Contractures
in Patients
With Williams
Syndrome
Paige
Kaplan,
FRCP(C),
Marc
Kirschner,
MD,
Gordon
Watters,
FRCP(C),
and M. Teresa
Costa,
FRCP(C)
From the Departments of Pediatrics and Neurology, Montreal Children’s Hospital and Research Institute, Montreal, Quebec, and the Department of Pediatrics, Hospital for Sick Children, Toronto, Ontario, Canada
ABSTRACT. Williams syndrome is a multisystem disor-der, including a characteristic facies and habitus. Intel-lectual, neurologic, and cardiovascular dysfunction occur;
vascular disease may be progressive. Joint contractures affected 10 of a group of 20 children and young adults. In 3 of 10 patients, the contractures were severe enough to interfere with daily activities; in 3 the effect was only moderate. The contractures developed in early childhood and usually did not improve or worsen with time. Large and small joints were affected and usually were symmet-rical. Their occurrence did not correlate with vascular disease. The contractures could not be attributed to a neurologic cause. Pediatrics 1989;84:895-899; Williams syndrome, joint contracture.
Williams syndrome is characterized by a distinc-tive facies and habitus and by psychomotor retar-dation. The facial appearance changes with age: in infancy, the face is usually round with periorbital fullness, upslanting palpebral fissures, lacy/stellate pattern in blue irises, flat nasal bridge, long phil-trum, and a wide mouth. As the child grows older, the lips thicken and the face becomes thinner and coarser. By adolescence and early adulthood, the face may appear quite gaunt because of a presumed
lack of subcutaneous fat. There is postnatal decel-eration of growth. Affected persons have mild to moderate psychomotor retardation with a charac-teristic personality; in infancy they may be ex-tremely irritable, but this usually resolves by the end of the first year. They later become
indiscrim-Received for publication May 23, 1988; accepted Dec 21, 1988. This is publication 88-026 of the Montreal Children’s Hospital
Research Institute.
Reprint requests to (P.K.) Division of Metabolism, Children’s Hospital of Philadelphia, 34th St & Civic Center Blvd,
Phila-delphia, PA 19104.
PEDIATRICS (ISSN 0031 4005). Copyright © 1989 by the
American Academy of Pediatrics.
inately friendly and talkative. In childhood they manifest distractibility and attention disorders. Their verbal skills and memory recall often belie their inability to write and calculate. They have hyperacusis and often are distressed by high-pitched sounds. Cardiovascular abnormalities such
as supravalvular aortic stenosis, peripheral vascular stenoses, and aortic stenoses with systemic hyper-tension are common.” Transient hypercalcemia
can sometimes be documented in the neonatal
period or in infancy. However, joint contractures have seldom been mentioned as part of the
syn-drome, although they appear to occur in many affected people. The purpose of this article is to describe contractures in 10 children and young
adults with Williams syndrome and to increase
awareness of them. The contractures were severe
enough to interfere with mobility and common daily activities in several children and caused social
em-barrassment. They were an additional cause of handicap in a multisystem disorder.
METhODS
The fmding of severe contractures in a
2-year-old girl with Williams syndrome (patient 1) led to
a search for similar abnormalities in others with the syndrome. Of 30 other patients in the files of the Montreal Children’s Hospital, 20 (10 males, 10 females) were available for study. All had the
typi-cal facies, habitus, and developmental delay de-scribed by Jones and Smith.3 Their ages ranged from 2 to 24 years. Each patient underwent a corn-plete physical examination that included anthro-pometric measurements and evaluation of move-ment at each joint. The degree of limitation at each
joint was compared with the range of movement at the contralateral joint. In addition, a thorough
TABLE. Clinical Data of Patients With Williams Syndrome and Joint Contractures* Patient No. (Montreal Children’s Hospital Sex Present Age (y) Contractures Calcium Concentration (mg/dL) (age) Cardiovascular Symptoms Onset Noted
Progressive Joints Involved Degree of Limitation
ID No.)
