Making Health Care Better
Addressing the Diabetes Challenge:
Progress in Research, Prevention, Coverage, and Quality
Health Care in America
After 100 years of talk and countless failed efforts, President Barack Obama finally made health care reform a reality for America. The reforms stemming from the Affordable Care Act (ACA), along with many additional accomplishments in health care and public health under the Obama Administration, have greatly improved the United States’ health care system and created new opportunities for Americans to get and stay healthy. Thanks to the ACA, 20 million Americans have gained health coverage. For the first time ever, more than 9 in 10 Americans now have health insurance.
Real change has been made with a meaningful impact on the lives of people across the nation: Americans can no longer be denied coverage because of pre-existing conditions, women cannot be charged more just for being women, covered Americans have access to recommended preventive screenings and services without cost-sharing, and there are no more annual dollar caps on the care patients receive. Hospitals, doctors, and other providers are changing the way they operate to deliver better care at lower cost. Many Medicare beneficiaries are taking advantage of free preventive services, and have saved over $20 billion on prescription drugs since the Affordable Care Act’s enactment. Between April 2010 and May 2015, an estimated 565,000 readmissions were prevented. The Affordable Care Act has helped put Medicare on stronger financial footing for the long term.
The ACA’s critics warned that the law would cause consumer health care costs to skyrocket, drive the nation deeper into debt, and hurt our economy. Instead, the country has seen the longest stretch of private-sector job creation on record, the lowest rate of health care price inflation in 50 years, and a decline in the Federal deficit of nearly three-quarters as a share of the economy. The ability to buy quality and affordable health insurance on a competitive marketplace allows countless Americans to relocate, start businesses, and dream without worrying whether an illness will leave them bankrupt.
Diabetes in America
For decades, Americans have been committed to combating diabetes, from our finest medical researchers, to dedicated health care and public health professionals, to supportive family and friends, to patients themselves. Through this journey, while the number of people with diabetes remains far too high, we have made meaningful progress.
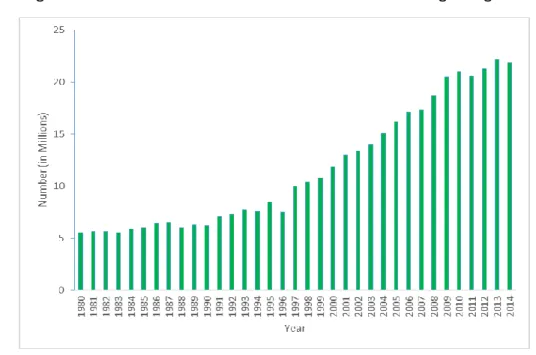
The growth in the number of individuals with diabetes is beginning to slow.1
Figure 1: CDC: Number of US Adults Aged 18 or Older with Diagnosed Diabetes, 1980-2014
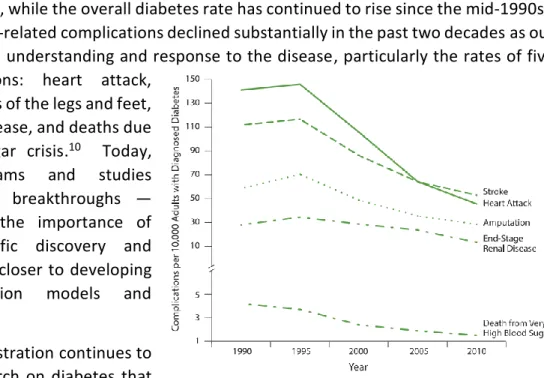
The rate of diabetes-related complications declined substantially in the past two decades.2
Thanks to the Affordable Care Act, insured Americans have access to a range of recommended preventive benefits that can help combat diabetes without out-of-pocket costs, including type 2 diabetes screening for adults with high blood pressure, blood pressure screening, and diet counseling for adults at higher risk for chronic disease. And, children at risk of becoming obese can receive screening and counseling without a copay or other cost sharing, which has the potential to lower their risk of developing diabetes as adults.3
Medicare beneficiaries lost on average 5 percent of their body weight through lifestyle alterations and increased physical activity as part of a Diabetes Prevention Program demonstration funded by the Affordable Care Act.
