Available
online
at
www.sciencedirect.com
j o ur na l ho me p ag e :h t t p : / / w w w . e l s e v i e r . c o m / l o c a t e / r p o r
Original
article
Results
of
combined
radiotherapy
and
hormonal
treatment
of
prostate
cancer
patients
with
initial
PSA
value
>40
ng/ml
Kube ˇs
Jiri
a,∗,
Cvek
Jakub
b,
Vondráˇcek
Vladimir
a,
Dvoˇrák
Jan
a,
Argalacsová
Sona
a,
Navrátil
Matej
a,
Buˇril
Jan
aaInstituteofRadiationOncology,FacultyHospitalNaBulovceand1stFacultyofMedicine,CharlesUniversity,Budínova2,Prague8, 18000,CzechRepublic
bOncologicalClinic,FacultyHospitalOstrava,17.listopadu1790,Ostrava-Poruba70852,CzechRepublic
a
r
t
i
c
l
e
i
n
f
o
Articlehistory:Received28November2011 Receivedinrevisedform 14December2011 Accepted15January2012 Keywords: Prostatecancer PSA Highrisk Radiotherapy
a
b
s
t
r
a
c
t
Aim:ToevaluatetheoutcomeofprostatecancerpatientswithinitialPSAvalue>40ng/ml. Background:TheoutcomeofprostatecancerpatientswithveryhighinitialPSAvalueisnot knownandpatientsarefrequentlytreatedwithpalliativeintent.Weanalyzedtheoutcome ofradicalcombinedhormonaltreatmentandradiotherapyinprostatecancerpatientswith initialPSAvalue>40ng/ml.
Methods:BetweenJanuary2003andDecember2007wetreated, withcurativeintent,56
patientswithnon-metastaticprostatecancerandinitialPSAvalue>40ng/ml.The treat-mentconsistedoftwomonthsofneoadjuvanthormonaltreatment(LHRHanalog),radical radiotherapy(68–78Gy,conformaltechnique)andanoptionaltwo-yearadjuvanthormonal treatment.
Results:Themediantimeoffollowupwas61months.5-Yearoverallsurvivalwas90%.5-Year biochemicaldiseasefreesurvivalwas62%.Tstage,Gleasonscore,PSAvalue,and radiother-apydosedidnotsignificantlyinfluencetheoutcome.Lategenitourinalandgastrointestinal toxicitywasacceptable.
Conclusion:Radicaltreatmentincombinationwithhormonaltreatmentandradiotherapy
canberecommendedforthissubgroupofprostatecancerpatientswithgoodperformance statusandlifeexpectancy.
©2012GreaterPolandCancerCentre,Poland.PublishedbyElsevierUrban&PartnerSp. z.o.o.Allrightsreserved.
Background
Theprostatespecificantigen(PSA)isthemainfactorin defin-ing the extent and prognosis of disease in patients with
∗ Correspondingauthorat:InstituteofRadiationOncology,FacultyHospitalNaBulovceand1stFacultyofMedicine,CharlesUniversity,
Budínova2,Prague8,18000,CzechRepublic.Tel.:+420777661574;fax:+420283840873. E-mailaddress:jiri.kubes@fnb.cz(J.Kubeˇs).
prostatecancer.Theriskoflocallyadvanceddisease,1lymph nodemetastasisanddistantbonemetastasis2increasewith risingPSAvalue.Thepredictionvalueofnomogramsfor dis-easeextentpredictiondecreaseswithincreasingPSAvalue.3 HighinitialPSAvaluecanoccurintheabsenceofmetastatic
1507-1367/$–seefrontmatter©2012GreaterPolandCancerCentre,Poland.PublishedbyElsevierUrban&PartnerSp.z.o.o.Allrightsreserved.
diseaseinduced,forexample,byinflammationoftheprostate, butvaluesareusuallynotveryhigh.4Amoreaccurate diagno-sisis,insuchcases,difficultandpotentiallyusefulmethods maybenatrium-fluoridPETscanningforthedetectionofbone metastasis5,6oraPETscanwith11C-cholin.7,8These examina-tionsarenotstandardtoday,however.
