SERVICES IN KENYA II
Lucy Anne Wanjiru aweru Bsc. (Family and Consumer Sciences) Reg. No. 157/11031104
A research thesis submitted for the award of the degree of Masters of Public Health in the School of Health Sciences of Kenyatta University
October, 2009
Waweru, Anne Wanjiru Effectsof
intergration of
1
1111
I!
IIIIII~ IIIIIIIIIIIIII~IIII
2011/357617
DECLARATION
This thesis is my original work and has not been presented for a degree or any other award in any other University.
Lucy Anne Wanjiru Waweru 157/11031/04
Signature ~~
SUPERVISORS' APPROVAL
This thesis has been submitted for review with our approval as University supervisors
Dr Margaret Keraka
Department of Public Health Kenyatta University
Signature __
----'
~
~=_=
_
__·
__
~
_
tt
Dateq
__
f_l_t_l_(
)
_9
__
Dr B.M Okello Agina Department of Public Health Kenyatta University
S;gnaWr
~'
-G
\J.-
a
~~
Date
cy \\\
l=7-J"DEDICATION
ACKNOWLEDGEMENT
Let me express my heartfelt appreciation to my supervisors Dr Margaret Keraka and Dr B.M Agina Okello for their invaluable guidance, counsel, suggestions, critical comments and encouragements during the writing of my thesis. Many thanks to Dr David Kiragu, Dr Naftali Oirere in addition to the members of staff of the Department of Public Health of Kenyatta University for their continued support. Special thanks go to Dr Joachim Osur and community of Family Health Options Kenya for creating a conducive environment for the study to be carried in. In addition to the members of staff and clients who took part in study in Nairobi-west and Thika Family Care Medical Clinics.
My appreciation goes to all my friends for their friendship, support and encouragement throughout the study period. I am greatly indebted to my parents, Miriam and Michael Waweru, my husband Julius Karuga and siblings for their prayers, support, and encouragement and for being my role models. Lastly to the Almighty God for granting
me sound health, wisdom, strength and grace to go through my Masters education. In addition to providing the resources that were required to facilitate my education.
TABLE OF CONTENTS
TITLE i
DECLARATION ii
DEDICATION .iii
ACKNOWLEDGEMENT iv
TABLE OF CONTENT v
LIST OF FIGURES .ix
LIST OF TABLES x
OPREATIONAL DEFINITION OF TERMS xi
ABBREVIATIONS AND ACROYNMS xii
ABSTRACT xiv
INTRODUCTION 1
1.1Background 1
1.2 Statement of the Problem 5
1.3 Justification of the Study 6
1.4'Research Questions 8
1.5 Null Hypothesis 8
1.6 Objectives 8
1.6.1 Broad Objective 8
1.6.2 Specific Objectives 8
1.7 Significance and Anticipated Output.. 9
CHAPTER TWO 14
LITERATURE REVIEW 14
2.2 Reproductive Health Services 14
2.3 Care for People Living With HIV and AIDS 15
2.4 Integration of Reproductive Health Services and HIV and AIDS Care 17
CHAPTER THREE 33
MATERIALS AND METHODS 33
3.1 Research Design 33
3.2 Variables 33
3.3 Location of the Study 35
3.4 Target Population 36
3.5 Study Population 37
3.5.1 Criteria for Inclusion 37
3.5.2 Criteria for Exclusion 37
3.6 Sampling Techniques and Sample Size : 38
3.6.1 Sampling Techniques 38
3.6.2 Sample Size Determination for Clients 38
3.7 Construction of Research Instruments 40
3.8 Pilot Study 40
3.8.1 Validity 41
3.8.2 Reliability 41
3.9 Data Collection 41
3.11 Logistical and Ethical Considerations 42
CHAPTER FOUR 44
DATA ANALYSIS, RESULTS AND DISCUSSIONS 44
4.1 Introduction 44
4.2 Socio-Demographic Characteristics of Study Population 44
4.3 Reproductive Health Services Utilized by Respondents 46
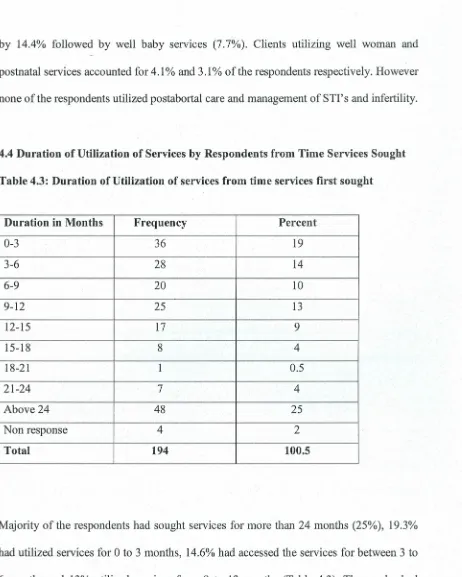
4.4 Duration of Utilization of Services by Respondents from Time Services
Sought 47
4.5 Reasons for Seeking Services from the Clinics 48
4.6 Utilization Patterns of Reproductive Health Services before Integration 48 4.7: Changes in Uptake of Reproductive Health Services Following Integration 50
,
4.8 Effects of Integration on the Utilization of Reproductive Health Services 54
4.8.3 Quality of Integrated Services 57
4.8.7 Work Load : 61
4.9 Factors affecting the Utilization ofIntegrated Services 61 4.9.1 Utilization Patterns of Integrated Services 61
4.9.3 Awareness of Availability ofHIV/ AIDS Related Services 63
4.10 Socio-Cu1tural Factors 66
4.11. Cost of Integrated Services 67
CHAPTER FIVE 70
SUMMARY, CONCLUSION AND RECOMMENDATION 70
5.2 Implication of the Findings 70
5.5 Recommendations 72
5.6 Areas for Further Research 73
REFERENCES , 74
Research Instrument. 77
7.4.1 Consent Form 77
Clients Questionnaire 78
LIST OF FIGURES
FIGURE PAGES
Figure 1.0 Conceptual Framework. 13
Figure 4.1 Quality of Integrated Services 56
Figure 4.2 Changes in Quality of Services after Integration 57
Figure 4.3 Utilization Levels of HIV and AIDS Related Services 60
LIST OF TABLES
TABLE
Table 2.0 Adding Family Planning to VCT Levels of Integration in Kenya .
Table 2.1 Potential Benefits and Challenges of Integration .
Table 4.1 Socio-Demographic Characteristic of Study Population .
Table 4.2 Reproductive Health Services Utilized by Respondents .
Table 4.3 Duration of Utilization of Services from Time Services First Sought.
Table 4.4 Utilization Patterns of Reproductive Health Services in Nairobi-West and Thika Family Care Medical clinic before Integration .
Table 4.5 General Changes in Uptake of Reproductive Health Services
following Integration .
Table 4.6 Changes in Utilization of Reproductive Health Services in
Nairobi-West Family Care Medical clinic following Integration .