One contributor to recent progress was research conducted by the National Institutes of Health (NIH); NIH studies have led to new classes of drugs to treat diabetes, reductions in complications due to diabetes, and improvements in length and quality of life.
However, diabetes remains the seventh most common cause of death in America, accounting for more than 200,000 deaths per year. Since 1980, the number of adults diagnosed with diabetes has quadrupled, and among adults, about 1.4 million new cases of diabetes are diagnosed each year. This is a decrease from 1.7 million in 2012, which indicates we are beginning to move in the right direction and must continue to work to prevent new cases of type 2 diabetes. Without additional prevention efforts, it is estimated as many as 1 in 5 adult Americans could have diabetes by 2030. However, there is no known way to prevent type 1 diabetes, which accounts for approximately 5 percent of all diagnosed cases of diabetes in the United States. The prevalence of diagnosed diabetes remains higher in minority populations: half of all Hispanic men and women and non-Hispanic black women are predicted to develop diabetes. Furthermore, national expenditures for diabetes cost the United States an estimated $245 billion in 2012.4
Despite our progress, we have more work to do because too many people are still developing type 2 diabetes.
Improving the Quality and Affordability of Health Care
Diabetes prevention and treatment can be complex, and its success is often dependent on the provision of quality, coordinated health care. The ACA includes numerous provisions designed to support healthy people and overall health system improvement. The law promotes the adoption of new care models that improve care coordination, advances measurement of quality and star-rating systems that help patients choose high-performing providers, and modifies how care is paid for to promote the delivery of high-quality, efficient health care. The National Diabetes Prevention Program, established by the Centers for Disease Control and Prevention (CDC) in 2010, is based on translation of the NIH and CDC research trials which demonstrated that structured lifestyle change – healthy eating, increased physical activity, and modest weight loss – could reduce the risk of type 2 diabetes. This community-based lifestyle change program provided the foundation for the Centers for Medicare and Medicaid Services (CMS) model called the Diabetes Prevention Program, an example of a successful new care model that has reduced net Medicare spending and improved the quality of patient care. In 2011, through funding provided by the ACA, CMS awarded the National Council of Young Men’s Christian Associations of the United States of America (Y-USA) more than $11.8 million to enroll eligible Medicare beneficiaries at high risk for type 2 diabetes in the Diabetes Prevention Program. This program produced an estimated savings of $2,650 for each enrollee over a 15-month period, more than enough to cover the cost of the program. Likewise, enrolled beneficiaries experienced meaningful improvements in their health, losing about five percent of their body weight by attending training sessions that focused on long-term dietary change,increased physical activity, and behavioral changes to control their weight. These findings are relevant not only to the Medicare program, but to employers and insurers who may want to support the Diabetes Prevention Programs for their workers and enrollees. Expanding the Diabetes Prevention Program is expected to reduce net Medicare spending and improve the quality of patient care without limiting coverage or benefits.
The Administration has undertaken a number of other initiatives to improve the quality of care for individuals with prediabetes or diabetes:
CMS is helping to drive the movement towards alternative payment models in health care, which reward quality and value over volume. These models include Medicare Accountable Care Organizations (ACOs) and advanced primary care, in which providers are accountable for quality performance and total costs of care. Health care providers in these models therefore have an incentive to improve prevention, quality, and coordination in the care of beneficiaries with diabetes.5 The Medicare Shared
Savings Program, the Pioneer ACO Model, and the new Next Generation ACO Model are designed for health care organizations and providers interested in coordinating care for patients across care settings. In the second and third performance years of the Pioneer ACO model, Pioneer ACOs on average performed above the 80th percentile on diabetes quality
measures compared to national benchmarks. Similarly, Medicare Shared Savings Program ACOs on average performed above the 70th percentile compared to national benchmarks in calendar
years 2013 and 2014.
