Office management of minor wounds
Serge Gouin, MDCM, FRCPC, FAAP Hema Patel, MD, MSC, FRCPC, FAAP
OBJECTIVE To review office inter ventions for minor wounds not requiring sutures, such as
abrasions, bites, and lacerations.
QUALITY OF EVIDENCEMost information on minor wound management comes from descriptive
studies. Few comparative studies examine the ef fectiveness of topical antisepsis for minor wounds. Several clinical trials have demonstrated that tissue adhesives produce short- and long-term cosmetic results equivalent to those achieved with suture materials.
MAIN MESSAGESterile saline is the least toxic solution for wound irrigation. Chlorhexidine (2%)
and povidone iodine (10%) have been the most investigated antiseptic solutions. Systemic antibiotics are unnecessary for wounds unlikely to be infected. All bite wounds require special attention. Primary closure of bite wounds is indicated in certain circumstances: less than 12-hour-old nonpuncture wounds, uninfected wounds, and low-risk lesions (such as on the face). In spite of their many advantages, skin tapes should be used for low-tension wounds only. The popularity of tissue adhesives has greatly increased. Since the advent of newer products (with increased bonding strength and flexibility), adhesives are used to manage most lacerations except those in areas of high tension (eg, joints) and on mucosal surfaces.
CONCLUSIONMinor wounds not requiring sutures can be managed easily in the office.
OBJECTIFPasser en revue les interventions en cabinet pour les plaies mineures qui n’exigent pas
de sutures, comme les abrasions, les morsures et les lacérations.
QUALITÉ DES DONNÉES La majorité des renseignements sur la prise en charge des plaies
mineures proviennent d’études descriptives. Quelques études comparatives examinent l’efficacité des agents antiseptiques topiques dans le cas de plaies mineures. Plusieurs essais cliniques ont démontré que les pansements de rapprochement (stéristrips) permettaient d’obtenir des résultats cosmétiques à court et long termes semblables à ceux que produit le matériel de sutures.
PRINCIPAL MESSAGEUne solution saline stérile constitue le produit le moins toxique pour l’irrigation de la plaie. La chlorhexidine (2%) et la polyvidone iodée (10%) sont les solutions antiseptiques ayant fait l’objet d’un plus grand nombre d’études. Les antibiotiques systémiques sont inutiles pour les plaies qui ne sont pas propices à l’infection. Toutes les morsures méritent une attention particulière. Une suture primitive des blessures par morsure est indiquée dans certaines circonstances: les plaies non punctiformes de moins de 12 heures, les plaies non infectées et les lésions à faible risque (comme celles au visage). En dépit de leurs nombreux avantages, les bandages cutanés ne devraient être utilisés que pour les plaies assujetties à une faible tension. Les pansements de rapprochement sont de plus en plus populaires. Depuis l’avènement de nouveaux produits (ayant une propriété de liaison et une flexibilité accrues), les pansements de rapprochement servent à la prise en charge de la plupart des lacérations, sauf dans les régions où la tension est forte (comme les articulations) ou les surfaces muqueuses.
CONCLUSIONLes plaies mineures qui n’exigent pas de sutures peuvent aisément être traitées en
cabinet
This article has been peer reviewed.
Cet article a fait l’objet d’une évaluation externe. Can Fam Physician 2001;47:769-774.
hildren’s minor wounds are frequently assessed in their primar y caregiver’s office.1,2
For the purposes of this article, minor wounds are defined as simple wounds (such as abrasions, most bite wounds, and lacerations) that do not require sutures.
We briefly describe common minor wounds suf-fered by children and focus on evidence-based manage-ment principles. We review interventions that can be easily performed in the office. Prompt office manage-ment of minor wounds can reduce costs to the health care system, time lost by patients and their families, and patient load in already busy emergency depart-ments (EDs). With a few key supplies and skills, minor wounds can be effectively managed in the office.
In particular, we review use of cleansing agents for wound care and management of bite and puncture wounds. Finally, use of skin tapes and tissue adhe-sives are addressed.
Quality of evidence
We conducted a MEDLINE database search of the English and French literature from 1976 to 2000. MeSH headings used for the search were Wounds and injuries; Anti-infective agents, local; and Bites and stings. Tissue adhesives was used as a text word. Clinical trials and review articles were sought.
