The location of the inferior angle of the scapula in
relation to the spinal level of prone patients
Robert Cooperstein,
MA, DC*Michael T. Haneline,
DC, MPH*Morgan D. Young,
DC, BS**Background: In two previous studies we established the mean location of the upright inferior angle of the scapula (IAS) to be near the spinous process of T8. The current study investigates the common belief that the prone IAS lines up with the T6 SP.
Methods: The location of the IAS in relation to the spine of 20 mostly asymptomatic subjects was assessed on a Hi-Lo table in 7 different postures, 2 upright and 5 prone.
Results: The scapula moved cephalad in two of the test positions: prone, arms at side and prone, chicken-wing. It moved caudad in the other 4 test positions, including prone, using armrest (18.4 mm).
Conclusions: With the prone patient’s arms on the arm pieces, the most likely patient posture, the average caudad IAS movement is about one vertebral level, notwithstanding the common belief that the IAS is one level cephalad to the upright level.
(JCCA 2009; 53(2):121–128)
k e y w o r d s: scapula, angle, spinal level
Introduction
In two previous studies,1–3 we established the location of
the inferior angle of the scapula angle (IAS) in the
up-right position to line up approximately, on average, with the spinous process (SP) of T8. This was in spite of the fact that there are numerous sources purporting the SP of
* Palmer Center for Chiropractic Research. ** Research Associate, Palmer West.
Contact: Robert Cooperstein, Palmer College of Chiropractic, West Campus, 90 East Tasman Drive, San Jose, CA 95134. Tel: (408) 944-6009. Fax: (408) 944-6118. cooperstein_t@palmer.edu
© JCCA 2009.
Historique : Dans deux études antérieures, nous avons établi que la position moyenne de l’angle inférieur d’épaule en position debout (IAS) se situait près de l’apophyse épineuse de T8. La présente étude se penche sur la croyance populaire voulant que l’IAS couché soit aligné avec la T6 SP.
Méthodologie : La position de l’IAS en rapport avec la colonne vertébrale de 20 sujets pour la plupart asymptomatiques a été évaluée sur une table Hi-Lo dans 7 postures différentes : 2 debout et 5 couché.
Résultats : L’omoplate s’est déplacée en direction céphalique dans deux des positions du test : couché, les bras à côté et couché, rassemblement des bras. Il s’est déplacé en direction caudale dans 4 autres positions, y compris la position couchée, rassemblement des bras (18,4 mm).
Conclusion : Le patient étant couché et ses bras reposant sur les bouts d’épaule, la posture la plus probable du patient, le mouvement moyen en direction caudale de l’IAS est d’environ d’un niveau vertébral, peu importe la croyance populaire voulant que l’IAS est d’un niveau debout, en direction céphalique.
(JACC 2009; 53(2):121–128)
T7 to line up with the IAS. In our first study1 we simply
placed a self-adhesive lead marker (i.e., a BB) at the SP process that was established through manual palpation to be closest to the IAS. Radiometric analysis of an upright x-ray, authorization for which was obtained on clinical grounds unrelated to our project, showed the marked SP to be close to T8, in a range spanning T6–10. In our sec-ond study,2 we retrospectively analyzed a convenience
sample of 50 x-rays that had been donated to our chiro-practic college by a doctor who had not used collimation and thus allowed visualization of the scapulae, unlike most modern x-rays. This allowed us to determine, con-sistent with the results of our first study, that the IAS tended on average to lie even with the SP of T8, and in a similar range, spanning T7–10.
Having determined that the conventional wisdom by which the standing IAS lines up on average with T7 ap-peared to be in error, we decided to investigate another common belief by which the prone position of the IAS would line up with the SP of T6. In fact, it is commonly stated in the context of chiropractic education that the IAS may be located using the rule “7 up, 6 down, referring to the position of the IAS in relation to the adjacent spinous process in an upright and prone position, respectively. Table 1 includes a convenience sample of citations repre-senting this conventional wisdom, three drawn from sourc-es at our own institution, the Palmer Chiropractic College.