1 F 6 6 mos No Hips -50#{176}(L) ND Mild SAS
(741994) Knees
Ankles Fingers 1,4,5(L)
Fingers 3, 4 (R) (PIP)
extension
(R); -25 (L)
-5#{176}(L)
2 M 22 Infancy No Fingers 1, 3, 4, 5 (bilateral):
PIP & DIP
11.3 (11 mo) Normal
(279430) Wrists; elbows
Knees Ankles Scoliosis (left)
-5-40#{176}
5
3 M 18 ChildhOOd No Thumb: MP ND Normal
(413383) Fingers 2-5 (bilateral): PIP
Elbows
Knees 15#{176}
4 F 16 Birth No Fingers 4, 5 (bilateral): PIP ND SAS
(690305) Knees Kyphosis Scoliosis 10#{176} 60#{176} 30#{176}
5 F 18 Childhood No Right knee ND
(83441) Ankles
Halluces
6 F 4 Infancy No Ankles 14.4 (7 mo) Mild SAS
(735951)
7 M 24 ? No Fingers Mild ND LAS
(351606)
8 M 19 ? No Fingers: left 1, 5 Mild ND LAS
(417318)
9 F 15 Infancy No Fingers 3, 4: PIP Mild 10 (14 mo) Normal
(435712)
10 F 14 ? No Knees 45#{176} ND Normal
(504250)
CAbbreviations: ND, not done; SAS, supravalvular aortic stenosis; LAS, long segment aortic stenosis; PIP, proximal interphalangeal;
DIP, distal interphalangeal; MP, metacarpophalangeal.
and cranial computed tomography scan was done on each patient. Electromyograms were also
per-formed in 2 patients with contractures.
CASE
REPORTSThe two most severely affected patients are briefly described, the features of all patients are summarized in the Table.
Patient I (MCH 741994)
A 6-year-old girl was the product of a pregnancy of uncertain gestational length. Birth weight was 2576 g. A heart murmur was heard at birth. She fed poorly and failed to thrive in the first 3 months of life. She was
noted to have joint stiffness between
6
and 12 months of age. Her psychomotor development was delayed. When she was not yet walking at 24 months of age, she was assessed by an orthopedic surgeon who detected no ab-normalities. However, when she did start taking steps alone shortly afterward, her knees were noted to be stiff. A diagnosis of rheumatoid arthritis was made despitelack of clinical and laboratory evidence. She did not
improve with acetylsalicylic acid therapy. At 30 months
of age, Williams syndrome was diagnosed in view of the
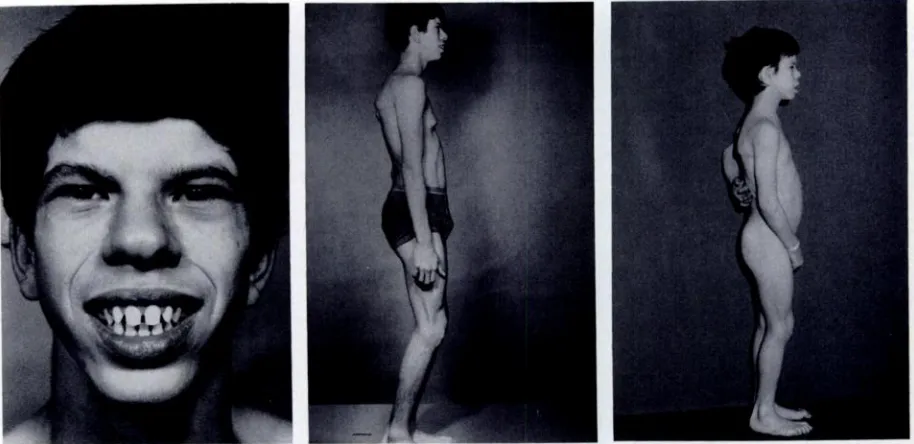
typical facies, characteristic personality, and supraval-vular aortic stenosis (Fig 1).
The girl
walked
stooped over with a wide-based gait(Fig 1, middle). She had marked limitation of movement, mainly in extension, ofthe left hip and both knees. There was milder restriction of ankles, wrists, and proximal interphalangealjoints ofthe first, fourth, and fifth fmgers on the left, and third and fourth fingers on the right (Fig 1,bottom). Neurologically, no specific abnormalities were
seen, cranial computed tomography scan appeared nor-mal, and mild diffuse disturbance was seen on an electro-encephalogram. The serum total calcium concentration was normal. There was some improvement in the mobility of her joints in the next few years. At 6 years of age she
profile (periorbital fullness, flat malar area, puffy cheeks) and umbilical protrusion. Bottom, contractures at large
and small
joints. Note stooped posture.Fig 2. Patient 2. Top, at 22 years of age, typical facies
in adulthood. Note loss of subcutaneous fat and the
widening of nasal tip compared with facies in childhood.
