STIs can be detrimental to both physical and psychological health and, without effective treatment, can result in serious complica-tions. Our Drug review describes the avail-able treatment options for the most
commonly encountered STIs, followed by sources of further information.
S
exually transmitted infections (STIs) are increas-ing in incidence and they constitute a major pub-lic health problem, not only in the UK but worldwide. A 2003 House of Commons Health Select Committeeinquiry into sexual health described a sexual health crisis in the UK that amounted to a public health emergency.1Effective management is imperative as STIs can be detrimental to both physical and psy-chological health, and can result in very costly com-plications.
The common STIs encountered in the general practice setting are Chlamydia trachomatis,Neisseria gon-orrhoeae, genital warts, genital herpes and Trichomonas vaginalis. The aim of this article is to summarise the drugs available to treat these infections, their effec-tiveness, principal side-effects and interactions, and their place in management.
Although the most common and important side-effects and interactions will be discussed, reference to the product literature and the BNFwill provide a more
Optimal management of
common STIs in general practice
Skyline
Imaging
Ltd
comprehensive list. Readers are also encouraged to read the British Association of Sexual Health and HIV guidelines for more detailed information (see Resources).
Drugs selected should have a high efficacy, low cost and acceptable toxicity and tolerance. Single-dose oral administration is preferred, and the treatment should not be contraindicated in pregnant or lactating women.2The tables outline the recommended treat-ment regimens.
It is beyond the remit of this article to discuss the treatment of syphilis and HIV infection.
Bacterial infections
Chlamydia trachomatis
One in ten sexually active young people aged between 16 to 24 years old have genital C. trachomatisinfection. Furthermore, results from the national Chlamydia screening programme demonstrate a high level of asymptomatic infection that would have other wise been missed, reinforcing the need for screening in community settings.3
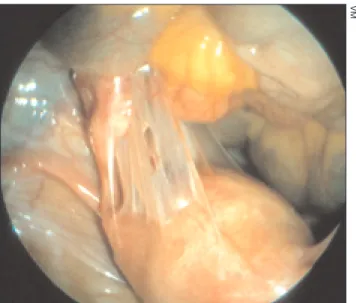
Women may develop pelvic inflammator y dis-ease (see Figure 1), which can lead to ectopic preg-nancy and infertility. In men, complications include urethritis and epididymitis. Chlamydia, like other acute bacterial and viral STIs, has also been associ-ated with an increased risk of HIV transmission and acquisition.4The consequences of these complica-tions represent a considerable health and economic burden.
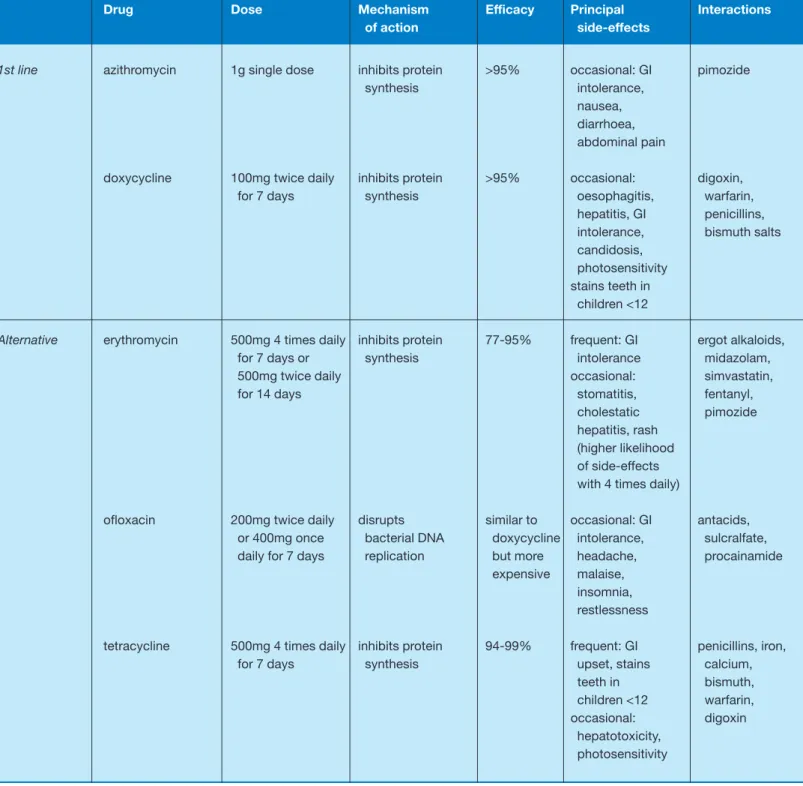
The antibiotics available to treat uncomplicated genital infection are summarised in Table 1. First-line therapy is usually with azithromycin or doxycycline. Contact tracing of sexual partners should be pursued, and patients should be advised to avoid sexual inter-course until they and their partner(s) have finished treatment.
