Team Training in the Neonatal Resuscitation Program
for Interns: Teamwork and Quality of Resuscitations
WHAT’S KNOWN ON THIS SUBJECT: Breakdowns in teamwork and communication are detrimental to neonatal resuscitations. A teamwork and error curriculum incorporated into the Neonatal Resuscitation Program may improve teamwork and the quality of resuscitations.
WHAT THIS STUDY ADDS: The 2-hour teamwork and error curriculum added to the Neonatal Resuscitation Program improved teamwork frequency and shortened the duration of simulated resuscitations immediately after training. Differences in teamwork behavior frequency persisted for at least 6 months.
abstract
+OBJECTIVE:Poor communication and teamwork may contribute to errors during neonatal resuscitation. Our objective was to evaluate whether in-terns who received a 2-hour teamwork training intervention with the Neo-natal Resuscitation Program (NRP) demonstrated more teamwork and higher quality resuscitations than control subjects.
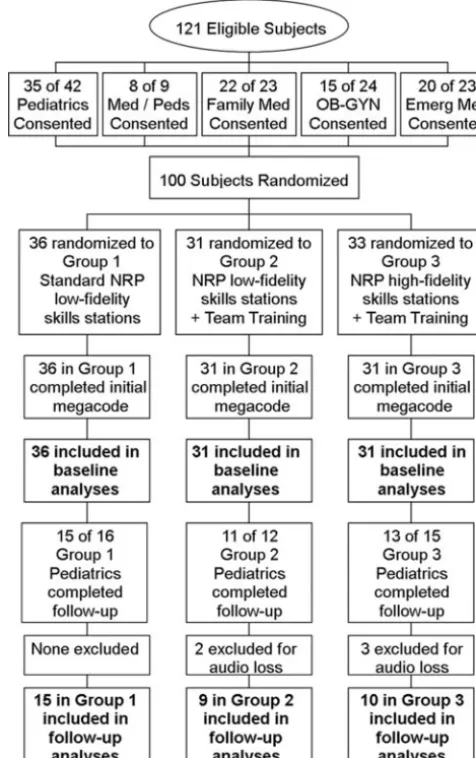
METHODS:Participants were noncertified 2007 and 2008 incoming in-terns for pediatrics, combined pediatrics and internal medicine, family medicine, emergency medicine, and obstetrics and gynecology (n⫽98). Pediatrics and combined pediatrics/internal medicine interns were eligi-ble for 6-month follow-up (n⫽34). A randomized trial was conducted in which half of the participants in the team training arm practiced NRP skills by using high-fidelity simulators; the remaining practiced with low-fidelity simulators, as did control subjects. Blinded, trained observers viewed video recordings of high-fidelity–simulated resuscitations for teamwork and resuscitation quality.
RESULTS:High-fidelity training (HFT) group had higher teamwork fre-quency than did control subjects (12.8 vs 9.0 behaviors per minute;P⬍ .001). Intervention groups maintained more workload management (con-trol subjects: 89.3%; low-fidelity training [LFT] group: 98.0% [P⬍.001]; HFT group: 98.8%; HFT group versus control subjects [P ⬍.001]) and com-pleted resuscitations faster (control subjects: 10.6 minutes; LFT group: 8.6 minutes [P ⫽ .040]; HFT group: 7.4 minutes; HFT group versus control subjects [P⬍.001]). Overall, intervention teams completed the resuscita-tion an average of 2.6 minutes faster than did control subjects, a time reduction of 24% (95% confidence interval: 12%–37%). Intervention groups demonstrated more frequent teamwork during 6-month follow-up resus-citations (11.8 vs 10.0 behaviors per minute;P⫽.030).
CONCLUSIONS:Trained participants exhibited more frequent teamwork behaviors (especially the HFT group) and better workload management and completed the resuscitation more quickly than did control subjects. The impact on team behaviors persisted for at least 6 months. Incorporat-ing team trainIncorporat-ing into the NRP curriculum is a feasible and effective way to teach interns teamwork skills. It also improves simulated resuscitation quality by shortening the duration.Pediatrics2010;125:539–546
AUTHORS:Eric J. Thomas, MD, MPH,a,bAmber L. Williams,
MS, CPH,a,bEric F. Reichman, MD, PhD,cRobert E. Lasky,
PhD,a,dSharon Crandell, MD,dand William R. Taggarte
aUniversity of Texas at Houston–Memorial Hermann Center for
Healthcare Quality and Safety, University of Texas Health Science Center at Houston, Houston, Texas; Departments ofbInternal
Medicine,cEmergency Medicine, anddPediatrics, University of
Texas Medical School at Houston, Houston, Texas; andeHuman
Factors Training and Consulting, Austin, Texas
KEY WORDS
teamwork training, neonatal resuscitation
ABBREVIATIONS
NRP—Neonatal Resuscitation Program HFT— high-fidelity training
LFT—low-fidelity training UVC— umbilical venous catheter
This trial has been registered at www.clinicaltrials.gov (identifier NCT00651794).