We wanted to learn the answer to two questions: (i) is it true that the prone IAS lines up with the T6 spinous process? and (ii) whatever the position of the prone IAS in relation to the spine, does it line up with a vertebral segment that is one level cephalad to the vertebral seg-ment with which it lines up, on average, in the upright position?
We believe knowing which spinal level corresponds to the IAS to be a matter of interest to several professions. It is common in chiropractic, orthopedic medicine, osteopa-thy, massage therapy, acupuncture, and nursing clinical situations to locate the putative location of spinal levels where intervention is intended by counting from up or down from the segment that lines up with the IAS, what-ever particular benchmark association the clinician is us-ing (usually T7 or T8). In the chiropractic profession, we think it likely that the most common reason for using such a benchmark is to locate a targeted area for manual inter-vention (i.e. an adjustment) based on information seen on an x-ray that has been taken in the upright position. That stated, such benchmarks are also likely to be used in con-junction with other types of examination procedures, such as thermography and motion palpation performed in the seated position, which generate sites for spinal interven-tions that are to be performed in the prone position.
A clinician, although the use of x-rays for biomechani-cal controversial remains controversial, may believe that Table 1 Convenience sample of citations regarding prone scapular position relative to spine
T6 found at the level of the tip of the scapula when the patient is prone
Downes JW. Life College School of Chiropractic Tech-nique Manual. 2nd ed.(4,p17)
6T – found at the level of the tip of the scapula – patient prone
Palmer College of Chiropractic Adjusting Technique Manual. Davenport, Il: PCC.5
7th dorsal: The spinous process corresponds to the inferi-or angle of the scapula when the subject is sitting with the arms hanging at the sides, and half an inch above when the subject is lying prone.
Gardner, PE. Chiropractic Philosophy and Practice. In: Review Course of fundamental subjects combined with chiropractic laws and state board questions and answers. Fourth Edition, 1939. Downloaded from http://www.chirobase.org/12Hx/gardner.html July 15, 20086
“IAS = T6 SP of a prone patient, T7 SP of a seated pa-tient”
1Q Palmer West Spinal Anatomy lab pg 15 (2006)
“T6–T7 interspace is level with IAS when prone, T7–T8 when seated ’7up.’”
a vertebral misalignment (i.e., subluxation) is clinically significant, especially if there are other associated clini-cal findings – fixation, tenderness, soft tissue textural changes, or neurological changes. Such a clinician would require a protocol which enables locating T5, for exam-ple, on a prone patient. The doctor might palpate down from where he or she believes the vertebra prominens (VP) is located, according to the common belief that it lies at either C7 or T1 (depending on which level is deter-mined using motion palpation to be lowest movable seg-ment on extension), or perhaps might palpate up from the level of the iliac crest, according to the common belief that the SP of L4 lines up with the iliac crest.
We think it most likely that a chiropractor targeting a mid-thoracic vertebral level in the prone position more often than not would use the IAS as the guide, according to the common belief that it would lie one level above the standing IAS. Conceivably one could use the VP or iliac crest to do so, although given the location, the IAS is the closest landmark and palpating from VP or iliac crest is much more tedious, whether or not it is more accurate. Our study, therefore, seeks to determine the likely accu-racy of such a targeting protocol.
Methods
The study included asymptomatic and minimally symp-tomatic chiropractic students, according to the following criteria: (a) spinous process tenderness T6–10 <3/10; and (b) the subject’s arms could assume each of the 7 test po-sitions in a pain-free manner. The n = 20 study popula-tion included 6 females (average age 25) and 14 males (average age 34). All 20 subjects were right-handed. The average height was 69 cm, range 61–76 cm. All subjects provided informed consent to participate in the study, and the Palmer Institutional Review Board approved the study.
