Original Article
The application of evidence-based nursing and its
effect on reducing surgical incision infections and
improving patient satisfaction with nursing
Yanhua Wang1, Shujing Wei2, Dan Zhang2
1Jining No. 1 People’s Hospital Center Sterile Supply Department East Campus, Jining, Shandong, China; 2
Opera-tion Room, Jining No. 1 People’s Hospital, Jining, Shandong, China
Received September 23, 2019; Accepted December 11, 2019; Epub February 15, 2020; Published February 28, 2020
Abstract: Objective: Evidence-based nursing in the operating room was successfully applied, and its effect on post-operative infections and patient satisfaction was investigated. Methods: 84 patients were randomly divided into an observation group (OG) (n = 42) and a control group (CG) (n = 42). The patients in the OG were given evidence-based nursing in the perioperative period. The patients in the CG received routine nursing. The infection rate, psychologi-cal negative sentiment (SAS and SDS) at 1 week after surgery, the length of the hospital stay, VAS scores at 48 h after surgery, the incidences of postoperative complications, quality of life, and patient satisfaction one month after surgery were evaluated. Results: The surgical wound infection rate, SAS and SDS scores, VAS scores, hospital stays and the incidence of postoperative complications in the OG were lower than they were in the CG (P<0.05). The qual-ity of life and nursing satisfaction in the OG were higher than those in the CG (P<0.050). Conclusions: Perioperative evidence-based nursing can significantly reduce the surgical wound infection rate and improve patients’ negative emotions.
Keywords: Operating room, evidence-based nursing, surgical wound infection rate, nursing satisfaction
Introduction
As a place for surgery and rescue, the operat-ing room is also a high-risk place where patients have incision infections [1]. Once the surgical incision infection occurs, the surgical efficacy is seriously affected. In addition, multiple organ failure and systemic infection can easily occur [2, 3]. Therefore, the prevention of incision infection in the operating room has also become an important direction for hospitals to control incision infections [4]. Scientific and reasonable layouts and strict disinfection and sterilization of the operating room, and enough equipment are necessary for infection preven-tion [5].
However, which nursing model is more suitable for the operating room is always a controversial focus clinically. The selection of a suitable sur-gical nursing model is of important clinical sig-nificance [6] due to the fact that clinical care staff and other health care workers are the
frontline defense for applying daily infection control practices to prevent infections and the transmission of organisms to other patients. Clinical care nurses directly prevent infections by performing, monitoring, and assuring compli-ance with aseptic work practices. They provide knowledgeable collaborative oversight on envi-ronmental decontamination to prevent the transmission of microorganisms from patient to patient. They also serve as the primary resource to identify and refer ill visitors or staff [7]. Nurses can reduce the risk of infection by diminishing the entry of endogenous or exoge-nous organisms via invasive medical devices [8].
the literature, and other scientific and system-atic methods. The best nursing resources and the most professional nurses are combined. The most suitable nursing protocol is devel-oped according to the clinical experience and the actual needs of patients [10, 11]. Evidence-based nursing has become more and more widely used clinically. For example, a study [12] showed that evidence-based nursing in spinal instrument surgery can effectively reduce the infection rate of the surgical site. Another study [13] found that evidence-based nursing can remarkably improve the efficacy of surgery and the prognosis of patients with heart failure. However, the study of the application of evi-dence-based nursing in the operating room is not well recognized due to the lack of study. The following study was intended to contribute to the further understanding of the application of evidence-based nursing in the operating room and its effect on the surgical wound infection rate and patients’ nursing satisfaction.
Materials and methods
General information
84 patients in our hospital were selected as the subjects, including 51 males and 33 females. The patients were aged 40.61±6.57 years old on average. 14 patients underwent a urologic surgical procedure. 23 patients received orthopedic surgery. 26 patients un- derwent general surgery. 16 patients were given gynecology and obstetrics surgery. 5 patients received other surgeries. All the patients were randomly categorized into an observation group (OG) (n = 42) and a control group (CG) (n = 42). The patients in the OG were given evidence-based nursing in the periopera-tive period. The patients in the SG were given routine nursing.
The inclusion criteria were as follows: Patients aged 20-65 undergoing elective surgery with general anesthesia were included. All the patients had a surgical incision >2 cm.