PatientswithanextremelyhighPSAvalueareoftentreated withpalliativeintent.Themainriskofthisapproachisthe progressionof localized disease and side-effects accompa-nyingpermanenthormonalblockade.Onthe otherhand,a radical approachwith radical radiotherapy carriesthe risk of overtreatment, early progression outside the treatment volume,and side-effectsofradical radiotherapy. The addi-tionofradiotherapytothepermanent hormonaltreatment increasedoverall survivalofpatientswithlocallyadvanced prostate cancer9 and the addition of hormonal therapy to radiotherapyincreasedoverallsurvivalofhighriskprostate patients.10,11 Thequestionremains,iftheradicaltreatment approachisalsosuitableforpatientswithextremelyhigh ini-tialPSAvalue.
Aim
Theaimofthisworkistoevaluatetreatmentresultsinagroup ofprostatecancerpatientswithinitialPSAvalue>40ng/ml.
Materials
and
methods
BetweenJanuary2003and December2007wetreated, with curativeintent,56patientswithnon-metastaticprostate can-cerandaninitialPSAvalue>40ng/ml.Staginginvestigations included PSA, biopsy,CT or MRI scan of pelvis, and bone scan.Themaincharacteristicsofthepatientgroupare out-lined in Table 1. The treatment consisted of neoadjuvant hormonaltreatment(2months,LHRHanalog),radiotherapy andoptionaladjuvanthormonaltreatment(antiandrogen2 years).Themaincharacteristicsofthetreatmentareoutlined inTable2.Thetreatmentwasperformedonlinear acceler-atorswithanominalphotonbeamenergyof6MeV,usinga conformal3Dtechnique.Clinicaltargetvolumefortheinitial phaseoftreatmentincludedthepelvicregionwithboosttothe prostate/seminalvesiclesduringthesecondphaseorprostate
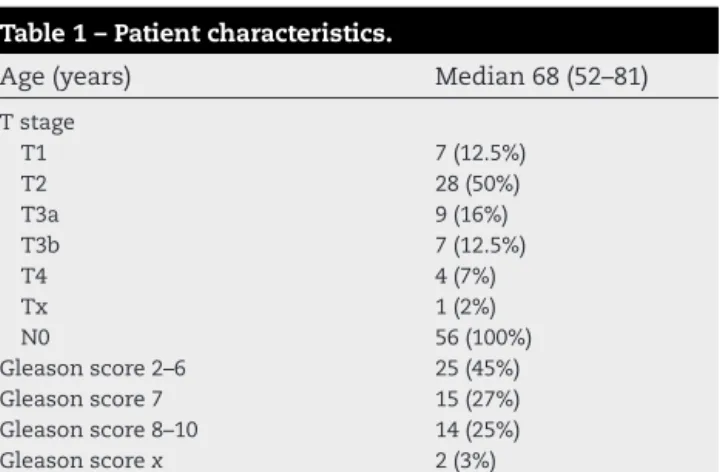
Table1–Patientcharacteristics.
Age(years) Median68(52–81)
Tstage T1 7(12.5%) T2 28(50%) T3a 9(16%) T3b 7(12.5%) T4 4(7%) Tx 1(2%) N0 56(100%) Gleasonscore2–6 25(45%) Gleasonscore7 15(27%) Gleasonscore8–10 14(25%) Gleasonscorex 2(3%) PSA(ng/ml) Median68ng/ml(42–276)
Table2–Proportionoftreatmentmodalities.
