A. Saifuddin, FRCR, Consultant Radiologist R. Mitchell, FRCR, Consultant Radiologist S. J. D. Burnett, FRCR, Consultant Radiologist Department of Radiology
A. Sandison, MRCPath, Consultant Pathologist J. A. S. Pringle, FRCS, Senior Lecturer in Pathology Department of Histopathology
The Royal National Orthopaedic Hospital Trust, Brockley Hill, Stanmore, Middlesex HA7 4LP, UK.
Correspondence should be sent to Dr A. Saifuddin. ©2000 British Editorial Society of Bone and Joint Surgery 0301-620X/00/110141 $2.00
Ultrasound-guided needle biopsy of primary
bone tumours
A. Saifuddin, R. Mitchell, S. J. D. Burnett, A. Sandison,
J. A. S. Pringle
From the Royal National Orthopaedic Hospital Trust, Stanmore, England
N
eedle biopsy is an established technique for the histological diagnosis of bone tumours, usually guided by fluoroscopy or CT. Surface lesions and aggressive tumours which have extended through the cortex are also amenable to imaging with ultrasound (US). We have assessed the diagnostic accuracy of US-guided Trucut needle biopsy in a consecutive series of patients referred to a Bone Tumour Unit with suspected primary bone tumours. Of 144 patients (83 men, 61 women; mean age 34.7 years) referred over a period of two years, 63 were considered suitable for US-guided biopsy. This was based on the presence of a relatively large extraosseous component, seen typically in osteosarcoma and malignant round-cell tumours. The results of needle biopsy were compared with those of surgical biopsy. The diagnostic accuracy was 98.4%, with only a single failed biopsy.Thus, in a selected group of patients, US is a very reliable technique of guidance for percutaneous needle biopsy of bone tumours.
J Bone Joint Surg [Br] 2000;82-B:50-4.
Received 27 April 1999; Accepted after revision 15 June 1999
Percutaneous needle biopsy of suspected primary bone neoplasms is a well-established procedure in specialist centres, with a reported accuracy in diagnosis ranging from 78% to 97%.1,2 Needle biopsy is guided using either biplane fluoroscopy1,2 or CT.3,4One study in the German literature has described the use of ultrasound (US) to guide needle biopsy in 15 patients with primary bone tumours5 and it has also been used to guide fine-needle aspiration of lytic skeletal metastases.6Saifuddin, Burnett and Mitchell7
recently reviewed the use of US in the management of patients with suspected primary bone tumours, and descri-bed their technique for US-guided biopsy.
We present the results of a study which determined the accuracy of US guidance for percutaneous needle biopsy.
Patients and Methods
Between November 1995 and November 1997, a record was kept of all patients who had needle biopsies after referral by the surgeons of the London Bone and Soft-tissue Tumour Unit. There were 144 patients (83 men, 61 women) with a mean age of 34.7 years (2 to 81 years) and all had a suspected primary bone tumour of the appendicular skel-eton, pelvis or sacrum. Before biopsy, they had plain radiography and MRI of the lesion (Fig. 1). Based on these results a decision was made by the radiologist to biopsy the lesion using either fluoroscopic, CT or US guidance (Fig. 2). Those lesions which showed a relatively large extra-osseous component (>2.0 cm in depth) were biopsied under US guidance using either a 14G Trucut needle (Baxter Healthcare Co, Deerfield, Illinois) or a 14G Temno needle (Allegiance Healthcare Co, McGaw Park, Illinois). Those which were purely intramedullary or demonstrated a rela-tively small extraosseous component were biopsied using fluoroscopic guidance with a 14G Jamshidi needle (Baxter Healthcare Co). CT with either a Trucut or a Jamshidi needle was used for those which could not be easily localised using fluoroscopy or in which the major extra-osseous component was in a difficult site for US guidance. Since the aim of the study was to determine when US could appropriately replace fluoroscopy as a guidance technique, the 29 patients biopsied using CT were not considered further. All biopsies were made through a small stab inci-sion. This left a scar which allowed identification of the site for excision of the biopsy track at the time of definitive surgery.