The exclusion criteria were: Patients with surgi-cal contraindications; patients with infectious diseases; patients with severe hepatic and renal dysfunction; patients with a severe coag-ulation disorder or patients with cognitive and communication disorders; patients with
diabe-tes and severe immunodeficiency; patients with a wound infection before surgery; and patients with surgical incisions less than 2 cm, were all excluded.
All the patients and their family members agreed to the study protocol. The informed consent forms were signed. The study was approved by the Ethics Committee.
Nursing methods
The patients in the CG were given routine nurs-ing, including preoperative routine precautions. The nurses cooperated with the doctors to ensure proper nursing. The postoperative inci-sion was kept dry and clean. Routine diet instructions and rehabilitation guidance were provided for the patients.
the doctor to complete the surgery. If abnor- mal vital signs occurred, communication was made with the doctor in time. The measures were completed in a timely manner. (4) Postoperative nursing: After surgery, the patients were kept in the proper positions. All record lists in the operating room were carefully filled out. The medial devices were arranged and sent to the disinfecting department. The intervention ended when the patient left the operating room.
Outcome measures
(1) The surgical wound infection rates were recorded and compared between the two groups at one week after surgery. The patient had a purulent discharge from the incision, accompanied by an increase in body tempera-ture. Their infection was confirmed by a pa- thological examination. (2) The psychologi- cal negative sentiment before surgery and 1 week after surgery was evaluated with a self-rating anxiety scale (SAS) and a self-self-rating depression scale (SDS) [15]. The length of the hospital stay was compared. (3) The pain degree 48 h after surgery was evaluated with the VAS score [16]. (4) The postoperative complications were recorded and compared. The postoperative complications included fe- ver, wound bleeding, urinary retention, and deep venous thrombosis (5) QLQ-C30 [17] was used to evaluate the quality of life 1 month after nursing. The role function, physical func-tion, emotional funcfunc-tion, cognitive funcfunc-tion, and social function were included in the scale, 30 items in total. The higher the score was, the higher the quality of life was. (6) The patients’ nursing satisfaction on perioperative nursing was evaluated in the form of a questionnaire on the third day after surgery and was graded as very satisfied, satisfied, or not satisfied. Nursing satisfaction = (Number of patients very satis-fied + number of patient satissatis-fied)/total num-ber of patients × 100%.
Statistical methods
The experimental data in the study were sta- tistically analyzed with SPSS 18.0 (Beijing NDTimes Science and Technology Co., Ltd.). For intragroup before-after comparisons, pairwise t
tests were used; for the between-group com-parisons, independent t tests were used chi-squared tests were used for the comparisons of the enumeration data. P<0.05 implied a sig-nificant difference.
Results
Comparison of the general information
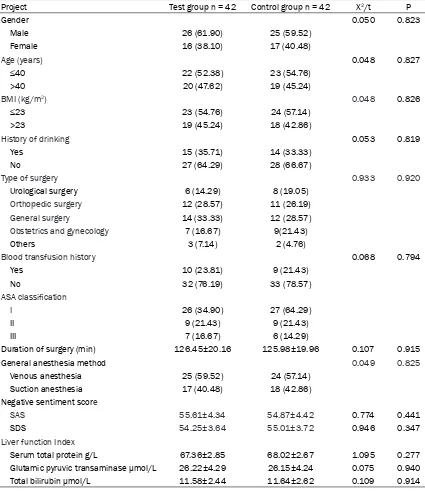
There was no difference in terms of gender, age, BMI, history of smoking, history of blood transfusion, negative emotional score, ASA classification, duration of surgery, liver func-tion, surgical type, or type of anesthesia between the two groups (Table 1, P>0.05).
Comparison of the surgical wound infection rates
One case of postoperative incision infection occurred in the OG. The incidence was 2.38%. 7 cases of postoperative incision infections occurred in the CG. The incidence in the CG was 16.67%, and it was higher than the rate in the OG (P<0.05) (Figure 1).
Comparison of psychological negative senti-ment 1 week after surgery
The SAS and SDS scores in the OG were (22.34±3.21) and (22.78±3.19) points respec-tively, which were lower than the scores in the CG (P<0.05) (Table 2).