Neoadjuvanthormonal treatment Yes55(98%),No1(2%) Adjuvanthormonal treatment Yes37(66%),No19(34%)
Radiotherapy—volume Pelvis48(86%),prostate8(14%)
Radiotherapy—dose(Gy) Median74Gy(68–78Gy)
gland/seminalvesiclesonly,dependentonthedecisionofthe
physician.Thedosewas44–50Gy/22–25fractionsforthepelvic
regionand24–28Gy/12–14fractionsfortheprostate±seminal
vesicles. The totaldose was 68–78Gy/7–8 weeks.The dose
wasnormalizedtothemaximuminPTVand thedosewas
prescribedtothereferenceisodose(usually93%).Acuteand
latetoxicitywasevaluatedaccordingtotheRTOGscale.The
follow-upinvestigationswereperformedat3–6months
inter-valswithPSAexamination,physicalexamination,andcontrol
CT/MRIofpelvis,andbonescaninthecaseofPSAelevation.
PSArelapsewasassessedaccordingtothePhoenixcriteria.
Statistics
Overall survival(OS) and biochemical disease freesurvival
(bDFS)werecalculatedusingtheKaplan–Meiermethod.
Uni-variateanalysisofpredictivefactorswasundertakenusingthe
Mantel-Coxtest.Thelog-ranktestprovidedastatistical
com-parisonoftwogroups.Ap-value<0.05wasconsideredtobe
significant.
Results
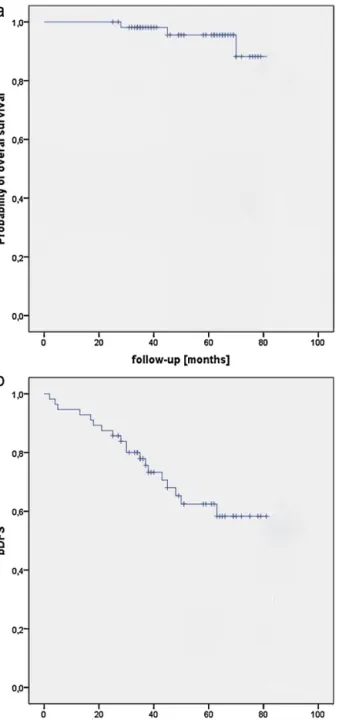
The median follow up time during the evaluation period
(March 2011) was61 months. 52 patients were alive,three
patientsdiedduetotumorprogression,andonediedwithout
tumor.5-Yearoverallsurvivalwas90%and5-yearbiochemical
diseasefreesurvival(bDFS)was62%.Kaplan–Meiersurvival
curves foroverall andbiochemical-diseasefreesurvivalare
shown inFig.1.WealsoanalyzedtheinfluenceofTstage,
Gleasonscore,PSAlevel(withmediancut-off),radiotherapy target volume (prostate only versus whole pelvis), radio-therapy dose (with 74Gy cut-off), and adjuvant hormonal treatmenttothebiochemicalrelapse-freesurvival.Noneof thesefactorssignificantlyinfluencedbDFS.Therewasastrong trendforbetterresultsinthe groupwithPSAvaluesbelow themedian(67.5ng/ml,p=0.075).20(37.5%)treatmentfailures wereobservedduringthetimeofevaluation.PSArelapsealone was detectedin 10 (17.8%) patients, eight (14.3%) patients hadPSArelapsefollowedbybonedissemination,one(1.8%) patienthadPSArelapse,localrelapse,andbonedissemination andone(1.8%)patienthadPSArelapseandparaaortallymph node dissemination.Acuteandlatetoxicitywereevaluated accordingtotheRTOGscale.Therapyoftherectalbleeding withArgon-laserwasconsideredasgradeIIItoxicity.Thedata foracuteandlategastrointestinal(GI)andgenitourinal(GU) toxicitycanbefoundinTable3.Notoxicity≥2forotherorgans wasobserved.
Table3–AcuteandlateGIandGUtoxicity. RTOGscale Gr.0 Gr.1 Gr.2 Gr.3 Gr.4 AcuteGI 30% 29% 41% 0% 0% AcuteGU 16% 53.4% 27% 1.8% 1.8% LateGI 41.1% 19.6% 33.9% 5.4%a 0% LateGU 87.5% 1.8% 10.7% 0% 0%
a Argon-lasercoagulationwasconsideredasgr.3laterectaltoxicity.
