior chamber depth, axial ocular length, and after an optimization process, the data related to the lens surface. Unpublished data collected in the fi rst Euro-pean multicenter clinical trial on the ray tracing abla-tion profi le demonstrated excellent safety and effi cacy visual outcomes. After 3 months, 75% of eyes gained one line of CDVA and 5% gained two lines, whereas no eyes lost lines. These results seem to be promising and if a clinically signifi cant effect is confi rmed, this ray tracing ablation profi le may be able to fulfi ll the promise of “super vision.”
AUTHOR CONTRIBUTIONS
Study concept and design (D.S.); data collection (D.S.); analy-sis and interpretation of data (D.S., G.R.M., M.R.S., R.R.K.); drafting of the manuscript (D.S., G.R.M.); critical revision of the manuscript (M.R.S., R.R.K.); supervision (R.R.K.)
REFERENCES
1. Munnerlyn C, Koons SJ, Marshall J. Photorefractive keratectomy:
a technique for laser refractive surgery. J Cataract Refract Surg.
1988;14(1):46-52.
2. Waheed S, Krueger RR. Update on customized excimer ablations:
recent developments reported in 2002. Curr Opin Ophthalmol.
2002;14(4):198-202.
3. Huang D, Arif M. Spot size and quality of scanning laser
correc-tion of higher-order wavefront aberracorrec-tions. J Cataract Refract Surg.
2002;28(3):407-416.
4. Lubatschowski H, Kermani O, Welling H, Ertmer W. A scan-ning and rotating slit arF excimer laser delivery system for
re-fractive surgery. J Refract Surg. 1998;14(2 Suppl):S186-S191.
5. Ciccio AE, Durrie DS, Stahl JE, Schwendeman F. Ocular
cy-clotorsion during customized laser ablation. J Refract Surg.
2005;21(6):S772-S774.
6. Bueeler M. Maximum permissible lateral decentration in
aberra-tion-sensing and wavefront-guided corneal ablation. J Cataract
Refract Surg. 2003;29(2):257-263.
7. Iseli HP, Mrochen M, Hafezi F, Seiler T. Clinical
photoabla-tion with a 500-Hz scanning spot excimer laser. J Refract Surg.
2004;20(6):831-834.
8. Artal P. What aberration pattern (if any) produces the best vi-sion? Personal communication, 6th International Wavefront Congress; Feb 11-13, 2005; Athens, Greece.
9. Mrochen M, Donitzky C, Wüllner C, Löffl er J.
Wavefront-op-timized ablation profi les: theoretical background. J Cataract
Refract Surg. 2004;(30):775-785.
10. Manns F, Ho A, Parel JM, Culbertson W. Ablation profi les for wavefront-guided correction of myopia and primary spherical
aberration. J Cataract Refract Surg. 2002;28(5):766-774.
11. Holladay JT, Bains HS. Optimized prolate ablations with
the NIDEK CXII excimer laser. J Refract Surg. 2005;21(5
Suppl):S595-S597.
12. Reinstein DZ, Archer TJ, Gobbe M. LASIK for myopic astigma-tism and presbyopia using non-linear aspheric
micro-monovi-sion with the Carl Zeiss Meditec MEL 80 platform. J Refract Surg.
2011;27(1):23-37.
13. Chalita MR, Chavala S, Xu M, Krueger RR. Wavefront analysis in post-LASIK eyes and its correlation with visual symptoms,
refraction, and topography. Ophthalmology. 2004;111(3):447-453.
14. Marcos S, Barbero S, Llorente L, Merayo-Lloves J. Opti-cal response to LASIK surgery for myopia from total and
corneal aberration measurements. Invest Ophthalmol.
2001;42(13):3349-3356.
15. Moreno-Barriuso E, Lloves JM, Marcos S, Navarro R, Llorente L, Barbero S. Ocular aberrations before and after myopic cor-neal refractive surgery: LASIK-induced changes measured with
laser ray tracing. Invest Ophthalmol Vis Sci.
2001;(42):1396-1403.
16. Williams D, Yoon GY, Porter J, Guirao A, Hofer H, Cox I. Vi-sual benefi t of correcting higher order aberrations of the eye. J Refract Surg. 2000;16(5):S554-S559.
17. Rocha KM, Vabre L, Chateau N, Krueger RR. Enhanced visual acuity and image perception following correction of highly
ab-errated eyes using an adaptive optics visual simulator. J Refract
Surg. 2010;26(1):52-56.
18. Seiler T, Mrochen M, Kaemmerer M. Operative correction of
ocular aberrations to improve visual acuity. J Refract Surg.
2000;16(5):S619-S622.
