Neurodevelopmental Burden at Age 5 Years in Patients
With Univentricular Heart
WHAT’S KNOWN ON THIS SUBJECT: With increasing survival rates, there is growing interest in long-term quality of life among patients with univentricular heart defects, and
neurodevelopmental deficits play a major role in adverse outcome.
WHAT THIS STUDY ADDS: Although median cognitive performance was within normal limits, major neurodevelopmental impairment was found in one-fourth, and minor neurologic dysfunction in almost half of patients. Brain MRI showed mostly ischemic findings of different degrees in the majority of patients.
abstract
BACKGROUND:Despite increasing survival, patients with hypoplastic left heart syndrome (HLHS) and other forms of functionally univentric-ular heart defects (UVHs) remain at increased risk of long-term neurodevelopmental deficits.
METHODS:A nationwide sample of 23 patients with HLHS, 13 with UVH, and 40 controls were followed prospectively until the age of 5 years, when neurologic, neuropsychological, and motor examinations and brain MRI were performed.
RESULTS:The median full-scale IQ was significantly lower in patients with HLHS (97,P,.001) and patients with UVH (112,P= .024) compared with controls (121). Major neurodevelopmental impairment was found in 26% of the patients with HLHS and 23% of those with UVH, and minor neurologic dysfunction was found in 43% and 46%, respectively. MRI revealed abnormalities, mostly ischemic changes of different degrees, in 82% of the patients with HLHS and in 56% of those with UVH. Prominent changes were significantly associated with neurodevelopmentalfindings and parental reports of adaptive behavior. In linear regression, significant risk factors for a worse outcome were a history of clinical seizures in connection with the primary operation, a lower diameter of the neonatal ascending aorta, and several pre-, peri-, and postoperative factors related to the primary and bidirectional Glenn operations.
CONCLUSIONS:Although median cognitive performance was within the normal range, neurodevelopmental and brain MRI abnormalities were found in the majority of the patients with UVH, and especially in those with HLHS, at preschool age. Both a narrowed ascending aorta and operation-related factors contributed to these findings. Pediatrics
2012;130:e1636–e1646
AUTHORS:Anne Sarajuuri, MD,aEero Jokinen, MD, PhD,b
Leena Mildh, MD, PhD,cAnna-Mari Tujulin, MSc,aIlkka
Mattila, MD, PhD,dLeena Valanne, MD, PhD,eand Tuula
Lönnqvist, MD, PhDa
Divisions ofaChild Neurology,bPediatrics, anddPediatric Surgery,
Department of Gynecology and Pediatrics,cDepartment of
Anesthesia and Intensive Care, andeHelsinki Medical Imaging
Center, Helsinki University Central Hospital and University of Helsinki, Helsinki, Finland
KEY WORDS
congenital heart defects, Fontan procedure, brain, MRI, risk factors
ABBREVIATIONS
AV—atrioventricular BDG—bidirectional Glenn CHD—congenital heart defect DHCA—deep hypothermic cardiac arrest FIQ—full-scale IQ
HLHS—hypoplastic left heart syndrome MDI—Mental Developmental Index MND—minor neurologic dysfunction
Movement ABC—Movement Assessment Battery for Children RLFP—regional low-flow perfusion
TCPC—total cavopulmonary connection UVH—functionally univentricular heart defect VABS—Vineland Adaptive Behavior Scales VIQ—verbal IQ
VMI—Beery-Buktenica Developmental Test of Visual-Motor Inte-gration
WPPSI-R—Wechsler Preschool and Primary Scale of Intelligence– Revised
www.pediatrics.org/cgi/doi/10.1542/peds.2012-0486 doi:10.1542/peds.2012-0486
Accepted for publication Jul 24, 2012
Address correspondence to Anne Sarajuuri, MD, Helsinki University Central Hospital, Children’s Hospital, PL 280, 00029 HUS, Helsinki, Finland. E-mail: anne.sarajuuri@hus.fi
PEDIATRICS (ISSN Numbers: Print, 0031-4005; Online, 1098-4275). Copyright © 2012 by the American Academy of Pediatrics
FINANCIAL DISCLOSURE:The authors have indicated they have nofinancial relationships relevant to this article to disclose.
The surgical and perioperative treat-ments of congenital heart defects (CHDs) have greatly developed during the past few decades, but, despite im-proved survival rates, the neurode-velopmental complications remain a major concern. In particular, patients with hypoplastic left heart syndrome (HLHS) or other forms of functionally univentricular heart defects (UVHs) have a high risk of long-term neurologic sequelae after staged palliative surgery according to the Norwood strategy
presented in 1983.1–5The latest reports
on patients who underwent the Nor-wood operation at the beginning of this century present early developmental results with mean Bayley Mental De-velopmental Indices (MDIs) at the lower end of normal limits, and un-equivocally lower psychomotor de-velopmental indexes at the lower end of mildly delayed performance.6–10
Recently, a mean full-scale IQ (FIQ) of 95 was reported at the age of 4 years among patients with HLHS, being
significantly lower than in patients with other forms of severe CHD.11
In considering whether further pre-vention of brain injury among patients with CHD is possible, it is necessary to recognize that the causes are multifac-torial. Which operative support strategy poses a bigger risk to the developing brain remains controversial,8,9,12 and
patient-related factors have in fact emerged alongside operative factors as major contributors.6 Nevertheless,
MRI studies indicate that perioperative
FIGURE 1
brain injury in the form of white matter injury or infarct is common,13,14although
its impact on later neurodevelopment remains uncertain.
We performed a prospective multipro-fessional neurodevelopmental follow-up study on a population-based sample of patients with HLHS or UVH with healthy age- and gender-matched controls. The neurodevelopmental outcome results at the age of 5 years were correlated with brain MRI results, and a wide range of risk factors were analyzed to further evaluate the risk points for brain damage in this high-risk patient group.