Fig.1–Overallsurvival(a)andbiochemical-diseasefree survival(bDFS)(b).
Discussion
AninitialPSA valuehigher than 40ng/mlis considered as a very poor prognostic factor and physicians often offer
less radical or only palliative treatment for this subgroup of patients. Thevalue ofthe PSA which excludespatients from radical treatment is not known. Some studies used PSA>150ng/mlasanexclusioncriterion.Themainproblem inthetreatmentofthissubgroupofprostatecancerpatients istheriskoflocalovertreatmentwithpossiblelateeffectsof radiotherapyintheradicalapproach.Ontheotherhand,there isahighriskofprogressionoflocalizeddiseasein combina-tion withside-effectsofthewhole-lifehormonaltreatment inthepalliativeapproach. Treatmentshouldbesufficiently effectiveinthediseasecontrolwithanacceptablefrequency ofsideeffects.Themainquestionishowmanypatientsare withouttumorprogressionuponthecompletionoftreatment andifthetreatmenttoxicityisacceptable.
A possible solution is a better selection of patients for radicaltreatment.Someproportionofpatientshad dissem-inated disease at the time of diagnosis, but a significant proportionofpatientswithhighinitialPSAhadtumor lim-ited to the prostate, without extra prostatic extension or seminal vesicle invasion.12 Current methods often cannot discriminatedisseminated disease.Bonescanswith99Tcis a standard examination in prostate cancer patients with PSA>20ng/ml. The probability of bone metastasis in this groupishigherthan 20%andtheriskincreaseswithrising values.13 Natrium fluoridePETmay offerhighersensitivity but reportsaboutthismethodarecontroversial.Markersof bone metabolism, like bone formation markers(bone spe-cific alkaline phosphatase, propeptides of type I collagen), boneresorptionmarkers(bonesialoprotein),and osteoclas-togenesis markers (osteoprotegerin) are other possibilities for improving the detection of bone metastasis.14–16 Dis-tinctsuggestionsfordiagnosingskeletallesionsforpatients with extremely high PSA levels donot exist. Secondmost probable locations of dissemination are pelvic or paraaor-tal lymph nodes. Thestandard investigation is a CT scan. Magnetic resonance imaging does not have a better sen-sitivity than a CT for detecting lymph node metastasis.17 Metastasestootherorgansareextremelyrareanditisnot nec-essarytodealwiththem.Cholin-PETisapromisingmethod withsensitivityof55–100%andspecificityof77–86%forthe detectionofprimarytumors.7,18–20Sensitivityandspecificity of18F-fluorocholinforthedetectionoflymph-node metas-tasis in men with intermediate or high risk tumors were 45% and 96%,respectively.21 Others investigatedthe value of this examination in the detection of bone metastasis and specifiedvaluesofsensitivityat79% andspecificityat 97%.22
Our strategy of radical treatment includes neoadjuvant hormonaltreatment,radicalradiotherapy(withdose escala-tioninsignificantproportionofmen),andoptionallyadjuvant hormonaltherapy.