Patients over the age of 16 years had local anaesthesia (3 to 5 ml 1% lignocaine) to the skin and subcutaneous tis-sues. All adults were treated as outpatients, unless they had been admitted for other reasons. The 35 patients aged under 16 years were admitted as day cases and biopsied under general anaesthesia. Between two and four passes were made depending on the quality of the specimens obtained.
This allowed sufficient tissue for any special techniques required by the pathologist. All biopsies were carried out by one of two consultant radiologists (AS and RM) or, in a few patients, by a radiology trainee under direct super-vision of the consultant.
The unfixed samples were taken direct to the Department of Histopathology for imprint cytology. This has several advantages in that it gives a rapid assessment of the presence of sufficient viable tissue, and in most cases, can immediately distinguish between benign and malignant lesions. With the latter it can differentiate between primary tumours, metastases and myeloma. The use of an alkaline phosphatase stain allows a diagnosis of osteosarcoma to be made when little or no tumour osteoid is present in the sample.8Stored imprints can be used for more sophistic-ated techniques including cytogenetics.
The results were divided into three categories. In cate-gory 1 a definitive diagnosis could be made using various immunohistochemical techniques as required. In category 2 a narrow differential diagnosis could be suggested which still allowed correct surgical management as in a benign osteoclast-containing lesion in which the differential diag-nosis is between a benign fibrous histiocytoma, a solid aneurysmal bone cyst or a giant-cell tumour. Such lesions could be adequately managed by curettage with or without bone grafting or the insertion of cement into the surgical defect. In category 3 insufficient material was obtained to allow a histological diagnosis. The results of needle biopsy from patients who had been treated by surgery were
Fig. 1a
Fig. 1b
Lytic osteosarcoma of the proximal tibia amenable to US-guided biopsy. Figure 1a – An anteroposterior plain radiograph showing a poorly defined purely lytic lesion in the proximal tibial metaphysis with extension through the anterolateral cortex. Figure 1b – Coronal T1-weighted spin-echo (left) and axial T2-weighted spin-echo (right) MR images showing the intra- and extraosseous extent of the tumour. A relatively large extraosseous component is present. Areas of high signal intensity on T2 indicate necrosis which can be easily identified on US (reproduced by permission of the publisher, W B Saunders: Saifuddin A, Burnett SJ, Mitchell R. Pictorial review: ultrasonography of primary bone tumours. Clin Radiol 1998;53:239-46).
Fig. 2
Longitudinal US of the humerus in a patient with radiation-induced sarcoma. Areas of necrosis are clearly identified (curved arrows). The needle tip is seen within an area of solid tumour (small arrow) (reproduced by permission of the publisher, W B Saunders: Sai-fuddin A, Burnett SJ, Mitchell R. Pictorial review: ultrasonography of primary bone tumours. Clin Radiol 1998;53:239-46.
compared with the final histological findings from tissue obtained at operation.
For calculation of diagnostic accuracy, we used the following definitions: 1) a true-positive result in which the needle biopsy provided lesional tissue and a correct diag-nosis; 2) a true-negative result in which the needle biopsy produced no lesional tissue and no tumour was present; 3) a false-positive result when the needle biopsy provided lesional tissue which was diagnosed as tumour when no tumour was present; and 4) a false-negative result in which the needle biopsy produced no lesional tissue, but tumour was present, or there was a mismatch in the diagnosis between the needle biopsy and the surgical histology.
