Original Article
Clinical characteristics of malignant
ovarian germ cell tumors
Na Zhang1, Jianguo Zhao1, Yue Wang2, Pengpeng Qu1
Departments of 1Gynecologic Oncology, 2Obstetrics, Tianjin Central Hospital of Gynecology Obstetrics, Tianjin,
China
Received June 16, 2016; Accepted April 20, 2017; Epub July 15, 2017; Published July 30, 2017
Abstract: This study was aimed to investigate the clinical characteristics, treatment and prognosis effect of malig-nant ovarian germ cell tumors (MOGCTs). A total of 39 patients with MOGCTs treated at Gynecology Obstetrics in Tianjin Central Hospital were enrolled from January 1999 to November 2009 in this study. All the patients under-went pathological examination and diagnosis was confirmed. We used univariate and multivariate logistic sion analysis to evaluate influencing factors, and Kaplan-Meier survival analysis and cox promotional hazard regres-sion analysis were used to evaluate the survival rate. All of patients were followed up until November 30, 2014. Eight cases (20.5%) were dead. Six months were the shortest survival time and this patient with IV stage yolk sac tumor was ill-controlled after operation, progressing to death rapidly. In respect of surgical procedures, 5 cases in pregnant group underwent laparotomy and 3 cases underwent laparoscope; In unpregnancy group, 3 cases under-went laparotomy and 3 cases underunder-went laparoscope. There were no significant differences between two groups (P=1.000). Seven cases in pregnant group received chemotherapy and one didn’t. In unpregnancy group, all the 6 cases received chemotherapy. The chemotherapy regimen was BEP (bleomycin, etoposide and cisplatine) and 4 courses were used. There were no significant differences between two groups (P=1.000). Kaplan-Meier survival analysis showed no significant differences in the impact of Federation of Gynecology and Obstetrics (FIGO) I-II stag-ing on survival prognosis (P > 0.05), however, manifeststag-ing significant differences were found when compared to stage IV respectively (I vs IV, X2=27.072, P < 0.001; II vs IV, X2=6.983, P=0.008; III vs IV, X2=10.671, P=0.001) and between stage I and stage III (X2=4.965, P=0.026). The result of Cox regression identified only MOGCT histologi-cal type as a predictor of overall survival (OS, Wald=6.240, P=0.012). For pregnancy analysis, univariate logistic regression analysis showed that no significant difference was found between pregnancy group and non-pregnancy (Wald=2.410, P=0.121). A multivariate logistic regression analysis also showed no statistical differences between two groups. FIGO staging and MOGCT histological type are critical factors affecting the prognosis of the patients with MOGCTs. The pregnant outcome of the patients receiving chemotherapy is desirable, and there are no significant effects of age, surgical-pathological staging, MOGCT histological type, surgical procedures and tumor size on the pregnancy outcome.
Keywords: Malignant ovarian germ cell tumors, clinical characteristics, treatment, prognosis
Introduction
Malignant ovarian germ cell tumors (MOGCTs) originate from embryonic primordial germ cells, and a higher incidence is found in adolescent and young adult women [1-3]. MOGCTs should be highlighted by the clinicians because of their high growth rate and relatively poor prognosis
[4-6]. Patients with MOGCTs have no specific
clinical manifestations, and the common symp-toms include stomachache, vaginal bleeding, abdominal distension or pelvic masses, etc. [7-9]. The late symptoms are mostly emaciation or weak, etc. Because MOGCTs have high grade
of malignancy and fast growth rate, their tumor capsules are more easily ruptured, and more than half of the patients complicated by fever [10]. Even in late stage of the MOGCT patients, the uterus and contralateral ovary are little affected. Pedicle torsion happens easily due to the shift of barycenter of teratoma. In this study, the clinical data of 39 cases of patients with malignant ovarian germ cell tumors were
retro-spectively analyzed. Their pathological feature,
Materials and methods
General materials
Inclusion criteria: All the case data were from
our hospital and pathologically confirmed,
the-se data were further reviewed by at least one doctor with senior position. Operation-patholo-
gic stage was based on the classification sys
-tem published by Federation of Gynecology and Obstetrics (FIGO) in 2013. Exclusion criteria:
Non-malignant ovarian germ cell tumors and cases with incomplete information.