PregnancyErythromycin is safe for use in pregnancy but less efficacious. A test of cure should therefore be performed three weeks after completion of therapy. Azithromycin may be taken in pregnancy but the man-ufacturers advise that it should only be used if there is no alternative.
Neisseria gonorrhoeae
Gonorrhoea (see Figure 2) is the second most com-mon bacterial STI in the UK. There are particularly higher rates in young people, men who have sex with men and black ethnic groups. Resistance to antibiotics complicates treatment of gonorrhoea: in 2007, 28 per cent of genitourinary medicine (GUM) clinic isolates were resistant to ciprofloxacin.3
The complications of gonorrhoea include epi-didymitis, involvement of the prostate gland, pelvic inflammatory disease and disseminated gonococcal infection.
Co-infection with C. trachomatisis common (up to 20 per cent of men and 40 per cent of women with gonorrhoea), and it is essential that screening for C. trachomatisis performed as a matter of routine.5
The sites of infection are the urethra, endocervix, pharynx, conjunctiva and rectum.
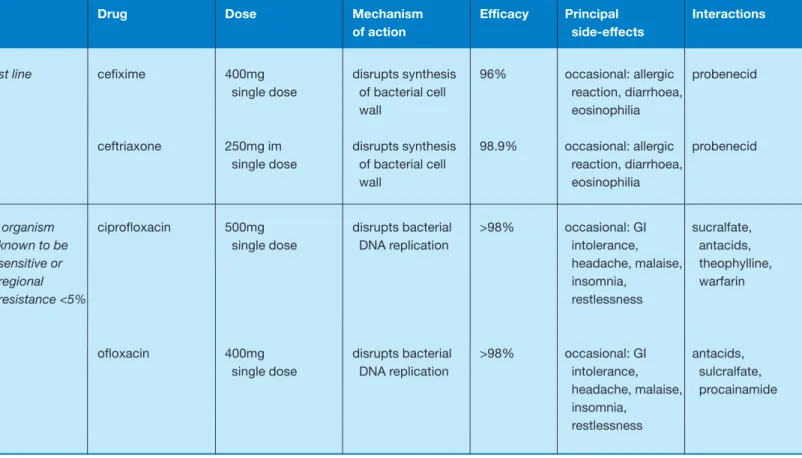
Table 2 summarises the main antibiotics used in the management of uncomplicated anogenital infec-tion. Cefixime (unlicensed indication) is a good first-line choice. Quinolones are generally not rec-ommended for use in children and growing adoles-cents as they may cause an arthropathy that affects weight-bearing joints.
Contact tracing of sexual partners should be pur-sued, and patients should be advised to avoid sexual intercourse until they and their partner(s) have fin-ished treatment.
PregnancyThe cephalosporins are safe for use in pregnancy.