Results
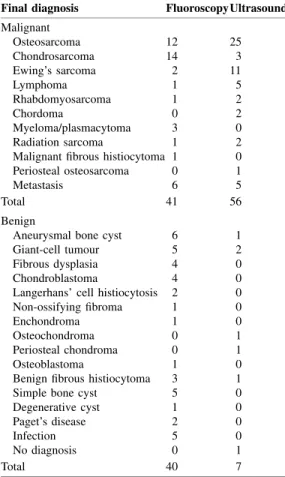
Based on the features seen on imaging, 63 lesions were considered suitable for US-guided biopsy and 81 for biopsy under fluoroscopic guidance. Table I lists the sites of the lesions. Table II gives the histological diagnoses based on needle biopsy and Table III shows the breakdown of the histological findings into the different diagnostic categories as differentiated by the guidance technique. Table IV sum-marises the diagnostic errors for those results of needle biopsy which were compared with the surgical histological findings. In seven cases, no diagnosis could be made on specimens from needle biopsy (category 3). Four of these proved to be cysts (2 aneurysmal bone cysts, 1 simple bone cyst and 1 subchondral cyst associated with osteoarthritis). Giant-cell tumour and osteoblastoma accounted for two other cases while one patient with ‘failed’ US-guided needle biopsy of a lytic lesion in the femur went on to have CT-guided needle biopsy. This also showed no diagnostic tissue and open biopsy was then undertaken which did not demonstrate tumour. The lesion was thought to represent a renal metastasis which had undergone spontaneous necro-sis. All biopsy diagnoses in category 2 were confirmed on examination of the surgical specimens. In no case did needle biopsy diagnose a benign lesion which proved to be malignant. In two cases, a low-grade malignant tumour was diagnosed on needle biopsy, but examination of the surgical specimen revealed a benign lesion. The diagnostic accuracy of needle biopsy is presented in Table V.
Discussion
Biopsy is an essential investigation for all suspected primary bone tumours after local staging.9It may be carried out either as an open operation or as a closed percutaneous procedure by an orthopaedic surgeon or a radiologist.9,10 It must, however, be undertaken in the centre where the definitive management of the patient will take place. A biopsy which has been inadequately obtained remains the commonest rea-son for inability to perform limb-salvage surgery.11
The major advantage of open biopsy is that a large amount of tissue can be obtained. Without radiological
Table III. Diagnostic category for needle biopsies comparing fluoroscopic guidance with US guidance for the 144 patients Diagnostic category 1 2 3 Total Fluoroscopy 62 14 5 81 Ultrasound 59 2 2 63 Total 121 16 7 144
Table I. Comparison of fluoroscopy and US guidance with respect to biopsy site for the 144 patients
Site Fluoroscopy Ultrasound
Femur 23 23 Tibia 14 12 Humerus 12 7 Fibula 4 5 Radius 5 1 Ulna 2 3 Ilium 1 6 Pubis 5 2 Acetabulum 2 0 Sacrum 2 2 Scapula 2 2 Clavicle 1 0 Patella 1 0 Calcaneus 1 0 Finger 5 0 Metatarsal 1 0 Total 81 63
Table II. Comparison of fluoroscopy and US guidance with respect to final diagnosis in the 144 patients
Final diagnosis FluoroscopyUltrasound
Malignant Osteosarcoma 12 25 Chondrosarcoma 14 3 Ewing’s sarcoma 2 11 Lymphoma 1 5 Rhabdomyosarcoma 1 2 Chordoma 0 2 Myeloma/plasmacytoma 3 0 Radiation sarcoma 1 2
Malignant fibrous histiocytoma 1 0
Periosteal osteosarcoma 0 1
Metastasis 6 5
Total 41 56
Benign
Aneurysmal bone cyst 6 1
Giant-cell tumour 5 2
Fibrous dysplasia 4 0
Chondroblastoma 4 0
Langerhans’ cell histiocytosis 2 0
Non-ossifying fibroma 1 0
Enchondroma 1 0
Osteochondroma 0 1
Periosteal chondroma 0 1
Osteoblastoma 1 0
Benign fibrous histiocytoma 3 1
Simple bone cyst 5 0
Degenerative cyst 1 0
Paget’s disease 2 0
Infection 5 0
No diagnosis 0 1
guidance, however, it is possible that this tissue may be either mainly necrotic or from a low-grade area of a lesion which has undergone dedifferentiation. Other disadvantages of open biopsy include the need for general anaesthesia and increased cost compared with needle biopsy which is carried out as an outpatient procedure under local anaesthesia.12 It is also associated with a higher rate of complications.11 Percutaneous needle biopsy has been criticised because of the small amounts of tissue obtained, which, it is suggested, may result in sampling errors.11The combination, however, of a needle biopsy and sections of good quality, reliable immunohistochemistry and pathologists experienced in making diagnoses from specimens of needle biopsy can result in a diagnostic accuracy as high as 97%.2 Proper placement of the biopsy allows the track to be excised at the time of surgery. Needle biopsy also preserves the perioste-um and is made through a small stab incision which leaves a scar visible to the surgeon at the time of surgery. This allows identification of the biopsy site.