The Center for Medicare and Medicaid Innovation (Innovation Center) awarded $85 million dollars to States under the Medicaid Incentives for the Prevention of Chronic Disease (MIPCD) grant program to test the effectiveness of providing incentives directly to Medicaid beneficiaries of all ages who participate in MIPCD prevention programs, and change their health risks and outcomes by adopting healthy behaviors. Grants must address at least one of the following prevention goals: tobacco cessation, controlling or reducing weight, lowering cholesterol, lowering blood pressure, and avoiding the onset of
The YMCA has over 42,000 participants in its National Diabetes Prevention Program attending at least one session in nearly 1,500 sites across 45 States. This is one participant’s story:
Joyce’s doctor informed her she was at risk for diabetes, then referred her to the YMCA’s Diabetes Prevention Program. She joined the program just expecting to lower her A1c but soon learned she’d get so much more.
“The support from our leader and the entire group was my favorite part of the program.”
After overcoming a few obstacles, Joyce lost 24.5 pounds at the age of 79. “Eating a balanced meal at night was tough since I have no appetite, but I have a stronger resolve to control my overall health.”
YMCA DIABETES PREVENTION PROGRAM
diabetes or in the case of a person with diabetes, improving the management of the condition. Many States that received awards are testing incentives and programs that will prevent, treat, and manage diabetes among their Medicaid beneficiaries.
The ACA enhanced Medicare coverage of recommended preventive services. For example, the ACA eliminates coinsurance and deductibles for Medicare beneficiaries for preventive services like medical nutrition therapy for people with diabetes and smoking cessation. An estimated 39 million people with Medicare (including those enrolled in Medicare Advantage) took advantage of at least one preventive service with no cost sharing in 2015. In addition, Medicare beneficiaries can now get a free Annual Wellness Visit with a personalized prevention plan. Nearly 9 million people with traditional Medicare took advantage of the Annual Wellness Exam in 2015.6
More than 10 million Medicare beneficiaries with prescription drug coverage have saved more than $20 billion on prescription drugs since 2010 as a result of the ACA closing of the “donut hole.” By 2020, the donut hole will be closed completely. For people with a diabetes diagnosis who take expensive drugs like insulin products and new oral therapies, this means that certain treatments will be more affordable.7
The ACA created a new funding pool for Community Health Centers to build, expand and operate health-care facilities in underserved communities. The Health Resources and Services Administration (HRSA) oversee the Health Center grantees, which serve more than 23 million patients and have received $11 billion from the Community Health Center Fund to offer a broader array of primary care services, extend their hours of operations, hire more providers, and renovate or build new clinical spaces. 8 The ACA also supported
Community Health Centers in improving their data-driven, quality improvement infrastructure, including Electronic Health Record (EHR) adoption and Patient-Centered Medical Home (PCMH) transformation which has led to improvements in quality metrics, including preventive care measures. 65.1 percent of health centers have received PCMH recognition and 92 percent of health centers have an EHR installed at all sites.
Since 2009, the Substance Abuse and Mental Health Services Administration (SAMHSA) funded more than 187 grantees in their Primary and Behavioral Health Care Integration (PBHCI) grant program. The purpose of the PBHCI program is to improve the physical health status of adults with serious mental illnesses (SMI) by supporting communities to coordinate and integrate primary care services into publicly funded community mental health and other community-based behavioral health settings. The PBHCI population has much higher health risks as compared to the general population. At intake, individuals receiving PBHCI services had two times the rate at risk or having diabetes; three times the rate at risk or having high cholesterol; almost double the rate at risk of having hypertension; and triple the rate of smoking. The program has received funds from the Prevention and Public Health Fund, established by the ACA.