Syphilis
There has been a marked increase in the number of cases of syphilis observed since the late 1990s. There were a total of 2680 cases of primary and secondary syphilis diagnosed in 2007 alone.3Rates of diagnosis were highest among men who have sex with men. Syphilis is caused by the spirochaete Treponema
www.prescriber.co.uk Prescriber 5 January 2009 17
Figure 1.Chlamydia trachomatisinfection in women can cause pelvic inflammatory disease. Azithromycin and doxycycline are first-line drug treatments in uncomplicated infection
VM
pallidum. It has a wide variety of presentations and may mimic many other diseases; clinical features of sec-ondary syphilis can be easily misdiagnosed as glandu-lar fever.
Diagnosis is based on history, clinical features and serological confirmation. Left untreated, it can lead to serious complications and even death. Suspect and
proven cases should always be referred for appropri-ate management.
Viral infections
Genital warts
Genital warts are caused by infection with human papilloma virus (HPV) and are the most prevalent
1st line azithromycin 1g single dose inhibits protein >95% occasional: GI pimozide
synthesis intolerance, nausea,
diarrhoea, abdominal pain
doxycycline 100mg twice daily inhibits protein >95% occasional: digoxin,
for 7 days synthesis oesophagitis, warfarin,
hepatitis, GI penicillins, intolerance, bismuth salts candidosis,
photosensitivity stains teeth in
children <12
Alternative erythromycin 500mg 4 times daily inhibits protein 77-95% frequent: GI ergot alkaloids,
for 7 days or synthesis intolerance midazolam,
500mg twice daily occasional: simvastatin,
for 14 days stomatitis, fentanyl,
cholestatic pimozide hepatitis, rash
(higher likelihood of side-effects with 4 times daily)
ofloxacin 200mg twice daily disrupts similar to occasional: GI antacids, or 400mg once bacterial DNA doxycycline intolerance, sulcralfate, daily for 7 days replication but more headache, procainamide
expensive malaise, insomnia, restlessness
tetracycline 500mg 4 times daily inhibits protein 94-99% frequent: GI penicillins, iron,
for 7 days synthesis upset, stains calcium,
teeth in bismuth,
children <12 warfarin, occasional: digoxin
hepatotoxicity, photosensitivity
Drug Dose Mechanism Efficacy Principal Interactions
of action side-effects
viral STI diagnosed in the UK. Infection may not be clinically apparent.
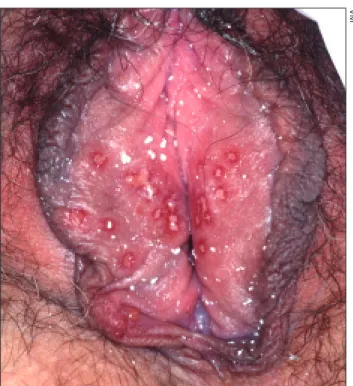
There are over 100 documented genotypes. Most anogenital warts are benign. However, there are cer-tain genotypes that are associated with an increased risk of anogenital neoplasia; specifically, genotypes 16 and 18 are associated with the greatest risk. However, most visible warts (see Figure 3) are due to types 6 and 11, which are the least likely to have neo-plastic potential.6
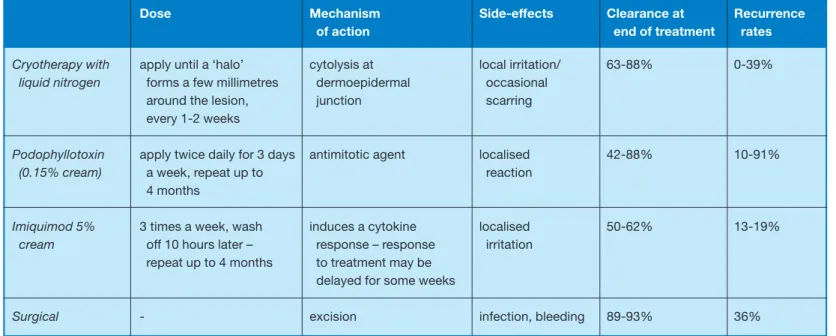
Treatment is usually for cosmetic rather than med-ical purposes. All treatments have significant failure and relapse rates,7and no single treatment is consid-ered to be better than another.