Level 1 evidence (clinical trials) distinguishes between antiseptic solutions in management of minor wounds. No studies have clearly demonstrated how cleansing intact skin affects rates of infection when patients are not treated in hospital.3,4
Furthermore, several clinical trials (level 1 evi-dence) have evaluated cosmetic outcomes following laceration repair with tissue adhesives.5-13
Tissue adhe-sives provide short- and long-term cosmetic outcomes equivalent to those achieved with suture materials.
Main message
Cleansing agents for wound care. Appropriate care of all acute traumatic wounds includes cleansing and removal of foreign material as well as débridement when necessary.2,14-17
For effective skin antisepsis, organic mat-ter (blood, pus exudates, loose crusts, dirt, etc) should be removed before an antiseptic solution is applied.
Water or normal saline are sufficient for irrigation; sometimes mechanical removal with clean gauze is appropriate.2
Cleansing reduces the bacterial inocu-lum in the wound to levels that can be managed by host defenses.2,3
Simply soaking the wound in an anti-septic solution is an inadequate substitute for the usual cleansing.18
The cleaning process should not be toxic to tissue or increase wound inflammation because this would make dealing with the bacterial load more difficult and would increase the likelihood of infection overall.
Sterile sodium chloride solution (0.9%) is pre-ferred for wound irrigation. Saline is inexpensive, has low tissue toxicity, ef fectively decreases bacterial loads, and does not increase infection rates.3,18-20
To complement saline wound irrigation, many antiseptic solutions are on the market. Antiseptic solutions are commonly used in clinical practice21
because they have been reported to reduce infection in some traumatic lacerations.22
Despite the results of many trials, whether adding antiseptic solution in wound cleaning is always necessar y for wounds remains unclear. It is important to consider the poten-tial tissue toxicity of antiseptic solutions.23
We discuss commonly used antiseptic solutions: chlorhexidine and iodine compounds.
Chlorhexidine: Chlorhexidine is a bactericidal agent with good coverage against Gram-positive and Gram-negative organisms. It also has antiviral and antifungal properties. Its main advantages are long-lasting antiseptic effect (hours) and continued effec-tiveness in the presence of soap, blood, and pus.15
No significant toxicity has been repor ted among neonates, infants, or children.24
Care should be taken to avoid contact with patients’ eyes so as to prevent serious irritation.
Chlorhexidine is available in several strengths. The 2% solution (2% aqueous base; preservative: 4% isopropyl alcohol) is appropriate for open wound sur-face disinfection and for mucous membrane disinfec-tion (mouth, nasal passages, anus, rectum, vagina, stomas). This concentration is contraindicated for irrigation of the deep tissues of open wounds because it can induce local inflammation. Chlorhexidine (0.5% in 70% isopropyl alcohol) is indicated for closed wound surface disinfection only. A weaker solution of chlorhexidine (0.05% aqueous base; preservative: 4% isopropyl alcohol) is used for irrigation of or cleaning deep wounds (traumatic or not) and for burn wounds, if an antiseptic is required.
Iodine:Many preparations on the market contain iodine. The most commonly manufactured form is a 10%
C
solution in water: povidone iodine solution (10% polyvinyl pyrrolidine complexed with 1% iodine). Povidone iodine is also available in a 7.5% concentration scrub with detergent. Surgical scrubs are not recom-mended for minor wounds because of their high tissue toxicity. Iodine compounds are bactericidal and effective against Gram-positive and Gram-negative organisms.21,25
Bacterial strains resistant to iodine solutions are unusu-al.2,25
Iodine products are recommended if patients have chlorhexidine allergy. In addition, povidone iodine 10% solution can be used for eye disinfection.
In spite of long use in preventing infection and treating wounds,25
povidone iodine has recently become less popular because of the theoretical risks of iodine toxicity and thyroid insufficiency in chil-dren.24,26,27
The association between the dose of iodine administered and thyroid dysfunction is controver-sial.26,27
Despite cytotoxicity documented by in vitro studies, results of in vivo studies suggest that povi-done iodine does not interfere with healing, especial-ly if it is used at concentrations of 1% or lower.27
Last, povidone iodine solution contains no added preserva-tive agents while chlorhexidine solutions do. Thus, contamination of povidone iodine solution is possible and care should be taken when handling bottles.