www.pediatrics.org/cgi/doi/10.1542/peds.2009-1635 doi:10.1542/peds.2009-1635
Accepted for publication Sep 9, 2009
Address correspondence to Eric J. Thomas, MD, MPH, 6410 Fannin St, UPB 1100, Houston, TX 77030. E-mail:
eric.thomas@uth.tmc.edu
PEDIATRICS (ISSN Numbers: Print, 0031-4005; Online, 1098-4275). Copyright © 2010 by the American Academy of Pediatrics
FINANCIAL DISCLOSURE:Mr Taggart works as a team training consultant; the other authors have no financial relationships relevant to this article to disclose.
suscitate newborns in the delivery room.1 It includes instruction about
life-saving therapies such as ventila-tion and chest compression and other beneficial treatments such as drying, warming, and stimulation2; however,
the quality of resuscitations is often suboptimal,3–5 a result in part of
poor teamwork and communication.6,7
There is broad consensus from expert groups that measuring and improving teamwork will help to improve the quality of health care.8–10Interventions
to improve teamwork and reduce devi-ations from the NRP could have a sig-nificant impact on the quality of care.
Researchers have recommended
teaching team behaviors during simu-lated neonatal resuscitations,11,12
de-veloping definitions specific for this care process,7and demonstrating that
they can be reliably measured.4The
ex-isting NRP course, taught to most care-givers in the United States who care for newborns, focuses on teaching the technical aspects of neonatal resuscita-tion with little attenresuscita-tion (1 page of the manual) paid to communication and teamwork. Adding teamwork instruction to NRP, based on crew resource manage-ment, may improve communication, teamwork, and the overall quality of neo-natal resuscitation.
This study incorporated team training into the NRP curriculum and used sim-ulation to evaluate the effectiveness of the training and the NRP performance quality. We also compared NRP with low-fidelity skills stations with NRP with high-fidelity skills stations within the team training group.
METHODS
Setting
The study was conducted in the Surgi-cal and CliniSurgi-cal Skills Center at the Uni-versity of Texas Medical School at Houston, a 14 000-ft2facility completed
in 2006. The resuscitation scenarios took place in two 400-ft2simulation theaters,
equipped with cameras and micro-phones. The NRP curriculum consists of 9 modules that cover specific skills. After completing each module, the partici-pants practiced the skills on either low-fidelity or high-low-fidelity mannequins, de-pending on the group assignment. SimBaby mannequins (Laerdal Medical Corp, Stavanger, Norway) were used in the high-fidelity skills stations. These mannequins have simulated heart tones, breath sounds, pulses, and cries.
Participants
All incoming interns for pediatrics, combined pediatrics and internal
med-icine, family medmed-icine, emergency medicine, and obstetrics and gynecol-ogy who began training in June 2007 or June 2008 and had not previously com-pleted NRP certification were eligible for participation in the study. Partici-pants who gave consent were ran-domly assigned (by Ms Williams using a random-number generator) to 1 of 3 groups: (1) standard NRP with low-fidelity skills stations (control); (2) NRP with low-fidelity skills stations and team training (LFT); or (3) NRP with high-fidelity skills stations and team training (HFT; Fig 1). Participants were randomly assigned to 3- or 4-person teams with other members from the
FIGURE 1
same study group. They remained with their teams throughout the lectures and skills stations and completed the final resuscitation simulation (mega-code) in their assigned teams. The in-stitutional review board approved all study procedures.
Intervention
A teamwork curriculum was created to advance the following learning ob-jectives: (1) to recognize the fre-quency, types, and causes of errors, both in medicine in general and in neo-natal resuscitation specifically, and (2) to understand and practice team be-haviors. The teamwork and human er-ror component was presented to LFT and HFT groups before the standard NRP course. The instructor for the teamwork training component (Mr Taggart) was an expert in team train-ing with experience in both aviation and health care. The teamwork curric-ulum lasted for 2 hours and consisted
of (1) information about human error, including limitations of human perfor-mance and the epidemiology of error in medicine and neonatal resuscita-tion; (2) examples of specific commu-nication behaviors (information shar-ing, inquiry, assertion, verbalizing intentions, workload management, vig-ilance, and leadership) used to pre-vent and manage error (Table 1); (3) other methods for improving commu-nication (using standard terminology, increasing clarity, repeating informa-tion, and sharing a mental model) and the SBAR model (situation, back-ground, assessment, and recommen-dation); and (4) customized video clips and role-playing to illustrate team-work behaviors. NRP instructors were certified and experienced in teaching NRP and were not involved in study de-sign, data collection, or analysis. Two instructors were present during each megacode simulation: 1 instructor
managed the simulator and the flow of the scenario, and the second instruc-tor acted as the facilitainstruc-tor (reading the scenario and answering designated questions). Instructors were told not to deviate from the scenarios and not to give any hints to the teams.