New Solutions through Research: Preventing, Treating,
and Curing Diabetes
In the United States, while the overall diabetes rate has continued to rise since the mid-1990s9,
the rate of diabetes-related complications declined substantially in the past two decades as our nation improved its understanding and response to the disease, particularly the rates of five major complications: heart attack,
stroke, amputations of the legs and feet, end-stage renal disease, and deaths due to high blood sugar crisis.10 Today,
innovative programs and studies continue to yield breakthroughs — reminding us of the importance of supporting scientific discovery and moving our nation closer to developing effective prevention models and treatment.
The Obama Administration continues to support vital research on diabetes that builds on this progress. The ACA requires CDC to issue a diabetes report card every
two years with the latest data about diabetes and prediabetes, preventive care practices, risk factors, quality of care, diabetes outcomes, and trend and State data. New technologies and strategic investments prevent the onset of diabetes and enhance the quality of life for many individuals living with diabetes today. In 2015, President Obama announced his plan to usher in a new era of discovery. By investing in new research methods that will enable clinicians to tailor treatments to individual patients, the Precision Medicine Initiative will revolutionize how our nation combats disease, including diabetes.
Funding for diabetes research and prevention programs under this Administration remains strong. The National Institutes of Health’s (NIH) annual funding for diabetes totals more than $1 billion per year.11
Because of these investments, NIH research initiatives during the Obama Administration have produced exciting results such as:
NIH research made possible by the Special Statutory Funding Program for Type 1 Diabetes Research (Special Diabetes Program) includes progress from clinical trials testing approaches to delay or prevent type 1 diabetes; recent advances toward the development of an artificial pancreas — technology to automate blood glucose sensing and insulin administration; progress on islet transplantation as a treatment approach for people with difficult-to-control type 1 Figure 2: CDC: Trends in Rates of Diabetes Complications Among US
diabetes; progress toward producing large quantities of insulin-producing cells in the laboratory for cell replacement therapies; and results of a trial testing different treatments for diabetic eye disease. The Special Diabetes Program was recently extended through Fiscal Year 2017. With the new funding, the Special Diabetes Program is poised to continue its track record of supporting cutting-edge type 1 diabetes research.12
The Food and Drug Administration (FDA) and NIH are working to help advance the development of artificial pancreas technologies. For example, the NIH vigorously supports basic, translational, and clinical research to develop, test, and optimize artificial pancreas systems and their components. The FDA is prioritizing the review of artificial pancreas research protocol studies, providing clear guidelines to industry, setting performance and safety standards, fostering discussions between government and private researchers, and finding ways to shorten study and review time. The NIH and FDA have also co-sponsored scientific workshops to propel progress in this field. Artificial pancreas technology would fully automate blood glucose sensing and insulin administration, and has the potential to help people with type 1 diabetes achieve recommended levels of blood glucose control and alleviate an enormous amount of burden that is currently associated with managing the disease.
Recent pharmacogenetic studies have yielded important information on how variants affecting metformin transporters and gene expression control sites modulate drug responses. NIH-supported research led to the discovery that oral sulfonylurea therapy can be used to treat children with certain forms of neonatal diabetes. Thus, children once treated with insulin (via multiple injections each day or an insulin pump) now take an oral medication to treat their diabetes, which greatly improves quality of life for patients and their families. In addition, the FDA approved many innovative drugs and devices for prevention, detection, and treatment including:
The first insulin pump to automatically suspend insulin delivery when the device detects that a patient has low blood glucose levels, preventing additional insulin delivery, which can further lower the patients’ blood glucose, causing coma and even death.
Eleven new molecular entities, which include several new therapeutic classes, and which have greatly expanded the range of therapeutic options for patients with diabetes.
Intragastric balloons, endoluminal sleeve devices, and endoscopically placed magnets for the treatment of morbid obesity that although not indicated for the treatment of diabetes, reduction in obesity is well-established as an important factor in the management and prevention of type 2 diabetes.
