Ultrasound Evaluation of Radial Nerve Palsy Associated
with Humeral Shaft Fractures to Guide Operative Versus
Non-Operative Treatment
Melissa Esparza
1, Jason R. Wild
1, Christopher Minnock
2, Kurt M. Mohty
1, Lisa M.
Truchan
1, Mihra S. Taljanovic
1Introduction
Injuries to the radial nerve in the setting of humeral shaft fractures are among the most common peripheral nerve lesions associated with trauma (1-5). The intimate relation-ship of the radial nerve with the shaft of the humerus within the spiral groove makes it particularly vulnerable to traction, transec-tion, or entrapment injuries with fractures of the middle and distal third of the hu-merus (6, 7). Humeral shaft fractures are commonly treated non-operatively owing to Dr. Sarmiento’s extensive work and research
with the functional brace (8). When there is an associated radial neuropathy, nonopera-tive management of the humeral shaft frac-ture and expectant management of the nerve palsy remain the most common treatment recommendation (2, 4, 5, 7). In a systematic review of studies of humeral shaft fractures associated with radial nerve palsy, Shao et al. report a prevalence of radial nerve palsy of 11.8%. They report a spontaneous recov-ery rate of 70.7% from their meta-analysis of 532 radial nerve palsies in 4517 fractures (3). Other studies have reported spontane-ous nerve recovery rates as high as 89% (9).
1University of Arizona/Banner University
Medical Center, Tucson, AZ, USA. Departments of Orthopaedics (ME, LMT, JRW, KMM) and Department of Medical Imaging (MST), 2DMC Children’s Hospital
of Michigan, Detroit, MI, USA (CM)
Correspondence:
melissa.esparza@gmail.com
Tel.: + 1 520 465 8107 Fax.: + 1 520 626 2668
Received: 1 February 2019 Accepted: 9 May 2019
Key Words: Humerus Fracture Ultrasound Radial Nerve Injury.
Objective. To determine the effectiveness of diagnostic ultrasound (US) at evaluating the condition of the radial nerve in the setting of humeral shaft fractures. Materials and Methods. An observational study was performed of 18 patients with radial nerve palsy associ-ated with humeral shaft fractures who underwent US examination to assess the condition of the radial nerve. Results. Six patients with humeral shaft fractures treated nonoperatively in a functional brace had US findings consistent with contusion or stretch radial nerve in-jury. Twelve patients ultimately underwent surgery either because US showed an entrapped or lacerated radial nerve, or for other operative indications. There was a 92% concordance (11/12 patients) between US and intraoperative findings with regards to the condition and loca-tion of the radial nerve, with the remaining case being complicated by delayed surgical treatment secondary to patient factors. Conclusion.
not only has the ability to determine if a nerve is intact, but it can reveal the precise location of the nerve in relationship to bone or other structures as well as show inflam-matory changes within and about the nerve (11, 12). US evaluation of the radial nerve in the setting of humeral shaft fracture allows for differentiation of nerve injury secondary to contusion or stretch injury versus lacera-tion or entrapment within the fracture site (3, 13-15). If signs of nerve transection, par-tial-thickness tear or entrapment are identi-fied, a change of management may be indi-cated with conversion to early exploration and operative fracture fixation to prevent delayed treatment and problematic healing of the fracture with interposed nerve tissue. Our study examines the utility of US evalu-ation of the radial nerve in cases of humeral shaft fractures associated with radial nerve palsy. We explore the correlation of US find-ings to the actual state of the nerve observed intraoperatively.
The purpose of this study is to determine the effectiveness of diagnostic US at evaluat-ing the condition of the radial nerve in the setting of humeral shaft fractures and to discuss whether this information may help guide surgeons in their clinical decision making for operative versus nonoperative treatment of these injuries.