Baseline Resuscitation Simulations On completion of NRP lectures and skills stations, all participants (includ-ing teams who practiced skills sta-tions on a low-fidelity mannequin) per-formed a megacode on a SimBaby mannequin (high-fidelity) with their assigned team. All teams were given a brief introduction to the simulator be-fore the scenarios. Each participant led a resuscitation scenario assisted by their team members. Three stan-dardized resuscitation scenarios were developed for the study (Appendix, which is published as supporting in-formation at www.pediatrics.org/con-tent/full/125/3/539). The scenarios
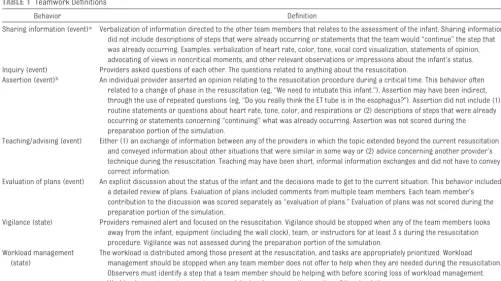
dif-TABLE 1 Teamwork Definitions
Behavior Definition
Sharing information (event)a Verbalization of information directed to the other team members that relates to the assessment of the infant. Sharing information
did not include descriptions of steps that were already occurring or statements that the team would “continue” the step that was already occurring. Examples: verbalization of heart rate, color, tone, vocal cord visualization, statements of opinion, advocating of views in noncritical moments, and other relevant observations or impressions about the infant’s status. Inquiry (event) Providers asked questions of each other. The questions related to anything about the resuscitation.
Assertion (event)b An individual provider asserted an opinion relating to the resuscitation procedure during a critical time. This behavior often
related to a change of phase in the resuscitation (eg, “We need to intubate this infant.”). Assertion may have been indirect, through the use of repeated questions (eg, “Do you really think the ET tube is in the esophagus?”). Assertion did not include (1) routine statements or questions about heart rate, tone, color, and respirations or (2) descriptions of steps that were already occurring or statements concerning “continuing” what was already occurring. Assertion was not scored during the preparation portion of the simulation.
Teaching/advising (event) Either (1) an exchange of information between any of the providers in which the topic extended beyond the current resuscitation and conveyed information about other situations that were similar in some way or (2) advice concerning another provider’s technique during the resuscitation. Teaching may have been short, informal information exchanges and did not have to convey correct information.
Evaluation of plans (event) An explicit discussion about the status of the infant and the decisions made to get to the current situation. This behavior included a detailed review of plans. Evaluation of plans included comments from multiple team members. Each team member’s contribution to the discussion was scored separately as “evaluation of plans.” Evaluation of plans was not scored during the preparation portion of the simulation.
Vigilance (state) Providers remained alert and focused on the resuscitation. Vigilance should be stopped when any of the team members looks away from the infant, equipment (including the wall clock), team, or instructors for at least 3 s during the resuscitation procedure. Vigilance was not assessed during the preparation portion of the simulation.
Workload management (state)
The workload is distributed among those present at the resuscitation, and tasks are appropriately prioritized. Workload management should be stopped when any team member does not offer to help when they are needed during the resuscitation. Observers must identify a step that a team member should be helping with before scoring loss of workload management. Workload management was not assessed during the preparation portion of the simulation.
aEvent behaviors were recorded as instantaneous events with no duration. State behaviors were recorded by using start and stop times because they continue for some duration. bFor questions that could be inquiry or assertion, inquiry was scored when the individual was seeking information (eg, “Can you check the HR?” “Can someone check for breath sounds?”), and assertion was scored when there was no information to be obtained (eg, “Can you start chest compressions?”).
did not have time to prepare their equipment before the infant was born, and 2 scenarios required volume ad-ministration when the infant did not respond to epinephrine. A debrief-ing occurred after each of the resus-citation scenarios in which the in-structors reviewed the management of the case. Video recordings were ed-ited to begin when the instructor started the scenario prompt and end immediately after the team indicated that the infant was ready to be trans-ferred to a NICU.