A total of 39 patients with malignant ovarian germ cell tumors (MOGCTs) treated at Tianjin Central Hospital of Gynecology and Obstetrics from January 1999 to November 2009 were enrolled in this study. All the patients
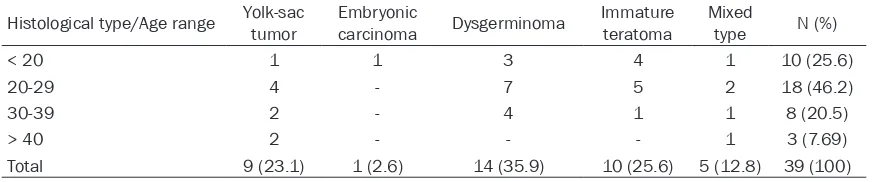
under-(12.8%) and 1 case was embryonic carcinoma (2.6%) (Table 1). Clinical data including age, cardinal symptom, sign, pathological diagnosis, stage, chemotherapy regimen and follow-up visit, etc. were collected. This research was approved by the Ethics Committee of Tianjin Central Hospital of Obstetrics and Gynecology.
Treatment
All the patients received surgery therapy.
[image:2.612.89.529.86.177.2]Fer-tility-preserving surgery was performed in the patients with the demands of fertility, and the adnexa tissue of diseased side was removed by tumorectomy. Patients without the demands of fertility underwent tumor staging surgery or cytoreductive surgery, then the abdominopelvic cavity was carefully detected. The full of uterus and its bilateral attachments, greater omen-tum appendix and pelvic lymph nodes were
Table 1. The age and MOGCT histological type of the patients
Histological type/Age range Yolk-sac tumor Embryonic carcinoma Dysgerminoma Immature teratoma Mixed type N (%)
< 20 1 1 3 4 1 10 (25.6)
20-29 4 - 7 5 2 18 (46.2)
30-39 2 - 4 1 1 8 (20.5)
> 40 2 - - - 1 3 (7.69)
[image:2.612.90.526.212.328.2]Total 9 (23.1) 1 (2.6) 14 (35.9) 10 (25.6) 5 (12.8) 39 (100)
Table 2. MOGCT histological type and clinical manifestation of the patients
Histological type N (cases)
Clinical manifestation [cases (%)] Abdominal
mass Abdominal distension Stomachache bleedingVaginal None
Yolk-sac tumor 9 5 (55.6%) 2 (22.2%) 1 (11.1%) 1 (11.1%) 0
Embryonic carcinoma 1 1 (100.0%) 0 0 0 0
Dysgerminoma 14 8 (57.2%) 2 (14.3%) 2 (14.3%) 1 (17.1%) 1 (17.1%)
Immature teratoma 10 6 (60.0%) 2 (20.0%) 2 (20.0%) 0 0
Mixed type 5 1 (20.0%) 2 (40.0%) 0 1 (20.0%) 1 (20.0%)
Total (cases) 39 21 (53.8%) 8 (20.5%) 5 (12.8%) 3 (7.7%) 2 (5.2%)
Table 3. Histological type and operation-pathologic stage of the patients Histological type (cases)N FIGO staging [cases (%)]
I II III IV
Yolk-sac tumor 9 4 (44.4%) 1 (11.1%) 3 (33.4%) 1 (11.1%)
Embryonic carcinoma 1 0 0 1 (100.0%) 0
Dysgerminoma 14 8 (57.1%) 2 (14.3%) 4 (28.6%) 0
Immature teratoma 10 5 (50.0%) 0 4 (40.0%) 1 (10.0%)
Mixed type 5 3 (60.0%) 2 (40.0%) 0 0
Total (cases) 39 20 (51.3%) 5 (12.8%) 12 (30.8%) 2 (5.1%)
went pathological exami-nation and the diagnosis
was confirmed.
