West Virginia Advanced Practice Registered Nurses
A White Paper to assist the West Virginia Nurses Association and West Virginia
Advanced Practice Registered Nurses in their efforts to provide unrestricted safe,
quality health care services to the residents of West Virginia.
Jennifer L Fellman RN MSN FNP-C, doctoral candidate, The George Washington University, in consultation with Andrea Brassard, RN, DNSc, FNP-C, Center to Champion Nursing in America
Table of Contents
Executive Summary………3
Introduction……….4
Definition of Advanced Practice Registered Nurses (APRNs)………6
Map of Physician-APRN Collaboration by state………..7
West Virginia APRNs……….7
Status of Health Care……….8
Primary Care Dilemma………..9
National Trends-IOM Report………12
APRN Quality and Cost Effectiveness Certified Nurse Midwives……….13
Nurse Practitioners………....14
Clinical Nurse Specialists………...15
Certified Registered Nurse Anesthetists………...16
APRN Safety………17
Conclusion………19
References……….20
Appendix A: Health Professional Shortage Area...………..24
Appendix B: Chronic Illness….………...25
Executive Summary
West Virginia faces many challenges in meeting the health care needs of its citizens with nearly half of the total population residing in rural areas. This region is further disadvantaged with a significant number of disabled, uninsured and underinsured people. These Appalachian citizens have high rates of chronic illness, unhealthy lifestyles, and have geographical and financial limitations to accessing a health care provider.
Ø The West Virginia Nurses Association is pursuing the removal of restrictive legislative language to allow autonomous practice for all advanced practice registered nurses in congruence with national scope of practice trends and to better meet the needs of West Virginia’s medically underserved residents.
Ø West Virginia is challenged by its geography and economy to adequately provide the primary care physicians needed to support access to care for its vulnerable population. Ø The Institute of Medicine issued a report in 2010 that calls for states to remove
unnecessary barriers that prevent advanced practice registered nurses from practicing to the full extent of their education and training.
Ø Advanced practice registered nurses provide high quality, cost-effective care that has been championed in research studies time and time again.
Ø The West Virginia requirement of a collaborative agreement for advanced practice registered nurses to practice or prescribe is unsupported in any research spanning nearly five decades.
Ø West Virginia legislature should focus its efforts to improve access to primary care services instead of supporting unnecessary, burdensome restraints that impede West Virginia from improving the health status of its citizens.
Introduction
The U.S. health care system has been challenged by the media and in the political arena, but most importantly, has impacted the health and wellbeing of millions of American families who are unable to find quality, cost-effective primary care. The Affordable Care Act (ACA), a historic piece of legislation that was signed into law in March 2010, will allow approximately 32 million uninsured and underinsured working-age Americans to obtain health insurance through either state-run health exchanges or Medicaid. In addition to outlining a plan for Americans to obtain health insurance outside of their employment, the ACA distinguishes the need for nurses to be key members in the delivery of health care.
The influx of newly insured individuals will strain an already fragile health care system that is not able to meet the health care needs of its current population. Most of these individuals will obtain health insurance through either a state health exchange or through Medicaid. In a national sample, no more than 60% of adult primary care physicians and only 43% of
pediatricians were planning to accept new Medicaid patients under the ACA (Olson, 2012). The primary care physician deficit is most pronounced in rural areas, small towns, and lower socio-economic areas.
There are no quick solutions to the current physician shortage. Medical students graduate with a significant amount of debt and many are choosing specialty practice, where salaries are often considerably higher than in primary care. Attracting physicians to practice in rural, impoverished regions is even more difficult. The utilization of advanced practice registered nurses in mitigating the health care shortage has met resistance from physician groups, despite many federal organizations and states removing restrictions that prevented these providers from practicing to the full scope of their education and training.
Advanced practice registered nurses (APRNs) have provided not only primary health care for over five decades, but also practice in ambulatory, acute, and long-term care. Primary care emphasizes health education, wellness, prevention, and screening for the early detection of disease. Providers of primary health care are trained to address a variety of health care needs across the lifespan (Colorado Health Institute, 2008). APRNs include nurse practitioners (NPs), certified nurse midwives (CNMs), certified registered nurse anesthetists (CRNAs), and clinical nurse specialists (CNSs).