Teamwork Observations
Table 1 describes the teamwork be-haviors that were measured in the study and were based on previous research.4,7,13–16 Observers received
training in teamwork behavior assess-ment for⬃50 hours each. Teamwork observers, blinded to intervention status, scored resuscitation videos for the occurrence of teamwork be-haviors by using Noldus Observer XT 7.0 (Noldus Information Technology, Wageningen, Netherlands). Ten videos, randomly distributed throughout the data sets, were scored by both observ-ers to assess interrater reliability.
Teamwork observers coded the spe-cific behaviors each time they oc-curred during the resuscitations. Five behaviors were scored as discrete ver-balizations (sharing information, in-quiry, assertion, teaching/advising, and evaluation of plans). Vigilance and workload management were scored as state behaviors, with a start and end time for each occurrence of the behavior (Table 1).
NRP Performance Observations The NRP Megacode Assessment Form (Advanced) was used as a template for scoring NRP performance.1
Perfor-mance observers were blinded to
par-(10 meetings and independently scor-ing 8 videos) durscor-ing the 6-month trainscor-ing period. During meetings, the observers discussed scoring discrepancies with an investigator (Ms Williams), and scoring rules were refined when nec-essary. Like the teamwork observers, performance observers met monthly while scoring the data set for recali-bration. Twenty videos were randomly distributed throughout both observ-ers’ data sets to evaluate interrater reliability.
Noldus Observer software was also used to facilitate the recording of observations for NRP performance assessment. Performance observers scored each NRP step every time the step occurred during the resuscita-tion. Some steps occurred only once per resuscitation, but some steps, such as providing positive pressure ventilation, occurred multiple times within a resuscitation. Observers re-corded a score for each NRP step every time it was performed or should have been performed. Scores were as-signed according to the NRP Megacode Assessment form, which indicates a score of 0 when a step is omitted; 1 when the step is performed incor-rectly, incompletely, or out of order; and 2 when the step is correctly per-formed. All steps on the Megacode Assessment Form were scored, in-cluding preparing and administering epinephrine and preparing and insert-ing the umbilical venous catheter (UVC). Technique for UVC insertion was not scored because proper technique was difficult to perform on the SimBaby. UVC insertion was scored as an error only when it was incorrectly omitted or performed at the incorrect time.
Because hints from instructors could potentially influence simulation out-comes, performance observers
re-tions. Hints were defined as “com-ments from the instructor giving some indication of the step the team should perform.” Examples of hints are, “What questions do you want to ask me?” and, “You should consider intubation.” Performance observers also recorded the occurrence of “teaching moments” imposed by the instructors. If the instructor stopped the scenario for ⬎5 seconds to ex-plain a concept, then those times were marked for later removal from the total resuscitation time. Whereas hints were scored as discrete events, teaching moments were scored as states (continuing for some duration). Teaching moments often included hints, but hints frequently occurred without stopping the resuscitation for 5 seconds.
Outcome Measures
We measured 3 teamwork outcomes: teamwork event rate, vigilance per-centage, and workload management percentage. The teamwork event rate was calculated by summing the num-ber of scored teamwork events (shar-ing information, inquiry, assertion, teaching/advising, and evaluation of plans) and dividing by the total resus-citation time (in minutes). Vigilance and workload management percent-ages were calculated by summing the total time the team demonstrated each behavior and dividing by the total re-suscitation time.
When a step was not indicated for the specific resuscitation scenario (eg, meconium aspiration), that step was not scored by the observers and it was not included in the denominator for performance calculation. This pro-duced a measure of performance per-centage ranging from 0% to 100% for each resuscitation. A second outcome for this study was the time required to complete the resuscitation, another important component of neonatal re-suscitation.1The total duration for each
resuscitation was calculated from the start of the instructor’s reading of the scenario to the team’s statement that the infant should be transferred to the NICU. When any teaching moments oc-curred during the simulation, the total teaching time was subtracted from the resuscitation duration.
Follow-up Resuscitation Simulations
Interns in pediatrics and combined pe-diatrics and internal medicine (n ⫽ 43) were eligible to return for a follow-up megacode 6 months after the NRP training course. The other in-terns did not perform follow-up be-cause of scheduling conflicts. Without additional instruction, participants completed a full megacode scenario with team members from the same study arm but not necessarily from the original team. Follow-up scenarios were the same 3 scenarios as baseline resuscitations. Follow-up resuscita-tions were randomly mixed into the data set so that teamwork and quality observers were blinded to baseline or follow-up status.