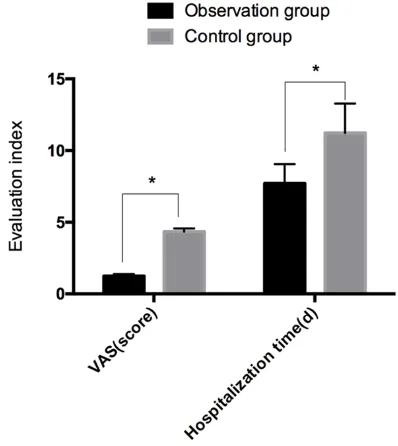
Comparison of postoperative VAS scores and hospital stays
The VAS scores and hospital stays in the OG were (1.24±0.14) points and (7.71±1.35) d. They were lower than the (4.35±0.22) points and (11.23±2.05) d in the CG respectively (P<0.05) (Figure 2).
Comparison of the postoperative complica-tions
Fever, wound bleeding, and urinary retention occurred in 2 patients, 1 patient, and 0 patien- ts in the OG. The total incidence of adverse reactions was 7.14%. 3 cases of fever, 4 cases of wound bleeding, and 4 cases of urinary retention occurred in the CG. The total inci-dence was 26.19%, and this was higher than the incidence in the OG (P<0.05) (Table 3).
Comparison of the quality of life 1 month after surgery
higher than the (65.34±2.12), (65.81±2.37), (65.51±3.04), (65.42±2.64), and (66.02±2.85) scores in the CG (P<0.05) (Table 4).
Comparison of nursing satisfaction
36 patients, 5 patients and 1 patient in the OG were respectively very satisfied, satisfied, and not satisfied. The numbers of patients who were very satisfied, satisfied, and not satisfied in the CG were respectively 19, 10, and 13. The nursing satisfaction in the OG was 97.62% and
this was higher than the 69.05% in the CG (P<0.05).
Discussion
[image:4.612.92.517.85.583.2]The operating room is the main place for the treatment of patients. The nursing work in the operating room is generally characterized by large personnel mobility and a long nursing time. Any carelessness is likely to lead to intra-operative infection and negatively affect the therapeutic effect [18, 19].
Table 1. General information table
Project Test group n = 42 Control group n = 42 X2/t P
Gender 0.050 0.823
Male 26 (61.90) 25 (59.52)
Female 16 (38.10) 17 (40.48)
Age (years) 0.048 0.827
≤40 22 (52.38) 23 (54.76)
>40 20 (47.62) 19 (45.24)
BMI (kg/m2) 0.048 0.826
≤23 23 (54.76) 24 (57.14)
>23 19 (45.24) 18 (42.86)
History of drinking 0.053 0.819
Yes 15 (35.71) 14 (33.33)
No 27 (64.29) 28 (66.67)
Type of surgery 0.933 0.920
Urological surgery 6 (14.29) 8 (19.05)
Orthopedic surgery 12 (28.57) 11 (26.19)
General surgery 14 (33.33) 12 (28.57)
Obstetrics and gynecology 7 (16.67) 9(21.43)
Others 3 (7.14) 2 (4.76)
Blood transfusion history 0.068 0.794
Yes 10 (23.81) 9 (21.43)
No 32 (76.19) 33 (78.57)
ASA classification
I 26 (34.90) 27 (64.29)
II 9 (21.43) 9 (21.43)
III 7 (16.67) 6 (14.29)
Duration of surgery (min) 126.45±20.16 125.98±19.96 0.107 0.915
General anesthesia method 0.049 0.825
Venous anesthesia 25 (59.52) 24 (57.14) Suction anesthesia 17 (40.48) 18 (42.86) Negative sentiment score
SAS 55.61±4.34 54.87±4.42 0.774 0.441
SDS 54.25±3.64 55.01±3.72 0.946 0.347
Liver function Index
During the nursing, there are some differences in the cooperation of nursing and treatment due to the differences among the patients. Therefore, many difficulties occur [20]. How- ever, the selection of the nursing model in the operating room has always been an important topic in clinical practice. Evidence-based nurs-ing combines the actual situations of the patients with the best evidence. It is scientific, rational, and rigorous. The nursing problems in actual situations are taken as the starting point. The nursing plan is developed by consult-ing the relevant literature and considerconsult-ing the specific situations of the patients [21, 22].