METHODS
All pediatric cardiac surgery in Finland is performed at the Department of Gyne-cology and Pediatrics of Helsinki Uni-versity Central Hospital. Between August 2002 and February 2005, all patients with HLHS or UVH were offered the possibility to take part in a 5-year prospective neurodevelopmental follow-up study.15,16
Forty-six healthy age- and gender-matched control children from low-risk deliveries at the Kätilöopisto Maternity Hospital of Helsinki University Central Hospital were recruited as newborns. At the median age of 5.1 (range, 5.0– 5.4) years, 23 patients with HLHS, 13 with UVH, and 40 healthy controls were
examined (Fig 1). The cardiac di-agnoses and operations performed before the study point are presented in Table 1.
Surgical and Perfusion Strategies
The aortic reconstruction during Norwood-type operations and possible additional aortic reconstructions were performed during either regional low-flow perfusion (RLFP) alone or in combination with short periods (,10 minutes) of deep hypothermic cardiac arrest (DHCA). During all operations involving aortic arch reconstruction, the hematocrit was kept at 30%, and cooling was aimed at 18°C. During the bidirectional Glenn (BDG) operation, as well as the total cavopulmonary connection (TCPC), the hematocrit was also aimed at 30%, but the body temperature was kept between 30 and 34°C.
Outcome Measures
The neurologic examination was per-formed according to a test modified from Touwen,17with a few items added
to more accurately assess gross and
fine motor skills. The findings were classified according to Hadders-Algra18
(Table 2). Height, weight, and head circumference were measured and
compared with Finnish national standards.19,20
Cognitive testing was performed according to the Finnish version of the Wechsler Preschool and Primary Scale of Intelligence–Revised (WPPSI-R), which provides an FIQ, comprising verbal IQ (VIQ) and performance IQ (PIQ).21
Visual-motor integration was tested according to the Beery-Buktenica Developmental Test of Visual-Motor Integration (VMI).22
For logistic reasons, 5 patients living further away were examined at their local hospitals.
Two patients with HLHS could not be assessed with WPPSI-R because of their severe intellectual disability, and their MDI was instead determined according to the Bayley Scales of Infant Devel-opment23 by dividing their
develop-mental age by their calendar age. These scores were used instead of FIQ in the risk factor analysis as the best available estimate of their developmental level, but their neuro-psychological results were not in-cluded in the comparison between the groups. The parents were interviewed according to the Vineland Adaptive Behavior Scales (VABS) to obtain reports on the adaptive behavior of the children in their daily environment.24
A physiotherapist assessed gross and
TABLE 1 HLHS and UVH Patients Examined at a Median Age of 5.1 Years (n= 36): Diagnoses and Operations Performed
Operation Diagnosis n Age, d CPB Time, min RLFP Time, min DHCA Time, min Aortic Cross-Clamp Time, min Primary operation
Norwood HLHS 23 7 (3–18) 177 (137–252) 72 (40–106) 5 (2-9) 44 (17–68) Norwood/DKS UVH 5 8 (4–37) 175 (116–181) 61 (42–81) — 44 (23–77)
Other UVH 7 2 (1–31) — — — —
No operation UVH 1
BDG operation 36 184 (63–394) 88 (48–232) 22 (8–50) 2 14 (4–106) (n= 34) (n= 9) (n= 1) (n= 7) TCPC operation 36 1054 (775–1769) 89 (43–166) 5 26 47 (6–108)
(n= 1) (n= 1) (n= 24) Additional operation
HLHS 5 140 (1–1940) 98 (34–132) 27 (25–29) — 57 (32–81) (n= 4) (n= 2) (n= 2) UVH 4 94 (44–132) 93 (81–139) — — —
(n= 3)
2 additional operations HLHS 3 677 (99–1624) 121 (92–148) — 20 — 3 additional operations HLHS 1 588 110 21 — —
fine motor skills according to the Move-ment AssessMove-ment Battery for Children (Movement ABC) test. This standardized test for gross andfine motor functions yields a total impairment score and im-pairment scores for 3 subtests (Table 3).25
An EEG recording and a brain MRI scan (Philips Intera 1.5 T; T1-weighted sag-ittal, T2-weighted axial and coronal,
fluid-attenuated inversion recovery and
diffusion-weighted axial images) were performed on the patients when clini-cally indicated and at the age of 5 years.
Extensive collection of possible risk factors was performed as described earlier16 concerning patient-related
data, operations, and clinical follow-up until the study visit at age 5 years. In addition, ultrasound data were col-lected on the lowest diameter of the
ascending aortic arch in the pre-operative neonatal period. Parental reports on their socioeconomic status (level of education and occupation)26,27
were updated. All these data (Table 4) were tested for associations with the primary outcome variable FIQ/MDI.
Statistics
SPSS version 17.0 software (SPSS Inc, Chicago, IL) was used for statistical analysis. Kruskal-Wallis and Dunn tests were used for comparison of the con-tinuous outcome variables between the subgroups (patients with HLHS, pa-tients with UVH, and controls). The Fisher exact test with Bonferroni cor-rection for multiple comparisons was used for binary data. The Pearson correlation coefficient was used for normally distributed continuous fac-tors, and the Spearman correlation coefficient was used for nonnormally distributed continuous and categorical factors to assess their correlation with FIQ/MDI. For nonnormally distributed continuous factors, logarithmic trans-formation was used if it produced a normal distribution and correlated significantly with FIQ/MDI.