19. Tuan K-mon A, Liang J. Improved contrast sensitivity and visual acuity after wavefront-guided laser in situ
keratomi-leusis: in-depth statistical analysis. J Cataract Refract Surg.
2006;32(2):215-220.
20. Schallhorn SC, Tanzer DJ, Kaupp SE, Brown M, Malady SE. Comparison of night driving performance after wavefront-guided
and conventional LASIK for moderate myopia. Ophthalmology.
2009;116(4):702-709.
21. Awwad ST, Haithcock KK, Oral D, Bowman RW, Cavanagh HD, McCulley JP. A comparison of induced astigmatism in conventional and wavefront-guided myopic LASIK using
LADARVision4000 and VISX S4 platforms. J Refract Surg.
2005;21(6):S792-S798.
22. Bottos KM, Leite MT, Aventura-Isidro M, et al. Corneal
aspheric-ity and spherical aberration after refractive surgery. J Cataract
Refract Surg. 2011;37(6):1109-1115.
23. Keir NJ, Simpson T, Hutchings N, Jones L, Fonn D. Outcomes of wavefront-guided laser in situ keratomileusis for hyperopia. J Cataract Refract Surg. 2011;37(5):886-893.
24. Moshirfar M, Espandar L, Meyer JJ, Tanner JR, Holz HA. Pro-spective randomized trial of wavefront-guided laser in situ keratomileusis with the CustomCornea and CustomVue laser
systems. J Cataract Refract Surg. 2007;33(10):1727-1733.
25. Awwad S, Bowman RW, Cavanagh HD, McCulley JP. Wave-front-guided LASIK for myopia using the LADAR
CustomCor-nea and the VISX CustomVue. J Refract Surg. 2007;23(1):26-38.
26. Durrie DS, Stahl J. Randomized comparison of custom laser in situ keratomileusis with the Alcon CustomCornea and the
Bausch & Lomb Zyoptix systems: one-month results. J Refract
Surg. 2004;20(5):S614-S618.
27. George MR, Shah RA, Hood C, Krueger RR. Transitioning to op-timized correction with the WaveLight ALLEGRETTO WAVE: case distribution, visual outcomes, and wavefront aberrations. J Refract Surg. 2010;26(10):S806-S813.
28. Arbelaez MC, Vidal C, Arba-Mosquera S. Excimer laser correc-tion of moderate to high astigmatism with a non-wavefront-guided aberration-free ablation profi le: six-month results. J Cataract Refract Surg. 2009;35(10):1789-1798.
29. Vongthongsri A, Phusitphoykai N, Siriboonkoom J. Compari-son of conventional and OATz ablation profi les for laser in situ
keratomileusis to correct myopia up to -10.00 diopters. J Refract
Surg. 2004;20(5 Suppl):S674-S675.
30. Phusitphoykai N, Tungsiripat T, Siriboonkoom J, Vongthongsri A. Comparison of conventional versus wavefront-guided laser in situ
keratomileusis in the same patient. J Refract Surg. 2003;19(2
Suppl):S217-S221.
31. Dougherty PJ, Bains HS. A retrospective comparison of LASIK outcomes for myopia and myopic astigmatism with conven-tional NIDEK versus wavefront-guided VISX and Alcon
plat-forms. J Refract Surg. 2008;24(9):891-896.
32. Kim T, Yang S, Tchah H. Bilateral comparison of wavefront-guided versus conventional laser in situ keratomileusis with
Bausch and Lomb Zyoptix. J Refract Surg. 2004;20(5):432-438.
33. Mastropasqua L, Nubile M, Ciancaglini M, Toto L, Ballone E. Prospective randomized comparison of wavefront-guided and conventional photorefractive keratectomy with the Meditec
MEL 70 Laser. J Refract Surg. 2004;20(5):422-431.
34. Lee HK, Choe CM, Ma KT, Kim EK. Measurement of contrast
sensitivity and glare under mesopic and photopic conditions following wavefront-guided and conventional LASIK surgery. J Refract Surg. 2006;22(7):647-655.
35. Mastropasqua L, Toto L, Zuppardi E, et al. Photorefractive kera-tectomy with aspheric profi le of ablation versus conventional photorefractive keratectomy for myopia correction: six-month
controlled clinical trial. J Cataract Refract Surg.
2006;32(1):109-116.
36. de Ortueta D, Arba Mosquera S, Baatz H. Comparison of stan-dard and aberration-neutral profi les for myopic LASIK with the
SCHWIND ESIRIS platform. J Refract Surg. 2009;25(4):339-349.
37. Stonecipher KG, Kezirian GM. Wavefront-optimized versus wavefront-guided LASIK for myopic astigmatism with the ALLEGRETTO WAVE: three-month results of a prospective
FDA trial. J Refract Surg. 2008;24(4):S424-S431.