Accord-ing to the tumor
patho-logical classification, 14
also resected. The diameter of residual tumor foci was controlled within 2 cm by cytoreduc-tive surgery.
BEP (bleomycin, etoposide and cisplatine) was adopted as the main chemotherapy regimen. Other chemotherapy regimens such as IEP (ifosfamide, etoposide and cisplatine) or VelP (vincristine, ifosfamide and cisplatine) were used in the patients with uncontrolled tumor or recurrence. The treatment time lasted 4-10 chemotherapy courses.
used to determine the effects of patients’ char-acteristics on the pregnancy. Inspection level
with bilateral α < 0.05 was considered as sta
-tistically significant.
Results
Clinical manifestation
[image:3.612.91.358.83.305.2]The major clinical manifestations of MOGCT patients were abdominal mass, abdominal dis-tension, stomachache and vaginal bleeding,
Table 4. Histological type and surgery type of the patients
Histological type Staging preserving Fertility-surgery(cases)
Tumor staging or cytoreductive
surgery (cases) N
Yolk-sac tumor I 4 0 4
II 1 0 1
III 1 2 3
IV 0 1 1
Embryonic carcinoma III 1 0 1
Dysgerminoma I 8 0 8
II 2 0 2
III 2 2 4
Immature teratoma I 5 0 5
III 4 0 4
IV 1 0 1
Mixed type I 3 0 3
II 1 1 2
Total (cases) 33 6 39
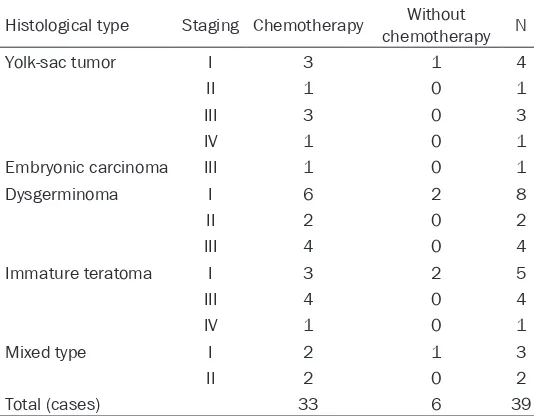
Table 5. Histological type and postoperative chemotherapy of the patients
Histological type Staging Chemotherapy chemotherapyWithout N
Yolk-sac tumor I 3 1 4
II 1 0 1
III 3 0 3
IV 1 0 1
Embryonic carcinoma III 1 0 1
Dysgerminoma I 6 2 8
II 2 0 2
III 4 0 4
Immature teratoma I 3 2 5
III 4 0 4
IV 1 0 1
Mixed type I 2 1 3
II 2 0 2
Total (cases) 33 6 39
Observational index
The follow-up visit was initiated for all the patients after the
sur-gery, the survival time was defined
as the time window from the start of surgery to death or the last fol-low-up visit. The survival time was counted as the day of last follow-up visit for patients who were lost in follow-up visit. The follow-ups included general conditions of the patients, pregnancy outcome of the patients with demands of fer-tility, recurrence or not, time of recurrence, treatment and effect after recurrence, etc.
Statistical methods
The collected data were analyzed
with SPSS17.0 software, mea-surement data of normal distribu-tion was presented with mean ± standard deviation (mean ± SD), and the comparison of the mean
of two groups was analyzed by
Student-t test. The comparison among groups of measurement data of non-normal distribution was based on non-parametric test. The comparison of sample rate of two groups using X2 test
and Fisher exact test was applied in this study. Kaplan-Meier sur -vival curves were created to deter-mine differences in survival. Cox regression was also performed using data that trended toward
[image:3.612.90.357.352.560.2]etc. In this study, the most common clinical manifestation was the appearance of abdomi-nal mass, which was found in 21 cases (53.8%), followed by 8 cases (20.5%) with abdominal distension, 5 cases (12.8%) with stomachache, 3 cases (7.7%) with vaginal bleeding, and 2 cases (5.2%) had no clinical manifestations.