The National Council of States Boards of Nursing (NCSBN) define APRN preparation as having:
1. Completed accredited graduate-level education program 2. Passed a national certification examination
3. Advanced clinical knowledge and skills for direct patient care
4. Education that prepares him/her with the responsibility and accountability to promote healthy lifestyles and to assess, diagnose, manage patient problems, including the use and prescription of pharmacologic and non-pharmacologic therapies.
5. Demonstrated proficiency in analysis of data, role autonomy, demonstrate greater depth and breadth of knowledge with registered nursing competency as the foundation (NCSBN, 2012).
Defining APRNs
Who Are They Numbers in the US What do they do?
Nurse Practitioners 158,348
Perform health histories and complete health exams; diagnose and formulate treatment plan for acute and chronic illnesses; prescribe and manage
medications; order and interpret lab and x-rays; teach and counsel patients
Clinical Nurse Specialists
59,242
Provide advanced nursing care in acute care facilities such as hospitals; provide acute and chronic care management; develop quality improvement programs; mentor and educate staff; work as researchers and consultants
Certified Registered Nurse Anesthetists
34,821
Administer anesthetics before and after surgical, obstetric, and therapeutic procedures; practice in hospitals, ambulatory surgical centers and dental offices; more than 65% of all anesthesia in the US is provided by these APRNs.
Certified Nurse
Midwives 18,492
Provide primary care to women, which include family planning, gynecological care, prenatal care, low risk labor and delivery and neonatal care. These APRN providers work in hospitals, birthing centers, community clinics, and in patient homes.
Source: Adapted with permission from AARP Center to Champion Nursing (2009). Types of Advanced Practice Registered Nurses. Retrieved from: http://championnursing.org/resources/advanced-practice-registered-nurses-charts.
APRNs maintain continuing education hours in medicine and pharmacology just like their physician counterparts. Though NPs can legally practice in all states and the District of Columbia, the ability of APRNs to practice to the full extent of their education and training is dictated by individual state laws. Eighteen states and the District of Columbia allow NPs to practice and prescribe independently (without any direct physician supervision or collaboration). The remaining states regulate NP practice with requirements such as direct physician supervision for diagnoses, treatment and/or prescriptive authority.
West Virginia APRNs
The West Virginia (WV) Board of Nursing is the sole regulating body for APRNs. The 908 NPs in West Virginia (Kaiser Family Foundation, 2012) have at least a master’s degree in nursing and obtain national certification to practice. Many APRNs also obtain postmaster’s certificates, doctoral degrees, or secondary specialty designations. Nurse practitioners and certified nurse midwives provide primary care to WV residents. Although NPs and CNMs may be designated as primary care providers for reimbursement with insurance carriers, they are restricted in their ability to provide primary care services due to legislative barriers. A nurse practitioner that wants to provide primary care services must find a physician with whom to
collaborate in order to prescribe medications. Certified nurse midwives must collaborate for prescribing and practice. These requirements limit West Virginia from implementing innovative solutions such as nurse-managed rural health or mobile clinics, which would increase health care access for all West Virginians.
The Status of Health Care in West Virginia
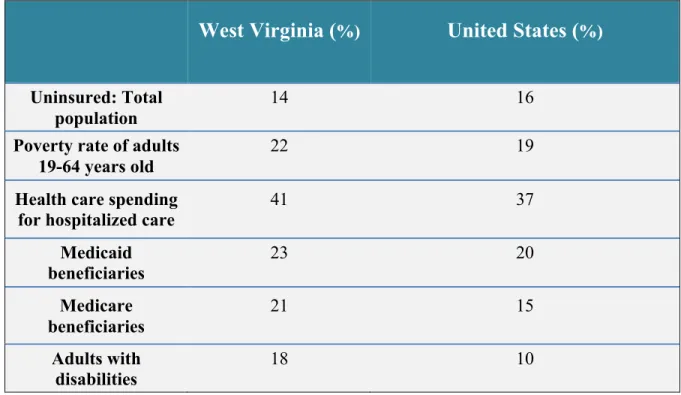
Chronic disease is the leading cause of death for West Virginians. A 2011 report from the West Virginia Department of Health and Human Resources found that West Virginians have significantly higher rates than the rest of the nation for poor nutrition, smoking, obesity, diabetes, hypertension, stroke, coronary heart disease, heart attack and arthritis (Appendix A). Table 1 below illustrates West Virginia compared to the U.S. population regarding insurance, health care spending and poverty rates:
West Virginia (
%)United States (
%) Uninsured: Totalpopulation
14 16
Poverty rate of adults 19-64 years old
22 19
Health care spending
for hospitalized care 41 37
Medicaid beneficiaries 23 20 Medicare beneficiaries 21 15 Adults with disabilities 18 10
According to the “State Scorecard” published by the Commonwealth Fund (2012), West Virginia ranks poorly for several criterion. Ranking is from 1st to 50th.