Materials and Methods
Institutional Review Board approval was obtained for this observational study. A ret-rospective review was conducted of patients with humeral shaft fracture who had under-gone US evaluation of the radial nerve from
addition, patients with a humeral shaft frac-ture that the treating surgeon deemed op-erative in nature were also eligible for study enrollment for as a control group to obtain US evaluation of presumably normal radial nerves. Operative indications for humeral shaft fractures included open fractures, frac-tures with associated vascular injury requir-ing surgical repair, and ipsilateral extremity fractures or polytrauma patients who would undergo surgery for improved mobilization of the extremity. Other relative indications for surgery included patient preference/de-sire for earlier mobilization, body habitus, and inability to tolerate a brace. Exclusion criteria included any pre-existing compro-mise to radial nerve function.
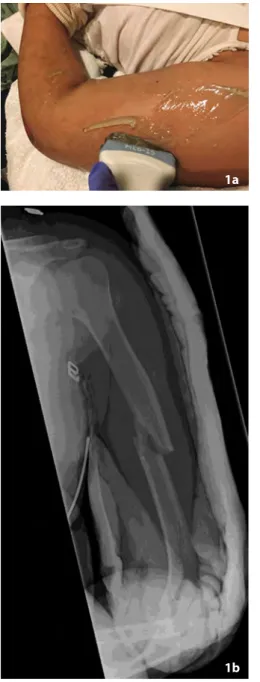
while contused nerves appear hypoechoic, heterogeneous and thickened. Entrapped nerves dive into the fracture site. Because of significant pain and discomfort in the setting of the acute humeral shaft fractures, all patients were examined in the supine position on the ultrasound stretcher or in the hospital bed with their affected arm at the examiner’s side. Figure 1 demonstrates patient positioning, humeral shaft fracture,
and the US technique utilized in this study in a patient and representative US images of their intact radial nerve.
The radial nerves were first traced along their short axis using the “elevator” tech-nique for rapid screening of long nerve seg-ments and after that along their long axis throughout the arm to their bifurcation into the superficial and deep branches at the an-terior aspect of the elbow proximal to the Figure 1. Intact radial nerve in 18-year-old female with humer-al shaft fracture and radihumer-al nerve phumer-alsy status post humer-all-terrain vehicle (ATV) accident (Patient 4). (A) Photograph of the left upper extremity shows ultrasound probe over the swollen posterior mid arm in the region of the humeral shaft fracture. (B) AP radiograph of the left humerus shows moderately dis-placed and mildly comminuted oblique humeral shaft fracture. (C) Long axis and (D) short axis grayscale ultrasound (US) im-ages at the posterior aspect of the left mid arm/humerus shows mildly edematous but intact radial nerve (arrows) superficial to the humeral shaft fracture site (block arrows) consistent with neurapraxia. Small portion of the radial nerve shows mildly increased echogenicity (arrowhead in C, between arrows in D) without discontinuity. The patient was treated conservatively in a Sarmiento brace with full radial nerve recovery achieved after 10 weeks.
1a
1b
body away from the examiner and enable better exposure of the examined upper ex-tremity along the pathway of the radial nerve. Of note, in the non-acute trauma set-ting, the radial nerve can be examined with the patient in a sitting position.
Seventeen of 18 patients had their US imaging within 24 hours after injury. Pa-tients with US diagnosis of radial nerve entrapment or laceration were treated with open reduction internal fixation (ORIF) of their humeral fracture. Patients were fol-lowed in clinic until they showed signs of nerve recovery or were lost to follow up. At the conclusion of the study, patients that had been lost to follow up were contacted via telephone.
Results
Eighteen patients were enrolled in the study (Table 1). The average age of patients was 48 years old (range 18-81), and 56.6% of patients were male. Mechanisms of injury included ground level fall (6), fall from sev-eral feet (3), motor vehicle or all-terrain ve-hicle (ATV) accidents (5), bicycle accidents (2), assault (1), and wrestling (1). Fourteen patients included in the study had a radial nerve palsy, four in the nonoperative brac-ing group and ten in the operative group. Two patients in the nonoperative group underwent US imaging because their ini-tial clinical exam on presentation was con-cerning for radial nerve palsy however they
initially treated with a functional brace. Of those eight, two subsequently went on to ORIF, one because of inability to tolerate the brace and one after developing a fracture nonunion. Six patients underwent ORIF due to US showing entrapment or laceration of the radial nerve (Figure 2). Four other pa-tients underwent ORIF for other indications including polytrauma, pathologic fracture, and surgeon judgement.