Previous studies of percutaneous needle biopsy of prim-ary and metastatic bone tumours have emphasised the value of fluoroscopy and CT as guidance techniques.1-4Skrzynski et al12obtained a diagnostic accuracy of 84% in outpatients with soft-tissue lesions or bone tumours with a palpable extraosseous mass. Trucut needle biopsy was guided by palpation alone. Possible reasons considered for a failed biopsy included a sampling error, necrosis of the central tumour and a geographical miss. The value of US guidance for Trucut biopsy of certain types of primary soft-tissue tumour has been well recorded,13,14 and the extension of this technique to primary bone tumours with a relatively large extraosseous tumour mass, is logical. Most primary bone tumours arise adjacent to a major joint and any extraosseous component will be separated from the skin by periosteum, muscle and subcutaneous fat. This distance is usually between 1 and 2 cm allowing most malignant tumours to be imaged well with US.7The areas of tumour necrosis are clearly visualised and the additional use of colour Doppler will identify regions of neovascularity in the tumour, which are areas of viable tissue as opposed to
those of solid necrosis. In the case of relatively hypovas-cular tumours, such as malignant round-cell tumours and the cartilage cap of peripheral chondrosarcomas, biopsy from the margin of the lesion will increase the likelihood of obtaining a diagnostic sample. With such a technique, infiltration of adjacent skeletal muscle can also be identi-fied. A major advantage of US is the lack of risk from ionising radiation to both the patient and staff. It is also quick and relatively cheap.
Our study has shown that most aggressive malignant bone tumours, particularly osteosarcoma and malignant round-cell tumours, can easily be biopsied using US guid-ance since they are typically associated with a relatively large extraosseous mass at the time of presentation. All needle biopsies from these two groups of tumours gave a correct diagnosis. Only two US-guided biopsies were clas-sified as category 3, and as mentioned earlier, one of these was a true-negative result for the presence of viable tumour. The other was a giant-cell tumour with a relatively small extraosseous component. Biopsy of this region revealed only inflammatory tissue. US guidance was associated with a diagnostic accuracy of over 98%.
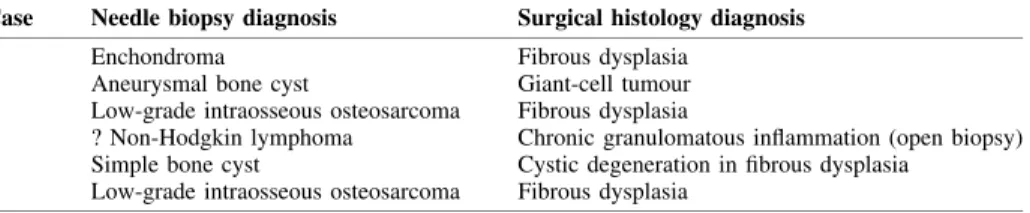
Comparison of the results of needle biopsy with surgical histology showed a diagnostic mismatch in six cases. These were all fluoroscopically-guided biopsies, the details of which are shown in Table IV. Although classed as false-negative results, only one of the misdiagnoses resulted in incorrect surgical management. Four of the biopsies which revealed no diagnostic tissue were from cysts. The diffi-culty in biopsy of such lesions has been previously docu-mented and is independent of the type of guidance technique used.1 A single fluoroscopically-guided biopsy was classed as a false-positive result. This lesion arose in the scapula and needle biopsy revealed a large number of atypical lymphocytes raising the possibility of non-Hodg-kin lymphoma. Special stains did not support this diagnosis and the patient was referred for open biopsy. Based on this, a diagnosis of chronic necrotising granuloma was made. Thus the needle biopsy result was not associated with an incorrect management decision.