Table 4.6.1 Changes in Utilization of Reproductive Health Services in Thika
Family Care Medical Clinic .
Table 4.7 Acceptance ofIntegration by Clients .
Table 4.8 Modes of Creating Awareness of Availability of HIV and AIDS
Related Services to Clients .
Table 4.9 Cost of Integrated Services .
Table 4.10 Changes on the Cost of Services after Integration .
OPERATIONAL DEFINITION OF TERMS
Reproductive health services: These are techniques and services that contribute to
reproductive health and well being by preventing and
solving reproductive health problems.
Comprehensive HIV/AIDS care: Focused care that meets patients' physical, social, psychological, emotional and spiritual needs.
Integration: Offering two or more services at the same facility,
during the same operating hours with the provider of one
service actively encouraging clients to consider using
the other services during the same visit.
Clients: Refers to women within the reproductive age bracket
(15-49 years) seeking reproductive health from the
clinics under study.
Service providers:
Refers to the short-term results or outcome of
integrating HIV and AIDS care into reproductive health
services and it can either be positive or negative.
Refers to the member of the medical clinics health facilities offering reproductive health services.
Effects:
Accessed: The utilization of reproductive health and HIV and
AIDS services that had been integrated. Synonymous to
AIDS ARBEF ARV CBOs EGPAF FBOs FGM FHI FHOK HIV NGO OVCs PLWHA PMTCT STI VCT ZNFPC
ABBREVIATIONS AND ACRONYMS
Acquired Immune Deficiency Syndrome
Association Rwandaise pour Ie Bien-Etre Familial
Antiretroviral
Community Based Organizations
Elizabeth Glaser Pediatric AIDS Foundation
Faith Based Organizations
Female Genital Mutilation
Family Health International
Family Health Options Kenya
Human Immune Deficiency Virus
Non-Governmental Organizations
Orphans and Vulnerable Children
People Living With HIV/AIDS
Prevention of Mother to Child Transmission
Sexually Transmitted Infections
Voluntary Counseling and Testing
ABSTRACT
CHAPTER ONE
INTRODUCTION
1.1 Background
Sub-Saharan Africa bears the largest burden of HIV and AIDS. In the year 2004, an
estimated 3.1 million people became infected, while 2.3 million people died of AIDS
almost 75% of deaths globally (UNAIDS, 2004). In 2005, Sub-Saharan Africa accounted
for 64% of the 5 million people who became newly infected with the HIV and AIDS
globally (UNAIDS, 2005). During 2006, around 4 million adults and children became
infected with HIV and AIDS. An estimated 39.5 million people were living with HIV and
AIDS globally with around 63% of PLWHA's living in Sub-Saharan Africa. The year
also saw around 3 million deaths from HIV and AIDS despite recent improvement in
access to antiretroviral treatment (UNAIDS 2006). Like many other parts of the world,
this region faces a rapid feminization of the epidemic. In Kenya, HIV and AIDS is still a
burden with 1.4 million people living with HIV. According to the results of the 2007
Kenya Aids Indicator Survey, 7.4% of adults aged 15-64 are infected with HIV, with
high HIV infection rates registered among old adults aged 50-64 years (KAIS,2007).
HIV and AIDS is disproportionately affecting women and girls. This is aggravated by
social and economic inequalities between men and women. Women and girls commonly
face discrimination in terms of access to education, employment, credit, health-care, land
and inheritance in addition to their biological vulnerability. These factors put women in a
position where they are particularly vulnerable to HIV and AIDS infection (UNAIDS
heterosexually, the vulnerability of women is increased by the fact that in many African
countries, sexual relationships are dominated by men as such women cannot always
practice safe sexs even when they know the risks involved (UNAIDS, 2006). Until an
effective and affordable vaccine or microbicide is developed they lack the means within
their control to prevent HIV/STI infection (UNAIDS, 2006). When women fall ill, their
families lose their primary care giver and often a primary bread winner. The women who
die leave behind millions of orphans. Meanwhile other sexually transmitted infections
remain both a cofactor in the spread of HIV and AIDS and a major problem in their own
right with an estimated 340 million new cases of STI's annually (WHO, 2003).
The gap in HIV and AIDS prevalence between men and women continues to grow. In
the year 2006, in Sub-Saharan Africa around 59% of those living with HIV and AIDS
were women. Many more young girls than young men are affected due to lack of access
to HIV and AIDS prevention services which leave them at risk for themselves and their
unborn children. In many countries of Southern Africa, one in five pregnant women is
infected with HIV and most children contract HIV and AIDS from their mothers (FHI,
2005). In 2005, an estimated 4.6% of women were living with the virus against 1.7%of
men living (UNAIDS, 2005). As is the case in many African countries, HIV prevalence
in Kenya is higher among women (8.7%) than among men (5.6%). According to the
results of Kenya Aids Indicators Survey released in 2007, young women between 15 and
34 years are more likely to have HIV in comparison to young men of the same age group.
Majority of the women infected with HIV come into contact with the health-care delivery system seeking reproductive health services. They do seek' the services either within clinical settings or through community based distribution programs. Reproductive health providers serve millions of women in developing countries now at the centre of global
HIV and AIDS pandemic (AGI and UNPF, 2003). Some half a million women in developing countries use a modem contraception method. Majority of pregnant women make at least one visit for prenatal care during pregnancy and a significant proportion of women make at least one post-natal clinic visit (AGI and UNPF, 2003). According to the Kenya Demographic Health Survey carried out in 2003 by Central Bureau of Statistics, 31% of women are on a modem method of contraception; about 90% of pregnant women make at least one antenatal visit, while post-partum care is accessed at least once by 42% of women, thus extending access to infants. Other reproductive health services that women seek from the clinics are well-baby, well-woman, management of STI's, management of infertility and lastly post-abortal care. For these reasons, the clinics and Community Based Distribution programs create opportunities to reach women with HIV and AIDS prevention information and services (AGI and UNPF, 2003).
solid base upon which stepped up interventions for HIV and AIDS prevention and
management can be built. These areas are counseling and advice about sexual health,
skills in communication with defined groups, sexual education for young people,
programs concerned with women's role in development, contraceptive counseling
especially valuable for PLWHA's and management of STI's. As such they are poised to
play an important role in reducing the incidents of HIV and AIDS infections over the
coming years. Policy makers, donors, researchers and activists should recognize the
benefits of supporting the fuller integration of HIV and AIDS prevention efforts with
reproductive health services (AGI and UNFPA, 2003).
All these in addition to the shift of focus at the beginning of 21stCentury to provision of
integrated reproductive health and HIV and AIDS services formed the basis for
integration to be implemented in Family Care Medical Centers managed by Family
Health Options Kenya (FHOK). FHOK formerly Family Planning Association of Kenya
is the pioneer of the family planning movement in Kenya. It was legally registered in
Kenya and affiliated to the International Planned Parenthood Federation (IPPF) in 1962.