Ultrasound and Operative Findings
Figure 2. Transverse humeral shaft fracture with associated radial nerve entrapment and partial laceration in a 33-year-old female status post bicycle accident (Patient 8). (A) AP radiograph of the left humerus shows com-pletely displaced mildly overriding humeral shaft fracture. (B) Long axis power Doppler US image at the level of the left humeral shaft fracture shows radial nerve entrapment at the fracture site (arrow) with partial laceration (arrowhead). (C) Long axis grayscale US image shows radial nerve entrapment (arrow) at the humeral shaft frac-ture site (block arrows). (D) Intraoperative photograph of the posterior aspect of the right arm confirmed radial nerve entrapment (arrow) and partial laceration (arrowhead) at the humeral shaft fracture site which correlates with the US findings. (E) AP and (F) lateral postoperative radiographs of the left humerus obtained two weeks later show a laterally applied low contact dynamic compression plate with 6 cortical screws transfixing the left humeral shaft fracture in anatomic alignment and without hardware complication. The patient achieved full radial nerve recovery at final follow up.
Table 1. Patient Information and Findings
Patients Age (y)
Sex Mechanism of injury
Humerus radiographs
Ultrasound findings Method of treatment
Operative findings 1 38 M MVC Transverse
midshaft with butterfly fragment
Difficult visualization secondary to large body habitus however no definitive entrapment seen as nerve appears superficial to fracture site
Functional bracing N/A*
2 31 M Assaulted with ice pick
Long spiral comminuted fracture
Normal appearance of radial nerve Functional bracing
N/A
3 37 M Ground level fall
Transverse midshaft fracture
Stretched and mildly thickened radial nerve with no evidence of entrapment
Functional bracing
N/A
4 18 F ATV
accident
Transverse midshaft fracture
Radial nerve superficial to fracture site without evidence of entrapment
Functional bracing
N/A
5 81 M Fall from bed
Midshaft spiral fracture
Radial nerve edematous but contiguous with no evidence of transection or entrapment
Functional bracing
N/A
6 21 F ATV Transverse Enlargement and irregularity of the Functional N/A
2a 2b 2c
laceration
9 33 M MVC Oblique
midshaft fracture with butterfly fragment
Nonvisualization of the radial nerve at the fracture site concerning for entrapment and transection, with associated thickening of the nerve just distal to the fracture
ORIF
Tendon transfers
RN§
10 52 F Fall from
truck Spiral fracture of distal shaft with butterfly fragment
Findings concerning for radial nerve entrapment at the level of the fracture with mild diffuse enlargement of the visualized nerve
ORIF RN||
11 76 F Ground level fall
Long spiral fracture of mid to distal shaft
Nonvisualization of the radial nerve at the fracture site worrisome for radial nerve entrapment
ORIF RN¶
12 74 F Ground level fall
Long spiral fracture of proximal to midshaft
1st US: irregular, enlarged, edematous radial nerve without discontinuity or entrapment
2nd US: abutment and possible impingement of the nerve at the posterior edge of the fixation plate distally
ORIF after unable to tolerate brace
RN**
13 59 F Ground
level fall Segmental comminuted midshaft fracture
Edematous radial nerve about the fracture site without definitive evidence of entrapment
ORIF after development of nonunion
RN††
14 60 M Ground level fall Oblique midshaft fracture with butterfly fragment
1st US: poor visualization of radial nerve suggesting focal entrapment 2nd US: findings consistent with partial entrapment at region of posttraumatic deformity
ORIF
Tendon transfers
RN‡‡
15 52 F Ground level fall
Spiral fracture of distal shaft with butterfly fragment
Thickened edematous nerve without entrapment
ORIF (surgeon judgement)*
RN§§
16 69 M Fall from
bed Midshaft oblique fracture
Unremarkable appearance of radial
nerve ORIF (pathologic