Specific data are shown in Table 2.
Operation-pathologic stage
All the patients were subjected to definite path -ological diagnosis after surgery, based on the
classification system published by FIGO in
2013, staging conditions were as follows: 20 cases (51.28%) were stage I; 5 cases (12.82%)
were stage II; 12 cases (30.77%) were stage III; 2 cases (5.13%) were stage IV and all showed the existence of pulmonary metastasis. Accor-
ding to the classification of histological type,
yolk-sac tumor and immature teratoma III/IV had a relatively high incidence, which were 4/9 and 5/10, respectively. Only one case was
embryonic carcinoma and classified in stage III. Specific data are shown in Table 3.
Surgical methods
[image:4.612.92.520.72.487.2]A total of 33 patients (84.62%) received fertili-ty-preserving surgery and 6 patients (15.38%) received tumor staging surgery or cytoreduc-tive surgery. Details were shown in Table 4.
Postoperative chemotherapy
Postoperative chemotherapy was performed in 33 patients. Chemotherapy regimen was
main-ly as BEP. For the patients with uncontrolled
tumor or recurrence, other chemotherapy regi-mens such as IEP or VelP were used. The che-motherapy courses were 4-10. Six patients didn’t receive chemotherapy, including 1 stage Ia yolk-sac tumor case, 2 stage Ia class G1 immature teratoma cases, 2 stage Ia dysgermi- noma cases and 1 stage Ia mixed case. See
Table 5.
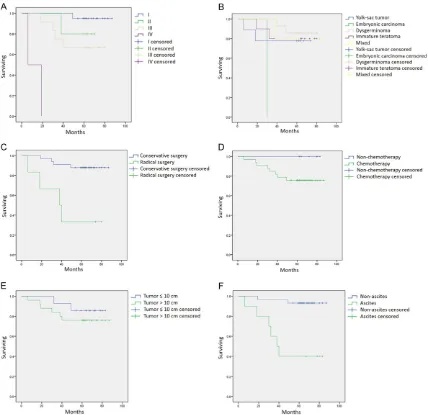
Survival analysis
All the 39 patients were followed up until November 30, 2014. Eight patients (20.5%) were dead. Six months were the shortest sur-vival time and this patient with IV stage yolk sac tumor was ill-controlled after operation, pro-gressing to death rapidly. The rest 7 patients died of tumor recurrence after operation. The
average of progression-free survival (PFS) were
22.0±11.4 months, the average of overall sur-vival (OS) were 29.0±14.5 months, and the lon-gest survival time were 49 months. Up to the
final day of fellow-up visit, 31 cases (79.5%)
survived free of tumor and no patients were dead above 5 years after operation. Among them, 4 cases were dead receiving conserva-tive operation and 5-year survival rate was 87.9%; 4 cases were dead receiving compre-hensive tumor staging surgery or cytoreductive surgery and 5-year survival rate was 33.3%.
Kaplan-Meier survival analysis showed no sig
-nificant differences in the impact of FIGO I-II
staging on survival prognosis (P > 0.05),
how-ever, manifesting significant differences were
found when compared to stage IV respectively (I vs IV, X2=27.072, P < 0.001; II vs IV, X2=6.983, P=0.008; III vs IV, X2=10.671, P=0.001) and between stage I and stage III (X2=4.965, P= 0.026, Figure 1A). Based on MOGCT
histologi-cal type, Kaplan-Meier survival analysis showed a significant difference of OS between embry -onic carcinoma and dysgerminoma (X2=14.000, P < 0.001), and between embryonic carcinoma and mixed type (X2=5.000, P=0.025, Figure
1B). The univariate analysis showed that patients undergoing tumor staging surgery or cytoreductive surgery had decreased OS com-pared with those receiving the conservative surgery (X2=12.307, P < 0.001, Figure 1C). How-
ever, no significant differences of the OS were
found between patients with and without che-motherapy (Figure 1D) and patients had a
big-ger (≥ 10 cm) and smaller (< 10 cm) tumor
(Figure 1E). In addition, patients with or without
ascites showed significantly different OS (X2= 15.509, P < 0.001, Figure 1F).