All factors significantly (P, .05) as-sociated with FIQ/MDI were included in a linear regression model adjusted for diagnosis (HLHS/UVH), gender, and maternal level of education. For this purpose, categorical factors were trans-formed into binary variables. Of those factors that measured closely related parameters, the one that correlated more significantly with FIQ/MDI was selected.
RESULTS
Neurologic Outcome
Abnormalities in the neurologic exami-nation were present in the majority of the patients, and they were most prevalent in gross andfine motor domains (Tables 2 and 5). The results of the neurologic examination were considered normal in
TABLE 2 Dysfunctional Clusters in Neurologic Examination Among Patient Groups and Controls
Functional Cluster Proportion (%) With Cluster Abnormality HLHS UVH Controls 1. Posture, muscle tone, and strengtha 5/23 (22)* 3/13 (23)* 0/40
Muscle tone regulation
Posture during sitting, standing, and walking Muscle strength
2. Gross motor function and balanceb 14/23 (61)** 8/13 (62)** 2/40 (5)
Kicking the hand of the examiner Romberg
Walking on heels and tiptoe Standing on 1 leg (10 s needed) Hopping on 1 leg (9 times needed) Walking along a straight line Balance in kicking a ball Catching a ball Jumping jacks
3. Fine motor function and coordinationc 15/23 (65)** 5/13 (39)* 3/40 (8)
Bead lacing Drawing
Cutting form from paper with scissors Finger-nose test
Fingertip-touching test Diadochokinesis
4. Choreiform dyskinesia 1/23 (4) 0/13 0/40 Spontaneous motor behavior of distal
and facial muscles Test with extended arms Face, eyes, tongue 5. Tendon reflexesd
Intensity and asymmetry (biceps jerk, triceps jerk, knee jerk, ankle jerk)
4/23 (17)* 1/13 (8) 0/40 Babinski sign
6. Cranial nervese 8/23 (35)** 1/13 (8) 0/40
Pupillary asymmetry and reactions Position and pursuit movements of eyes Visualfields
Motility of facial musculature Symmetry of soft palate Tongue motility Drooling
Criteria for dysfunctional cluster according to Hadders-Algra.17MND is defined as abnormality in at least 1 cluster. The findings of patients with cerebral palsy or other major neurodevelopmental impairments are included.
aOne or more consistent deviations in tone, strength, and/or posture. bAge-inadequate or abnormal performance in at least 2 functions. cClearly age-inadequate quality in 1 or mildly in 2.
dAt least 2 abnormal signs. eAt least 1 abnormal sign.
30% of the patients with HLHS (P ,
.001), and in 31% of the patients with UVH (P,.001), compared with 90% of the controls.
Neuropsychological Results
There were no significant differences in WPPSI-R and VMI results between the patients with HLHS and UVH, although the patients with HLHS performed more significantly below the controls (Table 3, Table 6, and Fig 2). Three patients, all with HLHS, had in-tellectual disability (defined as FIQ/ MDI ,70 and significant limitations in adaptive behavior). All 3 had an eventful recovery from the Norwood I operation with clinical seizures. Two of them showed global ischemic brain damage in early MRI and were later diagnosed with severe intellectual disability.
Motor Function
Four patients with HLHS (21%), 3 with UVH (25%), and 3 control children (8%) performed in gross and fine motor function according to the Movement ABC test in the borderline range, and 6 (32%), 3 (25%), and 1 (3%), respectively,
in the clearly abnormal range (Table 3). These results were highly congruent with thefindings in the neurologic ex-amination; those children with abnor-mal gross motor function (Table 2) had significantly higher (ie, worse) total scores in the Movement ABC (16.8 vs 4.1,P,.001), and, similarly, those with abnormalfine motor function had sig-nificantly higher scores in the manual dexterity subdomain (6.5 vs 2.1, P ,
.001).
Adaptive Behavior
Three patients with HLHS had adaptive behavior composite scores below the normative22 SD level of 70 (Table 3). The VABS scores correlated significantly with the corresponding professional assessments (VABS composite scores with FIQ/MDI,r= 0.632,P,.001; verbal communication subdomain with VIQ,r= 0.550,P,.001; motor skills subdomain with Movement ABC, r= 20.627,P,
.001). In addition, the motor skill sub-domain scores were associated with abnormal gross motor function (84.4 vs 104.0,P,.001) andfine motor function (82.6 vs 103.5,P,.001) in the neuro-logic examination.
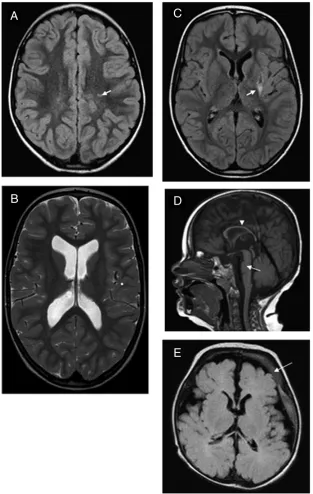
MRI and EEG
MRI was performed on 26 patients (17 with HLHS and 9 with UVH). The ab-normalities observed in MRI (Table 5, Fig 3) predominantly comprised is-chemic changes of different degrees. The patients with prominent MRI lesions (more severe than 1 or 2 minimal is-chemic lesions) had significantly lower cognitive performance (median FIQ/MDI 89.0 vs 107.0, P = .048) and worse Movement ABC results (20.5 vs 8.0,P= .015) and VABS composite scores (85.0 vs 98.5,P= .002) than the other patients. They all had either major neuro-developmental impairment (8/13) or minor neurologic dysfunction (MND; 5/ 13,P= .039 for the difference compared with the others, of which 8/13 had MND). No patient with normal results on the neurologic examination had any prom-inent MRIfindings.
