Mohamed et al. World Journal of Pharmaceutical Research
DETECTION OF BACTERIAL AGENTS CAUSING URINARY TRACT
INFECTION AMONG CHILDREN IN KHARTOUM STATE
*Huzaifa Abdallh Mimouna Mohamed and Magdi Babiker
Department of Microbiology& Immunology Al-Yarmouk College Medical Laboratories Science Program Khartoum.
ABSTRACT
Background: Tract infection (UTI) is one of the most common pediatric infections. It distresses the child, concerns the parents and may cause permanent kidney damage. Aim: To evaluate the frequency of the bacterial agents responsible for urinary tract infections among
children from age 5-15 and the antimicrobial sensitivity profile of the uropathogens involved in these infectious processes. Methods: Questionnaire was conducted to collect the data from patient under study then (100) mid-stream urine sample was form children, cultured on bacteriological media, then isolated bacteria subjected to antibacterial susceptibility test. Results: According to the results, the 100 sample was verified into female (72.8%), while male (77.8%). the most frequent Gram negative bacteria were Escherichia coli 33%,
S.aurues 14%, Proteus mirabilis 7%, Others Staphylococcus 5%,
Enterobacter spp 4%, Pseudomonas aeruginosa 4%, Klebsiella pneumonia 3% Conclusion:
With regard to bacterial susceptibility to antimicrobial agents, it was noted that gram negative bacteria have higher resistance to, AMC, AMP.
KEYWORDS: Etiology, UTIs, Susceptibility, Antimicrobial, Resistance.
INTRODUCTION
Urinary tract infection (UTI) consists of microbial invasion and multiplication in any of the structures of the urinary system. The severity of infection ranges from asymptomatic colonization, or that is without tissue degeneration through to symptomatic invasion of the tissues of any of the structures of the urinary system.[1-2] World-wide, a minimum occurrence of 150 million symptomatic cases of UTIs are observed every year, however the real
Volume 5, Issue 11, 861-868. Research Article ISSN 2277– 7105
Article Received on 28 Aug. 2016,
Revised on 18 Sept. 2016, Accepted on 09 Oct. 2016
DOI: 10.20959/wjpr201611-7217
*Corresponding Author
Huzaifa Abdallh
Mimouna Mohamed
Department of
Microbiology&
Immunology Al-Yarmouk
College Medical
Laboratories Science
incidence is underestimated because a large portion of urinary infections are cured without medical follow up.[3] The etiology of UT infections is related to the great diversity of microbialinvaders, such as: bacteria, viruses and fungi. UTI in children may indicate serious anatomic abnormality like Vesicoureteral reflux (VUR), or neurogenic bladder. It is very necessary to identify children with UTI and treat them as soon as possible to avoid any long term complications and to reduce the risk of any significant morbidity. Unrecognized UTI may progress into renal damage, hypertension and end stage renal disease.[33] Misdiagnosis, delay in diagnosis, and treatment of pediatric urinary tract infection appears to cause renal
scarring and may produce hypertension and end-stage renal disease.[34,35]
MATERIALS AND METHODS Ethical consideration
After approval of the management of the Hospitals demonstration concerned authority the approval of the patient on their own free without using any mean of pressure and taken in account all professional ethic and the sample were collected by the patient.
Study population
The study was conduct among children suffering from symptom of urinary tract infection.
Sample Collection
One hundred of Fresh mid-stream urine (MSU) samples were collected inside sterile container from Children suspected to have UTIs. The samples were labeled and transported to the Medical laboratory of the AL Yarmouk college and were processed within 1to 2 hour after sample collection.
Isolation of bacteria
All samples were cultured on CLED media and MacConkey agar followed by incubation at 37 °C for 24 hours.
Antibiotic sensitivity test
Seeding of inoculums: A suspension of the tested organism was prepared and compared with the McFarland turbidity standard. A sterile cotton swab was immersed in the suspension and the excess fluid removed by pressing and rotating in the edge of the tube above the level of the suspension, followed by streaking the swab evenly over the surface of the Nutrient agar in four directions, rotate the plate
Application of antibiotic disc
Sterile forceps was used to place antibiotic discs. Within 10 minutes of applying the discs the plates was incubated aerobically at 37°C for 24 hours, after overnight incubation a ruler used to measure the antibiotic discs zones size and then reporting the organism as resistant, intermediated or sensitive (Cheesbrough, 2006).
Isolated were identified by bacteriological and biochemical methods.