For 2009 West Virginia scored:
§ 50th for healthy lives (breast and colorectal cancer deaths, suicide, tobacco use, child obesity, infant mortality)
§ 47th for avoidable use of hospital care
§ 27th for overall access to health care services.
In order to improve access to care and to prevent unnecessary hospital admissions, the Commonwealth Fund recommends a relationship with a primary care provider who can coordinate care. If West Virginia was to match the best performing state for each criterion:
§ $41 million dollars would be saved from hospital readmissions § $71 million could be saved from overall hospitalizations
§ 71,000 adult citizens would receive recommended preventive care (colonoscopy, mammogram, flu shots)
§ 144,000 West Virginia adults would have a source of reliable care so that their health needs are coordinated and accessible (Commonwealth Fund, 2012).
Primary Care Dilemma in West Virginia
Rural areas have notoriously lacked adequate primary care physicians to meet the needs of their residents. Appalachia West Virginia is traditionally known to suffer from significant economic challenges and insufficient health care. This region faces continued physician shortages due to its rugged, vast geography. Some 42% of Appalachian residents reside in rural locales, further complicating access to primary care providers (Baker et al, 2012). In 2011,
819,192 people, just under half of the total population, were residing in a rural area in West Virginia (United States Department of Agriculture (2012).
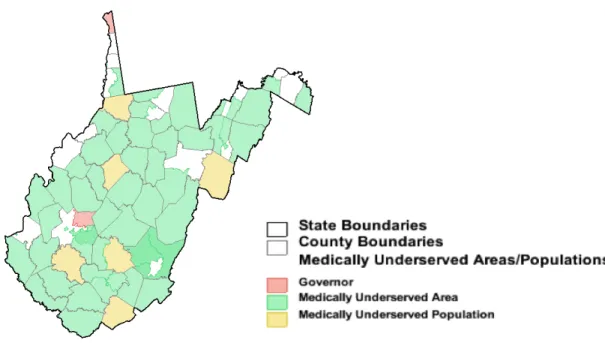
According to the Health Resources and Services Administration (2012), West Virginia has 53 designated medically underserved geographical areas (Figure 1) and has 89 designated primary care Health Professional Shortage Areas (HPSAs) (Appendix B) impacting 120,465 or nearly 6% of WV citizens. In addition to socioeconomic barriers to care, providers that are unwilling to accept patients with Medicare/Medicaid contribute to West Virginia’s HPSAs (2012).
Figure 1 Medically Underserved Areas and Medically Underserved Populations. Retrieved from Rural Assistance Center (2012).
http://www.raconline.org/racmaps/mapfiles/mua_muptype. png.
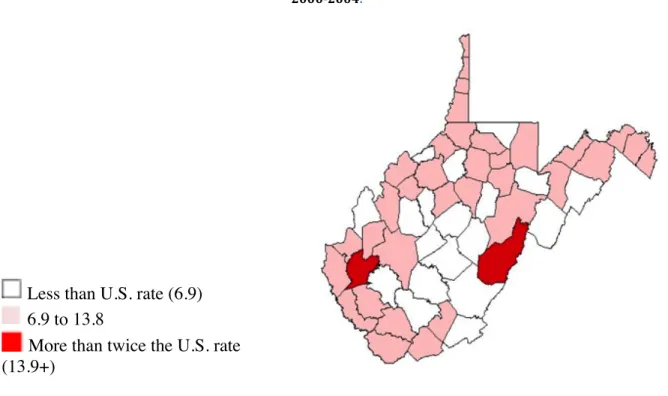
Infant mortality rate is another measure of the nation’s health and is measured as deaths per 1,000 live births. West Virginia’s overall infant mortality rate (Figure 2) is 7.7 compared to 6.9 for the rest of the United States. Thirty-six counties in West Virginia have an infant
mortality rate higher than the U.S. average, and 2 counties had a rate more than twice the national average.