The application of evidence-based nursing in the operating room was investigated in this study. The results showed that the surgical wound infection rate in the OG was lower than it was in the CG. A 3-year prospective study [23] showed that evidence-based nursing in the operating room can effectively reduce the infection rate. This conclusion is consistent with the one in this study. This is mainly due to the improvement of surgical cleanliness
[24]. In this study, special attention has also been paid to the sterile operation of surgery. Further studies [24] also found that evidence-based nursing can effectively reduce the post-operative infection of cesarean section. The results showed that the negative senti- ment score, the VAS pain score, and the hospi-tal stay in OG were much lower than the corre-sponding scores in the CG. Moreover, the qual-ity of life was higher than it was in the CG (P<0.05). A previous study [25] showed that evidence-based nursing has a significant effect on the improvement of the quality of life. Another study [26] showed that evidence-based nursing combined with routine nursing can remarkably improve the treatment compli-ance and quality of life of elderly patients with peptic ulcers. A previous study [27] found that evidence-based nursing can effectively improve the depressive state of patients with depres-sion. All the above-mentioned results confirm the partial results in this study.
[image:5.612.92.292.72.265.2]Finally, the results showed that the nursing satisfaction in the OG was higher than it was in the CG. A study [28] showed that the imple- mentation of evidence-based nursing can effectively improve the nursing satisfaction of patients with acute coronary syndrome in the hospital. Another study [29] showed that the
[image:5.612.322.521.73.296.2]Figure 1. Comparison of the surgical wound infection rate. The postoperative surgical wound infection rate in the observation group (OG) was lower than it was in the control group (CG) (P<0.05). Note: *implied P<0.05.
Table 2. Comparison of the SAS and SDS scores at 1 week after surgery in both groups Project Test group n = 42 Control group n = 42 t P SAS 22.34±3.21 37.31±4.32 18.03 <0.001 SDS 22.78±3.19 36.99±4.27 17.28 <0.001
[image:5.612.90.292.364.415.2]perioperative application of evidence-based nursing in patients with peritoneal neuroblas-toma can significantly improve the nursing sat-isfaction of patients. It also indicated that evi-dence-based nursing can increase the degree of treatment participation of the patients and their family members. Furthermore, the clinical results can be improved. The conclusions in the study are confirmed by the studies above.
In summary, evidence-based nursing in the operating room can remarkably reduce the sur-gical wound infection rate. Meanwhile, the neg-ative sentiment is improved. The postoperneg-ative pain is alleviated. The hospital stay is short-ened. The quality of life is improved. Moreover, the patients have higher nursing satisfaction. It is worthy of being popularized clinically. However, there are some deficiencies in this study. For example, the nursing factors affect-ing the incision infection were not further ana-lyzed. Only the evidence-based nursing was simply compared with the routine nursing. The most suitable nursing model in the operating room was not investigated. Therefore, evi-dence-based nursing will be compared with other nursing models in a future study. Thus, more theoretical data are provided for the application of evidence-based nursing in the operating room.
Disclosure of conflict of interest
None.
gery in a tertiary care academic medical cen-ter: a valid measure of surgical quality? J Gastrointest Surg 2017; 21: 1048-1054. [2] Nelson RL, Iqbal NM, Kravets A, Khateeb R,
Raza M, Siddiqui M, Taha I, Tummala A, Epple R, Huang S and Wen M. Topical antimicrobial prophylaxis in colorectal surgery for the pre-vention of surgical wound infection: a system-atic review and meta-analysis. Tech Coloproc-tol 2018; 22: 573-587.
[3] Cetinkaya RA, Yilmaz S, Unlu A, Petrone P, Marini C, Karabulut E, Urkan M, Kaya E, Kara-bacak K, Uyanik M, Eker I, Kilic A and Gunal A. The efficacy of platelet-rich plasma gel in MRSA-related surgical wound infection treat-ment: an experimental study in an animal model. Eur J Trauma Emerg Surg 2018; 44: 859-867.