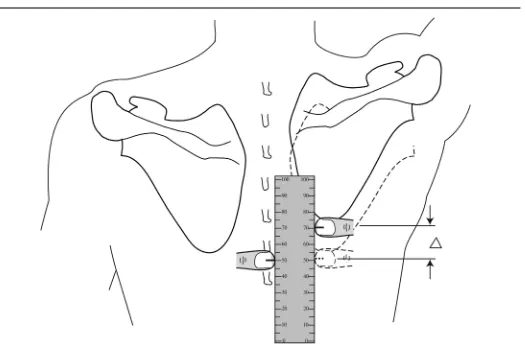
Each subject in turn stood on the platform of a Hi-Lo table, arms hanging at his or her side. An experienced palpator then determined using manual static palpation the location of the SP that lined up most closely to the right IAS. (It was not necessary for the purposes of this study to determine the actual level of this segment and number it.) To obtain this and subsequent measurements, we marked lines on each of the examiner’s thumbnails and measured using a ruler the axial displacement of the thumb contacting the IAS with respect to the SP. (see
Figure 1) With the palpator firmly holding his thumb on this SP to prevent displacement from soft-tissue move-ment, the standing subject was instructed to move his or her hands to the handles of the table, while an examiner measured the movement of the palpated SP in relation to the IAS. The table and subject were then moved to the prone position by means of activating the motor that ac-complishes this action. With the subject having become fully prone, and with the first investigator continuing to hold his thumb on the same SP, a second investigator measured and recorded the location of the targeted SP in relation to the IAS in 5 more test positions: hands on armrest, arms dangling over sides of table, held at side on table, arms fully flexed on table, and arms in “chicken-wing” position. Figure 2 shows all 7 measured positions for this study, 2 standing and 5 prone measurements. These are described in table 2. In all positions the subject was instructed to relax their arms and lay comfortably.
Results
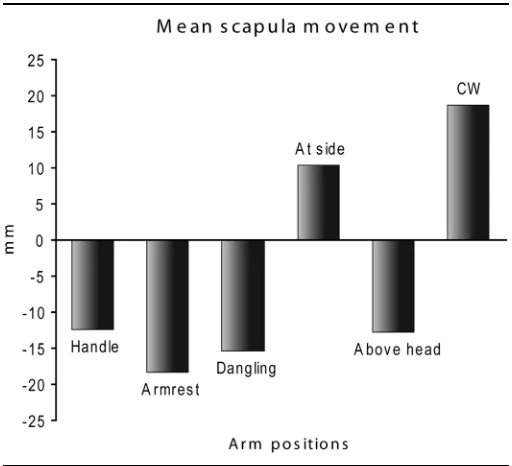
Figure 2 shows anatomically the direction of scapular movements in relation to a spinal baseline condition with the subject standing and arms dangling. Figure 3 further illustrates the mean scapular movements, compared with the standing neutral baseline position, for positions 1–7 in figure 2. Raising the arms to the handle in the standing position lowered the IAS 12.45 mm. Moving it to the armrest in the prone position lowered it 18.45 mm, allow-ing it to dangle in the prone position lowered it 15.45 mm, placing the arms at the side elevated the IAS 10.4 mm, placing the arms in the fully abducted position low-ered the IAS 12.75 mm, and finally putting the arms in what we called “chicken-wing position” raised the IAS 18.70 mm. To put these measurements in perspective, one vertebral level corresponds to about 20 mm, depend-ing on the height of the individual. The scapular move-ments showed great consistency in terms of direction of movement: in 120 measurements among 20 subjects, 110/120 movements were in the same direction as the mean. For example, when the subject’s were measured with their hands on the table armrest, 19/20 showed cau-dal movement and only 1/20 showed cephalad scapular movement.