38. Padmanabhan P, Mrochen M, Basuthkar S, Viswanathan D, Joseph R. Wavefront-guided versus wavefront-optimized laser
in situ keratomileusis : contralateral comparative study. J Cataract
Refract Surg. 2008;34(3):389-397.
39. Hantera M. Comparison of postoperative wavefront aberrations after NIDEK CXIII optimized aspheric transition zone treatment
and OPD-guided custom aspheric treatment. J Refract Surg.
2009;25(10 Suppl):S922-S926.
40. Feng J, Yu J, Wang Q. Meta-analysis of wavefront-guided
vs. wavefront-optimized LASIK for myopia. Optom Vis Sci.
2011;88(12):463-469.
41. Yu J, Chen H, Wang F. Patient satisfaction and visual symptoms after wavefront-guided and wavefront-optimized LASIK with
the WaveLight platform. J Refract Surg. 2008;24(5):477-486.
42. Perez-Straziota CE, Randleman JB, Stulting RD. Visual acuity and higher-order aberrations with wavefront-guided and
wave-front-optimized laser in situ keratomileusis. J Cataract Refract
Surg. 2010;36(3):437-441.
43. Koller T, Iseli HP, Hafezi F, Mrochen M, Seiler T. Q-factor cus-tomized ablation profi le for the correction of myopic
astigma-tism. J Cataract Refract Surg. 2006;32(4):584-589.
44. Ghoreishi SM, Naderibeni A, Peyman A, Rismanchian A, Esl-ami F. Aspheric profi le versus wavefront-guided ablation pho-torefractive keratectomy for the correction of myopia using the
Allegretto Eye Q. Eur J Ophthalmol. 2009;19(4):544-553.
45. Stojanovic A, Wang L, Jankov MR, Nitter TA, Wang Q. Wave-front optimized versus custom-Q treatments in surface ablation for myopic astigmatism with the WaveLight ALLEGRETTO laser. J Refract Surg. 2008;24(8):779-789.
46. Tuan KM, Chernyak D. A. Corneal asphericity and
visu-al function after wavefront-guided LASIK. Optom Vis Sci.
2006;83(8):605-610.
47. Netto MV, Wilson SE. Corneal wound healing relevance to
wavefront guided laser treatments. Ophthalmol Clin North Am.
2004;17(2):225-231.
48. Dupps W, Roberts C. Effect of acute biomechanical changes
on corneal curvature after photokeratectomy. J Refract Surg.
2001;17(6):658-669.
49. Applegate RA, Marsack JD, Ramos R, Sarver EJ. Interaction be-tween aberrations to improve or reduce visual performance. J Cataract Refract Surg. 2003;29(8):1487-1495.
50. Kim DS, Narváez J, Krassin J, Bahjri K. Comparison of the VISX
WaveScan and NIDEK OPD-Scan aberrometers. J Refract Surg.
2009;25(5):429-434.
51. Mrochen M, Bueeler M, Donitzky C, Seiler T. Optical ray trac-ing for the calculation of optimized corneal ablation profi les in
refractive treatment planning. J Refract Surg.
AUTHOR QUERIES
Your repeatedly mention that no algorithm has proven to be superior over another. Please remove all repetitive statements throughout the paper.
Regarding reference 8, did Dr Artal present a talk at this meeting? Did the author speak during the talk or after? The following was changed. Okay as edited?
Original: Decreased quality of vision reported by the patient as blurred vision under low light conditions,
ha-los, and glare are the main complaints after conventional excimer laser refractive surgery.13
Edited: The main complaints reported by patients after conventional excimer laser refractive surgery are
blurred vision under low light conditions, halos, and glare, which lead to decreased visual quality.13
Please clarify the following.
Following the company-driven technological developments, several studies comparing different
wave-front-guided laser platforms have been published despite the bias introduced such as the familiarization to the
use of a new platform and the need for nomogram adjustment that is surgeon-dependent. Please clarify the following.
These fi ndings also suggest that the custom-Q profi le was not able to deliver exactly the attempted
asphe-ricity with the current technology, probably affected also by an unexpected wound healing response.
Please clarify the following.
However, corneal wound-healing response tends to smooth features applied to the corneal stroma and
potentially avoid the effect of the intended ablation to correct HOAs.
Please provide a source and year for the unpublished data in the last paragraph of the article.
In unpublished data collected in the fi rst European multicenter clinical trial on the ray tracing ablation profi le, excellent safety and effi cacy visual outcomes were reported. After 3 months, 75% of eyes have gained one line of CDVA and 5% gained two lines, whereas no eyes lost lines
In the last sentence of the article, “super normal vision” was changed to “super vision,” as used in the Abstract and Introduction. Okay as edited?