There are multiple treatments available; Table 3 illustrates some of the most commonly used. By stim-ulating the immune response, imiquimod (Aldara) may have a lower relapse rate. Podophyllotoxin can be used as a 0.15 per cent cream (Warticon Cream) or a 0.5 per cent solution. The solution is an option when treating warts that are easily visible and accessi-ble to the patient: in practice this means that it is more appropriate in males.
Other treatments available in specialist settings include curettage, trichloroacetic acid, laser therapy and electrosurgery. These too have significant failure and relapse rates.
Patients should be reviewed to assess progress. Different options may need to be tried if the patient is not tolerating the treatment or if there is a poor response.
PregnancyCryotherapy is safe for use in pregnancy; podophyllotoxin, however, is contraindicated.
22 Prescriber 5 January 2009 www.prescriber.co.uk Figure 2.Treatment of gonorrhoea is complicated by
resistance. First-line antibiotics include cefixime (unlicensed) and ceftriaxone
Genital herpes
Herpes simplex virus (HSV) types 1 and 2 can both cause genital herpes. Genital herpes is the common-est ulcerative STI in the UK and its prevalence is increasing. The presence of genital ulcers also increases the likelihood of HIV transmission.9
Disease episodes may be initial (primary) or recur-rent, and symptomatic or asymptomatic. Primary gen-ital herpes (see Figure 4) can be ver y painful and distressing. Most clinicians would make a clinical diag-nosis and prescribe treatment after taking swabs for HSV; full STI screening is important but is usually deferred until lesions have healed.
General advice includes saline bathing, analgesia and lidocaine gel. Oral antiviral drugs reduce the severity and duration of the episode,10,11and are indi-cated within five days of the start of the episode and while new lesions are still forming. Topical agents are not as effective as oral.
The three antiviral drugs all have similar efficacy but differ in cost. It is the authors’ preference to use valaciclovir (Valtrex) for primary genital herpes as it achieves a high plasma drug concentration more rapidly, and aciclovir for recurrent infection.
Treatment of recurrent genital herpes could be episodic or suppressive. Episodic treatment should
ideally be patient initiated. Patients experiencing more than six episodes a year may be considered for suppressive treatment with aciclovir 400mg twice daily, usually for a maximum of one year.
Referral to a GUM clinic is recommended for man-agement during pregnancy and for those considering suppression therapy. Table 4 summarises the main options.
Human immunodeficiency virus
The prevalence of HIV infection is increasing. In 2006 there were an estimated 73 000 people living with HIV infection in the UK, about a third of whom were unaware of their infection.3Transmission rates in men who have sex with men remain high but het-erosexual transmission is rising. Hethet-erosexual acqui-sition now predominates among diagnosed cases worldwide.
HIV is a multisystem disorder. However, many peo-ple with early infection are essentially asymptomatic and unaware of their infection. Treatment involves complex antiretroviral regimens aimed at viral sup-pression.
The prognosis has improved dramatically since the advent of highly active antiretroviral therapy (HAART).