[4] Turtiainen J, Saimanen EI, Partio TJ, Makinen KT, Reinikainen MT, Virkkunen JJ, Vuorio KS and Hakala T. Supplemental postoperative oxy-gen in the prevention of surgical wound infec-tion after lower limb vascular surgery: a ran-domized controlled trial. World J Surg 2011; 35: 1387-1395.
[5] Rizalar S and Topcu SY. The patient safety cul-ture perception of Turkish nurses who work in operating room and intensive care unit. Pak J Med Sci 2017; 33: 374-379.
[6] Jiang Y and Liu T. Effect of operating room care combined with home care for the postopera-tive rehabilitation and prognosis of gastric can-cer patients with low PTEN gene expression. Oncol Lett 2017; 14: 2119-2124.
[7] Mody L, Krein SL, Saint S, Min LC, Montoya A, Lansing B, McNamara SE, Symons K, Fisch J, Koo E, Rye RA, Galecki A, Kabeto MU, Fitzger-Table 3. Postoperative complications in the two groups of patients [n, (%)]
Project Test group n = 42 Control group n = 42 X2 P
Heat 2 (4.76) 3 (7.14) 0.213 0.645
Wound bleeding 1 (2.38) 4 (9.52) 1.914 0.167
Urinary retention 0 4 (9.52) 4.200 0.040
Lower extremity deep venous thrombosis 1 (2.38) 3 (7.14) 1.050 0.306
[image:6.612.90.524.88.165.2]Total incidence 4 (9.52) 14 (33.33) 7.071 0.008
Table 4. Comparison of quality of life between the two groups of patients after 1 month of nursing
Project Test group n = 42 Control group n = 42 t P Role function 80.31±2.22 65.34±2.12 31.61 <0.001 Emotional function 80.12±2.39 65.81±2.37 27.55 <0.001 Physical function 81.15±2.72 65.51±3.04 24.85 <0.001 Cognitive function 80.54±3.03 65.42±2.64 24.38 <0.001 Social function 80.33±2.91 66.02±2.85 22.77 <0.001
Address correspondence to: Dan Zhang, Operation Room, Jining No. 1 People’s Hospital, No. 6, Jiankang Road, Rencheng District, Jining 272011, Shandong, China. Tel: +86-0537-2253493; E-mail: hhl-399gn@163.com
References
[image:6.612.91.339.212.303.2]sur-ald JT, Olmsted RN, Kauffman CA and Bradley SF. A targeted infection prevention intervention in nursing home residents with indwelling de-vices: a randomized clinical trial. JAMA Intern Med 2015; 175: 714-723.
[8] Saunders H and Vehvilainen-Julkunen K. The state of readiness for evidence-based practice among nurses: an integrative review. Int J Nurs Stud 2016; 56: 128-140.
[9] Manning MW, Bean EW, Miller AC, Templer SJ, Mackenzie RS, Richardson DM, Bresnan KA and Greenberg MR. Using medical student quality improvement projects to promote evi-dence-based care in the emergency depart-ment. West J Emerg Med 2018; 19: 148-157. [10] Borgert M, Binnekade J, Paulus F, Goossens A
and Dongelmans D. A flowchart for building evidence-based care bundles in intensive care: based on a systematic review. Int J Qual Health Care 2017; 29: 163-175.
[11] Travers C, Graham F, Henderson A and Beattie E. CogChamps-a model of implementing evi-dence-based care in hospitals: study protocol. BMC Health Serv Res 2017; 17: 202.
[12] Yamada K, Abe H, Higashikawa A, Tonosu J, Kuniya T, Nakajima K, Fujii H, Niwa K, Shino-zaki T, Watanabe K, Sakae T and OkaShino-zaki H. Evidence-based care bundles for preventing surgical site infections in spinal instrumenta-tion surgery. Spine (Phila Pa 1976) 2018; 43: 1765-1773.
[13] Labarthe DR, Goldstein LB, Antman EM, Arnett DK, Fonarow GC, Alberts MJ, Hayman LL, Khera A, Sallis JF, Daniels SR, Sacco RL, Li S, Ku L, Lantz PM, Robinson JG, Creager MA, Van Horn L, Kris-Etherton P, Bhatnagar A and Whit-sel LP; American Heart Association Advocacy Coordinating Committee, Council on Hyperten-sion, Stroke Council, Council on Cardiovascu-lar and Stroke Nursing, Council on Clinical Cardiology, Council on Quality of Care and Out-comes Research, Council on Cardiovascular Surgery and Anesthesia, Council on Functional Genomics and Translational Biology, and Council on Epidemiology and Prevention. Evi-dence-based policy making: assessment of the American heart association’s strategic policy portfolio: a policy statement from the American heart association. Circulation 2016; 133: e615-e653.