Discussion
Figure 1 Measuring IAS position
Table 2 Arm positions assumed in this study
Arm position Description
Position 1, neutral standing Standing upright, arms dangling at the side
Position 2, handle Standing upright, arms placed on handles prepared to be lowered on the Hi-Lo
Position 3, armrest Arms on the armrests of the table which are positioned below the headpiece
Position 4, dangling Arms dangling off the table with subject’s humerus perpendicular to the floor as a standardization
Position 5, at side Arms at the side, resting on the table with hands tucked under thigh or pressed to the leg
Position 6, above head Arms raised above the head with interlocked fingers touching the top of the head as a standardization and resting on the headrest
who placed their arms in 7 different positions. The data are reported as the deltas between the 6 test positions (1 standing, 5 prone) compared to a standing, arms dangling baseline condition. The scapula moves cephalad in two of the test positions: prone, arms at side; and prone,
chick-en-wing. It moved caudad in the other 4 test positions. Therefore, the conventional wisdom, at least in the chiro-practic profession, by which the IAS is one level cephal-ad in the prone position compared with the standing position, is not validated. The accuracy of the benchmark Figure 2 Scapular movements relative to a standing spinous process benchmark in 7 arm positions
Table 3 Magnitude and direction of scapular movements different arm positions (negative sign means cephalad movement)
Mean delta compared with
baseline Range (mm) Median Direction reversals
standing, arms dangling – – – –
standing, arms on handle 12.5 50 12.5 2
prone, hands on armrest 18.4 44 20 0
prone, arms dangling 15.5 48 17.5 2
prone, hands at side –10.4 56 –8 2
prone, hands above head 12.8 48 13.5 3
depends on subject arm placement. Since it is likely that most subjects are positioned with their hands placed on table’s armrests while prone, we would expect the aver-age caudad movement to be 18.45 mm, about one verte-bral level. This is in the opposite direction from the conventional wisdom. If an examiner were trying to lo-cate the IAS with the arm in the chicken-wing position, which makes the medial border of the scapula prominent, the IAS would indeed tend to rise about one vertebral level. However, returning the arms to the armrest prior to a clinical intervention would likely once again move the IAS caudad relative to the baseline standing position. It is interesting to note that the IAS moved cephalad about 10 mm (about ½ of a vertebral level) with the arms at the side, prone; the prone position that most resembles the standing baseline condition.
In this study we made no effort to determine the actual level of the IAS, since we were only concerned with its direction of movement relative to the spine in a number of subject arm positions. That stated, since we know from previous studies that the mean IAS position corresponds most closely to the SP of T8 +/–0.89 in the standing posi-tion, it would be safe to hypothesize that the mean
loca-tion of the IAS in prone subjects, with the arms in the position most likely to be assumed during a clinical inter-vention, will tend to be at the SP of T9, although not without some variability.
It is likely that a clinician attempting to locate a thorac-ic spinal landmark on a prone patient, transposing an ex-amination finding obtained on a patient in an upright position, using typical rules of thumb espoused at least by the chiropractic profession, will not locate the desired spi-nal level. If the IAS is used to locate thoracic SPs, the magnitude of the miss will be determined by anatomical variation in patients as to the location of their standing IAS, anatomical variation in patients as to the location of their prone IAS, doctor error in locating the IAS, the exact location of the patient’s arms during interventions, and the use of conventional spinal landmark associations that our current and prior research suggests are inaccurate. The cumulative error of these factors introduces a large degree of uncertainty in targeting thoracic spinal loca-tions, as might be expected as the consequence of relying on a mobile anatomical landmark. All this understood, let us work through a typical chiropractic technique scenario, to determine the likely accuracy a clinician obtains using conventional wisdom as to the IAS position, setting aside temporarily patient variation and doctor’s palpatory mis-takes as further considerations . Analysis of an upright x-ray suggests T7 needs to be adjusted. The clinician puts the patient in the prone position, hands on the armrest, and proceeds to locate the IAS, presuming it on a line with the T6 SP; then drops down one level to find the pu-tative T7 SP. In actuality, the prone IAS tends to line up with the T9 SP, and dropping one level below that would obtain the SP of T10. Thus, the clinician will in this case be off by 3 levels. Given the variation we found in our previous study for IAS location (range = T6–10, standard deviation = 0.89), the clinician might be off by more than 3 levels due to patient variation, or in fact less than 3 lev-els if the variation offsets error introduced by improper landmark application. Finally, given the likelihood of doctor error seen in our previous error in locating spinal landmarks seen in our previous work, the clinician might be off by more than 3 levels due to doctor palpatory error, or in fact less than 3 levels if the palpatory error offsets improper landmark application to some degree. The rang-es of error and variability prrang-esent a cloud of possible out-comes.
In reviewing the literature, we noted there was little in-formation to be found about scapular motion outside of the highly studied “scapular rhythm.” Scapular rhythm is concerned with motion of the scapula as the arm is ab-ducted and is significantly different from scapular motion as the arm is flexed, extended, and protracted. In our study, we also evaluated scapular position with two dif-ferent directions of gravitational pull (in the upright com-pared with prone positions) and the muscular sling that holds the scapula responds differently in these two posi-tions. Accordingly, there was very little information gathered from our search that was applicable to this study.