The integration was implemented in four Family Care Medical Centers. The four,
Nairobi-West, Thika, Nakuru and Eldoret Family Care Clinics were selectively upgraded
for the introductory phase of the integration, which is more than four years old. The
integration has been rolled out to remaining four of the Family Care Medical Clinics
namely Kisumu, Rebeiro, Phoenix and Meru. It is anticipated that after the integration is
However the effects of the integration on the uptake of reproductive health services are
yet to be established since in most settings the two services are offered independently.
1.2 Statement of the Problem
In most settings in the world, reproductive health and HIV and AIDS services have been
offered separately with little or no integration. Reproductive health services primarily
target married women of reproductive age bracket while HIV and AIDS services target
individuals at high risk of HIV infection (Foreit et al., 2002). However the potential
benefits of integrating these services are increasingly apparent as ever more women of
reproductive age become infected with HIV and AIDS or at risk of infection (Foreit et
al., 2002). In developing countries about half of the 40 million people now living with
HIV and AIDS are women of reproductive age with percentage approaching 60% in
some African countries. The potential of reproductive health service providers reaching
women who accounted for nearly half of all adults living with HIV and AIDS with HIV
prevention, information (UNAIDS 2004). In addition to a ready infrastructure which is as
a result of donors and government investing heavily in reproductive health services over
the last three decades and services (AGI and UNFPA, 2003).
This has resulted to many types of integrations being explored but their effects on
. reproductive health services have not been rigorously evaluated and largely unknown.
Research is essential to assess the effects of integration on service quality, acceptability,
this that this study was carried in selected Family Care Clinics that have implemented the
integration of services.
1.3 Justification of the Study
Majority of HIV and AIDS infections are sexually transmitted or associated with
pregnancy, childbirth and breastfeeding. The interactions between reproductive health
and HIV and AIDS are widely recognized. Most of HIV infected persons are within
reproductive age, 63% of all HIV and AIDS cases are in Sub-Saharan Africa with women
accounting for 60%, 75-80% of all HIV and AIDS infections in this region are
transmitted heterosexually, with women and youth being most vulnerable (UNAIDS
2006). In addition, reproductive ill-health and HIV and AIDS share root causes including
poverty, gender inequality and social marginalization of the most vulnerable population
(UNFP A, 2005) The international community agrees that the Millennium Development ~
Goals will not be achieved without ensuring access to reproductive health services and an
effective global response to HIV and AIDS ( UNFPA,2005). This can be achieved
through the integration of services.
The integration of HIV and AIDS and reproductive health services creates a number of
important synergies. When programs offer clients the chance to meet multiple needs,
either within the same visit or via referral, they are more likely to achieve these important
health goals. Integrated services or better linkages may promote reaching broader groups
with information and services that are not typically reached in a particular vertical
reproductive health services like family planning services. However the unmet need for
these services is often greatest in countries with high HIV and AIDS prevalence (Myaya,
2004). These needs can be better met if the reproductive health services are offered where
such women access HIV and AIDS services.
Meanwhile clients accessing reproductive health services may well need HIV and AIDS
prevention, diagnosis and treatment services. Many of these clients are married women
who are usually considered at low risk of HIV and AIDS infection (Altman, 2004). But
evidence from several countries suggest that marriage may offer women little protection
against HIV and AIDS infection since married women may have little or no power to
negotiate safe sexual practice with their husbands (Altman, 2004). Forty percent of new
infections in Thailand occur between spouses and 90% of those infections are
transmitted from husband to wife (Agence France Presse, 2004). For the integration to
be effective and realize the potential benefits; policies, conceptual frameworks and
legislative frameworks supporting the integration of services are required, rigorous
research is needed to expose the experiences of other sites integrating services, evaluate
the impact of other models of integration and identify effective models. This study will
generate findings that will be used to this end.
1.4 Research Questions
1. What were the utilization patterns of reproductive health services before integration of
HIV and AIDS care into reproductive health services?
2. What were the changes in the uptake of reproductive health services following
integration HIV and AIDS care into reproductive health services?
3. What were the effects of integration of HIV and AIDS care into reproductive health
services on the utilization of reproductive health services?
4. What were the factors determining the utilization patterns of the integrated services?
1.5 Null Hypothesis
1. Integration of HIV and AIDS care into reproductive health services does not affect the
utilization of reproductive health services.
1.6 Objectives
1.6.1 Broad Objective
1. To determine the effects of integration of HIV and AIDS care into reproductive
health services on the utilization of reproductive health services.
1.6.2 Specific Objectives
1. To determine the level utilization of reproductive health services that were offered
before integration of HIV and AIDS care into reproductive health services
2. To find out the changes in the uptake of reproductive health services following
3. To establish the effects of integration of HIV and AIDS care into reproductive
health services on the uptake of reproductive health services.
4. To determine the factors contributing to the utilization patterns of integrated
services
1.7 Significance and Anticipated Output
The AIDS epidemic is integrally linked to sexual and reproductive health. The majority
of HIV infections are sexually transmitted or associated with pregnancy, childbirth and
breastfeeding (UNFPA, 2009). Both HIV and AIDS and poor sexual and reproductive
health are driven by common root causes including poverty, gender inequality and social
marginalization of the most vulnerable populations. Responses to both health issues
should be closely linked and mutually reinforcing (UNFP A, 2009). UNFPA, along with
the rest of the international community, strongly advocate for closer linkages between
HIV and AIDS interventions and sexual and reproductive health care. This makes sense
in terms of public health benefit, economic efficiency and human rights. Integration of
services was called for at the 2005 World Summit when leaders identified universal
access to reproductive health as a combating HIV and AIDS and achieving the other
Millennium Development Goals (UNfP A, 2009).
The integration between reproductive health and AIDS programme should lead to a
number of important public health benefits:
• Improved access to, and uptake of key services.
• Reduced A}DS- related stigma and discrimination.
• Improved coverage of under served and marginalized populations such as injecting
drug users, sex workers or homosexuals.
• Greater support for dual protection against unintended pregnancy and STls
including HIV, for those in need, especialiy young people.
• Improved quality of care.
• Enhanced programme effectiveness and efficiency.
The investigation of effects of integration of HIV and AIDS Care into reproductive health
service on the utilization of reproductive health services is becoming increasingly
important. This is as a result of the shift of focus at the beginning of 21st century from
vertical programmes to integrated programmes. The shift in focus has led to many types
of integrations being explored and or implemented. Integrated services would be
convenient, perhaps a lifesaver to individuals who have limited access to sexual and
reproductive health care (UNFP A, 2009).
In Sub-Saharan Africa, where the HIV and AIDS epidemic is widespread, almost 61%of
women were living with HIV in 2007 (UNAIDS 2007). Majority of whom have unmet
need for effective contraceptive and consequently a high proportion of unintended
pregnancies. Many of these women do not know their HIV status, have limited access to
information and services thus risk to passing the virus to their children (UNFPA, 2009).