1st line cefixime 400mg disrupts synthesis 96% occasional: allergic probenecid
single dose of bacterial cell reaction, diarrhoea,
wall eosinophilia
ceftriaxone 250mg im disrupts synthesis 98.9% occasional: allergic probenecid single dose of bacterial cell reaction, diarrhoea,
wall eosinophilia
If organism ciprofloxacin 500mg disrupts bacterial >98% occasional: GI sucralfate,
known to be single dose DNA replication intolerance, antacids,
sensitive or headache, malaise, theophylline,
regional insomnia, warfarin
resistance <5% restlessness
ofloxacin 400mg disrupts bacterial >98% occasional: GI antacids,
single dose DNA replication intolerance, sulcralfate,
headache, malaise, procainamide insomnia,
restlessness
Drug Dose Mechanism Efficacy Principal Interactions
of action side-effects
24 Prescriber 5 January 2009 www.prescriber.co.uk Protozoal infection
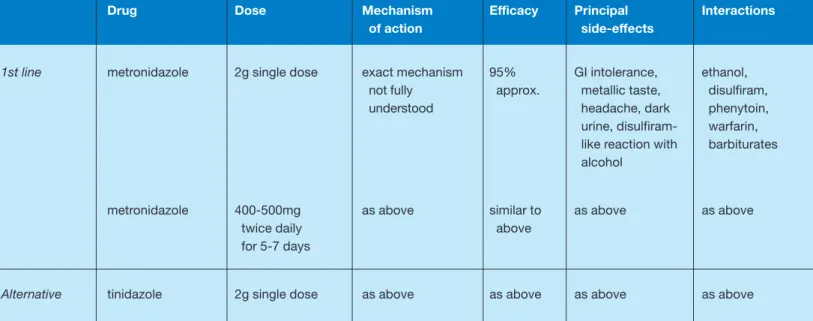
Trichomonas vaginalis
T. vaginalis(TV) is a flagellate protozoan and is one of the commonest STIs worldwide. The only preva-lence study in the UK within the last 10 years detected a prevalence of 0.1 per cent among women requesting cer vical smears;12 however, there is a high false-positive rate of trichomoniasis detected on cervical cytology. The prevalence in GUM clin-ics is much higher. TV is associated with premature labour, low birth weight, prostatitis and HIV trans-mission.12
Metronidazole is the drug of choice (see Table 5). A single dose has the advantage of improved compli-ance and being cheaper, although there is some
evi-dence to suggest that the failure rate is higher, though not significantly, especially if the partners are not treated concurrently.13
There are various drugs that have been adminis-tered in the form of topical preparations but these are largely ineffective; eradication requires systemic treat-ment. Patients should be advised to avoid sexual inter-course until they and their partner(s) have finished treatment. Partners should have a full STI screen and be treated for trichomoniasis irrespective of the results of investigations.
In the event of persistent treatment failure with metronidazole, there are other treatments avail-able such as tinidazole (Fasigyn). Refer ral is advised.
PregnancyCourse of metronidazole for one week; the manufacturers advise that single high-dose metronidazole should be avoided in pregnancy. Conclusion
The involvement of primary-care physicians in the diagnosis and management of STIs is encouraged within the National Sexual Health and HIV strategy.14 It should be emphasised that optimal management of any diagnosed STIs should include screening for other STIs, partner notification and follow-up where appro-priate. Patients should be given a detailed explana-tion of their condiexplana-tion with particular emphasis on the long-term health implications for themselves and their partners.
Early diagnosis and treatment of STIs not only alleviates symptoms and reduces complications, but
Cryotherapy with apply until a ‘halo’ cytolysis at local irritation/ 63-88% 0-39%
liquid nitrogen forms a few millimetres dermoepidermal occasional
around the lesion, junction scarring
every 1-2 weeks
Podophyllotoxin apply twice daily for 3 days antimitotic agent localised 42-88% 10-91%
(0.15% cream) a week, repeat up to reaction
4 months
Imiquimod 5% 3 times a week, wash induces a cytokine localised 50-62% 13-19%
cream off 10 hours later – response – response irritation
repeat up to 4 months to treatment may be delayed for some weeks
Surgical - excision infection, bleeding 89-93% 36%
Dose Mechanism Side-effects Clearance at Recurrence
of action end of treatment rates
Table 3.Summary of the treatments used in genital warts
Figure 3.A variety of treatments are available for genital warts; imiquimod has a lower recurrence rate
also reduces the period of infectivity and onward transmission.
References
1. House of Commons Health Committee. Sexual health. Third report of session 2002-3, vol. 1.
2. World Health Organization.Reproductive tract infections and sexually transmitted infections including HIV/AIDS. Factsheet. www.who.int/reproductive-health/stis/index.htm.