Other agents:Other agents, such as hydrogen per-oxide (3%), rubbing alcohol (isopropyl alcohol 70%), and detergents, should not be used to clean wounds because cytotoxic effects are possible2,4
and higher infection rates have been reported.28
After the wound has been cleaned, a protective dressing should be applied. For the first 24 to 48 hours, most wounds should be covered with a dry, non-adherent dressing until there is enough epithe-lialization to protect the wound from gross contami-nation.2
As well, bandages of dr y gauze absorb wound exudates to help manage copious drainage and débridement with gauze changes.29
After ward, wounds may be gently washed. Wounds should not be scrubbed or soaked.
In summary, sterile saline appears to be a reason-able choice for wound irrigation. The issue of which antiseptic solution is best remains unresolved. It is diffi-cult to recommend one agent above others while we are unsure of the balance between real or potential toxi-city of iodine products24,26
and the efficacy of chlorhexi-dine products.28
These products are similarly priced.
Prophylactic antibiotics. Most uncomplicated
wounds heal without systemic antibiotic therapy14
; clin-ical studies failed to demonstrate a lower infection rate among patients treated with prophylactic antibiotics
than among control subjects.2
Systemic antibiotics are recommended in certain situations only:
• lapse of more than 3 hours since injury; • presence of pus;
• contamination with saliva, feces, or vaginal secre-tions;
• preventing bacteremia in patients at risk for endo-carditis;
• prosthetic joint involvement;
• lymphedematous tissues involvement; and • immunocompromised hosts.14,15
For most infections of traumatic wounds, antibiotic therapy should be directed against the most common skin pathogens, Staphylococcus aureus and streptococ-ci.14
Cloxacillin and first-generation cephalosporins are appropriate as first-line therapy. If antibiotics are administered, they should be given promptly (in the first 3 hours after injury).2
Recently, application of top-ical antibiotic ointments had been proposed to help reduce infection rates and prevent scab forma-tion.2,14,23,30
So far, the effectiveness of topical antibiotic ointments in managing minor wounds has not been properly investigated.
Bite wounds. All bite wounds require special atten-tion. Even apparently minor wounds require careful exploration, because injuries that appear to be superfi-cial can overlie fractures; involve lacerated tendons, vessels, or nerves; extend into body cavities; penetrate joint spaces; or damage such structures as the eye.2,29
It is extremely important to cleanse and sponge away all visible dirt. Blind wound exploration for presumed foreign bodies is not recommended, as it can cause fur-ther tissue damage.30
The skin should be cleaned of for-eign matter to avoid permanent tattooing.2,30
Irrigation with large volumes of sterile saline with a high-pressure syringe is recommended.2
This practice markedly decreases the concentration of bacteria in contaminated wounds29
and thus lowers the infection rate.2,3
The opti-mal therapeutic balance between appropriate decontami-nation and irrigation-induced inflammation appears to be around 8 pounds per square inch (psi). This amount of pressure is most easily generated using a 30- to 35-mL syringe equipped with an 18- to 20-gauge plastic catheter or needle.2,16
The tip of the syringe should be approxi-mately 2 cm above the intact skin.3
Most wounds should be irrigated with at least 200 mL of saline.
Physicians should use plastic shield devices and protective goggles to avoid self-contamination through splashing of wound fluids.2,16
A theoretical risk of infection exists if bite wounds are sutured. Primary closure is absolutely contraindi-cated for closed-fist injuries.16
As a general r ule, wounds inflicted by humans should be initially left open.29
Primary closure is indicated in the following circumstances:
• less than 12-hour-old nonpuncture wounds to the arms and legs and less than 24-hour-old nonpunc-ture facial wounds16,29,31
; • uninfected wounds; and
• low-risk lesions, such as on the face, as these sel-dom become infected.
For all other wounds, secondary closure will reduce the chance of infection. Cosmetic appearance can always be improved at a subsequent revision of the scar. Edges of small wounds can be approximated using skin tapes. Because any foreign material in a contaminated wound increases the risk of infection, subcutaneous sutures should be used sparingly.29
Proper positioning of wounds is important; elevation of injured areas can decrease swelling.