Twenty-nine patients (16 with HLHS and 13 with UVH) underwent EEG recording. The EEG abnormalities (Table 5) included diffuse background abnormality in 1, asymmetry in 1, and epileptiform activity (either spiking or spike-wave discharges) in 7 patients. Of the patients with major neurodevelopmental impairment, 71%
TABLE 3 Neurodevelopmental Results for Patients With HLHS, Patients With UVH, and Controls
HLHS, Median (Range) UVH, Median (Range) Control, Median (Range) HLHS Versus Control,P UVH Versus Control,P
FIQ (WPPSI-R) 97 (45–122) 112 (81–132) 121 (97–139) ,.001 .024 VIQ 100 (50–121) 111 (76–126) 118 (96–136) ,.001 .051 PIQ 98 (61–121) 108 (94–127) 117 (98–130) ,.001 NS
(n= 21) (n= 13) (n= 40)
VMI 8 (4–13) 9 (5–15) 12 (7–16) ,.001 NS (n= 19) (n= 13) (n= 40)
VABS 90 (42–111) 101 (78–116) 104 (90–123) ,.001 NS Communication 91 (40–106) 100 (72–123) 101 (81–129) .002 NS Daily living skills 93 (38–115) 96 (89–117) 100 (81–125) .011 NS Socialization 95 (51–126) 102 (85–114) 110 (81–126) .008 NS Motor skills 90 (43–114) 100 (78–121) 100 (88–131) .001 NS
(n= 20) (n= 11) (n= 32)
Movement ABC 11 (1–34) 11 (1–29) 3 (0–20) .002 .003 Manual dexterity 3 (0–13) 3 (0–12) 2 (0–9) NS NS Ball skills 3 (0–7) 0 (0–6) 0 (0–4) .024 NS Balance 5 (0–14) 6 (1–13) 1 (0–11) .004 ,.001
(n= 19) (n= 12) (n= 39)
(5/7) had abnormal EEG results, com-pared with 18% (4/22,P= .016) of those with either MND or a normal neuro-logic examination results.
Risk Factor Analysis
Because the maternal level of education (median 5.0 vs 6.0,P= .035) and occu-pation (median 4.0 vs 3.0, P = .041)
were significantly lower among pati-ents with HLHS compared with con-trols, 2-way univariate analysis of variance was used to adjust for socio-economic status. There was no in-teraction between maternal skill level and patient group (P= .484). The main effect for patient group was statisti-cally significant (P , .001), but the
effect for maternal occupational skill level was not (P= .112).
In the linear regression model (Table 7), 5 factors related to the primary and BDG operations, and the preoperative car-diac status correlated significantly with FIQ/MDI, with an explanation rate of 76%. The most important correlate was a history of clinical seizures in connec-tion with the primary operaconnec-tion. These were most often clonic or tonic con-vulsions that appeared between post-operative days 4 and 12. Routine EEG recording performed on the same or following day revealed spikes or dis-charges. These seizures were also re-lated to a significantly smaller relative head circumference at the age of 5 years (median21.85 vs20.30 SD,P= .003). Prominent MRI abnormalities were seen in 7 of 9 of those with seiz-ures during the follow-up compared with 6 of 17 of those without (P= .048). Of the significant predictors of cognitive outcome, the highest hematocrit after the BDG operation was also higher in those with prominent MRI abnormali-ties (48.4 vs 43.4,P= .002).
After excluding the 2 outliers, a history of clinical seizures in connection with the primary operation (P , .001), significant preoperative atrioventric-ular (AV) valve regurgitation (P = .047), and reduced cardiac function after the BDG operation (P = .031) remained, and the neonatal diameter of the aortic arch (P= .016) emerged as a risk factor, with an overall ex-planation rate of 64%.
Longitudinal Comparison of the Follow-up Results
After the previous neurodevelopmental evaluation at the age of 30 months, 2 patients experienced a cerebral infarct leading to hemiplegia: on the seventh postoperative day after the TCPC op-eration in one, and 58 months after TCPC in the other. The FIQ results correlated significantly with MDI at the age of
TABLE 4 Data Used in the Risk Factor Analysis
Patient-related data Operative data (stage I, II, and III operations, continued) Maternal level of education Postoperative laboratory values (0–6 h, 6–24 h,
24–48 h, 48–72 h) Maternal level of occupation Highest lactate (mmol/L) Paternal level of education Highest/lowest arterial pH Paternal level of occupation Highest/lowest hematocrit (%) Gestational age (wk) Recovery period
Apgar 1 min Time in respirator (h) Apgar 5 min ICU stay (d) Maternal smoking during pregnancy (y/n) Hospital stay (d)
Gender Inotropic agents used (number of agents and days) Fetal diagnosis of cardiac defect (y/n) Nitric oxide inhalation used (y/n and days) Pregnancy/delivery complications (y/n) Diuresis 0–24 h, 24–48 h, and 48–72 h
(mL/kg per h)
CHD in family (y/n) Postoperative dialysis (y/n and hours) Developmental problems in family (y/n) Postoperative complications (y/n and number)a
Birth head circumference (cm and relative in SD)
Impaired postoperative systolic cardiac function (y/n)
Birth height (cm and relative in SD) Postoperative seizures (y/n) Birth weight (kg and relative weight for
height index)
Perioperative resuscitation (y/n) Preoperative data Before stage II and III
Lowest diameter of ascending arch on US (mm)
Preoperative O2saturation
Nonphysiologic AV valve regurgitation on US (y/n)
Preoperative NYHA
Restricted foramen ovale on US (y/n) Preoperative impaired cardiac function on US Impaired cardiac function on US (y/n) Follow-up data
Presence of ductalflow on US (y/n) Cumulative number of operations Lowest base excess in capillary/arterial
blood
Intermediate systolic cardiac function impaired (y/n)
Need of inotropic agents (y/n) Intermediate recoarctation of aorta (y/n) Use of prostaglandin infusion (y/n) Intermediate nonphysiological AV valve
regurgitation (y/n)
Operative data (stage I, II, and III operations) Complication in catheterizations (y/n) Age at the operation (d) Height (cm and relative in SD)
Norwood operation performed (y/n) Weight (kg and relative weight for height index %) DHCA (y/n and time in minutes) Head circumference (cm and relative in SD) CPB (y/n and time in minutes) Cumulative CPB time (min)
RLFP (y/n and time in minutes) Cumulative DHCA time (min) Aortic cross-clamping (y/n and time
in minutes)
Cumulative RLFP time (min)
Level of hypothermia (°C) Cumulative aortic cross-clamping time (min) Duration of hypothermia (min) Seizures during follow-up (y/n)
Rate of cooling (°C/min) Resuscitations during follow-up (y/n) Rate of rewarming (°C/min)
30 months (r= 0.731,P,.001), and the Griffiths general development at the age of 12 months (r= 0.436,P,.001). The Movement ABC results correlated significantly with earlier motor devel-opment (psychomotor develdevel-opmental indexes,r=20.490,P,.001; Alberta Infant Motor Scale,r = 20.500, P,
.001; Griffiths motor subdomain,r=2 0.527,P,.001).