Creation of a novel regulatory pathway to allow for rapid innovation of diabetes-specific mobile applications that alert friends and family members of patient’s glucose values. This is a life-saving technology that allows for prompt intervention when patients are experiencing, or are about to experience, acute complications from their diabetes that could lead to brain
These examples represent only a few of the many advancements in research and prevention achieved during this Administration.
In addition, the President’s Precision Medicine Initiative was launched in 2015. Building on the $200 million investment in 2016, the President’s fiscal year 2017 budget proposed a $100 million increase to:
Develop a voluntary national research cohort of a million or more individuals to propel our understanding of health and disease and set the foundation for a new way of doing research through engaged participants and open, responsible data sharing.
Scale up capacity to identify lifestyle, environmental, genomic, and other drivers of diseases like diabetes and apply that knowledge toward developing more effective approaches to prevention and therapy.
Advance the development of high quality, curated databases, and technology to support the regulatory structure needed to advance innovation in precision medicine and protect public health.
Support the development of interoperability standards and requirements that address privacy and enable secure exchange of data across systems, and will help devices work together to allow for seamless exchange of data between devices, patients, and health care providers.
Catalyze research by providing patient-generated data about chronic conditions like diabetes, and by engaging specific Cohort subpopulations to enroll in research to develop and test improved prevention and treatment strategies.
Improvements in Prevention and Detection
We can all take steps towards reducing our chances of developing pre-diabetes and diabetes by maintaining a healthy weight, staying physically active, and eating a balanced diet. It is also important to understand our risk factors and access preventive services that can help to detect this disease early. When an individual is identified as being at-risk of developing type 2 diabetes, actions can be taken to prevent the onset of the disease.
This Administration has invested in prevention and improving public understanding of risk factors and promoting healthy lifestyles. And, it has put laws like the ACA in place to ensure that evidence-based screenings and treatment are available and affordable.
This Administration has continued to invest in prevention and early detection as a public health priority:
The ACA established the Prevention and Public Health Fund (PPHF) to provide expanded and sustained national investments in prevention and public health, to improve health outcomes, and to enhance health care quality.13
CDC Prevention Fund investments to prevent type 2 diabetes and reduce its complications involve coordinated strategies that States, national, community, and tribal organizations are implementing to improve outcomes for people with prediabetes and diabetes.
Preventing Type 2 Diabetes Among People at High Risk funds six national organizations to expand and sustain the National Diabetes Prevention Program by establishing a lifestyle change program in multiple States. Over 840 CDC-recognized programs across 48 States and District of Columbia have reached over 37,000 people with prediabetes. By participating in a CDC-recognized diabetes prevention program, people with prediabetes can learn to make practical, real-life changes and cut their risk for developing type 2 diabetes by as much as 58 percent.
Through the National Diabetes Surveillance System, CDC analyzes national trends and provides State and county data. Public health professionals and communities can use these data to focus their diabetes prevention and control efforts on areas of greatest need. CDC connects State and Local health departments across the United States by monitoring disease patterns and sharing information that improves State responses to diabetes.14
The U.S. Administration for Community Living supports an initiative focused on Chronic Disease Self-Management Education, enabling older
Americans with chronic diseases, including diabetes, to better manage their conditions and take control of their health. Grantees include state agencies, nonprofit organizations, and educational institutions, who collaborate with local partners to increase availability of these proven programs, especially among low-income, minority, and other underserved populations. Local partners include senior centers, health care organizations, faith-based organizations, libraries, YMCAs, and senior housing. Since 2010, approximately 275,000 participants have been reached, with nearly one-third of participants reporting relevant data
CDC National Diabetes
Prevention Program
Funded by CDC, the American Association of Diabetes Educators has expanded the National Diabetes Prevention Program to over 40 sites, including Choctaw Nation, across 15 States.