Less than U.S. rate (6.9) 6.9 to 13.8
More than twice the U.S. rate (13.9+)
Source: NCHS Natality and Mortality Detail Files Data access from the Area Resource File Health Resources and Services Administration, HHS.
Increasing costs of medical liability insurance for providers performing obstetric care, a decline in the number of hospital and birthing facilities, and the lack of obstetricians practicing in rural locales contributes to inadequate access and timely prenatal care for West Virginian women (Appendix C). Clearly change is needed to improve West Virginia’s maternal-child health outcomes.
Figure 2 Infant mortality rates, 5-‐year average from 2000-‐2004.
National Trends
The Institute of Medicine (IOM), in a landmark consensus report: “The Future of Nursing: Leading Change, Advancing Health”, details recommendations for policymakers and others concerned with improving health care. The IOM, whose committee members include physicians and other professionals in business, academia, health policy and health care delivery, have recommended:
§ State legislatures should reform scope-of-practice regulations to conform to the National Council of State Boards of Nursing Model Nursing Practice Act and Model Nursing Administrative Rules;
§ Congress should expand the Medicare program to cover services provided by APRNs within their scope of practice just as physicians are currently covered
§ The Federal Trade Commission and Antitrust Division of the Department of Justice should review existing and proposed regulations affecting APRNs to ascertain those with anticompetitive effects without contributing to the health and safety of the public. States with unjustifiably restrictive regulations should be urged to revise them to allow APRNs to provide any and all care within their scope of practice, regardless of situation
Certified Nurse Midwives
These APRN providers have deep historical roots of caring for childbearing women. Records of midwifery practice date back to the time of Hippocrates. Maternal mortality rates in the 19th century were five times higher for physicians than midwives.
Quality of Care
Studies of nurse midwives caring for impoverished, urban women in New York in the 1930s found significantly lower rates of morbidity and mortality than any other hospital service in the area (Raisler & Kennedy, 2005). During the early 20th century, there was a paradigm shift in the care of childbearing women as obstetricians/surgeons began performing deliveries for all women in hospitals. The midwife profession was nearly eradicated until resurgence in the nurse-midwife model of care emerged in the Appalachian Mountains of Kentucky. Here, the Frontier Nursing Service provided community-based care to disadvantaged pregnant women, children, and families. (Ernst & Stone, 2013).
This historical perspective demonstrates that CNMs have always provided safe, quality care. Low-risk women are routinely subjected to medical interventions, many of which are unsupported in research as beneficial, such as continuous fetal monitoring, induction of labor, intravenous therapy, epidural anesthesia, and elective cesarean births. Pregnant women cared for by CNMs are less likely to undergo invasive interventions, which reduce health care costs without sacrificing quality (Johantgen et al., 2012).
Cost Effective Care
Certified nurse midwives have historically provided obstetric and gynecologic care to vulnerable female populations. These women are at higher risk for poor maternal and infant outcomes. The care provided by CNMs has been shown to be excellent with lower utilization of
often unnecessary, expensive medical interventions such as labor induction, vacuum or forceps delivery and caesarean section (MacDorman & Singh, 1998).