DISCUSSION
Our prospective follow-up results from a nationwide sample of patients with HLHS or UVH revealed a significantly lower cognitive outcome at preschool age among each patient group in com-parison with the controls. Despite improved surgical treatment, the im-plementation of RLFP to replace DHCA, and high survival rates, different degrees
of neurodevelopmental deficits were still found in the majority of patients. In comparison with our earlier cohort of patients born between 1995 and 1999,28 which included most of the
earliest Norwood survivors in Finland and were operated on before the application of RLFP, a similar percentage of patients presented with major neu-rodevelopmental impairment: 26% in the present and 29% in the earlier co-hort of the patients with HLHS, and 23% and 20% in the cohorts of the patients with UVH, respectively. Other recent studies on the early development of patients with HLHS operated on at the beginning of this century also support the paucity of improvement in the neurodevelopmental outcome of these patients.6–11
There is growing evidence that the ce-rebral circulation in patients with HLHS is already diminished during fetal life because of impaired antegradeflow in the aortic arch.29,30 This leads to
im-paired brain growth and maturation30–33
and increases the risk of white matter injury atypical for term infants.13,14,33
Therefore, we added the diameter of the ascending aortic arch to our risk factor analysis, and it correlated significantly with FIQ in multiple linear regression analysis after excluding 2 outliers with global ischemic brain damage. This
finding suggests that impaired fetal cerebral circulation may contribute to later neurodevelopmental deficits.
Our risk factor analysis revealed no sig-nificant associations with support times or support-related techniques, but sev-eral correlates of cognitive outcome related to the primary and BDG oper-ations with a high explanation rate, suggesting a multifactorial etiology of cognitive deficits. A history of clinical seizures in connection with the primary operation was the strongest correlate, clearly indicating brain injury, especially because seizures were also related to microcephaly and MRI abnormalities.
TABLE 5 Neurologic and Neuroradiological Findings and Growth at a Median Age of 5.1 (Range, 5.0–5.4) Years
HLHS,n(%) UVH,n(%) Control,n(%) Mild muscle hypotonia 12/23 (52) 5/13 (38) 5/40 (13) MND 10/23 (43) 6/13 (46) 4/40 (10) Major neurodevelopmental impairment 6/23 (26) 3/13 (23) 0
Hemiplegia 3/23 (13) 2/13 (15) 0 Intellectual disability 3/23 (13) 0 0 Sensorineural hearing deficit 0 1/13 (8) 0 Bilateral vocal cord paresis 1/23 (4) 0 0 Seizures at any time 6/23 (26) 3/13 (23) 0 Active epilepsy 3/23 (13) 0 0 Abnormal EEG at 5 y (n= 29) 6/16 (38) 3/13 (23)
Abnormal brain MRI (n= 26) 14/17 (82) 5/9 (56) Ischemic changes
Global 2/17 (12) 0 Infarct 4/17 (24) 2/9 (22) Diffuse 0 1/9 (11) Minimala 5/17 (29) 1/9 (11)
Volume loss
Cortical 1/17 (6) 0 Central 1/17 (6)b 1/9 (11)c
Microhemorrhages 1/17 (6) 1/9 (11)c
Received any therapy 13/23 (57) 6/13 (46) 7/40 (18) Physiotherapy 7/23 (30) 5/13 (39) 2/40 (5) Speech therapy 10/23 (44) 2/13 (15) 5/40 (13) Occupational therapy 7/23 (30) 2/13 (15) 0 Head circumference,22 SD 4/23 (17) 1/13 (8) 0 Height,22 SD 2/23 (9) 1/13 (8) 0
Intellectual disability was defined as significant limitations in intellectual functioning (FIQ/MDI,70) and in adaptive behavior (VABS composite score,70).
aIndicating 1 or 2 minimal focal ischemic lesions, located most often in the centrum semiovale. bThis patient also had atrophy of vermis.
cOne patient had both central volume loss and microhemorrhages.