fracture)
RN‡‡
17 68 M MVC Transverse distal shaft fracture
Mild nerve edema, no entrapment ORIF
(polytrauma) RN||||
18 23 M Bicycle
accident Comminuted distal shaft fracture
Radial neve perched on distal fracture fragment with mild thickening distally but no evidence of laceration or entrapment
ORIF (surgeon judgement)* RN¶¶
In one of the patients (Patient 14) with US findings consistent with radial nerve entrapment, surgery was delayed six weeks due to patient factors and systems issues. This patient did not undergo US examina-tion at his initial presentaexamina-tion to the Emer-gency Department due to the unavailabil-ity of an MSK trained US technologist on a weekend evening. He was initially treated in a Sarmiento brace and instructed to have an US study performed the following week as an outpatient. The ultrasound was per-formed two weeks later and showed radial nerve entrapment. Despite US findings, this patient didn’t follow-up in orthopaedic clin-ic until five weeks after his injury, at whclin-ich time radiographs showed varus alignment of the fracture site with minimal callus forma-tion. After that the patient underwent ORIF of the right humeral shaft fracture. Opera-tive note described that the radial nerve was protected during the procedure however the condition of the nerve was not described in the operative report. Postoperatively this patient did not regain radial nerve function and ultimately underwent tendon transfers ten months later.
Based on results of our study, there was a 92% (11/12 patients) concordance between US examination and intraoperative findings with regards to the condition and location of the radial nerve (including the six patients in the control group), with the remaining case being complicated by delayed surgical treatment secondary to patient factors.
Orthopaedic Clinic Follow-up and Clinical Results
There were two patients who did not follow up in orthopaedic clinic. Of the remaining 16 patients, mean follow up time was 13 weeks (range 2-40 weeks). Only 11 patients had greater than four weeks of follow up, all of whom went on to fracture union. Four of the six patients treated nonoperatively had
full radial nerve function at their final clinic follow up visit. One patient had partial re-covery of radial nerve function at her two week postoperative visit. Upon phone inter-view at nine months post-injury, she report-ed full motor recovery with remaining mild paresthesias that she felt were continuing to improve. The last of the six patients treated non-operatively was lost to follow-up.
Of the operatively treated group, six pa-tients reported full radial nerve recovery and two patients reported partial recovery. Two patients underwent tendon transfers after initial fixation of their humeral shaft fracture. Another patient passed away two weeks postoperatively secondary to meta-static esophageal cancer, and the final pa-tient in the operatively treated group did not have clinic or phone follow-up.
Discussion
Humeral shaft fractures associated with ra-dial nerve palsies are a debilitating injury. Several studies have described a high level of disability and poor functional outcomes associated with upper extremity peripheral nerve injuries (16-18). Management of these injuries has traditionally been with expect-ant care as humeral shaft fractures frequent-ly heal well with functional bracing and the majority of associated nerve palsies recover spontaneously. However, approximately 30% of patients with these injuries may not regain adequate radial nerve function with expectant management (3). Recovery for these patients may be long and cumbersome as radial nerve function is often monitored for 3-6 months before it is determined that the nerve will not recover spontaneously.
benefit from early surgical intervention may help to decrease disability and improve re-covery time for these patients.