Interrater Reliability
Differences were calculated between the study outcome measures scored by each observer for the reliability re-suscitation scenarios, according to the method described by Bland and Alt-man.17Mean differences between
ob-servers are presented for normally
distributed variables, and median dif-ferences are presented for nonpara-metric data. For teamwork event rates, the average difference between the 2 observers was 0.12 events per minute, and the difference ranged from⫺4.2 to 2.4 events per minute (r⫽0.85,P⫽ .002). The median difference for vigi-lance was 0%, and the difference ranged from 0% to 2% (r⫽0.58,P⫽ .079). The median difference for work-load management was 0%, ranging from⫺4% to 41% between observers (r ⫽ 0.23, P ⫽ .523). Performance score difference averaged 4%, ranging from⫺14% to 17% difference for the 20 reliability videos for the NRP observ-ers (r⫽0.68,P⫽.001). Resuscitation duration (without teaching times) had an average difference of 11 seconds; the difference ranged from⫺16 to 85 seconds (r⫽0.99,P⬍.001).
Analyses
We hypothesized that teams who re-ceived team training would demon-strate higher rates of teamwork be-haviors and higher NRP performance scores during their megacodes than would control subjects. One-way anal-ysis of variance models were calcu-lated to compare teamwork rates, NRP performance, and resuscitation dura-tion between the control subjects and the 2 team training groups. Bonferroni test of multiple comparisons was cal-culated when statistically significant differences were found between
groups. Kruskal-Wallis equality-of-proportions rank tests were calcu-lated (including ties) to compare
vigi-lance and workload management
percentages between groups because these outcomes were not normally dis-tributed. Teamwork outcomes were also compared between the LFT and HFT groups. We expected that no differ-ences would be found between these 2 groups. Follow-up megacodes were compared for all team training partic-ipants (LFT and HFT) versus control subjects to increase power. Only pedi-atrics and combined pedipedi-atrics and internal medicine interns were eligi-ble to return for follow-up. T tests were calculated to compare normally distributed outcome measures at follow-up (teamwork rate, perfor-mance, and duration), and Wilcoxon rank-sum tests were used to compare measures that were not normally dis-tributed (vigilance and workload man-agement percentages). Statistical sig-nificance was assessed at␣⫽.05. All presentedPvalues are 2-sided.
RESULTS
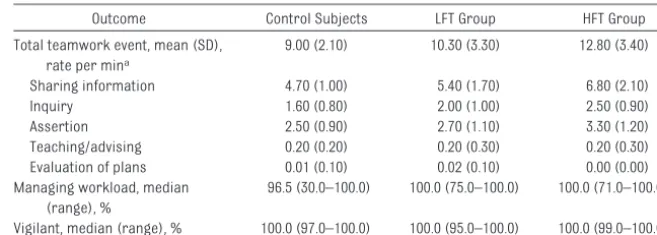
Intervention Effects on Teamwork Teamwork outcomes in all groups are included in Table 2. Teamwork event rates differed significantly among the 3 groups (P⬍.001). The HFT group had significantly higher teamwork event rates than did control subjects (P⬍ .001). Teamwork event rates did not TABLE 2 Teamwork Outcomes
Outcome Control Subjects LFT Group HFT Group Total teamwork event, mean (SD),
rate per mina
9.00 (2.10) 10.30 (3.30) 12.80 (3.40) Sharing information 4.70 (1.00) 5.40 (1.70) 6.80 (2.10) Inquiry 1.60 (0.80) 2.00 (1.00) 2.50 (0.90) Assertion 2.50 (0.90) 2.70 (1.10) 3.30 (1.20) Teaching/advising 0.20 (0.20) 0.20 (0.30) 0.20 (0.30) Evaluation of plans 0.01 (0.10) 0.02 (0.10) 0.00 (0.00) Managing workload, median
(range), %
96.5 (30.0–100.0) 100.0 (75.0–100.0) 100.0 (71.0–100.0) Vigilant, median (range), % 100.0 (97.0–100.0) 100.0 (95.0–100.0) 100.0 (99.0–100.0)
aTotal teamwork event rate is the sum of individual behavior event rates: sharing information, inquiry, assertion, teaching/ advising, and evaluation of plans.
.198). With the exception of teaching and evaluation of plans, which were rarely observed in any group, this pat-tern was consistent for all teamwork event behaviors (Table 2).
There were significant differences be-tween the groups with respect to workload management (P⬍.001) but not vigilance (P⫽ .454). Teams who received teamwork training managed the resuscitation workload better than did control subjects. The LFT group managed the workload for a median of 100% of the resuscitation, versus 96.5% for control subjects (P⬍.001). The HFT group’s median workload management was also 100% of the re-suscitation (control comparisonP⬍ .001). The effect of team training on vig-ilance is less clear. All teams main-tained vigilance for at least 95% of the resuscitation scenario.