RESULTS
Table: 1. Frequency of bacteria growth according to gender
Out of one hundred sample urine 70 showed positive bacterial growth (70%) total female were 55, 40 of them (72.8%) had urine bacterial growth while 30 (66.7%) male out of total 45 also showed urine bacterial growth (Table 1).
Gender Growth (%) No growth (%) Total (%) Male 30(66.7) 15 (33.3) 45 (45) Female 40(72.8) 15 (26.2) 55 (55)
Total 70(70) 30 (30) 100
Frequency between growth and age group
Related to age group, children age (5-10) years were 25 (80.7%) had high level of growth, in contrast those aged (11-15) years were 45 (66.7) with low level of growth (Table 2)
Table: (2) growth and no growth according to the age
Age group Growth (%) No growth (%) Total (%) Age 5-10
Age 11-15 Total
25(80.7) 45(65.3) 70(70)
6(19.3) 24(34.7)
30(30)
31(31) 79(79) 100(100)
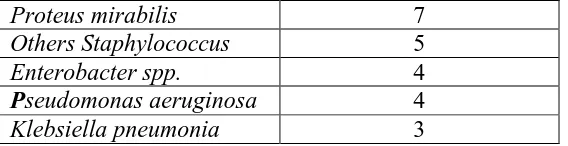
Population of bacteria among UTI
Different types of microorganism were isolated from urine ranging from gram negative bacteria were E.coli constituted (33%) followed by Staphylococcus aurues (14%) then
Proteus mirabilis (7%), other staphylococci (5%), Enterobacter spp. (4%), Pseudomonas
aeruginosa (4%) and Klebsiella pneumoniae (3%) (Table 3)
Table (3) Show the number of isolate pathogen
Pathogen Percentage (%) isolated
Escherichia coli 33
Proteus mirabilis 7
Others Staphylococcus 5
Enterobacter spp. 4
Pseudomonas aeruginosa 4
Klebsiella pneumonia 3
The frequency of bacteria according to age and gender
In the table (4) shows that in male and female was E.coli and according to age group from 5-10 and 11-15 was E.coli fallowed by second dominating bacteria.
Table (4).The frequency of bacteria according to age and gender
Pathogen Male
(%)
Female (%)
Age 5-10 (%)
Age 11-15 (%)
E.coli 13
(28.9)
20 (36.4)
10(40) 23 (51.2)
S.aurues 4 (8.8) 10
(18.2)
8 (32) 6 (13.3)
Proteus mirabilis 4 (8.8) 3 (5.4) 2 (8) 5 (11.1)
Others Staphylococcus 2 (4.4) 3 (5.4) 4 (16) 1 (2.2)
Enterobacterspp 3 (6.7) 1 (1.8) 1 (4) 3 (6.6)
Pseudomonasaeruginosa 3 (6.7) 1 (1.8) 0 (0) 4 (8.8)
3Klebsiellapneumonia 1 (2.3) 2 (3.7) 0 (0) (6.6)
Antimicrobial result
Then all positive samples was manipulated to antimicrobial sensitivity test The antimicrobial used was Amoxicillin, Ampicillin, Co-Trimoxazole, Cefotaxime, Norfloxacine, High resistance rate to AMP and AMC show in table (5)
Table (5) show the result of the antimicrobial n=70
AMC A MP CTX COT NX
Pathogen Numb Of path R % S % R % S % R % S % R% S% R% S%
E.coli 33 78.8 21.2 93.9 6.1 27.2 72.8 24.2 75.8 21.2 78.8
S.aurues 14 85.7 14.3 7.1 92.9 21.4 78.6 21.2 78.8 21.2 78.8
p. mirabilis 7 71.5 28.5 57.1 42.9 28.5 71.5 14.2 85.8 14.2 85.2
Others
Staphylococcus
5 60 40 0 100 80 20 100 0 40 60
Enterobacter Spp. 4 75 25 75 25 25 75 75 25 0 100
Pseudomonas aeruginosa
4 100 0 100 0 50 50 25 75 25 75
Klebsiella pneumonia
3 100 0 66.6 33.4 66.6 33.4 100 0 100 0
DISCUSSION
[image:4.595.158.442.72.145.2]female 55, the female was show high number of isolated bacteria 40 ( 72.8%) while male was 30(66.7%).