Shao et al. (3) published a systematic re-view in 2005 of radial nerve palsy associated with humeral shaft fractures and presented an algorithm to guide treatment of these injuries. The algorithm includes US evalua-tion within three weeks of injury to assess the status of the radial nerve (3). If the nerve is continuous, loss of function is thought to be secondary to neurapraxia which may be managed conservatively. If the nerve is lac-erated or entrapped, early surgical interven-tion is preferred as nerve funcinterven-tion would not be expected to recover spontaneously. Depending on the condition and location of the entrapped and/or injured nerve, opera-tive treatment could include simple extrac-tion of the nerve from within the fracture site, nerve repair, or acute tendon transfers. If the nerve is severely contused or has an ir-reparable laceration, the likelihood of a pro-longed or unpredictable recovery is high. In some cases, the nerve would not be expect-ed to recover at al. In these settings, early tendon transfers may be beneficial in opti-mizing the patient’s functional recovery by restoring active extension of the wrist and digits. For example, pronator teres to exten-sor carpi radialis brevis is an ideal transfer as it restores wrist extension while sacrificing few if any functional deficits given that the pronator teres muscle maintains its function as a pronator after transfer while also allow-ing the patient to be able to actively extend their wrist. This eliminates the necessity of prolonged wrist bracing that patients with a wrist drop secondary to radial nerve palsy
weeks with a mean of 19 days which is dif-ferent from our study in which 17 of 18 pa-tients had their US studies within 24 hours of injury. It is more difficult to perform an US study in patients with hyperacute trauma with associated marked soft tissue edema and limited range of motion. However, we believe that prompt US examination of pa-tients with acute humeral shaft fractures and associated radial nerve palsy during their initial evaluation in the emergency depart-ment may expedite clinical decision making of nonoperative versus operative treatment and avoid delays in surgical treatment.
There may be several challenges to im-plementing a protocol of routine prompt US evaluation for patients with humeral shaft fractures and associated radial nerve palsy. At our institution, MSK US studies are read by fellowship-trained MSK radiologists with experience in US evaluation of peripheral nerve injuries, however we recognize that not all institutions will have these resourc-es available. Musculoskeletal US trained technologists or fellowship trained MSK radiologists are not routinely available at most institutions on nights and weekends. Patients may be instructed to follow up for an US examination on an outpatient basis, however issues of patient compliance, insur-ance coverage, etc. may delay evaluation or treatment.
influ-enced by their knowledge of the US find-ings. However, this limitation could not be avoided because the clinical decision mak-ing for nonoperative versus operative treat-ment was partially based on US findings.
The focus of this study was to evaluate the accuracy of US evaluation of the radial nerve in predicting intraoperative findings with a secondary goal of assessing clinical outcomes. However, our cohort had poor clinic follow-up, and for many patients we relied on phone calls and thus the patients’ subjective impression of their arm function and symptoms in reporting of our final out-comes. A potential focus for future studies is to evaluate clinical outcomes to determine whether routine use of US in patients with radial nerve palsies associated with humeral shaft fractures may lead to faster recovery, improved function, and differences in health care costs.
We had a small sample size due to the relative infrequency of this injury. However, to our knowledge this is the largest case se-ries in the literature evaluating US use for humeral shaft fractures associated with ra-dial nerve injuries. We found a high concor-dance (92%) between US and intraoperative findings describing the state of the radial nerve. Based on results of our study, we rou-tinely perform US examination in patients with humeral shaft fractures associated with radial nerve palsy at our institution at the time of their initial presentation.
Conclusion
Diagnostic US is an effective and efficient method for evaluating the radial nerve in the face of humeral shaft fractures. US evalua-tion provides a means of separating patients with a radial nerve palsy due to laceration or entrapment where surgical intervention is indicated from those who have a neura-praxia that can be managed nonoperatively. Patients with radial nerve injuries not
ex-pected to recover spontaneously may benefit from nerve repair or early tendon transfers. Earlier surgical intervention in this subset of patients may allow for earlier initiation of rehabilitation protocols, faster recovery, and reduced costs.
What Is Already Known on this Topic
The majority of radial nerve palsies associated with humeral shaft fractures may be treated nonoperatively with successful return of nerve function. However, injuries in which the radial nerve is lacerated or entrapped in the fracture site, as opposed to nerve palsies caused by contusion or stretch injuries, would not be expected to recover spontaneously and may require fur-ther treatment such as nerve repair or tendon transfers.
What this Study Adds
Our study demonstrates that US is an effective diagnostic tool in evaluating radial nerve injuries in the setting of acute hu-meral shaft fractures and can aid in clinical decision making by differentiating between patients with nerve laceration or entrapment who may benefit from surgery from those with neurapraxia managed nonoperatively.