Middle,
contractures of large and small joints and exag-Fig 1. Patient 1. Top, at 30 months of age, typical facies in early childhood. Note periorbital puffiness, medialflare of eyebrows, thick lips, small teeth. Middle, stiff gait with limitation of joint movement. Note typical facial
there was improvement of neurologic function in the
lower limbs but the contractures of the upper limbs
persisted.
Patient 2 (MCH 279430)
A 22-year-old man (Fig 2, top) had multiple contrac-tures that had first been noted in infancy. They affected the thumb, third, fourth, and fifth fingers’ proximal and
gerated lordosis. Note typical facial profile (periorbital
fullness, flat malar area, thick lips, and small chin) and long neck. Bottom, at 8 years of age, contractures of large joints.
distal interphalangeal joints, wrists, elbows, and knees. He had tight heel cords, hyperextension of the neck, and
lordosis. These caused a stiff gait and difficulties with fine motor and some gross motor function of the hands.
The serum total calcium concentration was 11.3 mgI dL when first measured when the patient was 11 months of age, but was at a normal level when he was 3 years of age. There were no cardiovascular problems.
RESULTS
Of 20 children and young adults with Williams syndrome, 10 had joint contractures with varying degrees of severity. Details are summarized in the
Table.
In addition, among photographs of patientsnot available for examination there was one depict-ing definite, moderately severe contractures of the fingers. Severe multiple joint involvement was seen in 3 patients (1 to 3) personally examined, causing them difficulty in daily functioning in gross motor functions such as walking and climbing
stairs
and in fine hand manipulations such as buttoning clothes, writing, and using cutlery, which were often difficult and caused frustration. These patients were regarded as being clumsy. Three other patients(4
to 6) with knee and/or ankle contractures had abnormal gait but were only mildly incapacitated. They had adapted to their “disability” and corn-plained of only occasional discomfort. Sometimesthere was the need to stop an activity earlier than others. The remaining 4 patients (7 to 10) were not bothered by their finger contractures. The contrac-tures were noted early in childhood. They appeared to remain static with time except in patient 1, who improved but still had limitation in her joint mo-bility at 7 years of age, and possibly in patient 2, whose family believed that the contractures had become more severe (although this was not appar-ent in photographs taken throughout a 14-year period). Another patient (4) also had kyphosis and scoliosis.
Physical therapy had been tried in a few of the patients, in hospital and at home, but had not alleviated the limitation of mobility of the joints. However, the therapy had not been intensive or prolonged. Results of neurologic assessments, in-cluding electromyograms in 2 patients and corn-puted tomography scans in all patients, were nor-mal. The myelogram and magnetic resonance im-aging, performed in Toronto on patient 1, were not performed on the other patients.
DISCUSSION
There has been brief mention of contractures in Williams syndrome in previous reports, even in those with large numbers of patients.7 There are references to tight heel cords3’8’9 and kyphoscoliosis9 in a few patients. It is noteworthy, however, that half of our patients as well as half of a large series
reported recently by Morris et al’#{176}had joint limi-tation. Although not generally recognized as a part of the constellation of abnormalities in Williams syndrome, joint contractures are probably quite common, with less severe contractures being over-looked.
The contractures appeared to develop within the first few years of life. In general, they did not seem to progress (Fig 2), although in one girl they had improved by midchildhood. The contractures in-volved both large and small joints and usually were symmetrical. One third of the affected persons with contractures had severe involvement that affected them socially as well as physically. In our experi-ence, adolescents and young adults with Williams syndrome have sensitivity and insight into their handicaps and differences compared with their sib-lings and peers. The contractures made them ap-pear clumsy. They had difficulty performing ordi-nary daily tasks such as dressing, especially manip-ulating buttons and laces. Using cutlery, opening and closing doors, and walking up and down stairs became obstacles. Their stiff movements high-lighted an already unusual appearance, making them self-conscious in public. This limitation con-tributed to the arduous task of training them for manual occupations, because most had limited in-tellectual abilities.
The three moderately affected patients did not complain of interference with daily activities. They had involvement of large joints mainly but walked, sat, and climbed
stairs,
although in a rather awk-ward way. In this group, only one girl had involve-ment of fmgers, the fourth and fifth, and these did not interfere with fine movements such as a pincergrasp. In contrast, the mildly affected children and
their families were usually unaware of their con-tractures.