To exclude potential confounding, Cox regres-sion was performed concerning the variables
significant on univariate analysis (FIGO staging,
MOGCT histological type and ascites) as well as
variables previously identified as potential con -founders (age, surgical method, chemotherapy
and tumor size). The result of Cox regression identified only MOGCT histological type as a
predictor of OS (Wald=6.240, P=0.012).
Pregnancy analysis of the patients
We observed the pregnancy outcome of the patients with an age of 20-39 years. Of these, a total of 14 patients had a demand of fertility, and stopped chemotherapy and removed the
contraceptive measures ≥ 1 year. The patients
were divided into pregnancy group (8 cases, with an average age of 26.0±4.1) and non-preg-nancy group (6 cases, with an average age of 25.8±5.7). Patients in both groups had com-pared age, underwent conservative surgery, received chemotherapy and without ascites. The operation-pathologic staging of pregnancy group was as follows: 6 cases were stage I and 2 cases were stage II; In non-pregnancy group, 3 cases were stage I and 3 cases were stage III. Univariate logistic regression analysis showed
that no significant difference was found
between two groups (Wald=2.410, P=0.121). In MOGCT histological type, patients in pregnancy group had three yolk-sac tumors, three dysger-minomas, one immature teratoma and one mixed type. Patients in non-pregnancy group had one yolk-sac tumor, one dysgerminoma, three immature teratomas and one mixed type.
No significant differences in histological types
Table 6. Univariate logistic regression analysis of the pregnancy in patients
Factors B S.E. Wald P
FIGO staging -1.230 0.793 2.410 0.121 MOGCT histological type -0.474 0.428 1.224 0.269 Tumor size -0.182 1.133 0.026 0.872 Surgical approach -0.511 1.095 0.217 0.641
were found between two groups (Wald=1.224, P=0.269). In pregnancy group, three patients
had a tumor ≤ 10 cm, and five had a tumor > 10
cm; In non-pregnancy group, two patients had a
tumor ≤ 10 cm, and four had a tumor > 10 cm.
Univariate logistic regression analysis showed
no significant difference in tumor size between
two groups (Wald=0.026, P=0.872). In
preg-nancy group, five patients received laparotomy,
three patients received laparoscope approach; In non-pregnancy group, three patients receiv- ed laparotomy, three patients received
laparo-scope approach. There were no significant dif -ferences when these two groups were com-pared (Wald=0.217, P=0.641). Details were shown in Table 6. A multivariate logistic regres-sion analysis also showed no statistical differ-ences between two groups.
Discussion
MOGCT patients have the common symptoms such as stomachache, vaginal bleeding, ab- dominal distension or pelvic masses [11-13]. The late symptoms are mostly emaciation or weak, etc. Because MOGCTs have high grade of malignancy and fast growth rate, their tumor capsules are more easily ruptured. Above half of the patients have the complication of fever [14]. Even in late MOGCT patients, the uterus and contralateral ovary are less affected. Since the gravity center of teratoma deviates fre-quently, pedicle torsion happens easily. It is usually misdiagnosed as acute appendicitis, indigitation or intestinal twist, etc.
Since MOGCTs have a higher incidence in ado-lescent and young adult women, most in this age window have the demands of fertility after marriage. Therefore, higher requirements were proposed for conventional surgical treatment [15]. The principle of conventional treatment of MOGCTs is tumor staging surgery or cytoreduc-tive surgery. The operation extent includes uter-us and its attachment on both sides. In addi-tion, bilateral accessary, greater omentum re- section, pelvic lymphadenectomy and basin abdominal peritoneal multi-point biopsy are also involved [16]. This type of surgery often leads to fertility lose perpetually and low life quality [17].
In this study, one stage I patients was dead, the 5-year survival rate was 95.0%; One stage II
patients was dead, the 5-year survival rate was
80.0%; Four stage III patients were dead, the
5-year survival rate was 66.7%; Two stage IV patients were dead, the 5-year survival rate
was 0%. Survival analysis showed significant
differences between stage I, II, III and stage IV, respectively, and between stage I and stage III. These results showed that the patients with
higher FIGO staging had a worse prognosis.