Theeffectivenessofneoadjuvanthormonaltreatmentwas demonstrated in a number of clinical studies. This treat-menthasalowincidenceofside-effectsandisindicatedfor patientswithintermediateandhighriskprostatecancer.23,24 Weusedashorttermhormonaltreatment,althoughtodaya longerneoadjuvanttreatmentisrecommended.25PSAdecline afterneoadjuvanttreatmentmaybeusedasanother prog-nosticfactorforthedecisionbetweenradicalandpalliative treatment.26
Radiotherapyisthekeyfactorindeterminingthesuccess ofradicaltreatmentandtheseverityofsideeffectsin com-parisonwiththepalliativeapproach.Theeffectofradiation dependsondose,targetvolumes,andradiotherapytechnique. Thetreatmentofthepelviclymphaticregionhassome advan-tagesincomparisonwithprostateonlyradiotherapyinhigh riskprostatecancerpatients.RTOG9413trialsdemonstrated a 13% improvement ofprogression freesurvival for pelvic RT versus prostate only RT.27–29 Our data showed a much betterdisease freesurvivalfortheprostate only radiother-apy group. The limited volume was indicated only for T1 orT2stage,Gleasonscore<7and PSAbelowmedianvalue and,therefore,thenumberofthesepatientswassmall(14%). Inspite ofthis,wehypothesized that this wasa selection biasandthatwholepelvisradiotherapywasindicatedinthis extremelyhighriskgroup,especiallyhigherTstageor Glea-sonscore. Dose-response characteristics ofprostatecancer arewelldocumented.30,31 Effectsofhigherdosagewerenot demonstrated inourgroup. Thereissometrend forbetter resultswithhigherdoses.Wehypothesizedthatthismight beduetotheshorttimeoffollowup.Thenextissueisthe frequencyoflateeffectsoftheradiotherapy.Weuseda3D con-formaltechnique.IMRT techniquesignificantlyreducesthe numberofsideeffects,aswasdemonstrated,32andmaybe usedforadditionaldoseescalation.33,34Themajorityoflate effectswereinourrectalbleedinggroup.5.4%ofourpatients neededtreatmentwithlasercoagulationandnoneofthem requiredsurgery.Wedidnotobserve urogenitallateeffects worsethangrade2.Ourconclusionfromtoxicitydataisthat benefitsofaddingradiotherapyaremuchhigherthan disad-vantages.Thefrequency oflate siteeffects was similar as inpublishedreportsforthe3DCRT.35Moreover,we hypoth-esize, that by using IMRT and optimization of treatment position the frequencyof side effects may be significantly diminished.36,37
Adjuvant hormonaltherapy isa standard option inthe high risk prostate cancer group and improves overall sur-vivalofhighriskgroupby16%.38However,long-termadjuvant treatmenthasmanysideeffects,includingcardiovascular dis-ordersandahigherincidenceofdiabetes,39,40althoughrecent reportsdisputetheriskofcardiovasculareffects.41Wedidnot observedstatisticallysignificantdifferencebetweenadjuvant treatmentandnoadjuvanttreatment.WeindicateAHB espe-ciallyinpatientswithhighGleasonscore(8–10)orstageT3b orhigher.AHBisoptionalforotherpatients.Interestingly,we didnotobserveanydifferencesinbDFSbetweenhigherand lowerGleasonscoregroupsorhigherandlowerTstage.We hypothesizethatneoadjuvanthormonaltreatmentin com-binationwithradicalradiotherapymaybesufficientinhigh riskpatientswithalowGleasonscoreandlowTstage.This assumptionneedsfurtherevaluation.
Treatmentfailure,inthemajorityofpatients,consistedof PSAfailurefollowedbybonemetastasis.Onlyonerelapsein the radiotherapytreatmentvolumewasobserved.Verylow frequency oflocalproblems isanother benefitofthe radi-calapproach.Therewasastatisticallyinsignificanttrendfor betterresultsforthesubgroupwithinitialPSAvaluebelow medianvalueof68ng/ml,ascanbeexpected.5-YearbDFSfor thissubgroupis76%andforpatientswithhigherinitialvalues itis48%.Icanbeconcludedthat,specifically,patientswithPSA valuesof40–70ng/mlshouldbetreatedwitharadicalintent. Dataabouttreatmentoutcomeofpatientswithveryhigh initialPSAvaluesarenotavailable.Recently,Canadianauthors publishedbDFSandOSat5years39%and78%,respectively, in64patientswithinitialPSA>40ng/ml.Ourresultsare bet-ter, possibly due to higher doses and intensive hormonal treatment.42
Conclusion
RadicaltreatmentofpatientswithinitialPSAvalues>40ng/ml hasanexcellent5-yearbiochemicaldiseasefreesurvivalwith alowriskofsideeffectsfromthetreatment.Progressionof diseaseisusuallyoutsidetheradiotherapytreatmentvolume withlocalproblemseliminated.Wecanrecommendthe rad-icaltreatmentapproachforthissubgroupofprostatecancer patientswithagoodperformancestatusandlifeexpectancy.