Tetanus immunization status should be assessed as for all wounds.2
As recommended in the 2000 Red Book (Report of the Committee on Infectious Diseases of the American Academy of Pediatrics),32
clean minor wounds should be approached differently from all the other wounds (ie, those contaminated with dirt, feces, soil, and saliva; punctures; avulsions; missiles; crushing; burns; frostbite). For clean minor wounds when the patient’s immunization status is unknown or fewer than three tetanus toxoid doses have been given, tetanus-diphtheria toxoid should be given. If at least three doses have been given and it is more than 10 years since the last dose, tetanus-diphtheria toxoid should be given. For wounds that are neither clean nor minor (described above), for patients whose immunization status is unknown, or for patients who have received fewer than three tetanus toxoid doses, tetanus-diphtheria toxoid and also tetanus immunoglobulin should be provided. In these cases, it is important to offer both active and passive immunization. If at least three doses of tetanus have been given and it is more than 5 years since the last dose, tetanus-diphtheria toxoid should be given. Special risk of infection must be considered for bite wounds. The associated risk of rabies should be evaluated for animal bites. Rabies is most common in raccoons, skunks, foxes, and bats. These animals should be regarded as rabid unless the geographic area is known to be free of rabies.32
Patients who might have contracted rabies should have immediate vaccination with human diploid cell vaccine as well as immunoprophylaxis with rabies immunoglobulin.
Only when dogs and cats are rabid or suspected of being rabid should their bites be treated with imme-diate vaccination and immunoprophylaxis. The dogs or cats should be observed for 10 days. If in doubt about the prevalence of rabies in an area, contact the public health department. Human bites require con-sideration of hepatitis B, herpes simplex, and human immunodeficiency virus transmission.2
Follow-up evaluation should be done within 48 hours to assess for signs of infection and also to reevaluate wounds that were initially left open to deter-mine whether delayed primary closure would be appro-priate.29
Infected wounds usually have 5 mm or more of redness that is painful or tender to touch, fever, erythe-matous streaking of the skin, or wound swelling; occa-sionally, pus can be expressed from the wound.33
Prophylactic use of antibiotics for bite wounds is controversial. Reported rates of infection after bites are as high as 50%.14,29
Currently, antibiotics are not given routinely.29
Previous clinical trials did not con-clusively show that prophylactic antibiotics reduce infections from bite wounds.2
For mild injuries with skin abrasion only, antibiotics are unnecessar y. Systemic antibiotics are indicated for bite wounds if wounds are severe with edema or crush injuries; if skin was punctured (especially if bone, tendon sheath, or joints were penetrated)31
; if bites were to the face, hand, foot, or genitals; if the patient has asplenia; and if the host is immunocompromised. A recent prospective study of infected wounds sec-ondary to dog and cat bites confirmed that infected dog and cat bites have a complex microbiologic mix of aer-obes and anaeraer-obes (median of five bacterial isolates per culture).1Pasteurella
species were the most com-mon isolates, but other comcom-mon aerobes included streptococci, staphylococci, moxarella, and neisseriae. Therefore, if antibiotics are prescribed, a β-lactam antibiotic with a β-lactamase inhibitor is appropriate.29
The oral antimicrobial of choice is amoxicillin–clavulanic acid. If patients are allergic to penicillin, trimethoprim-sulfamethoxazole, clindamycin, or a cephalosporin (pos-sibility of cross-reactivity) is appropriate. A duration of 2 or 3 days only is recommended, especially if the antibiotic is started less than 8 hours after the wound is inflicted. If parenteral antibiotics are required, the first-line choice is ampicillin-sulbactam.32
For penicillin-allergic patients, cefotaxime or ceftriaxone and clin-damycin or metronidazole may be substituted.
Skin tapes. Skin tapes (Steri-Strips) are ideal for wounds with low tension only (eg, abrasions, simple lacerations).2
of the wound is achieved and the surrounding skin is dr y.2
Skin tapes have many advantages: low tissue reactivity, low infection rates, rapidity and ease of application, patient comfort, low cost, no risk of nee-dle injury, and no return visit for suture removal is required. Disadvantages include low tensile strength, high rate of dehiscence, cannot be used in hair y areas, and the wound must remain dry for 2 days. As well, tapes are not recommended over areas of high motion (eg, joints).2
Application of skin tapes can be reinforced with ben-zoin tincture to prevent detachment. A dry dressing may be placed over skin tapes for 2 days. Skin tapes usually spontaneously detach within 7 days. They can be manually removed after that time if necessary.