Nurse Practitioners
Dr. Henry Silver, a pediatrician and Dr. Loretta Ford, a nurse, were the innovators of the NP role in the 1960s to meet the primary care needs of an underserved pediatric population. Since that time, the NP role has expanded with well-documented research that NPs provide quality care at substantially lower cost (Gardner, Posmontier, & Conti, 2011)
Quality of Care
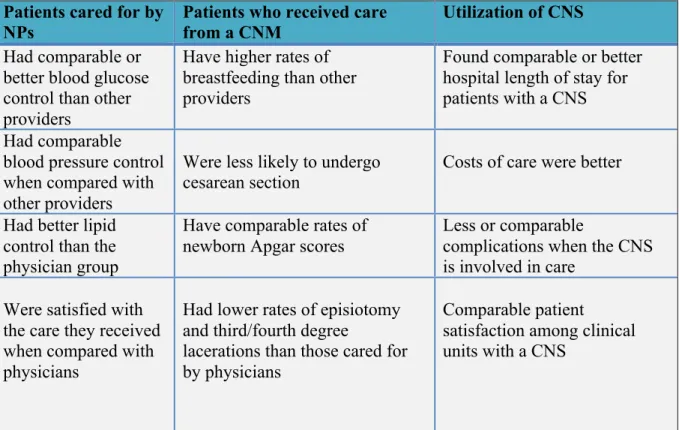
A notable physician-led study compared the effectiveness of nurse practitioners and physicians given the same setting and same level of authority. The physician researchers were concerned that if the NPs were given the same patient caseload, were required to the same on-call demands, and work independently that patient care would suffer. Their concerns were unsupported, as patient outcomes for asthma and diabetes were equivalent for both provider groups. The patients in the NP group had lower blood pressure readings than the patients in the physician group (Mundinger et al., 2000). Key points from a large systematic review of literature that compared the quality and effectiveness of patient care when provided by NPs, CNMs and CNSs to other providers (physicians or teams without an APRN) follows below (Table 2). Cost Effective Care
Nurse practitioner cost savings was estimated by a RAND Corporation analysis in the state of Massachusetts. Savings of $4 to $8 billion could be expected over a 10-year period by allowing the substitution of NPs for physicians in primary care. Utilizing a NP in the primary care setting is 20-35% less costly than using physicians (Eibner, Hussey, Ridgely, & McGlynn, 2009).
Actual cost savings were found in a nearby southern state. A manufacturing firm implemented a NP managed onsite clinic for its 4300 employees and their dependents. The NP
managed minor acute illnesses, encouraged health promotion and prevention and helped individuals with chronic medical conditions such as diabetes in managing their condition. Annual savings of health care costs for the company was $1.3 million with an initial investment of $83,000, generating a cost-benefit ratio of 1:15. These cost savings did not take into account the additional savings than a NP managed clinic can generate such as reducing on-site injuries or enhancing employee productivity (Chenoweth, Martin, Pankowski, & Raymond, 2005).
Reduction of costs and improvement of quality and patient satisfaction by using NPs has been documented at:
o Veterans Administration Health System o Geisinger Health System
o Kaiser Permanente
o U.S. retail health clinics (Fairman, Rowe, Hassmiller, & Shalala, 2011). NPs are highly skilled at providing comprehensive assessments resulting in clinical decision-making that is safe and cost effective. Nurse practitioners have favorable outcomes in acute care settings such as hospitals by reducing length of stay and hospital-associated costs (Carruth & Carruth, 2011).
Clinical Nurse Specialists
The clinical nurse specialist role was first developed in 1940s and has evolved to meet the needs of an ever-changing healthcare system.
Quality
These clinical nurse experts serve in a variety of roles in the hospital and outpatient clinics. Multiple studies have demonstrated the positive outcomes associated with CNS involvement in patient care. The CNS role adds value to the delivery of healthcare services by providing education, support and advocacy.
Cost Effective Care
Clinical nurse specialists are experts in their specialties. The costs of managing chronic illness decrease when a CNS is involved in management of the patient. Research supports the utilization of a CNS as part of the interdisciplinary team to lower hospital costs and improve the outcomes of patients with chronic illness (Moore & McQuestion, 2012).
Patients cared for by NPs
Patients who received care from a CNM
Utilization of CNS
Had comparable or better blood glucose control than other providers
Have higher rates of breastfeeding than other providers
Found comparable or better hospital length of stay for patients with a CNS Had comparable
blood pressure control when compared with other providers
Were less likely to undergo cesarean section
Costs of care were better
Had better lipid control than the physician group
Have comparable rates of newborn Apgar scores
Less or comparable
complications when the CNS is involved in care
Were satisfied with the care they received when compared with physicians
Had lower rates of episiotomy and third/fourth degree
lacerations than those cared for by physicians
Comparable patient
satisfaction among clinical units with a CNS
Table 2 Information adapted from Newhouse et al. (2011). Advanced practice nurse outcomes 1990-‐2008: A systematic review. Nursing Economic$, 29(5), 230-‐251.