Under these circumstances, access to even a minimal integrated package of care can
AIDS in addition to preventing HIV transmission to their children. Integration of HIV
and AIDS care and reproductive health services is one of many steps called for by the
Maputo Call to Action 'Plan'of Action on Sexual and Reproductive Health and Rights'
(UNFPA, 2009). Therefore the integration of HIV and AIDS care and reproductive health
services in Thika and Nairobi-West Family Care Medical clinic can help in reversing the
feminization of HIV and AIDS in the Kenya. More so the integration will aid in meeting
the unmet reproductive needs of women.
1.8 Delimitation and Limitation of the Study
1.8.1 Limitations of the Study
The study was limited to only two of the four Family Care Clinics implementing the
integration due to a scarcity of resources. In addition, due to limited time the
retrospective and prospective study of services following integration was carried for a
short period of time as such yielding short term effects only. Respondents thought they
would be given a token of participation since there was a parallel study taking place in
one of the clinics where by participants were rewarded financially. As such they had to be
convinced to participate. Lastly there was a degree of non response from the respondents.
1.8.2 Delimitations of the Study.
The study focused on people both in the urban and rural set-ups of Nairobi-West and
Thika Town and their vicinities respectively. The findings were limited to Nairobi
Province and Thika District. The study established the short term effects of integration
-only. As such the findings should be generalized selectively in studies establishing long
term effects of integration.
1.9 Basic Assumptions of the Study
The following assumptions were made to serve as a guideline for the study;
• Integration of service had been fully implemented and yielded effects on the
existing reproductive health services, service providers and clients.
• Both the service providers and clients were aware that integration had been
implemented.
• Clients who utilized the services were aware of the effects of integration on
1.9 Conceptual Framework
Independent variable
Components of
comprehensive HIV/AIDS
Dependent variables
Reproductive health services
Expected outcome
.:.
VCT.:.
Family planning.:.
PMTCT.:.
Well baby clinicImproved
.:.
Ante-retrieval.:.
Well-womantherapy clinic access to and
.:.
Psychological care.:.
Antenatal clinic ---+uptake of key
.:.
Home based care.:.
Post-natal clinic.:.
Nutritional.:.
Post-Abortal care HIV/AIDS &counseling
.:.
Management ofReproductive
.:.
Management of STI'sopportunistic
.:.
Management of Health infections infertilityServices
Figure 1.0
Key
• -+Point of formation of Linkages and Interactions between the two sets of
services once the integration is fully implemented
Adopted from www. Unfpa.org/icpd/1 O/docs/hiv-aids-rh-call-commitment.doc
CHAPTER TWO
LITERA TURE REVIEW
2.1 Introduction
As the spread of HIV and AIDS has.spiraled into a pandemic, funds have been poured
into vertically structured efforts to combat the disease. HIV and AIDS is primarily a
sexually transmitted disease, separating prevention, care and treatment from reproductive
health context hampers long term prevention efforts and solution to reproductive health
issues related to HIV and AIDS. Hence the need for the integration of the two services to
counteract this (Moloney et al, 2003).
2.2 Reproductive Health Services
Reproductive health is a state of complete physical, mental and social well- being and not
merely the absence of disease or infirmity in all matters relating to the reproductive
system and to its functions and processes (Jay and Sharifar, 1994). Reproductive health
therefore implies that people are able to have a satisfying and safe sex life and that they
have the capability to reproduce and the freedom to decide if, when and how often to do
so. Implicit in this last condition are the rights of men and women to be informed and
have access to safe, effective, affordable and acceptable methods of family planning of
their choice, as well as other methods of their choice for regulation of fertility which are
not against the law. More so the rights of access to appropriate health care services that
will enable women go through pregnancy, child birth and provide couples with the best
chance of having a healthy infant (Jay and Sharifar, 1994). In line with the above
services that contribute to reproductive health and wellbeing by preventing and solving
reproductive health problems. It also includes sexual health, the purpose of which is the
enhancement of life and personal relations and not merely counseling and care related to
reproductive and sexually transmitted diseases (Jay and Sharifar, 1994). Although the
priority for specific reproductive health services will differ from country to country, the
following are the basic components of reproductive health; family planning counseling,
information, education and services, prevention and treatment of reproductive tract
infections including sexually transmitted infection, prenatal care, delivery, postnatal care
including breastfeeding and infant and women's health care, prevention and appropriate
treatment of infertility, prevention of abortion and post-abortal care and gynecological
services for women (Jay and Shari far, 1994).
According to World Bank, in the year 1993, about a third of the total disease burden in
women in developing countries is linked to health problems related to pregnancy, child
birth, abortion HIV/AIDS and reproductive tract infections. In addition problems such as
FGM malnutrition, unregulated fertility, osteoporosis and prolepses contribute to
women's ill health in their life cycle (Jay and Sharifar, 1994).
2.3 Care for People Living With HIV and AIDS
Treatment and care for HIV and AIDS consists of a number of different elements apart
from ARVs and indeed should be provided before ARVs are available. The care must be
comprehensive and continuous and not simply restricted to treatment (National
with not only physical but also social, psychological, emotional and spiritual care
(National AIDS/STD Control Program, 2005). Such comprehensive care encourages
disclosure of status, thus helping prevent on-going transmission, promote positive living,
promote good nutrition, encourage living a healthy lifestyle, manages opportunistic
infections and sexually transmitted infections medically, provides treatment with
antiretroviral therapy and lastly provide home-based care and end of life support
(National AIDS/STD Control Program, 2005). Home based care is the care of people
infected and affected by HIV and AIDS within the home and community, serving as a
link between hospital or health facility and the client' home through family participation
and community involvement (National AIDS/STD Control Program, 2005).
In Kenya, home based care is community based with most care provided by community
health workers, volunteers supported by clinicians, nurses, and spiritual counselors.
Quality home-based care has four main components; clinical care which entails early
diagnosis, prescribes rational treatment and plans for follow-up care of HIV related
illnesses, nursing care which promotes maintaining good health, hygiene and nutrition,
counseling and psycho spiritual care that helps reduce stress and anxiety, promotes
positive living and helps make informed decisions on testing for HIV, changing their
behavior and planning for the future and lastly social support which provides
information about support groups and welfare services and refers patient to them,
provides legal advice for individuals and families, including surviving family members
The most important entry point into the continuum of care is voluntary HIV counseling
and testing. The VCT is an important patt of any national prevention program. It is
widely recognized that individuals living with HIV and AIDS who are aware of their
status are less likely to transmit HIV infection to others and that through testing they can
be directed to care and support that can help them stay alive (UNAIDS, 2006). VCT also
provides benefit for those who test negative in that their behavior may change as a result
of the testing. The provision of VCT has become easier, cheaper and more effective as a
result of the introduction of the rapid HIV testing, which allows individuals to be tested
and get the results the same day (UNAIDS 2006). The testing and counseling is now
available through VCT, PMTCT, diagnostic testing and counseling in tuberculosis clinics
as well as out and in-patients department.