There are some limitations of the study that need to be acknowledged.
• For each measurement position, the position of the right IAS was determined in relation to the thoracic spinous processes. We did not measure the position of the left IAS, which could have shown a different movement pattern.
• Although each of three examiners who palpated the SP closest to the IAS agreed the grip could be easily main-tained as the table went from the upright to the down position, no effort was made to prove that this in fact occurred.
• Although we collected data on the distance between the first sacral tubercle and the vertebra prominens, to permit subsequent transformation and thus normaliza-tion of the data anthropometrically, we ultimately de-cided it was not necessary to do so. Normalizing our shortest subject to the tallest subject would have only altered the mean IAS movement about 5 mm, or 1/4 of a vertebral level, and would not have altered our con-clusions.
• We obtained all of our data using one particular Hi-Lo table, the motorized design of which allows convenient changing from the prone to an upright position. A dif-ferent table, with handles or arm-rests in a difdif-ferent po-sition from ours might have produced somewhat different results. However, we suspect this would like-ly have affected the magnitude of movement in each position, not the direction of movement, which is the main concern in this study.
• Different results may have been obtained with a more symptomatic patient population.
• The practice of x-ray line marking, and more generally speaking, using x-rays for biomechanical analysis, re-mains controversial. The authors, in exploring the con-sequences of using a wrong benchmark rule as part of the overall process of connecting x-ray and palpatory findings, are not themselves advocating this particular use of radiography.
Conclusions
Our data suggest that the application of benchmark rules commonly used in the chiropractic profession to relate the position of the IAS to the spine routinely results in a failure to locate prone spinal levels sought on the basis of upright examination findings, such as upright palpation, thermography, or x-ray. Attempting to situate a radio-graphic lesion on a prone patient, assuming the upright IAS corresponds to the SP of T7, as is commonly done, introduces a one level error. Assuming the prone IAS moves cephalad one level compared to the standing IAS, whereas in actuality it moves about one level caudad when the patient’s arms are placed on the armrest, results in an additional two level error, for a total of 3 levels. Pa-tient variation and doctor palpatory error could increase or decrease the amount of miss. We have reason to be-lieve that a non-radiological upright finding such as thermographic or palpatory would likely result in a two level targeting area, rather than the three level error asso-ciated with radiological examination.
It is possible that misidentifying the spinal level that is treated results in care that is less safe, less effective, or both. At minimum, it prevents accurate record keeping as to what was treated. Doctors who use upright x-rays or other upright examination procedures to help them determine spinal levels worthy of intervention need to explain their clinical outcomes in view of the fact that conventional spinal landmark rules are likely to intro-duce multi-level errors in force application. If adjustive specificity is clinically important, then their results may have been suboptimal; or, if their results have been opti-mal, adjustive specificity may be less important than has been commonly believed.
Acknowledgment
We would like to acknowledge the contributions of our Research Assistants, Tamara Ghazi and Erica Janssen, who are the co-presidents of our college’s Evidence-Based Chiropractic club. They helped design and execute the project. We would also like to thank the Palmer Cen-ter for Chiropractic Research for its support.
Disclaimer
None of the authors have any competing interests, or stand to gain in any financial way from the publication of this manuscript.
References
1 Cooperstein R, Haneline M. Spinous process palpation using the scapular tip as a landmark vs a radiographic criterion standard. J Chiropr Med. 2007; 6(3):87–93.
2 Haneline M, Cooperstein R, Young M, Ross J. Determining spinal level using the inferior angle of the scapula as a reference landmark: a retrospective analysis of 50 radiographs. J Can Chiropr Assoc. 2008; 52(1):24–9. 3 Cooperstein R, Haneline M. Where is the inferior angle of
the scapula? Dynamic Chiropractic. 2008; 26(8).
4 Downes JW. Life College School of Chiropractic Technique Manual. 2nd ed.
5 Palmer College of Chiropractic Adjusting Technique Manual. Davenport, Il: PCC.