Certified Registered Nurse Anesthetists
The profession emerged during the American Civil War by assisting surgeons in giving chloroform to wounded soldiers during surgery. The role developed further through both World
Wars, with national certification beginning in 1945.
The fourth category of APRNs, certified registered nurse anesthetists (CRNAs) provide safe, high-quality anesthetic care. Currently, 70% of all anesthetics in rural hospitals are safely delivered by CRNAs (Gardner et al., 2011). The U.S. military has allowed CRNAs to practice
autonomously for decades (Jenkins, Elliott & Harris, 2006). The Centers for Medicare and Medicaid in 2001 allowed states to “opt-out” of physician (surgeon or anesthesiologist) oversight of CRNAs as research failed to support the need for such restriction. During a 6-year period, those states that opted out of physician supervision of CRNAs did not see any increase in patient mortality (Dulisse & Cromwell, 2010).
Cost Effective Care
Certified registered nurse anesthetists are able to perform the same anesthetic procedures as anesthesiologists. Anesthesia training for CRNAs and anesthesiologists is equivalent, but the costs to train CRNAs are substantially less: $160,000 for CRNA preparation and $1million for anesthesiologists (Teske, 2012). Research has not shown that patient care, safety or quality compromised when a CRNA practices without physician oversight. In addition to education and training costs, CRNAs practicing independently can provide anesthesia services at 25% lower costs (Jordan, 2011).
Safe Practice of APRNs
Americans have consistently ranked nurses as the most trusted profession for more than a decade. In fact, when the Gallup poll first added nurses to their list of “most trusted” professions in 1999, they were ranked in 1st place and have maintained that position every year since with the exception of 2001, when firefighters (after the September 11th attacks) took the top spot. The American public holds the nursing profession in very high regard for honest and ethical
standards when compared with other professions including physicians, pharmacists, clergy, and police officers (Jones, 2010). The nursing profession is built on a foundational code of ethics that embodies integrity, accountability, self-respect, and care of individuals regardless of social or economic status (ANA, 2001).
The safety of APRN providers is often an issue of debate for physician groups and
legislators when discussing the role of APRNs and independent practice. Collaboration of health care providers is the professional norm. When faced with an issue or situation outside of a provider’s own proficiency, it is expected that they will refer to a provider with the specialized skill required of the situation. Malpractice rates do not increase when APRNs practice
independently. From 2007-2008, the top 5 malpractice cases against APRNs (108 of 501 total cases) were in states with the most restrictive physician/APRN collaborative agreements (Miller, 2011). The argument for retaining a physician-APRN collaborative agreement because it makes care safer is unsupported in this scenario.
Nurse practitioners are independently licensed in all states. Each NP is personally accountable for the care they provide to patients, regardless of collaborative or supervisory requirement. No research has demonstrated that physician supervision of an APRN improves patient safety. Autonomous practice of a NP does not negate collaboration. It merely implies accountability, since NPs, like physicians, will consult or refer when the patient situation is outside of the scope of the provider. Further support is evidenced by data from the National Practitioner Data Bank (NPDB), where malpractice rates of NPs are no higher in states with independent NP practice when compared with those where collaboration is required for practice (Pearson, 2012).
Some physicians maintain that they fear being held liable when collaborating with, or accepting referrals from, APRNs. Vicarious liability, the financial responsibility for malpractice of another provider, can only exist in an employer-employee relationship. The physician is not liable for the actions of an APRN if an agreement to refer or collaborate is in place. The
providers of different scopes of practice (Booth, 2007). Physicians and APRNs should carry malpractice insurance that terms them as responsible, individual providers.