2.4 Integration of Reproductive Health Services and HIV and AIDS Care
Integration in the health sector has been defmed as offering two or more services at the
same facility during the same operating hours, with the provider of one service actively
encouraging clients to consider using the other services dwi.ng the same visit in order to
make those services more convenient and efficient (Foreit et al., 2002). In practice
integrated services are not always offered under one roof, but in such instances strong
referral systems are required to ensure that clients receive the high quality services that
they deserve (Myaya, 2004). Where services are currently integrated some HIV and
When the HIV and AIDS epidemic emerged in 1980s, family planning organizations
responded with some of the first HIV and AIDS prevention projects in the developing
world. Yet a review of the contributions of sexual and reproductive health services to
HIV and AIDS, conducted in 2003 for the World Health Organization found that
integrating HIV and AIDS services had not yet been implemented effectively except in a
few cases (Askew and Berer, 2003). Still it would be premature to conclude that
integration does not work. Much has been learnt, moreover from implementing various
strategies designed to achieve integration. Such strategies include diagnosis and treatment
of STIs, sexual risk reduction counseling, condom promotion and HIV voluntary
counseling and testing (Kathleen, 2004).
2.4.1 Integration of STI / HIV Prevention Messages into Family Planning.
Incorporating STIIHIV prevention messages in family planning services has been an
appealing strategy because family planning programs attract clients who often do not
access HIV programs services. Family planning staff can be trained to provide basic HIV
and AIDS prevention information and run an infrastructure of clinics and community
based programs for service delivery (Askew and Berer, 2003). However providing
STIIHIV prevention services through family planning programs is problematic because
these programs usually do not reach those at the greatest risk of HIV and AIDS infection,
including men, youth and single women (Lush et al., 1999). Even when married women
are among those at the highest risk of HIV and AIDS, they often do not have the powers
to protect themselves by either abstaining from sex insist on fidelity or condom use by
Family planning programs providers are often reluctant to offer HIV and AIDS services.
Many are concerned about the potential negative effects of HIV and AIDS
responsibilities and overall quality of services. Others fear occupational exposure to HIV
and AIDS or worry that providing the services will discredit family planning programs
(Maggwa and Ominde, 2003). Nevertheless providers have an obligation to their clients
to do what they can, wherever family planning services are offered, providers should be
equipped to counsel clients about STI's and HIV and AIDS and refer them for services
(Maggwa and Ominde, 2003).
2.4.2 Integration of Family Planning into HIV andAIDS Services.
Integration is also starting to move in the opposite direction. Pilot efforts have begun to
add family planning counseling and services to HIV services such as VCT and PMTCT.
VCT centers are emerging as primary targets for integration. Research from Africa and
the Caribbean shows that such integration is feasible and acceptable and large scale
integration efforts are being launched and expanded there (Strachan
et al.,
2004). Inresponse to research demonstrating the feasibility of integrating family planning into
VCT centers in Kenya, the government has moved quickly to develop and begin
implementing a strategy for family planning services at all VCT centers in the country.
Government leadership, an effective task force and stakeholder commitment have been
key to translating this important research into improved family planning and VCT
services for Kenyan clients.
The research conducted in June 2002 on the feasibility of integrating family planning into
VeT centers in Kenya suggested that it was feasible (Reynolds et al., 2003). The
feasibility research identified the opportunities, challenges for integration and to inform
the development of integration strategy. Overall, results suggested that counselor
training, referrals and contraception supply needs varied among centers. Researchers
concluded that decisions on whether to integrate services and to what extent to integrate
needed to be made at the facility level (Strachan et al., 2004).
Kenya was a promising site for integration even before the feasibility research was
conceptualized. The Ministry of Health had an ambitious program to expand veT
services. Nearly 300 VeT centers have been registered in the country and it is one of the
few countries to have developed national veT guidelines. The government also
recognized the benefits of family planning; with Kenya identified in a recent analysis as
one of six countries to mention family planning in its VeT guidelines (Strachan et al.,
2004). The VeT centers were funded through different mechanisms and because some
service providers thought they might be overburdened if family planning was introduced
into their facilities. To address these concerns the MOH established a subcommittee to
develop a strategy that could be applied to all facilities would not disrupt existing VeT
services and would not compromise the quality of either the family planning or the veT
services provided (Kenya Ministry of Health, 2004).
The subcommittee developed a strategy that identifies four levels of integration, each
and sexually transmitted infections, provision of information and counseling on
contraceptive methods that are not available at the veT centers are included in all levels.
Each progressive level requires more extensive training of VeT counselors and more
equipments and supplies. Thus the strategy recommends that VeT centers first focus on
achieving at least the first level of provision, while the fourth is viewed as a long term
goal (Kenya Ministry of Health, 2004). Tools for training current and new veT
counselors to provide family planning services have been developed and will be
combined to one comprehensive curriculum by Ministry of Health. The levels shown on
the table below differ however, in the methods that are provided on site (Kenya Ministry
of Health, 2004).
FHI is working with AMKENI and JHPIEGO to implement the first level of integration
as outlined in the strategy, into 20 proposed veT centers in two provinces in Kenya.
Operations Research will test the effectiveness, cost of implementation and lessons leamt
from this will inform activities to scale up integration throughout Kenya (Kenya Ministry
of Health, 2004).
Table 2.0 Adding Family Planning to VeT: Levels of Integration in Kenya
I
Level Services Provided
• Assessment of pregnancy and STI risks
• Information and counseling on methods
• Provision of condoms and pills
• Referral for other methods
Requiremen ts
• Minimal training of counselors to provide services • Availability of job aids,
condoms and pills
• Time and space to provide services
II • All services in level I • Provision of injectables
• All requirements in level I • Counselors trained to provide
injectables
• Adequate infection control procedures in place
• Additional equipment and supplies
III • All services provided in level II
• Provision of IDDS
• All requirements in level II • Counselors trained to provide
IUDS
• Additional equipment and supplies
IV • All services provided in level III
• Provision of full range of methods
• All requirements in level III • Medical doctor to perform
surgical procedures
• Additional equipments and supplies
Source: Kenya Ministry of Health. Strategy for the Integration of HIV Voluntary counseling and Testing Services and Family Planning Services. Nairobi, Kenya: National AIDS and STD Control Program and Division of Reproductive Health, 2004.
In 2006, in promoting an integrated approach to PMTCT in Sub-Saharan Africa, WHO
named Uganda a learning site where different ways of providing comprehensive PMTCT
services can be tested and evaluated (FBI, 2007). The integration was as a result of
findings of a research carried out in rural parts of the country by the US. Centre for
Disease Control and Prevention in Uganda. Nine out of 10 pregnancies among
HIV-positive women were unintended. These preliminary findings, based on 86 pregnancies
among 618 women in Tororo, Uganda, highlight the need to integrate the country's
family planning and HIV and AIDS services. Providing such services can help
HIV-positive women avoid unintended pregnancies and contribute to preventing PMTCT
(FHI, 2007).