TABLE 6 WPPSI-R Subtest Results for Patients With HLHS, Patients With UVH, and Controls at a Median Age of 5.1 (Range, 5.0–5.4) Years
HLHS UVH Control HLHS Versus Control UVH Versus Control Information 11 (3–15) 12 (8–15) 13 (8–16) ,.001 NS Comprehension 11 (5–16) 11 (2–15) 12 (5–15) NS NS Arithmetic 9 (4–14) 10 (8–15) 13 (9–17) ,.001 .005 Vocabulary 10.5 (4–16) 12 (6–16) 13 (5–18) .013 NS Similarities 11.5 (6–16) 13 (6–17) 14 (8–18) .011 NS Object assembly 11 (5–17) 12 (8–16) 12 (5–18) .040 NS Block design 10 (1–15) 10 (8–13) 12 (8–17) .002 NS Mazes 8 (2–17) 10 (5–15) 11 (8–17) ,.001 NS Picture completion 11 (1–15) 12 (10–15) 13 (9–15) ,.001 NS
Other studies on children with CHD have also associated clinical or electro-graphic seizures with a worse cognitive outcome.3,4,11In the early postoperative
period after the Norwood operation, regional cerebral oxygenation de-creases and is significantly influenced by the systemic hemodynamics.34 In
our patients, a clinically significant neonatal AV valve regurgitation and impaired cardiac function after the BDG operation increased the risk of brain damage, most likely because of impaired hemodynamics. A high he-matocrit level after the BDG operation, leading to higher blood viscosity, cor-related with both worse motor de-velopment at the age of 30 months and lower cognitive development at the age of 5 years. These values, ranging from 40% to 59%, may have led to a de-creased microcirculatory bloodflow or increased risk of thrombosis and thus impaired cerebral oxygen supply. The hematocrit level as well as a history of seizures during the follow-up were also significantly associated with prom-inent abnormalities in MRIfindings. As a potentially modifiable factor, the he-matocrit level presents 1 possibility to optimize the postoperative care of these patients.
In addition to the postoperative hemat-ocrit level, the reduced cardiac systolic function after the BDG operation also emerged as a significant risk factor at the age of 30 months.16The stay in the
respirator after stage I correlated sig-nificantly with both MDI and FIQ, but it is also strongly related with the duration of inotrope use, which had an even more significant correlation with FIQ and was therefore chosen for linear regression. The maternal level of education corre-lated significantly with MDI, and its correlation with FIQ also approached significance (P = .072). Height was a significant predictor of MDI, but growth parameters were only significant pre-dictors of FIQ in the univariate, not in the
FIGURE 2
multivariate analysis. Surprisingly, the history of seizures was not a significant factor in the risk factor analysis at the age of 30 months, but in the less
com-prehensive analysis at the age of 1 year it was. In multivariate models with sev-eral risk factors and a rather small number of patients, some factors may
emerge as significant by chance, which may explain the differences between results at different ages. However, it is clear that these patients may experi-ence brain damage with multiple inter-acting mechanisms at different phases of treatment and even before treatment. Most of the significant factors in our analysis represent factors that are phys-iologically plausible and have potential clinical relevance. Thus, these results may help in optimizing treatment and in recognizing patients with the highest risk of neurodevelopmental sequelae.
The impact on later neurodevelopment of the often transitory pre- and post-operative white matter injury reported in neonates with HLHS or other forms of CHD13,33 remains unknown. Few
neu-roradiological studies have been con-ducted at a later age on Fontan survivors. MRI abnormalities, mostly previous ischemia or infarction, were found in half of these patients at the age of 34 to 96 months, but did not correlate with the cognitive outcome.4
In our earlier cohort, 4 of 6 of patients with HLHS and 2 of 13 of those with UVH had abnormalities in brain computed tomography scans or MRI at the age of 5 to 7 years.28In the current study, we
observed different degrees of ischemic MRI changes or volume loss in the majority of the patients who un-derwent imaging. Prominent changes were significantly associated with cognition, motor scores, abnormalities in the neurologic examination, and also adaptive behavior reported by the parents. Of those 8 patients with either infarct or global ischemic damage on MRI, in 5 the occurrence of clear neu-rologic symptoms could date the insult to the I or II postoperative stage. Three others experienced a brain infarct be-tween the ages of 1 and 5 years, 2 of them without a connection to any op-eration. Thus, these patients remain at risk for major brain injury outside the stages of palliative surgery.
FIGURE 3
The cognitive and motor develop-mental assessments at the age of 5 years correlated significantly with the earlier longitudinal follow-up results at the age of 12 and 30 months. Thus, neurodevelopmental impairments could often be recog-nized in early infancy. Multipro-fessional assessments of different developmental domains at the age of 5 years yielded similar results com-pared with each other and with pa-rental reports. Probably owing to a more accurate assessment at this older age, and to the age-related in-crease in the complexity of brain
function,35 neurologic abnormalities
were found more often than earlier. They mainly included difficulties in gross and fine motor functions and balance, which are known to be the most disturbed areas of functioning among patients with CHD.3,7–11,28 A
recent volumetric study on infants with different forms of CHD several months after cardiac surgery re-vealed that the frontal gray matter volume was reduced, especially in those patients with preoperative hypoxia or a diagnosis of HLHS. This reduction correlated weakly with impaired psychomotor development,
attributable to the motor cortex lo-cated in this area.32
Methods of neuromonitoring such as near-infrared spectroscopy, transcranial Doppler, and continuous EEG recording, which were not yet in use at our clinic during this study, may help in detect-ing vulnerable peri- and postopera-tive periods, which may relate to the neurodevelopmental outcome.14,36
Whether an improved neurodevelop-mental outcome is achievable needs to be further evaluated with prospective studies. The prevention of brain injury alongside improvement in survival rates among patients with complex CHD remains the main future challenge in pediatric heart surgery.