Conflict
of
interest
Nonedeclared.r
e
f
e
r
e
n
c
e
s
1. CaireAA,SunL,LackBD,etal.Predicting
non-organ-confinedprostatecancerinmendiagnosedafter 2000.ProstateCancerProstaticDis2010;13:248–51.
2. PartinAW,KattanMW,SubongEN,etal.Combinationof prostate-specificantigen,clinicalstage,andGleasonscoreto predictpathologicalstageoflocalizedprostatecancer.A multi-institutionalupdate.JAMA1997;277:1445–51.
3. GallinaA,JeldresC,ChunFK,etal.Predictionofpathological stageisinaccurateinmenwithPSAvaluesabove20ng/mL. EurUrol2007;52:1374–80.
4. AnimJT,KehindeEO,PrasadA,etal.Relationshipbetween serumprostatespecificantigenandthepatternof
inflammationinbothbenignandmalignantprostaticdisease inMiddleEasternmenInternational.UrolNephrol
2006;38:27–32.
5. SchirrmeisterH,GuhlmannA,ElsnerK,etal.Sensitivityin detectingosseouslesionsdependsonanatomiclocalization: planarbonescintigraphyversus18FPET.JNuclMed
1999;40:1623–9.
6. Even-SapirE,MetserU,MishaniE,etal.Thedetectionof bonemetastasesinpatientswithhighriskprostatecancer: 99mTcMDPplanarbonescintigraphy,singleandmultifield ofviewSPECT,18F-fluoridePETand18F-fluoridePET/CT.J NuclMed2006;47:287–97.
7. EschmannSM,PfannenbergAC,RiegerA,etal.Comparison of11C-cholinePET/CTandwholebody-MRIforstagingof prostatecancer.Nuklearmedizin2007;46:161–8.
8. ScattoniV,PicchioM,SuardiN,etal.Detectionof
lymph-nodemetastaseswithintegrated[11C]cholinePET/CT inpatientswithPSAfailureafterradicalretropubic
prostatectomy:resultsconfirmedbyopen
pelvic-retroperitoneallymphadenectomy.EurRadiol 2007;52:423–9.
9. WidmarkA,KleppO,SolbergA,etal.Endocrinetreatment, withorwithoutradiotherapy,inlocallyadvancedprostate cancer(SPCG-7/SFUO-3):anopenrandomisedphaseIIItrial. Lancet2009;373:301–8.
10. BollaM,ColletteL,BlankL,etal.Long-termresultswith immediateandrogensuppressionandexternalirradiationin patientswithlocallyadvancedprostatecancer(anEORTC study):aphaseIIIrandomisedtrial.Lancet2002;360: 103–6.
11. BollaM,vanTienhovenG,deReijkeTM,etal.Concomitant andadjuvantandrogendeprivation(ADT)withexternal beamirradiation(RT)forlocallyadvancedprostatecancer:6 monthsversus3yearsADT:resultsoftherandomizedEORTC PhaseIIItrial22,961.JClinOncol2007;25:5014.
12. GallinaA,JeldresC,ChunF,etal.Predictionofpathological stageisinaccurateinmenwithPSAvaluesabove20ng/mL. EurUrol2007;52:1374–80.
13. GleaveME,CouplandD,DrachenbergD,etal.Abilityofserum prostate-specificantigenlevelstopredictnormalbonescans inpatientswithnewlydiagnosedprostatecancer.Urology 1996;47:708–12.
14. JungK,LeinM,StephanC,etal.Comparisonof10serum boneturnovermarkersinprostatecarcinomapatientswith bonemetastaticspread:diagnosticandprognostic implications.IntJCancer2004;111:783–91.