The MOH of Uganda began integrating family planning, maternal and child health and
HIV and AIDS services in 2005. The technical support from WHO gives the Ministry an
opportunity to accelerate these efforts while strengthening the evidence base for
integration. A working group of reproductive health and HIV and AIDS expert has laid a
foundation for an integrated approach in Uganda. Its members incorporated information
about how to provide and evaluate HIV and AIDS services into family planning tools and
guidelines. They also developed training materials and service delivery guidelines, which
were used to train a central team of master trainers. Non-medical health workers will be
trained to provide certain community based services including HIV testing and
counseling (FBI, 2007).
This kind of integration aims at providing VCT and PMTCT clients, regardless of their
HIV status, the opportunity to avoid unintended pregnancies. For HIV infected women
ready access to family planning can help avert unintended pregnancies and thus reduce
the number of HIV infected infants. ART programs are also ideal sites for linking HIV
and AIDS and reproductive health services, such as gynecological care and screening for
gender-based violence. In Ghana, Engender Health and FHI are integrating family
planning interventions in ARV treatment and care programs (Perchal and Farrel, 2006).
Also being explored is the integration of family planning into care and support for
PLWHA. An FHI study was assessing integration of family planning promotion into the
services provided by volunteer care givers in a home-based care program for PLWHA in
South Africa and the results are yet to be published (USAID, 2003). Managers of a
similar program in Kenya ,the HIV and AIDS care support and prevention (COPHIA)
program carried out by US based Pathfinder International, decided that it was important
to train community healthy workers in family planning services and HIV prevention so
that they could respond to the reproductive health needs of clients and family members.
2.4.3 Integration of
mv
and AIDS Services outside Clinical SettingHIV and AIDS services or preventive health messages can also be integrated outside
clinical settings through interventions such as behavior change communication, peer
education, communication outreach, youth programs and social marketing (Shelton,
2004). For example in Nigeria's Lagos state, family planning counseling and referrals are
Communication Partnership, After training hot line counselors in family planning
counseling and referral in February 2004, HCP began promoting the new services
through radio advertisements, community rallies and USAID- sponsored family planning
programs (Shelton, 2004). In addition partners such as FBOs and CBOs can be crucial in
the integration of services. At the same time playa part in a successful referral systems.
Many CBOs represent the only accessible service point for integration at the community
levels and they need support in their efforts to deliver integrated services (Moloney et al,
2003). In Ethiopia, the main entry points of integrated services are the community-based
reproductive health agents who in their role in reproductive health services not only
promote family planning but also provide PLWHA's with HIV and AIDS and OVC'S
with home-based care kits, provide' referrals for HIV and AIDS services and spread
preventive messages (Kane and Colton, 2005).
Zimbabwe has followed suit and integrated family planning and HIV and AIDS services
at the community level. In primary health care clinics throughout the country, a single
health care provider is expected to offer not only basic services such as immunizations,
but also family planning services and information about HIV prevention. Some also
provide the antiretroviral drug neverapine for prevention of mother to child transmission
of HIV and AIDS (FHI, 2007). At other levels of the country's health system, however,
family planning and HIV and AIDS services are separate, vertical programs. Providers
countrywide are uncertain about how to advise HIV-positive women and couples about
family planning, which is a primary strategy for reducing HIV-infected births. Despite
services, family planning services have not been well integrated into PMTCT and remain
the program's weak link as such a change at the national level is required to strengthen
this link ( FHI, 2007).
The integration initiative began with an assessment of the family planning content of
national HIV and AIDS and reproductive health policies, guidelines and training
materials in June 2006. Eight of the 14 documents mentioned family planning, but none
provided guidance on how to integrate services. By October 2006, the assessment's
recommendations for strengthening or adding family planning content had been
incorporated into the national strategy on PMTCT and pediatric HIV and AIDS
prevention, care and treatment. Contraception for women and couples with HIVIAIDS, a training module developed by FHI and Engender Health, was adapted for inclusion in the
national PMTCT training curriculum to strengthen providers' ability to provide family
planning services (FHI, 2007). The module was also to train HIV and AIDS counselors
supported by a partnership project. These efforts and most other integration work in Zimbabwe have introduced family planning into HIV/AIDS services. Recently, however,
the Zimbabwe National Family Planning Council (ZNFPC) together with partnership
project trained family planning counselors to provide HIV and AIDS services. The
training covered; family planning and other 'positive living' issues such as diet, exercise,
medical care and psychological and social support.
The Ministry of Health and Child Welfare of Zimbabwe in conjunction with partnership
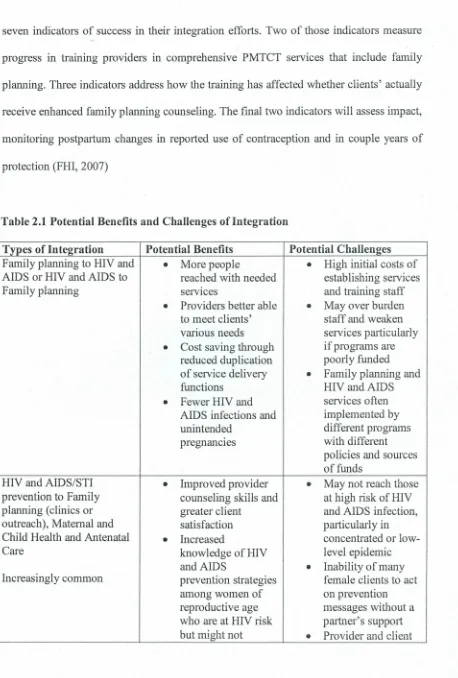
seven indicators of success in their integration efforts. Two of those indicators measure
progress in training providers in comprehensive PMTCT services that include family
planning. Three indicators address how the training has affected whether clients' actually
receive enhanced family planning counseling. The final two indicators will assess impact,
monitoring postpartum changes in reported use of contraception and in couple years of
protection (FHI, 2007)
Table 2.1 Potential Benefits and Challenges ofIntegration
Types of Integration Potential Benefits Potential Challenges
Family planning to HIV and
•
More people•
High initial costs ofAIDS or HIV and AIDS to reached with needed establishing services
Family planning services and training staff
•
Providers better able•
May over burdento meet clients' staff and weaken
various needs services particularly
•
Cost saving through ifprograms arereduced duplication poorly funded
of service delivery
•
Family planning andfunctions HIVandAIDS
•
Fewer HIV and services oftenAIDS infections and implemented by
unintended different programs
pregnancies with different
policies and sources of funds
HIV and AIDS/STI
•
Improved provider•
May not reach thoseprevention to Family counseling skills and at high risk of HIV
planning (clinics or greater client and AIDS infection,
outreach), Maternal and satisfaction particularly in
Child Health and Antenatal
•
Increased concentrated orlow-Care knowledge of HIV level epidemic
and AIDS
•
Inability of manyIncreasingly common prevention strategies female clients to act
among women of on prevention
reproductive age messages without a
who are at HIV risk partner's support
otherwise receive bias against
-HIVandAIDS condoms
information and
•
Difficult for manycounseling Family planning
•
Many HIV-infected programs to assume births averted by new tasks due to preventing HIV reduced funding and infection among weak systemswomen of
•
Need to train reproductive age providers to talkabout sexual behavior and relationships VCT to Family planning or
•
Increased access to•