Table IV. Final diagnosis in six patients in whom there was mismatch between the needle biopsy diagnosis and surgical histology
Case Needle biopsy diagnosis Surgical histology diagnosis
1 Enchondroma Fibrous dysplasia
2 Aneurysmal bone cyst Giant-cell tumour
3 Low-grade intraosseous osteosarcoma Fibrous dysplasia
4 ? Non-Hodgkin lymphoma Chronic granulomatous inflammation (open biopsy) 5 Simple bone cyst Cystic degeneration in fibrous dysplasia
6 Low-grade intraosseous osteosarcoma Fibrous dysplasia
Table V. Diagnostic accuracy of needle biopsy
Diagnostic True-positive True-negative False-positive False-negative Total accuracy (%)
US 61 1 0 1 63 98.4
Fluoroscopy 70 1 1 9 81 87.7
Our experience indicates that in carefully selected cases, US is a highly reliable alternative to fluoroscopy as a guidance technique for percutaneous needle biopsy of sus-pected bone tumours arising outside the spine. The lack of risk of ionising radiation is a major advantage to both patients and staff.
The authors would like to thank Mr S. R. Cannon and Mr T. W. R. Briggs, Consultant Orthopaedic Surgeons, Royal National Orthopaedic Hospital Trust, Stanmore, for allowing us to present data on their patients.
No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
References
1. Ayala AG, Zornosa J. Primary bone tumors: percutaneous needle biopsy: radiologic-pathologic study of 222 biopsies. Radiology 1983; 149:675-9.
2. Stoker DJ, Cobb JP, Pringle JAS. Needle biopsy of musculoskeletal lesions: a review of 208 procedures. J Bone Joint Surg [Br] 1991; 73-B:498-500.
3. White LM, Schweitzer ME, Deely DM. Coaxial percutaneous needle biopsy of osteolytic lesions with intact cortical bone. AJR Am J Roentgenol 1996;166:143-4.
4. Dupuy DE, Rosenberg AE, Punyaratabandhu T, Tan MH, Mankin HJ. Accuracy of CT-guided needle biopsy of musculoskeletal neo-plasm. AJR Am J Roentgenol 1998;171:759-62.
5. Konermann W, Wuisman P, Hillmann A, Rössner A, Blasius S.
Ultrasound guided needle biopsy for histological diagnosis of benign and malignant soft-tissue and bone tumours. Z Orthop Ihre Grenzgeb
1995;133:411-21.
6. Civardi G, Livraghi T, Colombo P, et al. Lytic bone lesions suspected for metastasis: ultrasonically guided fine needle aspiration biopsy. J Clin Ultrasound 1994;22:307-11.
7. Saifuddin A, Burnett SJ, Mitchell R. Pictorial review: ultrasono-graphy of primary bone tumours. Clin Radiol 1998;53:239-46.
8. Pringle JAS. Bone forming neoplasms arising within bone. In: Helliwell TR, ed. Pathology of bone and joint neoplasms. Volume 37. Major problems in pathology. Philadelphia:WB Saunders Co, 1998: 168-92.
9. Simon MA, Biermann JS. Biopsy of bone and soft-tissue lesions.
J Bone Joint Surg [Am] 1993;75-A:616-21.
10. Springfield DS, Rosenberg A. Editorial. Biopsy: complicated and risky. J Bone Joint Surg [Am] 1996;78-A:639-43.
11. Mankin HJ, Mankin CJ, Simon MA. The hazards of biopsy revis-ited. J Bone Joint Surg [Am] 1996;78-A:656-63.
12. Skrzynski MC, Biermann JS, Montag A, Simon MA. Diagnostic accuracy and charge-savings of outpatient core needle biopsy com-pared with open biopsy of musculoskeletal tumours. J Bone Joint Surg [Am] 1996;78-A:644-9.
13. Kissin MW, Fisher C, Carter RL, Horton LWL, Westbury G. The value of trucut biopsy in the diagnosis of soft-tissue tumours. Br J Surg 1986;73:742-4.
14. Ball AB, Fisher C, Pittam M, Watkins RM, Westbury G. Diagnosis of soft-tissue tumours by trucut biopsy. Br J Surg 1990;77:756-8.