Report indicates that patients with dysgermi-noma have the best prognosis, while followed by immature teratoma and yolk-sac tumor, and the prognosis of mixed and embryonic carcino-ma is the worst [18]. In eight dead patients, two with yolk-sac tumor, the 5-year survival rate was 77.8%; One with embryonic carcinoma, the 5-year survival rate was 0%; Two with dysgermi-noma, the 5-year survival rate was 85.7%; Two with immature teratoma, the 5-year survival rate was 80%; One with mixed type, the 5-year survival rate was 80%. The 5-year survival rate of dysgerminoma was the highest and embry-onic carcinoma was the lowest in our study.
Kaplan-Meier survival analysis showed a sig
-nificant difference of OS between embryonic
carcinoma and dysgerminoma, as well as be- tween embryonic carcinoma and mixed type. A total of 33 patients (84.62%) received con-servative surgery. The extent of surgical resec-tion includes unilateral ovaries and fallopian tubes, the greater omentum and pelvic lymph nodes, however, the uterus and the contralat-eral attachments remained to be preserved.
Four cases who received conservative surgery
were dead, the 5-year survival rate was 87.9%;
Four received comprehensive tumor staging or
cytoreductive surgery were dead and the 5-year survival rate was 33.3%, which was related to
the late overall FIGO staging. The univariate
analysis in this study also showed that patients undergoing tumor staging surgery or cytoreduc-tive surgery had decreased OS compared with those receiving the conservative surgery.
To determine the influence of the above factors
on the pregnancy of the patients, 14 patients having demand of fertility were divided into pregnant group and non-pregnancy group. The-
re was no significant difference in age between
two groups. Univariate logistic regression
anal-ysis showed that there were no significant dif
-variate logistic regression analysis also showed no statistical differences between two groups. The above results suggested that there were no
significant effects of age, surgical-pathological
staging, MOGCT histological type, surgical
pro-cedures and tumor size on pregnancy.
The clinical characteristics, treatment and prognosis effect of MOGCTs were investigated, and advantage of this study is to evaluate the pregnant outcome of the patients by univariate logistic regression analysis and multivariate logistic regression analysis. Disadvantages of this study were such as the limited number of patients, and some patients were excluded because of incomplete information. Additional follow-ups are needed to evaluate long-term clinical outcomes.
In conclusion, the treatment of surgery com-bined with chemotherapy is the major method for malignant ovarian germ cell tumors. BEP is the preferred chemotherapy regiment after
MOGCT operation. FIGO staging and MOGCT
histological type are critical factors affecting the prognosis of the patients with MOGCTs. Most of patients receiving BEP chemotherapy can be naturally pregnant and the pregnant
outcome is desirable. There are no significant
effects of age, surgical-pathological staging, MOGCT histological type, surgical procedures
and tumor size on pregnancy outcome.
Disclosure of conflict of interest
None.
Address correspondence to: Dr. Pengpeng Qu, De- partment of Gynecologic Oncology, Tianjin Central Hospital of Gynecology Obstetrics, No. 156, Nankai Three Road, Nankai District, Tianjin 300100, China. Tel: +86-022-58287187; E-mail: qu.pengpeng@hot-mail.com
References
[1] Zhang R, Sun YC, Zhang GY, Wu LY and Zuo J. Treatment of malignant ovarian germ cell tu-mors and preservation of fertility. Eur J Gynae-col OnGynae-col 2012; 33: 489-492.
[2] Nagai Y, Inamine M, Kudaka W and Aoki Y. [Chemotherapy for ovarian malignant germ cell tumors]. Nihon Rinsho 2012; 70 Suppl 4: 648-655.
[3] Liu Y, Ren T, Feng FZ, Wan XR, Shen K and Xiang Y. [Clinical analysis of 15 cases of malig-nant ovarian germ cell tumors with lung
metas-tasis]. Zhonghua Fu Chan Ke Za Zhi 2012; 47: 40-44.