The patient under study was distribute into two age group, the age group which show high level of growth was (5-10 ) 25 (80.7%) than group (11-15), 45 (66.7%) respectively. The most frequent Gram negative bacteria were Escherichia coli 33%, S.aureus 14%, Proteus
mirabilis 7%, Others Staphylococcus 5%, Enterobacter spp. 4%, Pseudomonas aeruginosa
4%, Klebsiella pneumonia 3% This result was in disagreement with (Alo Moses.et al 2012)
due to his report that Staphylococcus aurues was dominate 43.6% and that could be to the personal hygiene and the method.
Other study in Nablus by (Raya Mohammad 2009) that E.coli was most dominated 51.8% and the two agree that female gender was the most effect gender than male The higher percentage of E.coli infection compared with the other organisms could be explained on the basis of their normal habitat in the intestinal tract that is why it is the most common organism founded. The gender difference should also be considered, since the urine orifice was so close to the anal opening. Most of the infections were observed in the second and third groups of age (5-10yrs) and this can be explained by their improper cleaning of themselves in the toilets and the bad hygiene status of their families. That is why they are more susceptible to the infection at this stage of life.
All the isolated bacteria showed different patterns of susceptibility and resistance to the available antibiotics. Higher resistant levels were detected in Amoxicillin, Ampicillin, respectively. These findings require careful selection of the drug for the treatment and management of UTIs among pediatrics.
CONCLUSION
In conclusion, study showed that bacteria have a great role in urinary tract infections (UTIs) among pediatrics constituting which caused by different type of microorganism.
RECOMMENDATIONS
1. In reference to the generated data from this study, it is recommended that; Carryout
2. Immediate contact with physician when suffering from problems in the urinary tract and
avoid having any medication before getting the results of urine analysis and urine culture.
3. Doctors are encouraged to ask their patients to do urine culture and sensitivity when they suspect UTI, in order to give the best treatment.
4. More health promotion programs are needed to be implemented at schools, to increase the awareness of students and their teachers and improve their healthy behaviors.
REFERENCES
1. Menezes EA, Carneiro HM, Cunha FA, Oliveira IRN, Ângelo MRF, Salviano MNC. Freqüência de microrganismoscausadores de infecçõesurináriashospitalaresempacientes do Hospital Geral de Fortaleza. Rev Bras AnálClín, 2005; 37(4): 243-6.
2. Modarres S, Nassiri N. Bacterial etiologic agents of urinary tract infection in children in the Islamic Republic of Iran. J. East Mediterr. Health, 1997; 3.
3. Goldman L, Ausiello D. Cecil – Tratado de MedicinaInterna. 22ª ed. Rio de Janeiro:
Guanabara Koogan; {32005.
4. Perugini MRE, Vidotto MC. Característicasclínicas e virulência de Escherichia coli
eminfecções do tratourinário. Semina, 1992; 13(2): 33-9.
5. Mendes CL, Araújo AA, Sena KXFR, Chiappeta AA. Prevalência de Candidasp.
eminfecçõesvaginais. NewsLab, 2005; 68: 104-12
6. Nicolle LE "Uncomplicated urinary tract infection in adults including uncomplicated
pyelonephritis". UrolClin North Am, 2008; 35(1): 1–12, v. doi:10.1016/j.ucl.2007.09.004.PMID 18061019.
7. Vieira JMS, Saraiva RMC, Mendonça LCV, Fernandes VO, Pinto MRC, Vieira ABR.
Suscetibilidadeantimicrobiana de bactériasisoladas de infecções do tratourinário de pacientesatendidos no Hospital Universitário Bettina Ferro de Souza, Belém-PA. Rev Bras AnálClín, 2007; 39(2): 119-21.
8. Polleto KQ, Reis C. Suscetibilidadeantimicrobiana de uropatógenosempacientesambulatoriaisnacidade de Goiânia, GO. Rev Soc Bras Med Trop, 2005; 38(5): 416-20.
10. Camargo ILBC, Maschieto A, Salvino C, Darini ALC. Diagnósticobacteriológico das
infecções do tratourinário – umarevisãotécnica. Medicina (RibeirãoPreto), 2001; 34(1): 70-8.
11. *.Blatt J M, Miranda MC. Perfil dos microrganismoscausadores de infecções do tratourinárioempacientesinternados. Rev PanamInfectol, 2005; 7(4): 10-4.
12. Bail L, Ito CAS, Esmerino LA. Infecção do tratourinário: comparação entre o perfil de susceptibilidade e a terapiaempírica com antimicrobianos. Rev Bras AnálClín, 2006; 38(1): 51-6.
13. Lane, DR; Takhar, SS. "Diagnosis and management of urinary tract infection and
pyelonephritis.". Emergency medicine clinics of North America, August, 2011; 29(3): 539–52. doi:10.1016/j.emc.2011.04.001. PMID 21782073.