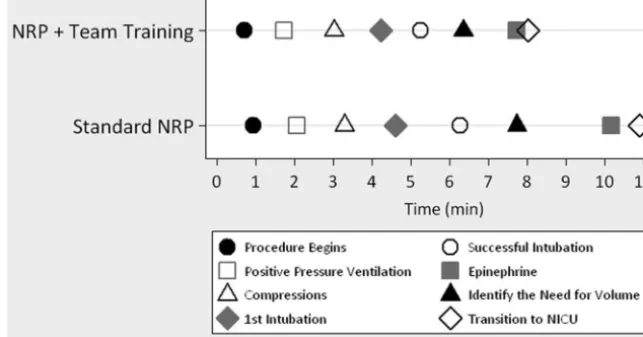
Intervention Effects on Quality There was no evidence of an associa-tion between the teamwork training intervention and NRP performance. The average performance scores were 72% for control subjects, 74% for LFT teams, and 72% for HFT teams, and none of the differences between groups were significant at the .05 level (P⫽.654). Resuscitation duration was significantly different among the 3 groups (P ⬍ .001). Control subjects took an average of 10.6 minutes to complete the resuscitation, compared with 8.6 minutes for LFT teams (control comparisonP⫽.040) and 7.4 minutes for HFT teams (control comparisonP⬍ .001). Intervention teams completed the resuscitation an average of 2.6 minutes faster than control subjects, a time re-duction of 24% (95% confidence interval: 12%–37%). Figure 2 compares specific resuscitation time points between con-trol subjects and team training groups (combined LFT and HFT).
Low-fidelity Versus High-fidelity Skills Practice
HFT teams demonstrated more team-work event behaviors than did LFT teams (P⫽.004). HFT teams were not significantly more vigilant (P⫽ .923) or more likely to manage the workload (P⫽.244) than LFT teams. We found no evidence that HFT teams differed from LFT teams in NRP performance (P ⫽ 0.999) or resuscitation duration (P⫽ .452).
Follow-up Assessments
Interns who received team training demonstrated more frequent
team-work behaviors in the 6-month
follow-up megacodes than did control subjects (mean: 11.8 vs 10.0 behaviors per minute;P⫽.030). We found no ev-idence that trained participants main-tained more vigilance (median: 100% [control subjects] vs 100% [interven-tion];P⫽.951) or workload manage-ment (median: 100% [control subjects] vs 100% [intervention];P⫽.549) than did control subjects. There were no significant differences in NRP perfor-mance at follow-up (mean: 68.9% [con-trol subjects] vs 69.6% [intervention]; P⫽.742) or in resuscitation duration, although the intervention groups had shorter duration resuscitations as they did immediately after training
(mean: 9.3 minutes [control subjects] vs 8.3 minutes [intervention]; P ⫽ .314).
DISCUSSION
Interns whose NRP course included a brief teamwork curriculum used more frequent teamwork behaviors and completed simulated resuscitations more quickly than did interns who re-ceived NRP without team training. The effect of the intervention on team be-haviors persisted for at least 6 months. This is only the second blinded, randomized trial of team training to be conducted with train-ees,15and it is the first study in any
setting to show a positive impact on both team behaviors and a measure of quality (resuscitation time).
We expected that participants who received team training would dem-onstrate more frequent teamwork behaviors during their megacodes be-cause the training focused on methods for improving communication, situa-tional awareness, and task distribu-tion, which directly correlate to the be-havior outcomes for this study. We also found that teams who received team training took less time to complete the resuscitation scenarios. This may have resulted from an increase in team be-haviors such as assertiveness or
in-FIGURE 2
quiry in team-trained groups: they were more willing to ask questions of each other or to make suggestions about the resuscitation procedure. When the newborn was not responding to the current strategy, teams who re-ceived team training were more likely to suggest a new tactic immediately. Several important milestones of re-suscitation occurred more quickly among the teams who received team training (Fig 2). It is interesting that the only randomized, controlled trial of team training among nontrainees also found a positive impact on measures of time for care processes but not other patient outcomes.18Shorter
re-suscitations in team-trained groups also explained the increase in team-work behavior rate for those groups. Because the team training did not fo-cus on task performance, it may not be surprising that the training did not im-prove the performance of NRP skills.