Conclusion
The overwhelming research that supports the safe, quality, cost-effective care provided by APRNs should alleviate hesitation on the part of legislators to move forward with eliminating unnecessary, burdensome restrictions for APRNs. West Virginians have inherent obstacles to primary health care due to geography and limited primary care physicians serving in rural areas. More physicians’ train and establish practices in urban areas, leaving the most vulnerable citizens with limited options in care (Larson et al. 2003). States with similar rural populations such as Montana, Wyoming, Vermont, Idaho and Maine have removed restrictive APRN barriers to allow their residents improved access to primary care. West Virginia faces many challenges in meeting the health care needs of its citizens. Removing APRN scope of practice barriers would align West Virginia with national models, improving West Virginians access to care.
References
American Nurses Association (2001). Code of ethics for nurses with interpretive statements. Retrieved from:
http://www.nursingworld.org/MainMenuCategories/EthicsStandards/CodeofEthicsforNur ses/Code-of-Ethics.pdf
Baker, H.H., Pathman, D.E., Nemitz, J.W., Boisvert, C.S., Schwartz, R. J., & Ridpath, L.C. (2012). Which U.S. medical schools are providing the most physicians for the Appalachian region of the United States? Academic Medicine, 87 (4), 498-505. doi: 10.1097/ACM.0b013e318248f3be.
Booth, J.W.(2007). An update on vicarious liability for certified nurse-midwives/certified midwives. Journal of Midwifery & Women’s Health, 52(2), 153-157.
Carruth, P.J. & Carruth, A.K. (2011). The financial and cost accounting implications of the increased role of advanced nurse practitioners in U.S. healthcare. American Journal of Health Sciences, 2(2). Retrieved from
http://www.journals.cluteonline.com/index.php/AJHS/article/download/6622/6698. Chenoweth, D., Martin, N., Pankowski, J., Raymond, L.W. (2005). A benefit cost analysis of a
worksite nurse practitioner program: First impressions. Journal of Occupational and Environmental Medicine, 47(11), 1110-1116. Retrieved from
http://chenoassociates.com/Documents/JOEM-05-262.pdf.
Colorado Health Institute (2008). Collaborative scopes of care. Retrieved from www.coloradohealthinstitute.org.
Commonwealth Fund (2012). Health system data center: State scorecard. Retrieved from http://www.commonwealthfund.org/Maps-and-Data/State-Data-Center/State-Scorecard.aspx.
Dulisse & Cromwell (2010) No harm found when nurse anesthetists work without supervision by physicians. Health Affairs, 29(8), 1469-1475.
Eibner, C.E., Hussey, P.S., Ridgely, M.S., & McGlynn, E.A. (2009). Controlling health care spending in Massachusetts: An analysis of options. RAND Corporation. Retrieved from www.rand.org/pubs/technical_reports/TR733.html.
Ernst, E.K. &Stone, S.E. (2013). The birth center: Innovation in evidence-based midwifery care. In B.A. Anderson & S. Stone (Eds.), Best practices in midwifery: Using the evidence to implement change (pp. 79-82). New York, NY: Springer.
Fairman, J.A., Rowe, J.W., Hassmiller, S., & Shalala, D.E. (2011). Broadening the scope of nursing practice. The New England Journal of Medicine, 364(3), 193-196. Retrieved from
http://www.floridanurse.org/arnpcorner/ARNPDocs/NEJMNursePractitionerArticle.pdf. Gardner, M.R., Posmontier, B. & Conti, M.E. (2011). The evolution of advanced practice
nursing roles. In H.M. Dreher & M.E. Smith Glasgow (Eds.), Role development for doctoral advanced nursing practice (pp. 69-81). New York, NY: Springer.
Health Resources and Services Administration (HRSA) (2012). HRSA in your state fact sheet: West Virginia. Retrieved from:
Institute of Medicine (2010). The future of nursing: Leading change, advancing health report recommendations. Retrieved from
http://www.iom.edu/~/media/Files/Report%20Files/2010/The-Future-of-Nursing/Future%20of%20Nursing%202010%20Recommendations.pdf.
Jenkins, C.L., Elliott, A.R., & Harris, J.R. (2006). Identifying ethical issues of the department of the Army civilian and Army nurse corps certified registered nurse anesthetists. Military Medicine, 171, 762-769.
Johantgen, M., Fountain, L., Zangaro, G., Newhouse, R., Stanik-Hutt, J., & White, K. (2012). Comparison of labor and delivery care provided by certified nurse-midwives and
physicians: A systematic review, 1990 to 2008. Women’s Health Issues, 22(1), e73-e81). doi: 10.1016/j.whi.2011.06.005.