15. KamiyaN,SuzukiH,YanoM,etal.Implicationsofserum boneturnovermarkersinprostatecancerpatientswithbone metastasis.Urology2010;75:1446–51.
16. KataokaA,YuasaT,KageyamaS,etal.Diagnosisofbone metastasisinmenwithprostatecancerbymeasurementof serumICTPincombinationwithalkaliphosphataseand prostate-specificantigen.ClinOncol2006;18(August(6)):480–4. 17. HovelsAM,HeesakkersRA,AdangEM,etal.Thediagnostic
accuracyofCTandMRIinthestagingofpelviclymphnodes inpatientswithprostatecancer:ameta-analysis.ClinRadiol 2008;63:387–95.
18. TestaC,SchiavinaR,LodiR,etal.Prostatecancer:sextant localizationwithMRimaging,MRspectroscopy,and 11C-cholinePET-CT.Radiology2007;244:797–806. 19. YamaguchiT,LeeJ,UemuraH,etal.Prostatecancer:a
comparativestudyof11C-cholinePETandMRimaging combinedwithprotonMRspectroscopy.EurJNuclMedMol Imaging2005;32:742–8.
20. BaumanG,BelhocineT,KovacsM,WardA,BeheshtiM, RachinskyI.(18)F-fluorocholineforprostatecancerimaging: asystematicreviewoftheliterature.ProstateCancerProstatic Dis2011,doi:10.1038/pcan.2011.35.August16[Epubaheadof print].
21. BeheshtiM,ImamovicL,BroingerG,etal.18FcholinePET/CT inthepreoperativestagingofprostatecancerinpatients withintermediateorhighriskofextracapsulardisease:a prospectivestudyof130patients.Radiology2010;254:925–33. 22. BeheshtiM,ValiR,WaldenbergerP,etal.TheuseofF-18
cholinePETintheassessmentofbonemetastasesinprostate cancer:correlationwithmorphologicalchangesonCT.Mol ImagingBiol2009;11:446–54.
23. Roach3rdM,BaeK,SpeightJ,etal.Short-termneoadjuvant androgendeprivationtherapyandexternal-beam
radiotherapyforlocallyadvancedprostatecancer:long-term resultsofrtog8610.JClinOncol2008;26:585–91.
24. D’AmicoAV,ChenMH,RenshawAA,LoffredoM,KantoffPW. Androgensuppressionandradiationvsradiationalonefor prostatecancer:arandomizedtrial.JAMA2008;299:289–95.
25. DenhamJW,SteiglerA,LambDS,etal.Short-termandrogen deprivationandradiotherapyforlocallyadvancedprostate cancer:resultsfromtheTrans-TasmanRadiationOncology Group96.01randomisedcontrolledtrial.LancetOncol 2005;6:841–50.
26. AlexanderA,CrookJ,JonesS,etal.Isbiochemicalresponse moreimportantthandurationofneoadjuvanthormone therapybeforeradiotherapyforclinicallylocalizedprostate cancer?Ananalysisofthe3-versus8-monthrandomized trial.IntJRadiatOncolBiolPhys2010;76:23–30.
27. RoachIIIM,DeSilvioM,ValicentiR,etal.Whole-pelvis, “mini-pelvis,”orprostate-onlyexternalbeamradiotherapy afterneoadjuvantandconcurrenthormonaltherapyin patientstreatedintheRadiationTherapyOncologyGroup 9413trial.IntJRadiatOncolBiolPhys2006;3:647–53. 28. LawtonCA,DeSilvioM,RoachIIIM,etal.Anupdateofthe
phaseIIItrialcomparingwholepelvictoprostateonly radiotherapyandneoadjuvanttoadjuvanttotalandrogen suppression:updatedanalysisofRTOG94-13,withemphasis onunexpectedhormone/radiationinteractions.IntJRadiat OncolBiolPhys2007;69:646–55.