Within the team training group, half of the participants practiced skills sta-tions on low-fidelity mannequins and the other half practiced skills on high-fidelity mannequins. We did not expect to find differences between these groups in teamwork behaviors or re-suscitation quality during the final megacodes (all using high-fidelity mannequins); however, teams who practiced NRP skills on high-fidelity mannequins exhibited more frequent teamwork behaviors during the final resuscitation megacodes. These re-sults are consistent with previous thinking about the importance of high-fidelity simulation for teaching teamwork.11,12
During 6-month follow-up assess-ments, team-trained groups continued to demonstrate more frequent team-work than did control subjects. We were unable to detect any differences in vigilance and workload manage-ment or resuscitation quality at
follow-up. The ceiling effects for vigilance and workload management as well as the reduced follow-up sample size may have contributed to the lack of signifi-cant differences at follow-up.
A guiding principal of this research was to build on and integrate our re-search into the current NRP curricu-lum, not to create a stand-alone team training program. This is advanta-geous because with only slight modifi-cation, the widely accepted standard curriculum would become the delivery vehicle to provide team training to large numbers of health care provid-ers. Even with the team training, we remained able to complete the NRP training in 1 day, as had been the norm at our institution. We also built on ex-isting NRP practices by using the NRP’s Megacode Assessment Form and scor-ing method for 1 of our primary out-come measures.
The study has several methodologic strengths that are rarely found in team training studies and educational re-search. Participants were randomly assigned to control and intervention arms to control for confounding fac-tors, and observers were blinded. A re-cent review of team training programs for medical students and interns found no previous randomized trials.19
Outcome measurements were per-formed by highly trained individuals who made reliable assessments. Teamwork behaviors and the mega-code performance measures were re-corded by separate observers, further reducing bias. Additional measures were collected to evaluate the poten-tial effects of hints from instructors on resuscitation outcomes. The fre-quency of hints did not differ signifi-cantly between the study groups at baseline (P⫽.498) or follow-up (P⫽ .646). Finally, the behaviors that we measured were previously validated in that they are correlated with mea-sures of NRP quality.7
Although the participants for this study were not multidisciplinary teams, many residency programs con-duct NRP training in a similar manner to the study protocol. Questions re-main about whether similar training will be effective for other types of care-givers. Generalizability might be lim-ited if other sites were not able to re-create the team training content; however, it used commonly available methods knowledge.
The team training intervention was originally conceived as a curriculum to reduce errors, but the results of this study do not indicate error reduction in the intervention group. We found no differences in the NRP performance score between control subjects and participants who received team train-ing. The human error portion of the training may have had less impact on the participants than the team behav-ior components. A teamwork curricu-lum with less emphasis on error might be explored in future research.
Our intervention differs from other team training curricula in 2 important ways. The most widely known courses are TeamSTEPPS20and those delivered
by private consultants. These courses are much longer than ours, and they often do not focus on a specific care process such as neonatal resuscita-tion. It may be that brief and focused curricula, such as ours, are most ef-fective. Alternatively, the 2 approaches may be complementary. Over time, medical schools and health care orga-nizations may implement several types of team training courses in multiple contexts. This may be necessary to train properly and then maintain effec-tive teamwork skills in caregivers.
CONCLUSIONS
It is feasible to add team training to the NRP curriculum, and it results in im-proved teamwork and a marked re-duction in the time required to
haviors persisted for at least 6 months. Our results should prompt ed-ucators and the NRP curriculum com-mittee to include brief team training
generalizable to other courses, such as Advance Cardiac Life Support, Ad-vanced Trauma Life Support, and Pedi-atric Advanced Life Support.
from the dean’s office of the University of Texas Medical School at Houston and National Institutes of Health grant UL1 RR024148 (CTSA).
REFERENCES
1. Kattwinkel J, ed.Textbook of Neonatal Re-suscitation. Elk Grove Village, IL: American Academy of Pediatrics and American Heart Association; 2006
2. Tyson JE. Immediate care of the newborn infant. In: Sinclair JC, Bracken MB, eds. Ef-fective Care of the Newborn Infant. New York, NY: Oxford University Press; 1992: 21–39
3. Carbine DN, Finer NN, Knodel E, Rich W. Video recording as a means of evaluating neonatal resuscitation performance. Pedi-atrics.2000;106(4):654 – 658
4. Thomas EJ, Sexton JB, Lasky RE, Helmreich RL, Crandell S, Tyson J. Teamwork and qual-ity during neonatal care in the delivery room.J Perinatol.2006;26(3):163–169 5. Falck AJ, Escobedo MB, Baillargeon JG,
Vil-lard LG, Gunkel JH. Proficiency of pediatric residents in performing neonatal endotra-cheal intubation.Pediatrics.2003;112(6 pt 1):1242–1247
6. 2003 sentinel event data. Jt Comm Per-spect.2004;24(6):11
7. Thomas EJ, Sexton JB, Helmreich RL. Trans-lating teamwork behaviors from aviation to healthcare: development of behavioral markers for neonatal resuscitation.Qual Saf Health Care.2004;13(suppl 1):i57–i64 8. Kohn LT, Corrigan JM, Donaldson MS, eds.