Acknowledgements: Melissa Esparza, MD received a grant from the University of Arizona ACGME Resi-dent Leadership Scholarship to support submission, presentation, travel expenses, etc. related to this proj-ect. No authors have any proprietary interests in the materials described in this article.
Authors’ Contributions: Conception and design: CM, ME, JW and MT; Acquisition, analysis and in-terpretation of data: CM, ME, KM, JW, MT and LT; Drafting the article: CM and ME; Revising it critically for important intellectual content: ME, JW, MT, LT and CM; Approved final version of the manuscript: ME, JW, MT, LT, CM and KM.
Conflict of Interest: The authors declare that they have no conflict of interest.
References
1. Rockwood CA Jr, Green DP, Bucholz RW, Heck-man JD. Rockwood and Green’s Fracture in Adults. 4th ed. Philadelphia: Lippincott-Raven Publishers; 1996. p. 1043-5.
2. Crenshaw AH. Fracture of humeral shaft with ra-dial nerve palsy. In: Crenshaw AH, editor. Camp-bell’s Operative Orthopaedics, Vol. 2. 8th ed. St. Louis: Mosby Year Book; 1992. p. 1016.
ment of humeral shaft fractures with associated radial nerve palsy: a review of 117 cases. Arch Or-thop Trauma Surg. 2010;130(4):519-22.
6. Holstein A, Lewis GM. Fractures of the Humerus with Radial-Nerve Paralysis. J Bone Joint Surg Am. 1963;45:1382-8.
7. Ekholm R, Ponzer S, Tornkvist H, Adami J, Tider-mark J. The Holstein-Lewis humeral shaft fracture: aspects of radial nerve injury, primary treatment, and outcome. J Orthop Trauma. 2008;22(10):693-7.
8. Sarmiento A, Kinman PB, Galvin EG, Schmitt RH, Phillips JG. Functional bracing of fractures of the shaft of the humerus. J Bone Joint Surg Am. 1977;59(5):596-601.
9. Ekholm R, Ponzer S, Tornkvist H, Adami J, Tide-rmark J. Primary radial nerve palsy in patients with acute humeral shaft fractures. J Orthop Trau-ma. 2008;22(6):408-14.
10. Strandberg EJ, Mozaffar T, Gupta R. The Role of Neurodiagnostic Studies in Nerve Injuries and Other Orthopedic Disorders. J Hand Surg Am. 2007;32(8):1280-90.
11. Lawande AD, Warrier SS, Mukund SJ. Role of ul-trasound in evaluation of peripheral nerves. In-dian J Radiol Imaging. 2014;24(3):254-8.
14. Bodner G, Huber B, Schwabegger A, Lutz M, Waldenberger P. Sonographic detection of radial nerve entrapment within a humerus fracture. J Ul-trasound Med. 1999;18(10):703-6.
15. Cartwright MS, Yoon JS, Lee KH, Deal N, Walker FO. Diagnostic ultrasound for trau-matic radial neuropathy. Am J Phys Med Reha-bil. 2011;90(4):342-3.
16. Novak CB, Anastakis DJ, Beaton DE, Katz J. Pa-tient-reported outcome after peripheral nerve in-jury. J Hand Surg Am. 2009;34(2):281-7.
17. Novak CB, Anastakis DJ, Beaton DE, Mackinnon SE, Katz J. Biomedical and psychosocial factors associated with disability after peripheral nerve injury. J Bone Joint Surg Am. 2011;93(10):929-36. 18. Rivera JC, Glebus GP, Cho MS. Disability fol-lowing combat-sustained nerve injury of the up-per limb. Bone Joint J. 2014;96-B(2):254-8. 19. Nachef N, Bariatinskya V, Sulimovic S, Fontainea
C, Chantelot C. Predictors of radial nerve palsy recovery in humeral shaft fractures: A retrospec-tive review of 17 patients. Orthop Traumatol Surg Res. 2017;103(2):177-82.