Tissue adhesives.Cyanoacr ylate tissue adhesives have gained in popularity over the last decade for man-agement of pediatric traumatic wounds. Many random-ized clinical trials involving children5-13
and adults demonstrate that tissue adhesives offer long-term cos-metic outcomes as good as those with sutures. Overall, rates of wound infection and dehiscence are similar for both tissue adhesives and sutures.
Tissue adhesives offer many advantages: rapidity of application, patient comfort, resistance to bacterial growth, no need for removal, low cost, and no risk of needle-stick injury.12
These products also have shown no toxicity when applied topically for skin closure.12
They polymerize via an exothermic reaction in the presence of skin moisture or tissue fluid. Therefore, a strong bond is formed with the skin.12
In Canada, many products are available, including n-butyl 2-cyanoacr ylate and 2-octyl cyanoacr ylate. Recent emphasis is on the creation of single-use packages. To alleviate costs, many emergency departments use single packages on many patients. This practice is probably acceptable for infectious risk exposure as long as the applicator tip is changed for each patient. The Canadian Paediatric Society rec-ommends use of n-butyl 2-cyanoacrylate products in the following situations34
: lacerations less than 4 cm, no gaping wound edges more than 0.5 cm, and low-tension wound location. Scalp lacerations may also be repaired with tissue adhesive. Hair should be trimmed around the laceration.
Several 2-octyl cyanoacrylate products (Dermabond from Ethicon Inc in Somerville, NJ) have recently been introduced in Canada. These products have four times the bonding strength of older products.12
As well, 2-octyl cyanoacrylate products offer increased wound flexibility. These advantages make these compounds
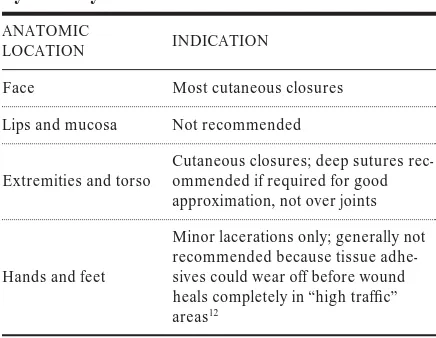
useful for long lacerations. Not surprisingly, 2-octyl cyanoacrylate products are three to four times more expensive than n-butyl 2-cyanoacrylate ones. Specific indications for use are summarized in Table 1.12
Tissue adhesives have not been studied for ani-mal or human bite wounds, stellate crush wounds, or wounds crossing the mucocutaneous junction.12
Some general guidelines of application exist for all tissue adhesives. They should be used topically only. Hemostasis of the wound should be obtained first. Once the tissue adhesive is applied, wound edges should be held together for at least 30 s. It is important to avoid excess glue and to avoid placing adhesive in the wound or between the margins.34
As the exothermic reaction occurs, children12,34
might feel the heat as a slight burning sensation. Wound stability could be reinforced with skin tapes once the tissue adhesive has dried (after 30 s). Caution should be used around the eyelids to avoid eye con-tact. If the eyelids are “glued” together, petrolatum products can be used to remove excess material. Excess glue can be carefully peeled off with forceps, if necessary.
Follow-up care for these wounds is similar to that for wounds closed by other methods. The wound should remain dry for 2 days.12
Dressings (if provid-ed) can be removed after 2 days. After 48 hours, patients may shower but should avoid soaking or scrubbing the area. The tissue adhesive will disap-pear in 7 to 14 days.
Conclusion
This brief overview addresses management of minor wounds in the office. Careful irrigation with sterile saline is important for all wounds. Now that skin tapes
ANATOMIC
LOCATION INDICATION
Face Most cutaneous closures
Lips and mucosa Not recommended
Extremities and torso
Cutaneous closures; deep sutures rec-ommended if required for good approximation, not over joints
Hands and feet
Minor lacerations only; generally not recommended because tissue adhe-sives could wear off before wound heals completely in “high traffic” areas12
Table 1.Indications for use of octyl
and tissue adhesives are available, many wounds can be treated effectively without sutures.