29. DirixP,HaustermansK,JuniusS,WithersR,OyenR,Van PoppelH.Theroleofwholepelvicradiotherapyinlocally advancedprostatecancer.RadiotherOncol2006;79:1–14. 30. CheungR,TuckerS,LeeA,etal.Dose–response
characteristicsoflow-andintermediateriskprostatecancer treatedwithexternalbeamradiotherapy.IntJRadiatOncolBiol Phys2005;61:993–1002.
31. PollackA,ZagarsG,StarkschallG.ProstateCancerradiation doseresponse:resultsoftheM.D.AndersonphaseIII randomizedtrial.IntJRadiatOncolBiolPhys2002;53:1097–105. 32. SharmaNK,LiT,ChenDY,PollackA,HorwitzEM,
BuyyounouskiMK.Intensity-modulatedradiotherapy reducesgastrointestinaltoxicityinpatientstreatedwith androgendeprivationtherapyforprostatecancer.IntJRadiat OncolBiolPhys2010,doi:10.1016/j.ijrobp.2010.02.040. November2[Epubaheadofprint].
33. DolezelM,OdrazkaK,VaculikovaM,etal.Doseescalationin prostateradiotherapyupto82Gyusingsimultaneous integratedboost:directcomparisonofacuteandlatetoxicity with3D-CRT74GyandIMRT78Gy.StrahlentherOnkol 2010;186(April(4)):197–202.
34. CeylanC,KucukN,BasAyataH,GudenM,EnginK.
DosimetricandphysicalcomparisonofIMRTandCyberKnife plansinthetreatmentoflocalizedprostatecancer.RepPract OncolRadiother2010;15(6):181–9.
35. AshmanJB,ZelefskyMJ,HuntMS,LeibelSA,FuksZ.Whole pelvicradiotherapyforprostatecancerusing3Dconformal andintensity-modulatedradiotherapy.IntJRadiatOncolBiol Phys2005;63:765–71;
DeMeerleerG,FonteyneVH,VakaetL,etal.
Intensity-modulatedradiationtherapyforprostatecancer: latemorbidityandresultsonbiochemicalkontrol.Radiother Oncol2007;82:160–6.
36. BollaM,GonzalezD,WardeP,etal.Improvedsurvivalin patientswithlocallyadvancedprostatecancertreatedwith radiotherapyandgoserelin.NEnglJMed1997;337:295–300. 37. BajonT,PiotrowskiT,AntczakA,etal.Comparisonofdose
volumehistogramsforsupineandpronepositioninpatients irradiatedforprostatecancer—apreliminarystudy.RepPract OncolRadiother2011;16:65–70.
38. TyrrellaCH,PaynebH,SeecWA,etal.Bicalutamide (‘Casodex’)150mgasadjuvanttoradiotherapyinpatients withlocalisedorlocallyadvancedprostatecancer:results fromtherandomisedEarlyProstateCancerProgramme Group.RadiotherOncol2005;76:4–10.
39. KeatingNL,O’MalleyAJ,SmithMR.Diabetesand
cardiovasculardiseaseduringandrogendeprivationtherapy forprostatecancer.JClinOncol2006;24:4448–56.
40. SaigalCS,GoreJL,KrupskiTL,HanleyJ,SchonlauM,Litwin MS.Androgendeprivationtherapyincreasescardiovascular morbidityinmenwithprostatecancer.Cancer
2007;110:1493–500.
41. AlibhaiSM,Duong-HuaM,SutradharR,etal.Impactof androgendeprivationtherapyoncardiovasculardiseaseand diabetes.JClinOncol2009;27:3452–8.
42. AlexanderAS,MydinA,JonesSO,etal.Extreme-riskprostate adenocarcinomawithprostate-specificantigen
(PSA)>40ng/ml:prognosticsignificanceofthepreradiation PSAnadir.IntJRadiatOncolBiolPhys2011,
doi:10.1016/j.ijrobp.2010.11.068.January27[Epubaheadof print].