CONCLUSIONS
At the age of 5 years, neurodevelop-mental deficits were frequently found in patients with UVH, and especially in those with HLHS, and were associated with ischemic findings on brain MRI. Despite declining mortality rates, im-provement in the neurodevelopmental outcome during recent decades thus remains limited. Risk factors identified were the narrowness of the ascending aortic arch leading to impaired fetal cerebral circulation and hemodynamic factors related to the first operative stages performed in infancy. Never-theless, neurologic injury can occur at any phase, and clinical seizures are indicators of brain damage.
ACKNOWLEDGMENT
We thank Professor Seppo Sarna for statistical advice during this study.
REFERENCES
1. Norwood WI, Lang P, Hansen DD. Physio-logic repair of aortic atresia-hypoplastic left heart syndrome. N Engl J Med. 1983; 308(1):23–26
2. Rogers BT, Msall ME, Buck GM, et al. Neu-rodevelopmental outcome of infants with
hypoplastic left heart syndrome.J Pediatr. 1995;126(3):496–498
3. Mahle WT, Clancy RR, Moss EM, Gerdes M, Jobes DR, Wernovsky G. Neurodevelopmental outcome and lifestyle assessment in school-aged and adolescent children with
hypoplastic left heart syndrome. Pediat-rics. 2000;105(5):1082–1089
4. Goldberg CS, Schwartz EM, Brunberg JA, et al. Neurodevelopmental outcome of patients after the Fontan operation: a comparison between children with hypoplastic left TABLE 7 Significant Risk Factors for a Poor Cognitive Outcome in Patients With HLHS or UVH in
Univariate and Multivariate Analysis
Univariate Median P Univariate Correlation Coefficient
P MultivariateP
With Variable
Without Variable Preoperative factors
Maternal level of education.4 (22 vs 14)
107.0 94.5 .032a NS
AV valve regurgitation (10 vs 26) 89.0 106.0 .050b .041a
Diameter of aortic arch (mm,n= 28) 0.396 .037a NSa
Primary operation
Respiratory timec 20.381 .024b
Duration of the use of inotropic agents 20.559 ,.001b .023b
Seizure (6 vs 29) 57.5 105.0 .001a ,.001a
BDG operation
Highest hematocrit 6–24 h postoperatively
20.444 .007b 0.004b
Duration of the use of inotropic agents 20.360 .031a NS
Reduced cardiac function (8 vs 28) 87.0 106.0 .015a .016a
TCPC operation
Lowest arterial pH 6–24 h 0.464 .004a NS
Lowest arterial pH 24–48 h 0.473 .004a NS
Cumulative
Relative height at age 5 y 0.530 .001a NS
Relative head circumference at age 5 y 0.577 ,.001b
Seizure by age 5 y (9 vs 27) 74.0 107.0 .001a
The results are presented for the whole study group, but footnotes are used to indicate the results with the 2 outliers excluded. NS, not significant.
aSignificant after exclusion of 2 outliers who were examined with Bayley Scales of Infant Development. bNonsignificant after exclusion of 2 outliers.
heart syndrome and other functional sin-gle ventricle lesions.J Pediatr. 2000;137(5): 646–652
5. Wernovsky G, Stiles KM, Gauvreau K, et al. Cognitive development after the Fontan operation. Circulation. 2000;102(8):883– 889
6. Tabbutt S, Nord AS, Jarvik GP, et al. Neu-rodevelopmental outcomes after staged palliation for hypoplastic left heart syn-drome.Pediatrics. 2008;121(3):476–483 7. Atallah J, Dinu IA, Joffe AR, et al; Western
Canadian Complex Pediatric Therapies Follow-Up Group. Two-year survival and mental and psychomotor outcomes after the Norwood procedure: an analysis of the modified Blalock-Taussig shunt and right ventricle-to-pulmonary artery shunt surgi-cal eras. Circulation. 2008;118(14):1410– 1418
8. Visconti KJ, Rimmer D, Gauvreau K, et al. Regional low-flow perfusion versus circu-latory arrest in neonates: one-year neuro-developmental outcome.Ann Thorac Surg. 2006;82(6):2207–2211, discussion 2211–2213 9. Goldberg CS, Bove EL, Devaney EJ, et al. A randomized clinical trial of regional cere-bral perfusion versus deep hypothermic circulatory arrest: outcomes for infants with functional single ventricle. J Thorac Cardiovasc Surg. 2007;133(4):880–887 10. Newburger JW, Sleeper LA, Bellinger DC,
et al; Pediatric Heart Network Inves-tigators. Early developmental outcome in children with hypoplastic left heart syn-drome and related anomalies: the single ventricle reconstruction trial. Circulation. 2012;125(17):2081–2091
11. Bellinger DC, Wypij D, Rivkin MJ, et al. Adolescents with d-transposition of the great arteries corrected with the arterial switch procedure: neuropsychological as-sessment and structural brain imaging. Circulation. 2011;124(12):1361–1369 12. Gaynor JW, Gerdes M, Nord AS, et al. Is
cardiac diagnosis a predictor of neuro-developmental outcome after cardiac sur-gery in infancy?J Thorac Cardiovasc Surg. 2010;140(6):1230–1237
13. Mahle WT, Tavani F, Zimmerman RA, et al. An MRI study of neurological injury before and after congenital heart surgery.Circulation. 2002;106(12 suppl 1):I109–I114
14. Dent CL, Spaeth JP, Jones BV, et al. Brain magnetic resonance imaging abnormalities
after the Norwood procedure using re-gional cerebral perfusion [retraction inJ Thorac Cardiovasc Surg. 2006;131(6):1226]. J Thorac Cardiovasc Surg. 2006;131(1): 190–197
15. Sarajuuri A, Lönnqvist T, Mildh L, et al. Pro-spective follow-up study of children with univentricular heart: neurodevelopmental outcome at age 12 months.J Thorac Car-diovasc Surg. 2009;137(1):139–145, e1–e2 16. Sarajuuri A, Jokinen E, Puosi R, et al.