A participant’s view:
"I am writing this letter to give some insight as to why I needed this class and why I feel it has made a drastic, much-needed change in my life. I was informed that if I did not make some life changes I would be a stage [type] II diabetic in the next three years. At the age of 43 this was a huge shock to me! Choctaw Diabetes Prevention Class has turned all of this around for me. Through the weekly meetings I was held accountable to a group of peers as well as myself and the Lifestyle Coaches. I was educated on the importance of the effect of not only eating healthy and making the right choices for myself, but exercise and activity. During the weekly meetings I had actually lost 30+ pounds and have been taken off of one of my high blood pressure medications. This was all made possible through information and sharing with the class during the 16 sessions and continues on with the post core sessions. To the ‘Choctaw Nation’: Thank you for the opportunity to participate in such a ‘life changing’ class, my family and I cannot thank you enough."
In all 50 States, the District of Columbia, six Pacific territories/former territories, Puerto Rico, and the U.S. Virgin Islands, CDC funding and technical assistance for diabetes programs support activities to improve health outcomes for people living with diabetes by preventing health complications among those most at risk; adopt diabetes care guidelines in health care settings; help State Medicaid programs monitor quality care outcomes among people with diabetes; educate health care providers, public health professionals, and the public about optimal diabetes care and self-management; and involve communities in diabetes prevention and control activities.16
The Partnerships Active in Communities to Achieve Health Equity Program in the Office of Minority Health seeks to improve health outcomes among racial and ethnic minorities through community based networks that adopt evidence-based disease management and preventive health activities and increase access to and use of preventive health care, medical treatment, and supportive services. Several grantees are working to improve the prevention, detection, and management of diabetes.17
State Public Health Actions to Prevent and Control Diabetes, Heart Disease, Obesity and Associated Risk Factors and Promote School Health provides resources to States to raise awareness of type 2 diabetes risk and securing coverage of the National Diabetes Prevention Program for State/public employees. Efforts have contributed to more than a million total covered lives.
State and Local Public Health Actions to Prevent Obesity, Diabetes, and Heart Disease and Stroke intensifies work in 17 State and four large city health departments through type 2 diabetes prevention programs, systems and environmental changes that support healthy choices.
A Comprehensive Approach to Good Health and Wellness in Indian Country supports twelve American Indian tribes and Alaska Native villages and eleven Tribal Organizations using community-chosen and culturally adapted public health interventions to encourage healthy eating through planting and harvesting traditional foods; increasing physical activity within Native communities and educating individuals about the National Diabetes Prevention Program.
The Special Diabetes Program for Indians (SDPI) offered by the Indian Health Service is a $150 million annual program that provides grants for diabetes prevention and treatment services to 400 IHS, tribal, and urban health programs for Native Americans. The SDPI has three major components: community-directed grants for diabetes prevention and
treatment, Diabetes Prevention and Healthy Heart Initiative grants, and data infrastructure improvement for the IHS.18
Let’s Move! is a comprehensive initiative, launched by the First Lady, dedicated to helping
kids and families lead healthier lives. Let’s Move! is about putting children on the path to a healthy future during their earliest months and years; giving parents helpful information and fostering environments that support healthy choices; providing healthier foods in our schools; ensuring that every family has access to healthy, affordable food; and, helping
children become more physically active. Nearly 80 million people – or nearly 1 in 4 Americans – now live in a Let’s Move! City, Town or County where children can walk to school on new sidewalks, participate in a summer meal program, or join a local athletic league.19 Developing
these healthy habits in children can help prevent the onset of diabetes at a young age.20
Through the National School Lunch Program and the School Breakfast Program, over 30 million children have access to healthier school breakfasts and lunches.21
Ensuring Access to Health Care
Access to quality, affordable health care is essential in the fight against diabetes. The average cost of care for a person with diabetes can reach up to $13,700 per year, of which about $7,900 is directly attributed to diabetes.22 Those affected by
diabetes should not have to choose between health care and other basic needs. That is why this Administration fought so hard for the ACA, which has helped 20 million uninsured Americans gain the security they deserve.