Competing interests None declared
Correspondence to:Dr Serge Gouin, Assistant Professor, Division of Emergency Medicine, Department of Pediatrics, Sainte-Justine Hospital, 3175 Côte-Sainte-Catherine, Montreal, QC H3T 1C5; telephone (514) 345-4931, extension 3498; fax (514) 345-4965; e-mail sergegouin@aol.com
References
1. Talan DA, Citron DM, Abrahamian FM, Moran GJ, Goldstein EJ. Bacteriologic analysis of infected dog and cat bites. N Engl J Med 1999;340(2):85-92. 2. Barkin RM, Caputo GL, Jaffe DM, Knapp JF, Schafermeyer RW, Seidel JS, et al.
Pediatric emergency medicine, concepts and clinical practice. 2nded. St Louis, Mo:
Mosby; 1997. chap 32-33, p. 439-75.
3. Chisholm CD. Wound evaluation and cleansing. Emerg Clin North Am 1992;10(4):665-72. 4. Niedner R. Cytotoxicity and sensitization of povidone-iodine and other frequently
used anti-infective agents. Dermatology 1997;195(Suppl 2):89-92.
5. Quinn JV, Wells G, Sutcliffe T, Jarmuske M, Maw J, Stiell IG, et al. Tissue adhesive versus suture wound repair at 1 year: randomized clinical trial correlating early, 3-month, and 1-year cosmetic outcome. Ann Emerg Med 1998;32(6):645-9. 6. Bruns TB, Robinson BS, Smith RJ, Kile DL, Davis TP, Sullivan KM, et al. A new
tissue adhesive for laceration repair in children. J Pediatr 1998;132(6):1067-70. 7. Singer AJ, Hollander JE, Valentine SM, Turque TW, McCuskey CF, Quinn JV.
Prospective, randomized, controlled trial of tissue adhesive (2-octylcyanoacrylate) vs stan-dard wound closure techniques for laceration repair. Acad Emerg Med 1998;5(2):94-9. 8. Quinn JV, Wells G, Sutcliffe T, Jarmusske M, Maw J, Stiell IG, et al. A randomized
trial comparing octylcyanoacrylate tissue adhesive and sutures in the management of lacerations. JAMA 1997;277(19):1527-30.
9. Simon HK, McLario DJ, Bruns TB, Zempsky WT, Wood RJ, Sullivan KM. Long-term appearance of lacerations repaired using a tissue adhesive. Pediatrics 1997;99(2):193-5.
10. Bruns TB, Simon HK, McLario DJ, Sullivan KM, Wood RJ, Anand KJS. Laceration repair using a tissue adhesive in a children’s emergency department. Pediatrics1996;98(4):673-5.
11. Quinn JV, Drzewiecki A, Li MM, Stiell IG, Sutcliffe T, Elmslie TJ, et al. A random-ized, controlled trial comparing a tissue adhesive with suturing in the repair of pediatric facial lacerations. Ann Emerg Med 1993;22(7):23-7.
12. Osmond MH. Pediatric wound management: the role of tissue adhesives. Pediatr Emerg Care1999;15(2):137-40.
13. Singer AJ, Hollander JE, Quinn JV. Evaluation and management of traumatic lac-erations. N Engl J Med 1997;337(16):1142-8.
14. Eron LJ. Targeting lurking pathogens in acute traumatic and chronic wounds. J Emerg Med1999;17(1):189-95.
15. Henretig FM, King C. Textbook of pediatric emergency procedures. Baltimore, Md: Williams & Wilkins; 1997. chaps 7,110, p. 43-9,1125-39.
16. Dieckman RA, Fiser DH, Selbst SM. Pediatric emergency and critical care proce-dures. St Louis, Mo: Mosby; 1997. chaps 131-3, p. 669-89.
17. Fleischer GR, Ludwig S, Henvetig FM, Ruddy RM, Silverman BK. Textbook of pediatric emergency medicine. 3rded. Philadelphia, Pa: Williams & Wilkins; 1993.
chap 110, p. 1288-97.