[14] Ikaheimo TM, Jaakkola K, Jokelainen J, Sauk-koriipi A, Roivainen M, Juvonen R, Vainio O and Jaakkola JJ. A decrease in temperature and humidity precedes human rhinovirus infec-tions in a cold climate. Viruses 2016; 8. [15] Priano LL and Solanki D. Operating room
tem-perature. Anesth Analg 1981; 60: 226-227. [16] Li HJ, Huang L, Li TJ, Su J, Peng LR and Liu W.
Short-term outcomes of single-incision versus
conventional laparoscopic surgery for colorec-tal diseases: meta-analysis of randomized and prospective evidence. J Gastrointest Surg 2017; 21: 1931-1945.
[17] Zaslansky R, Eisenberg E, Peskin B, Sprecher E, Reis DN, Zinman C and Brill S. Early admin-istration of oral morphine to orthopedic pa-tients after surgery. J Opioid Manag 2006; 2: 88-92.
[18] Haroutounian S, Ratz Y, Ginosar Y, Furmanov K, Saifi F, Meidan R and Davidson E. The effect of medicinal cannabis on pain and quality-of-life outcomes in chronic pain: a prospective open-label study. Clin J Pain 2016; 32: 1036-1043.
[19] Eichhorn V, Henzler D and Murphy MF. Stan-dardizing care and monitoring for anesthesia or procedural sedation delivered outside the operating room. Curr Opin Anaesthesiol 2010; 23: 494-499.
[20] Archer T and Macario A. The drive for operating room efficiency will increase quality of patient care. Curr Opin Anaesthesiol 2006; 19: 171-176.
[21] Munyisia EN, Yu P and Hailey D. The impact of an electronic nursing documentation system on efficiency of documentation by caregivers in a residential aged care facility. J Clin Nurs 2012; 21: 2940-2948.
[22] Mittal C, Lee HCD, Goh KS, Lau CKA, Tay L, Siau C, Loh YH, Goh TKE, Sandi CL and Lee CE. ValuedCare program: a population health mod-el for the dmod-elivery of evidence-based care across care continuum for hip fracture pa-tients in Eastern Singapore. J Orthop Surg Res 2018; 13: 129.
[23] Trautner BW, Petersen NJ, Hysong SJ, Horwitz D, Kelly PA and Naik AD. Overtreatment of as-ymptomatic bacteriuria: identifying provider barriers to evidence-based care. Am J Infect Control 2014; 42: 653-658.
[24] Reilly J. Evidence-based surgical wound care on surgical wound infection. Br J Nurs 2002; 11: S4, S6, S8, S10, S12.
[25] Herstad L, Klungsoyr K, Skjaerven R, Tanbo T, Eidem I, Forsen L, Abyholm T and Vangen S. Maternal age and elective cesarean section in a low-risk population. Acta Obstet Gynecol Scand 2012; 91: 816-823.
[26] Baird LG, Banken R, Eichler HG, Kristensen FB, Lee DK, Lim JC, Lim R, Longson C, Pezalla E, Salmonson T, Samaha D, Tunis S, Woodcock J and Hirsch G. Accelerated access to innovative medicines for patients in need. Clin Pharmacol Ther 2014; 96: 559-571.
pa-tients receiving highly active antiretroviral ther-apy. Int J STD AIDS 2015; 26: 582-589. [28] Grypma L, Haverkamp R, Little S and Unutzer J.
Taking an evidence-based model of depres-sion care from research to practice: making lemonade out of depression. Gen Hosp Psy-chiatry 2006; 28: 101-107.
![Table 3. Postoperative complications in the two groups of patients [n, (%)]](https://thumb-us.123doks.com/thumbv2/123dok_us/288689.528374/6.612.91.339.212.303/table-postoperative-complications-groups-patients-n.webp)