Under the ACA:
As many as 129 million Americans with pre-existing conditions, including diabetes, can no longer be denied coverage or charged more because of their health or family health history.
Annual and lifetime dollar limits on coverage of essential health benefits, which could disrupt diabetes treatments, are prohibited for most plans.
Out-of-pocket costs for consumers enrolled in non-grandfathered coverage are limited, ensuring financial stability even in the face of a costly illness like diabetes. Consumers enrolled in non-grandfathered coverage have
the right to appeal decisions made by their health plan to external review.
Under the ACA, most health insurance plans are required to provide coverage for recommended preventive services without cost sharing. This includes services such as obesity screening for children and certain diabetes screening and counseling. Getting recommended preventive services is a key step to good health in preventing type 2 diabetes or in
The Affordable Care Act prohibits health insurance companies from denying or charging more for coverage because of an individual’s health or family history. Here is one story that represents the countless people with diabetes who gained coverage under the ACA.
“I was floored by what I saw. I filled out the simple questionnaire on the website to see my options. They asked me about my age, my income, my family size. And that was it. No medical history. No ‘Do you have diabetes?’
It’s an amazing feeling — I felt liberated. Even now, I get chills just thinking about that feeling of, ‘Hey, you’re just one of us now.’ It’s incredible. It’s profoundly American, to feel like I have choices and the freedom to
THANKS TO THE AFFORDABLE CARE ACT
when steps can be taken to manage or avoid developing the disease altogether.
More Americans with insurance means more people are receiving obesity and cholesterol-level screenings. Nearly 8 in 10 people with insurance had their cholesterol cholesterol-level checked within the past five years, compared to about half of all individuals without health insurance.23 High cholesterol levels can raise an individual’s risk of developing diabetes.
If all States expanded Medicaid, hundreds of thousands more people would have access to recommended preventive services. In this scenario, each year more than 600,000 people would receive cholesterol-level screenings, once expanded coverage was fully in effect. States that have already expanded Medicaid will achieve these outcomes for an additional 600,000 people.24
Our Work is Not Over
Legislative and executive actions are continuing to advance the goal of quality, affordable, and accessible health care and public health for all Americans. Along with patients, consumer advocates, researchers, and health care professionals who tirelessly battle this disease every day, together, we as a nation continue to invest in, and work for, better prevention, detection, and treatment of diabetes — and look toward a future free of the disease.
1 Centers for Disease Control and Prevention, National Center for Health Statistics, Division of Health Interview Statistics, data from the National
Health Interview Survey. Statistical analysis by the Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Division of Diabetes Translation. http://www.cdc.gov/diabetes/statistics/prev/national/figadults.htm Accessed March 30, 2016.
2 National Institute of Diabetes and Digestive and Kidney Diseases. NIDDK Recent Advances & Emerging Opportunities: Diabetes, Endocrinology, and Metabolic Diseases. January 2016.
http://www.niddk.nih.gov/about-niddk/strategic-plans-reports/Documents/3_2016FebDoc_FINAL_DEM_508c.pdf
3 HealthCare.gov. Preventive Health Services. 2016. https://www.healthcare.gov/coverage/preventive-care-benefits/ 4 Centers for Disease Control and Prevention. 2014 Diabetes Report Card. 2014.