Patient 1 had an Arnold-Chiari malformation that might have explained the abnormalities in her lower limbs. However, she and six other patients had contractures in the upper limbs, suggesting a generalized connective tissue abnormality. Never-theless, the Arnold-Chiari malformation may not be coincidental because other neurologic abnormal-ities have been noted in patients with Williams syndrome (Kirschner M, Kaplan P, Watters G. Unpublished data) and it should be sought in other patients with Williams syndrome.
dysho-meostasis, which has been implicated in the path-ogenesis of the syndrome,’2”3 although there is not definite proof of this condition in these patients. In four patients, the serum calcium concentration had been measured in infancy: it was increased in one patient (14.4 mg/dL), mildy increased (11.3 mg/ dL) in another patient, and normal in the other 2 patients. However, it is accepted that hypercal-cemia may be transient and, therefore, inapparent in a person with Williams syndrome.
There did not appear to be a relationship between the severity of the contractures and cardiovascular anomalies or hypertension. Only one of the three most severely affected patients had a cardiovascular problem (mild supravalvular aortic stenosis), whereas the least affected patients had severe aortic narrowing (patients 7 and 8).
The developmental delay, coarse facies, hoarse voice, and joint contractures in patient 1 led us to consider a storage disease. Results of a skeletal survey as well as serum levels of acid hydrolases
and urinary mucopolysaccharides were normal.
In-terestingly, among 19 patients described by Jones and Smith,3 2 patients had undergone rectal biopsy for evidence of storage material that was not found. It is possible that there has not been much em-phasis on the joint contractures in Williams syn-drome because the developmental delay and vas-cular disease have overshadowed the joint prob-lems. Physical therapy may help to overcome the limitations ofjoint movement if started at an early stage and continued for long periods. Williams syn-drome should be regarded as a multisystem, pro-gressive disorder requiring early and frequent ex-aminations, with meticulous attention paid to each organ at risk for involvement. It may then be pos-sible to prevent or alleviate important physical handicaps such as contractures and hypertension,
allowing a better quality of life for persons with Williams syndrome.
ACKNOWLEDGMENTS
We thank the patients and their families for their
cooperation in these studies, Lise Vertefeuille and Suz-anne Landry for coordination of all the investigations, and Marie-France Williams, Janice Papaleo, and Isabella Fisher for preparing the manuscript. The electromy-ograins were performed by Dr Kenneth Silver.
REFERENCES
1. Daniels SR, Loggie JMH, Schwartz DC, Strife JL, Kaplan
S. Systemic hypertension secondary to peripheral vascular
anomalies in patients with Williams syndrome. J Pediatr. 1985;106:249
2. Williams RL, Azouz EM. Acetic anomalies in an adolescent
with the Williams elfm facies syndrome. Pediatr Radial.
1984;14:122
3. Jones KL, Smith DW. The Williams elfin facies syndrome.
J Pediatr. 1975;86:718
4. Vernant P, Corone P, Rossignol AM, Bielman C. Etude des
120 observations des syndromes de Williams et Beuren. Arch Mal Coeur. 1980;73:661
5. Martin NDT, Snodgrass GJAI, Cohen RD. Idiopathic
infan-tile hypercalcemia-a continuing enigma. Arch Dis Child. 1984;59:605
6. Grimm T, Wesselhoeft H. The genetic aspects of Williams Beuren syndrome and the isolated form ofthe supravalvular
aortic stenosis. Investigations of 128 families. Z KardioL 1980;69:168
7. Burn J. Williams syndrome. J Med Genet. 1986;23:309
8. Preus M. The Williams syndrome-objective definition and diagnosis. Clin Genet. 1984;25:422
9. Williams JCP, Barratt-Boyes BG, Lowe JB. Supravalvular aortic stenosis. Circulation. 1961;24:1311
10. Morris CA, Demsey SA, Leonard CO, Dilts C, Blackburn BL. Natural history of Williams syndrome: physical
char-acteristics. J Pediatr. 1988;113:318
11. Jones KL Smith’s Recognizable Patterns ofHurnan Maifor-motion. Philadelphia, PA: W B Saunders Co; 1988:106
12. Garabedian M, Jacqz E, Guillozo H, et al. Elevated
1,25-dihydroxy vitamin D concentrations in infants with
hyper-calcemia and an elfin facies. N EngI J Med. 1985;312:948-952