[4] Mangili G, Sigismondi C, Gadducci A, Cormio G, Scollo P, Tateo S, Ferrandina G, Greggi S, Candiani M and Lorusso D. Outcome and risk factors for recurrence in malignant ovarian germ cell tumors: a MITO-9 retrospective study. Int J Gynecol Cancer 2011; 21: 1414-1421. [5] Salonen J, Leminen A, Stenman UH, Butzow R,
Heikinheimo M and Heikinheimo O. Tissue AP-2gamma and Oct-3/4, and serum CA125 as diagnostic and prognostic markers of malig-nant ovarian germ cell tumors. Tumour Biol 2008; 29: 50-56.
[6] Fan X, Zhang H, Meng S, Zhang J and Zhang C. Role of diffusion-weighted magnetic reso-nance imaging in differentiating malignancies from benign ovarian tumors. Int J Clin Exp Med 2015; 8: 19928-19937.
[7] Masch WR, Kamaya A, Wasnik AP and Maturen KE. Ovarian cancer mimics: how to avoid being fooled by extraovarian pelvic masses. Abdom Radiol (NY) 2016; 41: 783-93.
[8] Fawzy A, Mohamed MR, Ali MA, Abd El-Magied MH and Helal AM. Tissue CA125 and HE4 gene expression levels offer superior accuracy in discriminating benign from malignant pelvic masses. Asian Pac J Cancer Prev 2016; 17: 323-333.
[9] Nella AA, Kaplowitz PB, Ramnitz MS and Nan-dagopal R. Benign vaginal bleeding in 24 pre-pubertal patients: clinical, biochemical and imaging features. J Pediatr Endocrinol Metab 2014; 27: 821-825.
[10] Chen CA, Lin H, Weng CS, Wen KC, Lu CH, Chou HH, Huang YF, Kang CY, Ho CM, Yu MH and Chou CY. Outcome of 3-day bleomycin, etopo-side and cisplatin chemotherapeutic regimen for patients with malignant ovarian germ cell tumours: a taiwanese gynecologic oncology group study. Eur J Cancer 2014; 50: 3161-3167.
[11] Park JY, Kim DY, Suh DS, Kim JH, Kim YM, Kim YT and Nam JH. Significance of the complete surgical staging of stage i malignant ovarian germ cell tumors. Ann Surg Oncol 2016; 23: 2982-7.
[12] Park JY, Kim DY, Suh DS, Kim JH, Kim YM, Kim YT and Nam JH. Outcomes of surgery alone and surveillance strategy in young women with stage I malignant ovarian germ cell tumors. Int J Gynecol Cancer 2016; 26: 859-864.
[13] Yang ZJ, Liu ZC, Wei RJ and Li L. An analysis of prognostic factors in patients with ovarian ma-lignant germ cell tumors who are treated with fertility-preserving surgery. Gynecol Obstet In-vest 2016; 81: 1-9.
and II utero-ovarian anastomoses during uter-ine artery embolization for fibroid tumors: im-pact on symptom recurrence and permanent amenorrhea. J Vasc Interv Radiol 2013; 24: 1347-1352.
[15] Shahsiah R, Jahanbin B, Rabiei R, Ardalan FA, Sarhadi B and Izadi-Mood N. Malignant ovari-an germ cell tumours in gonadal Y chromo-some mosaicism. J Clin Pathol 2011; 64: 973-976.
[16] Karimi Zarchi M, Mousavi A, Gilani MM, Baroo-ti E, Amini Rad O, Ghaemmaghami F, Teimoori S and Behtas N. Fertility sparing treatments in young patients with gynecological cancers: Ira-nian experience and literature review. Asian Pac J Cancer Prev 2011; 12: 1887-1892.
[17] Roukos DH, Murray S and Briasoulis E. Molec-ular genetic tools shape a roadmap towards a more accurate prognostic prediction and per-sonalized management of cancer. Cancer Biol Ther 2007; 6: 308-312.