http://www.cdc.gov/diabetes/pdfs/library/diabetesreportcard2014.pdf
5 Centers for Medicare and Medicaid Services, “Accountable Care Organizations (ACOs): General Information,”
https://innovation.cms.gov/initiatives/aco/
6 Centers for Medicare and Medicaid Services, "More than 10 million people with Medicare have saved over $20 billion on prescription drugs
since 2010," news release, February 8, 2016, https://www.cms.gov/Newsroom/MediaReleaseDatabase/Press-releases/2016-Press-releases-items/2016-02-08.html
7 Centers for Medicare and Medicaid Services, "More than 10 million people with Medicare have saved over $20 billion on prescription drugs
since 2010," news release, February 8, 2016, https://www.cms.gov/Newsroom/MediaReleaseDatabase/Press-releases/2016-Press-releases-items/2016-02-08.html
8 U.S. Department of Health and Human Services, During National Health Center Week, HHS announces an additional $169 million in Affordable Care Act funding to 266 community health centers. News release. August 11, 2015. http://www.hhs.gov/about/news/2015/08/11/hhs-announces-an-additional-169-million-in-affordable-care-act-funding-to-266-community-health-centers.html
9 National Institute of Diabetes and Digestive and Kidney Diseases. NIDDK Recent Advances & Emerging Opportunities: Diabetes, Endocrinology, and Metabolic Diseases. January 2016.
http://www.niddk.nih.gov/about-niddk/strategic-plans-reports/Documents/3_2016FebDoc_FINAL_DEM_508c.pdf
10 Centers for Disease Control and Prevention. 2014 Diabetes Report Card. 2014.
http://www.cdc.gov/diabetes/pdfs/library/diabetesreportcard2014.pdf
11 U.S. Department of Health and Human Services, Research Portfolio Online Reporting Tools. Estimates of Funding for Various Research, Condition, and Disease Categories (RCDC). February 10, 2016. http://report.nih.gov/categorical_spending.aspx.
12 National Institute of Diabetes and Digestive and Kidney Diseases. NIDDK Recent Advances & Emerging Opportunities: Diabetes, Endocrinology, and Metabolic Diseases. January 2016.
http://www.niddk.nih.gov/about-niddk/strategic-plans-reports/Documents/3_2016FebDoc_FINAL_DEM_508c.pdf
13 U.S. Department of Health & Human Services. "Prevention and Public Health Fund." Last modified April 30, 2015.
http://www.hhs.gov/open/prevention/index.html
14 Centers for Disease Control and Prevention. Diabetes. http://www.cdc.gov/diabetes/data/ 15 U.S. Administration for Community Living. Chronic Disease Self-Management Programs.
http://www.aoa.gov/AoA_Programs/HPW/ARRA/PPHF.aspx
16 Centers for Disease Control and Prevention. State Public Health Actions to Prevent and Control Diabetes, Heart Disease, Obesity and Associated Risk Factors and Promote School Health. http://www.cdc.gov/chronicdisease/about/state-public-health-actions.htm
17 Office of Minority Health. Grantee Best Practices and Promising Approaches. http://minorityhealth.hhs.gov/omh/browse.aspx?lvl=3&lvlid=23 18 Indian Health Service. Special Diabetes Program for Indians. http://www.ihs.gov/MedicalPrograms/Diabetes/?module=programsSDPI 19 Let’s Move. Parents Have the Power: First Lady Hosts Parenting Blogger Event.
http://www.letsmove.gov/blog/2016/03/16/parents-have-power-first-lady-hosts-parenting-blogger-event
20 Let’s Move. Child Nutrition Program. http://www.letsmove.gov/child-nutrition-programs 21 Let’s Move. Child Nutrition Program. http://www.letsmove.gov/child-nutrition-programs
22 American Diabetes Association. Cost of Diabetes. http://www.diabetes.org/advocacy/news-events/cost-of-diabetes.html
23 Sara R. Collins et al., The Rise in Health Care Coverage and Affordability Since Health Reform Took Effect: Findings from the Commonwealth Fund Biennial Health Insurance Survey, 2014, 7, January 2015, http://www.commonwealthfund.org/~/media/files/publications/issue-brief/2015/jan/1800_collins_biennial_survey_brief.pdf
24 The White House Council of Economic Advisors. Missed Opportunities: TheConsequences of State Decisions Not to Expand Medicaid.
2015. https://www.whitehouse.gov/sites/default/files/docs/medicaidmissedopportunities2015_final_v3.pdf