To Err Is Human: Building a Safer Health System. Washington, DC: National Academy Press; 1999
9. Helmreich, RL, Schaefer HG. Team perfor-mance in the operating room. In: Bogner MS, ed.Human Error in Medicine. Hillside, NJ: Lawrence Erlbaum and Associates; 1994:225–253
10. Morey JC, Simon R, Jay GD, et al. Error re-duction and performance improvement in the emergency department through formal teamwork training: evaluation results of the MedTeams project. Health Serv Res.
2002;37(6):1553–1581
11. Halamek LP, Kaegi DM, Gaba DM, et al. Time for a new paradigm in pediatric medical education: teaching neonatal resuscitation in a simulated delivery room environment.
Pediatrics. 2000;106(4). Available at: www.pediatrics.org/cgi/content/full/106/ 4/e45
12. Weinstock P, Halamek LP. Teamwork during resuscitation.Pediatr Clin North Am.2008; 55(4):1011–1024
13. Helmreich RL, Foushee HC. Why crew re-source management: empirical and theo-retical bases of human factors training in aviation. In: Wiener EL, Kanki BG, Helmreich RL, eds. Cockpit Resource Management. San Diego, CA: Academic Press; 1993:3– 41 14. Helmreich RL, Wilhelm JA, Gregorich SE,
Chidester TR. Preliminary results from eval-uation of cockpit resource management training: performance ratings of flight crews.Aviat Space Environ Med.1990;61(6): 576 –579
15. Thomas EJ, Taggart B, Crandell S, et al. Teaching teamwork during the neonatal re-suscitation program: a randomized trial.J Perinatol.2007;27(7):409 – 414
16. Williams AL, Lasky RE, Dannemiller JL, An-drei A, Thomas EJ. Teamwork behaviors and errors during neonatal resuscitation.Qual Saf Health Care.2009 (in press)
17. Bland JM, Altman DG. Statistical methods for assessing agreement between two methods of clinical measurement.Lancet.
1986;1(8476):307–310
18. Nielsen PE, Goldman MB, Mann S, et al. Ef-fects of teamwork training on adverse out-comes and process of care in labor and delivery: a randomized controlled trial. Ob-stet Gynecol.2007;109(1):48 –55
19. Chakraborti C, Boonyasai RT, Wright SM, Kern DE. A systematic review of teamwork training interventions in medical student and resident education.J Gen Intern Med.
2008;23(6):846 – 853
DOI: 10.1542/peds.2009-1635 originally published online February 15, 2010;
2010;125;539
Pediatrics
Crandell and William R. Taggart
Eric J. Thomas, Amber L. Williams, Eric F. Reichman, Robert E. Lasky, Sharon
and Quality of Resuscitations
Team Training in the Neonatal Resuscitation Program for Interns: Teamwork
Services
Updated Information &
http://pediatrics.aappublications.org/content/125/3/539
including high resolution figures, can be found at:
References
http://pediatrics.aappublications.org/content/125/3/539#BIBL
This article cites 13 articles, 3 of which you can access for free at:
Subspecialty Collections
http://www.aappublications.org/cgi/collection/neonatology_sub Neonatology
sub
http://www.aappublications.org/cgi/collection/fetus:newborn_infant_ Fetus/Newborn Infant
s_sub
http://www.aappublications.org/cgi/collection/interdisciplinary_team Interdisciplinary Teams
_management_sub
http://www.aappublications.org/cgi/collection/administration:practice Administration/Practice Management
following collection(s):
This article, along with others on similar topics, appears in the
Permissions & Licensing
http://www.aappublications.org/site/misc/Permissions.xhtml
in its entirety can be found online at:
Information about reproducing this article in parts (figures, tables) or
Reprints
http://www.aappublications.org/site/misc/reprints.xhtml
DOI: 10.1542/peds.2009-1635 originally published online February 15, 2010;
2010;125;539
Pediatrics
Crandell and William R. Taggart
Eric J. Thomas, Amber L. Williams, Eric F. Reichman, Robert E. Lasky, Sharon
http://pediatrics.aappublications.org/content/125/3/539
located on the World Wide Web at:
The online version of this article, along with updated information and services, is
http://pediatrics.aappublications.org/content/suppl/2010/02/18/peds.2009-1635.DC1
Data Supplement at:
by the American Academy of Pediatrics. All rights reserved. Print ISSN: 1073-0397.