Jones, J. (2010). Nurses top honesty and ethics list for the 11th year: Lobbyists, care salespeople, members of Congress get the lowest rating. GALLUP Economy.
Jordan, L. (2011). Studies support removing CRNA supervision rule to maximize anesthesia workforce and ensure patient access to care. AANA Journal, 79 (2), 101-104.
Kaiser Family Foundation (2012). Statehealthfacts.org: West Virginia
Retrieved from http://www.statehealthfacts.org/profileind.jsp?cat=8&rgn=50.
Larson, E.H., Johnson, K.E., Norris, T.E., Lishner, D.M., Rosenblatt, R.A., & Hart, L.G. (2003). State of the health workforce in rural America: Profiles and comparisons. Retrieved from http://depts.washington.edu/uwrhrc/uploads/RuralCh4Comparisons.pdf.
MacDorman, M.F. & Singh, G.K. (1998). Midwifery care, social and medical risk factors, and birth outcomes in the USA. Journal of Epidemiology and Community Health, 52(5), 310-317.
Miller, K.P. (2011). Malpractice: Nurse practitioners and claims reported to the national practitioner data bank. The Journal for Nurse Practitioners, 7(9), 761-773.
Moore, J. & McQuestion, M. (2012). The clinical nurse specialist in chronic disease. Clinical Nurse Specialist, 26(3), 149-163. doi: 10.1097/NUR.0b013e3182503fa7.
Mundinger, M.O., Kane, R.L., Lenz, E.R., Totten, A.M., Tsai, W.Y., Cleary, P.D., …Shelanski, M.L. (2000). JAMA, 283(1), 59-68.
National Council of State Boards of Nursing (2012). Campaign for APRN consensus. Retrieved from https://www.ncsbn.org/aprn.htm.
Olson, L.K. (2012). Medicaid, the states and health care reform. New Political Science, 34(1). doi: 10.1080/07393148.2012.646020.
Pearson, L.J. (2012). The Pearson report. Retrieved from http://www.pearsonreport.com/. Raisler, J. &Kennedy, H. (2005). Midwifery care of poor and vulnerable women, 1925-2003.
Journal of Midwifery & Women’s Health, 50(2), 113-121. Doi: 10.1016/j.jmwh.2004.12.010.
Teske, A.E. (2012). Advanced practice nurses in Ohio community hospitals. Journal for Nurse Practitioners 8(2). doi: 10.1016/j.nurpra.2011.06.006.
United States Department of Agriculture (2012). State fact sheets: West Virginia. Retrieved from http://www.ers.usda.gov/StateFacts/WV.htm.
Appendix A
Adapted from the West Virginia Department of Health & Human Resources (2011) Retrieved from
http://www.wvdhhr.org/bph/hsc/pubs/other/chronicdiseasemanandprev2011/advocating_for_chronic_dise ase_management_and_prevention_2011.pdf.
*West Virginia’s rate is significantly higher than the national rate.
Risk Factor or Disease/Condition WV (%) US Average (%)
Overall Rank (compared to all 50 states and US territories) Poor nutrition* 83.8 76.2 3 Current smoking* 25.6 18.0 1 No exercise* 33.2 24.6 1 Obesity* 31.7 24.6 6 Diabetes* 12.4 9.1 2 Hypertension* 37.6 29.3 1
Ever had stroke* 3.7 2.5 4
Coronary heart disease* 7.1 4.0 1
Ever had heart attack* 6.5 4.0 1
Arthritis* 33.9 25.9 3
Appendix B
West Virginia Counties in Health Professional Shortage Areas
County not part of a HPSA
Whole county is designated as HPSA Part of county designated as HPSA
Source: Bureau of Health Professions, HHS Data accessed from the Area Resource File Health Resources
Appendix C
There is no federal designation for maternity-specific health professional shortage areas. Approximately 11,000 women in West Virginia have greater than a 30-minute drive to a birthing facility. A less than 30-minute drive to a birthing facility is standard for best outcomes. Retrieved from http://www.wvperinatal.org/shortage.htm.