Neu-rodevelopment in children with hypoplastic left heart syndrome.J Pediatr. 2010;157(3): 414–420, 420.e1–e4
17. Touwen BC. Examination of the Child With Minor Neurological Dysfunction. London, UK: William Heinemann Medical Books; 1979
18. Hadders-Algra M. Developmental coordination disorder: is clumsy motor behavior caused by a lesion of the brain at early age?Neural Plast. 2003;10(1-2):39–50
19. Kantero RL, Tiisala R. Studies on growth of Finnish children from birth to 10 years. V. Growth of head circumference from birth to 10 years. A mixed longitudinal study. Acta Paediatr Scand Suppl. 1971;220:27–32 20. Sorva R, Lankinen S, Tolppanen EM, Perheentupa J. Variation of growth in height and weight of children. II. After in-fancy.Acta Paediatr Scand. 1990;79(5):498– 506
21. Wechsler D. WPPSI-R. Wechsler Preschool and Primary Scale of Intelligence - Revised [in Finnish]. Helsinki, Finland: Psykologien kustannus; 1995
22. Beery K. TheBeery-Buktenica Developmental Test of Visual-Motor Integration: VMI With Supplemental Developmental Tests of Visual Perception and Motor Coordination: Admin-istration, Scoring and Teaching Manual. Parsippany, NJ: Modern Curriculum Press; 1997
23. Bayley N. Manual for the Bayley Scales of Infant Development. 2nd ed. San Antonio, TX: Psychological Corporation; 1993 24. Sparrow SS, Balla DA, Cicchetti DV.Vineland
Adaptive Behavior Scales, Second Edition: Survey Forms Manual. San Antonio, Texas: AGS Publishing; 2005
25. Henderson SE, Sudgen DA. Movement As-sessment Battery for Children Manual. London, UK: The Psychological Corporation Ltd.; 1992
26. Unesco. International Standard Classifi ca-tion of Educaca-tion (ISCED). Paris, France: Unesco; 1997
27. International Labour Office. International Standard Classification of Occupations. Geneva, Switzerland: ILO; 1990
28. Sarajuuri A, Jokinen E, Puosi R, et al. Neu-rodevelopmental and neuroradiologic out-comes in patients with univentricular heart aged 5 to 7 years: related risk factor analysis. J Thorac Cardiovasc Surg. 2007; 133(6):1524–1532
29. Kaltman JR, Di H, Tian Z, Rychik J. Impact of congenital heart disease on cerebrovas-cular blood flow dynamics in the fetus. Ultrasound Obstet Gynecol. 2005;25(1): 32–36
30. Limperopoulos C, Tworetzky W, McElhinney DB, et al. Brain volume and metabolism in fetuses with congenital heart disease: evaluation with quantitative magnetic res-onance imaging and spectroscopy. Circu-lation. 2010;121(1):26–33
31. Shillingford AJ, Ittenbach RF, Marino BS, et al. Aortic morphometry and microceph-aly in hypoplastic left heart syndrome. Cardiol Young. 2007;17(2):189–195 32. Watanabe K, Matsui M, Matsuzawa J, et al.
Impaired neuroanatomic development in infants with congenital heart disease. J Thorac Cardiovasc Surg. 2009;137(1): 146–153
33. Andropoulos DB, Hunter JV, Nelson DP, et al. Brain immaturity is associated with brain injury before and after neonatal cardiac surgery with high-flow bypass and cerebral oxygenation monitoring. J Thorac Cardiovasc Surg. 2010;139(3):543– 556
34. Li J, Zhang G, Holtby H, et al. The influence of systemic hemodynamics and oxygen transport on cerebral oxygen saturation in neonates after the Norwood pro-cedure.J Thorac Cardiovasc Surg. 2008; 135:83–90
35. Hadders-Algra M. Two distinct forms of mi-nor neurological dysfunction: perspectives emerging from a review of data of the Groningen Perinatal Project.Dev Med Child Neurol. 2002;44(8):561–571
DOI: 10.1542/peds.2012-0486 originally published online November 19, 2012;
2012;130;e1636
Pediatrics
Valanne and Tuula Lönnqvist
Anne Sarajuuri, Eero Jokinen, Leena Mildh, Anna-Mari Tujulin, Ilkka Mattila, Leena
Services
Updated Information &
http://pediatrics.aappublications.org/content/130/6/e1636 including high resolution figures, can be found at:
References
http://pediatrics.aappublications.org/content/130/6/e1636#BIBL This article cites 28 articles, 7 of which you can access for free at:
Subspecialty Collections
http://www.aappublications.org/cgi/collection/cardiology_sub
Cardiology
http://www.aappublications.org/cgi/collection/surgery_sub
Surgery
following collection(s):
This article, along with others on similar topics, appears in the
Permissions & Licensing
http://www.aappublications.org/site/misc/Permissions.xhtml in its entirety can be found online at:
Information about reproducing this article in parts (figures, tables) or
Reprints
DOI: 10.1542/peds.2012-0486 originally published online November 19, 2012;
2012;130;e1636
Pediatrics
Valanne and Tuula Lönnqvist
Anne Sarajuuri, Eero Jokinen, Leena Mildh, Anna-Mari Tujulin, Ilkka Mattila, Leena
Heart
Neurodevelopmental Burden at Age 5 Years in Patients With Univentricular
http://pediatrics.aappublications.org/content/130/6/e1636
located on the World Wide Web at:
The online version of this article, along with updated information and services, is
by the American Academy of Pediatrics. All rights reserved. Print ISSN: 1073-0397.