May not be cost-Antenatal care and use ofVCT effective if mostservices clients are not at risk
Limited but increasing
•
Reduce stigma of HIV and AIDSassociated with HIV
•
Possible provider and AIDS reluctant to offer•
Increased awareness HIVandAIDSof healthy sexual services due to behavior stigma associated
•
More targeted with HIV and AIDS family planning and fears ofcounseling based on occupational
HIV serostatus exposure to the virus
•
Many HIV-infected•
For VCT, special births averted by skills and equipment identifying infected plus strong systemswomen, then for supervision, helping those who monitoring, logistics are not pregnant management and
avoid unintended referrals for follow-pregnancies or up care needed refening those who
are pregnant for antiretroviral drug therapy
Family planning to VCT or
•
Expanded access to•
For family planning,Antenatal Care ( usual site famil y planning for special provider
of PMTCT services) all VCT clients, skills, equipment,
Limited, but increasing youth aswell as strong
•
Increased systems forknowledge of dual supervision,
protection strategies monitoring logistics to prevent both management and unintended referrals for follo w-pregnancies and up care needed HIV and AIDS 8 Unique
"infection contraception
•
Greater opportunity consideration for for clients, HIV infected regardless ofHIV women serostatus to avoidinitial or subsequent unintended
pregnancy
•
Can greatlycontribute to averting HIV-infected births among HIV -infected women
STI care to Family
•
Reduced risk of HIV•
Misdiagnosis moreplanning, Maternal and and AIDS infections likely since family Child Health or Antenatal through STI planning clients may
Care prevention, not be at high STI detection and risk
Emphasis decreasing treatment
•
Current lack of•
Fewer cases of simple, effectivesecondary infertility, technologies to pelvic inflammatory diagnose and treat disease and negative STI's in
pregnancy outcome asymptomatic arising from women orwomen untreated with vaginal reproductive tract discharge
infections/STI's in
•
When diagnosis iswomen uncertain, partner notification not
feasible; women treated
syndromically at
risk ofreinfection
Regardless of when, where and how family planning and HIV and AIDS services are
integrated, family planning remains one of the most effective ways to enhance the we
ll-being of women and their families. By enabling women to avoid unintended pregnancies
and by reducing the risks associated with age at pregnancy, too many pregnancies, or
pregnancies spaced too closely together, family planning prevents about 2.7 million
infants deaths and 215 000 pregnancy-related deaths in the developing world each year
These benefits of family planning may be particularly important for HIV-infected
women, whose health is already compromised and for their children (Singh et al, 2003).
2
.
5 Factors to consider when Integrating HIV and AIDS and Rep
r
oducti
v
e
H
ealth
Serv
i
ces
According to the new technical guidelines from the US Agency for International
Development (USAID), integration is most appropriate in countries where the epidemic
is generalized. In these countries the number of people who need reproductive health
services and HIV and AIDS services are likely to be high (USAID, 2003). Family
planning and HIV and AIDS services needs intersect in a growing number of countries.
In 2000,55 countries had generalized epidemics up from 25 countries in 1990 (Walker et
al, 2001). In contrast in countries where the epidemic is low level or concentrated among
people at highest risk of infection, HIV and AIDS services specifically targeting those
individuals are needed. Integrating services in such settings is unlikely to be cost
-effective (USAID, 2003). Even in countries where HIV and AIDS primarily affect high
risk groups, good opportunities may exist to reach people in need HIV and AIDS or
family planning services through service integration.
Table 2.3 Appropriate Service by Type ofHIV/AIDS Epidemic
HIVIAIDS Epidemic Type Service for Type of Population
Generalized: HIV prevalence above 1% Integrated family planning and HIV and
among pregnant women. AIDS services for general population and
high-risk population.
Concentrated: HIV prevalence above 5% Family planning for general population
in at least one at risk sub population but HIV and AIDS services and possibly
below 1% among pregnant women. family planning for high-risk population.
Low level: HIV and AIDS prevalence Family planning for general population
below 5% in at risk sub-populations and HIV and AIDS services for high-risk
below I% among pregnant women population
Table 2.3 shows the appropriate service by type of HIV and AIDS epidemic adapted from
USAID. Family planning and HIV integration: Technical Guidance for USAID-suppOlted
field program.
Some reproductive health services for instance may tailor their services to reach those at
highest risks such as the youth, men and commercial sexs workers (Kathleen, 2004).
Before attempting to integrate services, program managers need to be aware of the
potential benefits and challenges confronting them and consider whether integration
make sense. The likely hood that combining the two services will be cost effective
depends on clients' need, the prevalence of HIV and AIDS in the area and the strength of
integration depends on a program's capacity, the costs and resources available to support
CHAPTER THREE
MATERIALS AND METHODS
3.1 Research Design
A longitudinal study design was employed. Records of clients utilizing the eight
study sites were reviewed. Retrospectively and prospectively for six months from the reproductive health services namely family planning, antenatal, postnatal, well-baby,
well-woman, Postabortal, management of STIs, and management of infertility from the
onset of integration. The results of the retrospective review generated the baseline data.
While the prospective review generated results that would be compared against the
'I
1 . I I
I
baseline data to assess whether the integration had affected the utilization of the
respective reproductive health services. In addition to how the integration had affected
the utilization of the respective reproductive health services. To build on the data
generated from the review of records, primary data was collected from clients seeking
reproductive health services from the study sites and to service providers working in the
same sites.
3.2 Definition and Measurement of Study Variables
The independent variable was HIV and AIDS Care that was integrated into reproductive
health services. The utilization of reproductive health services was the dependent
variable. The study used several variables within the independent variable to assess the
effects of integration on the utilization of reproductive health services. The variables
were changes in uptake of services, acceptance levels of integrated services, changes in
quality of services and awareness.
3.2.1 Changes in Uptake of Services
Uptake of services refers to the utilization of HIV and AIDS Care and reproductive health
services. It is synonymous to sought and access. The changes were measured through the
comparison of the total number of clients who utilized services before and after
integration in general. Also comparisons were drawn between the total number of clients
utilizing services from Nairobi-West and Thika Family Care Medical clinics before and
after integration. Further, comparisons were drawn between the number of clients who
utilized the respective reproductive health services in general and from Nairobi-West and
Thika Family Care Medical clinic before and after integration. The data that was used for
comparison purposes was generated through the review of monthly medical records
prospectively and retrospectively for six months after integration.
3.2.2 Acceptance of Integration
Acceptance is the willingness to adopt and utilize the services that had been integrated.