18. Lammers RL, Fourre M, Callaham ML, Boone T. Effect of povidone-iodine and soak-ing on bacterial counts in acute, traumatic, contaminated wounds. Ann Emerg Med 1990;19(6):709-14.
19. Dire DJ, Welsh AP. A comparison of wound irrigation solutions used in the emer-gency department. Ann Emerg Med 1990;19(6):704-8.
20. Badia JM, Torres JM, Tur C, Sitges-Serra A. Saline wound irrigation reduces the postoperative infection rate in guinea pigs. J Surg Res 1996;63(2):457-9. 21. Kunisada T, Yamada K, Oda S, Hara O. Investigation on the efficacy of
povidone-iodine against antiseptic-resistant species. Dermatology 1997;195(Suppl 2):14-8. 22. Gravett A, Sterner S, Clinton JE, Ruiz E. A trial of povidone-iodine in the
preven-tion of infecpreven-tion in sutured lacerapreven-tions. Ann Emerg Med 1987;16(2):167-71. 23. Williford PM. Opportunities for mupirocin calcium cream in the emergency
department. J Emerg Med 1999;17(1):213-20.
24. Lacour JP, Castanet J, Boutte P, Ortonne JP. Umbilical cord care in the neonates: a survey and recommendations. Arch Pediatr 1999;6:631-4.
25. Fleischer W, Reimer K. Povidone-iodine in antisepsis; state of the art. Dermatology1997;195(Suppl 2):3-9.
26. Linder N, Davidovitch N, Reichman B, Kuint J, Lubin D, Meyerovitch J, et al. Topical iodine-containing antiseptics and subclinical hypothyroidism in preterm infants. J Pediatr 1997;131:434-9.
27. Rodeheaver G, Bellamy W, Kody M, Spatafora G, Fitton L, Leyden K, et al. Bactericidal activity and toxicity of iodine-containing solutions in wounds. Arch Surg1982;117:181-6.
28. Harkavy KL. A topical topic; toxicity of antiseptics? J Pediatr 1998;133:309-10.
29. Fleisher GR. The management of bite wounds [editorial comments]. N Engl J Med1999;340(2):138-40.
30. Bikowski J. Secondarily infected wounds and dermatoses: a diagnosis and treat-ment guide. J Emerg Med 1999;17(1):197-206.
31. Baldwin G, Colbourne M. Puncture wounds. Pediatr Rev 1999;20(1):21-3. 32. Committee on Infectious Diseases, American Academy of Pediatrics. 2000 Red
Book, Report of the Committee on Infectious Diseases, American Academy of Pediatrics. 25thed. Elk Grove Village, Ill: American Academy of Pediatrics; 2000.
33. Laberge JM. Trucs et conseils pour traiter les lacérations chez le jeune enfant. Le clinicien1997;Oct:67-82.
34. Nijssen-Jordan C. Skin glue; emergency medicine practice points. Pediatr Child Health1997;2(3):192.
...
Editor’s key points• Wound cleansing and débridement are the most important first steps in management; sterile saline is best.
• If antiseptic solutions are used, chlorhexidine (2%) and povidone iodine (10%) solutions have been most investigated; hydrogen peroxide, rubbing alcohol, and detergents cause tissue damage and higher infection rates.
• In general, prophylactic systemic antibiotics are unnecessary except in some higher-risk cases; top-ical antibiotics have not been shown to aid healing. • Bite wounds need special attention; most should be
closed.
• Skin tapes are useful for low-tension wounds; tis-sue adhesives are gaining in popularity, especially for children’s wounds.
Points de repère du rédacteur
• Le nettoyage et le débridement des plaies représentent les premières étapes les plus impor-tantes dans leur prise en charge; la solution saline est le produit privilégié.
• Si on a recours à des solutions antiseptiques, la chlorhexidine (2%) et la polyvidone iodée (10%) ont fait l’objet d’un plus grand nombre d’études; le peroxyde d’hydrogène, l’alcool à friction et les détergents peuvent endommager les tissus et amener des taux plus élevés d’infection.
• En général, les antibiotiques systémiques prophy-lactiques sont inutiles, sauf dans les cas à risque élevé; il n’a pas été démontré que les antibiotiques topiques aidaient à la guérison.
• Les morsures requièrent une attention particulière; la plupart devraient être refermées.