14. Salvatore, S; Salvatore, S, Cattoni, E, Siesto, G, Serati, M, Sorice, P, Torella, M.
"Urinary tract infections in women.". European journal of obstetrics, gynecology, and reproductive biology, June 2011; 156(2): 131–6. doi:10.1016/j.ejogrb.2011.01.028. PMID 21349630.
15. Arellano, Ronald S. Non-vascular interventional radiology of the abdomen. New York:
Springer, 67. ISBN 978-1-4419-7731-1.
16. Bhat, RG; Katy, TA, Place, FC. "Pediatric urinary tract infections.". Emergency medicine
clinics of North America, August 2011; 29(3): 637–53. doi:10.1016/j.emc.2011.04.004. PMID 21782079.
17. Lucchetti G, Silva AJ, Ueda SMY, Perez MCD, Mimica LMJ. Infecções do tratourinário: análise da frequência e do perfil de sensibilidade dos agentescausadores de infecções do tratourinárioempacientes com cateterizaçãovesicalcrônica. J Bras Patol Med Lab, 2005; 41(6): 3839
18. Koneman EW, Allen SD, Janda WM, Schreckenberger PC. Diagnósticomicrobiológico – texto e atlas colorido. 5ª ed. Rio de Janeiro: Medsi; 2001.
19. Hinman F. Jr., “Bacterial elimination,” Journal of Urology, 1968; 99(6): 811-825.
20. Nicolle LE; Asymptomatic Bacteriuria: When to Screen and When to Treat. Infect. Dis.
Clin. North Am, 2003; 17(2): 367-94.
21. Lazarevic, G., Petreska, D., Pavlovic, S. Antibiotic sensitivity of bacteria isolated from
the urine of children with urinary tract infections from 1986 to 1995. SrpArhCelokLek. 1998 Nov-Dec;
22. Alper, B., Curry,S. Urinary Tract Infection in children. American Family physician, Dec,
23. *Alan J. Wein. Volume 4, Campbell-Walsh urology. 9th ed. China: Saunders Elsevier;
2007.
24. Ghedira, L., Messaoudi, A., Ben Meriem, C., Guediche, MN. Profile of antimicrobial resistance of agents causing urinary tract infections in children. Tunis Med., Mar, 2004; 82(3): 299-305.
25. Yuksel, S., Ozturk, B., Kavaz, A et al. Antibiotic resistance of urinary tract pathogens and evaluation of empirical treatment in Turkish children with urinary tract infections. Int J Antimicrob.
26. Tanagho, Emil A., Mcaninch, Jack W., editors. Smith's General Urology. United States of
America: McGraw-Hill companies Inc; 2004.Bacterial Infections of the genitourinary tract, 203-227.
27. Wu, CY., Chiu, PC., Hsieh, KS., Chiu, CL et al. Childhood urinary tract infection: a
clinical analysis of 597 cases. Acta Paediatr Taiwan, Nov-Dec, 2004; 45(6): 328-33. 28. Mangiarotti, P., Pizzini, C., Fanos, V. Antibiotic prophylaxis in children with relapsing
urinary tract infections. J chemother, Apr, 2000; 12(2): 115-23.
29. Ashkenazi, S., Even-Tov, S., Samra, Z., Dinari, G. Uropathogens of various populations
and their antibiotic susceptibility. Pediatr Infect Dis., Oct, 1991; 10(10): 742-6.0. 30. Asymptomatic urinary tract infection among school children in rural area of Ebonyi
State1Alo Moses, et.al.
31. Prevalence of Urinary Tract Infection among.
32. Children of Primary Schools in Nablus. Raya Mohammad Hussein Sawalha.
33. Ramadan, A. Prevalence of urinary tract infection in primary school children and its relation to school achievement in Ismailia Governorate [thesis]. Egypt : University of Cairo;2003.184p. Available from: Jordan university thesis center.
34. Sahi, R., Carpenter, C. Does This Child Have a Urinary Tract Infection?. Annals of Emergency medicine .2008
35. Adjei,O., Opoku, Ch. Urinary tract infections in African infants. International Journal of Antimicrobial Agents.2004 S32-S34.
36. Schlager, TA. Urinary tract infections in children younger than 5 years of age:
epidemiology, diagnosis, treatment, outcomes and prevention. Paediatr Drugs, 2001; 3(3): 219-27.
37. National Institute for Health and Clinical Excellence (NICE). Urinary tract infection in