Information to assist the study to measure the acceptance of integration was collected
through questionnaires. The study population responded to questions on awareness of the
implementation of integration, their preference based the pro and cons of integrated
3.2.3 Changes in Quality of Services
Quality is the goodness of services. Rating of goodness of services as very poor, poor,
fair, good and very good was used to capture the views of clients. To measure changes in
quality, clients utilizing the services drew comparisons on four parameters of qualities of
services before and after integration. The four parameters were; waiting time before
being attended to, efficiency and number of service providers, availability of services
sought for and accuracy of information relayed to clients. Clients responded to questions
related to these parameters.
3.2.4 Awareness
Awareness is being well informed on the implementation of integration and the HIV and
AIDS services that were integrated. The awareness was measured through the study
population responding to questions on how they got informed about the integration and
the availability of HIV and AIDS care services.
3.3 Location of the Study
The study was conducted in Nairobi-West and Thika Family Care Medical clinic in
Nairobi city and Thika town respectively. The two clinics are part of the four Family
Care Medical Clinics currently integrating HIV and AIDS care into reproductive health
clinics managed by F.H.O.K.
33.1 Description of Thika Town
Thika town is a market town in Central Province, Kenya lying on the A2 road 40 km
north east of Nairobi city and on the Thika river. According to 1999 census results, the
town has a population of 88,265 people. It is externally serviced by a dual carriage way to
Nairobi city, a high way to Garissa and also a railway line. Economic activities of the
town include agriculture, food processing, tannery, textile and motor vehicle assemblies.
The Thika Family Care Medical clinic is located opposite the main bus terminus along
workshop road in the town.
3.3.2 Description of Nairobi City
Nairobi is the capital and largest city in Kenya. It is the most populous city in East Africa
with an estimated population of 3 million. It is currently the 13th largest city in Africa, In
addition, it is one of the most prominent cities in Africa politically and financially. It is
home to many companies and organizations. More over it is an established hub for
business and culture. Nairobi enjoys full administrative province and is the smallest
province in size and entirely urban. Nairobi - West Family Care Medical clinic is located along Mai -Mahiu road off Langata / Mbagathi road junction in Kibera division.
3.4 Target Population
Service providers working in integrated set-ups and clients seeking services in the same
3.5 Study Population
The study population consisted of;
• Reproductive health services offered in Nairobi-West and Thika Family clinic.
The reproductive health services of interest to the study were; antenatal, postnatal,
management of STls, postabortal care, family planning, well-woman, well-baby,
and management of infertility.
• Clients seeking reproductive health services from the two clinics. The clients were
women of the reproductive age bracket which is 15 to 49 years of age.
• Service providers working in the study areas.
3.5.1 Criteria for Inclusion
1. Clients seeking reproductive health services at the specific time of the study and
were willing to participate.
11. Service providers who were on duty at the specific time of the study in the clinics
and were willing to participate.
3.5.2 Criteria for Exclusion
1. Clients seeking reproductive health services at the specific time of the study and
were not willing to participate
11. Service providers who were on duty at specific time of the study and were not
willing to participate.
3.6 Sampling Techniques and Sample Size
3.6.1 Sampling Techniques
Nairobi-West and Thika Family Care Clinics were conveniently sampled due to their proximity to the research team. A census of all reproductive health services offered in the
study was conducted. In addition a key informant interview was canied out where all the
service providers working in the two facilities were eligible. Availability sampling was
used to select the clients who participated in the study. This involved the sampling of
clients readily available and willing to participate in the study till desired sample size was
arrived at. The study employed the availability method of sampling because the
population of interest to the study was out patient. This meant that the members of the population visited and left the clinics at their own convenient time without being
admitted into the wards.
3.6.2 Sample Size Determination for Clients
The sample size was arrived at by calculating using the standard formula as used by
Fisher et al., (1998).
Where,
N
=
Sample sizeZ= standard normal deviate (1.96) which corresponds to 95% confidence interval
q
=
1-p=
0.5d = Degree of accuracy = 0.05
D = Design effect = 1
= Thus n = 1.962 x 0.5 x 0.5 x 1
=
384The above formula is only applicable for a population that is more than 10,000. Therefore
after calculation of sample size with the above formulae, the formulae below was used
since the average monthly population of clients seeking reproductive health services in
the two clinics was 391 which was less than 10,000
nf = n
l+n
N
Where,
nf = sample size of a population less than 10,000
n = sample size arrived at using the formula as it was used by Fishers et al., (1998), for a
population greater than 10,000
n ~ the population of clients seeking reproductive health services i.e. 391: (~
nf= n
l+n
N
nf= 384 1+384
391
=
194 womenProbability proportion to sample size as shown below was used to determine the number
of clients to be interviewed in the two clinics as shown below.
Nairobi West
=
140 x 194391
69 women
Thika =251 x 194 = 125 women
391
3.7 Construction of Research Instruments
Interview schedules and self-administered questionnaires were used to collect clients'
perception towards integration. The instruments contained both open and close-ended
questions. Further the instruments were subdivided into three sections; demographic,
reproductive health services and integrated services. This was to aid in capturing the
clients' perception of integrated services. In addition a key informant interview schedule
was constructed to collect the views of service providers regarding integration.
3.8 Pilot Study
Pilot study was carried out at Phoenix Family Care Clinic along Kenyatta Avenue in
self-administered questionnaires were used to collect clients' perception on integration.
Availability sampling was used to select the clients. Key informant interviews were also
carried out to collect the service providers' views regarding integration. After the pilot
study a mini analysis was carried out to determine whether the instruments yielded the
required data. Based on the results of the mini analysis the instruments were revised
accordingly.
3.8.1 Validity
Research assistants were trained on the contents of the interview schedule and on how to
carry out an interview. The research instruments were pre-tested in the selected pilot
center.
3.8.2 Reliability
The research instruments were pre-tested in the selected pilot center. A mini analysis was done the data collected. After which the instruments were reviewed accordingly.
3.9 Data Collection
Primary and secondary data were used. Interview schedules and self-administered
questionnaires were used to collect the views of the clients regarding integration. The two
research instruments were administered to each and every client who was available and
willing to participate in the study at the time the research was happening till the desired
sample size of 194 was achieved. The literate clients filled in the self-administered
schedules with the help of a researcher. Key informant interview schedules were used to
collect service providers' views regarding integration. The information collected through
the key informant interview was used to build on the data collected through the
questionnaires and interview schedules. Records of reproductive health services utilized
by clients were reviewed retrospectively and prospectively. The review entailed
extracting the number of clients who utilized the respective reproductive health services
from the medical reports generated on a monthly basis in the study sites. Retrospective
study covered six months preceding integration while the prospective study was done for
six months from the onset of the integration.
3.10 Data Analysis
Statistical analysis was done using SPSS software. Data was edited, coded and entered.
Descriptive analysis was done to determine frequencies, percentages and means.
ANOVA was used to test whether there was a significant difference in the utilization of
reproductive services before and after integration. Chi-square was used to test clients'
perceptions and the views of service providers regarding the integration of the services.
Data was presented in graphs, pie-charts and tables.
3.11 Logistical and Ethical Considerations
Permission to carry out the study was sought from the Ethical Committee of Ministry of