3. Health Protection Agency (HPA) data, www.hpa.org.uk. 4. Fleming DT, Wasserheit JN. From epidemiological syn-ergy to public health policy and practice: the contribution of other sexually transmitted diseases to the sexual trans-mission of HIV infection. Sex Transm Infect1999;75:3-17. 5. Centers for Disease Control and Prevention. Sexually trans-mitted disease treatment guidelines 2002. MMWR 2002;51(No. RR-6):36-42.
6. Kazzi A, Ghadishah D. Genital warts. www.emedicine. com/emerg/topic640.htm.
7. Beutner KR, Wiley DJ. Recurrent external genital warts: a literature review. Papilloma Virus Rep1997;8:69-74. 8. Department of Health. Immunisation against infectious dis-ease - the Green Book. www.dh.gov.uk/greenbook. 2006. 9. Keet IPM, Lee FK, Van Griensven GJP,et al. Herpes simplex virus type 2 and other genital ulcerative infections as a risk factor for HIV-1 acquisition. Genitourin Med1990; 66:330-3. 10. Corey L, Benedetti J, Critchlow C, et al. Treatment of pri-mary first-episode genital herpes virus infections with aci-clovir: results of topical, intravenous and oral therapy.J Antimicrob Chemother1983;12(Suppl B):79-88.
11. Fife KH, Barbarash RA, Rudolph T, et al. Valaciclovir ver-sus aciclovir in the treatment of first-episode genital herpes
infection. Results of an international, multicentre, double-blind randomised clinical trial. The Valaciclovir International Herpes Simplex Virus Study Group. Sex Transm Dis1997;24:481-6.
12. Bowden FJ, Garnett GP. Trichomonas vaginalis epi-demiology: parameterising and analysing a model of treat-ment interventions. Sex Transm Infect2000;76:248-56.
1st line aciclovir 200mg 5 times a converted by viral significant usually none probenecid,
day for 5 days or thymidine kinase reduction in occasional: rash, theophylline 400mg 3 times and cellular duration of nausea, diarrhoea,
daily for 3-5 days catalase into active lesions and renal and hepatic form – inhibits viral viral dysfunction DNA polymerase shedding
1st line famciclovir 250mg 3 times converted into as above usually none probenecid
daily for 5 days penciclovir, then occasional:
active form – headache,
inhibits viral DNA dizziness,
polymerase nausea,
diarrhoea
1st line valaciclovir 500mg twice daily cleaved into as above as for famciclovir probenecid
for 5 days aciclovir
Drug Dose Mechanism Efficacy Principal Interactions
of action side-effects
Table 4.Summary of the drugs used to treat genital herpes
Figure 4.Oral antiviral drugs are recommended for primary and recurrent genital herpes infection
26 Prescriber 5 January 2009 www.prescriber.co.uk
13. Hager WD, Brown ST, Kraus SJ. Metronidazole for vagi-nal trichomoniasis. Seven-day vs single-dose regimens. JAMA
1980;244(11):1219-20.
14. Sexual health and HIV strategy. Department of Health, June 2001.
Dr Gupta is a specialist registrar in the Department of Genitourinary Medicine, and Professor Kinghorn is clini-cal director for communicable diseases and honorary pro-fessor in genitourinary medicine, Royal Hallamshire Hospital, Sheffield
1st line metronidazole 2g single dose exact mechanism 95% GI intolerance, ethanol,
not fully approx. metallic taste, disulfiram,
understood headache, dark phenytoin,
urine, disulfiram- warfarin, like reaction with barbiturates alcohol
metronidazole 400-500mg as above similar to as above as above
twice daily above
for 5-7 days
Alternative tinidazole 2g single dose as above as above as above as above
Drug Dose Mechanism Efficacy Principal Interactions
of action side-effects
Table 5.Summary of the drugs used to treat trichomoniasis
Resources
Associations
The British Association for Sexual Health and HIV (BASHH), RSM, 1 Wimpole Street, London W1G 0AE. Tel: 020 7290 2968, email: bashh@rsm.ac.uk, website: www.bashh.org.
The Royal College of Obstetricians and Gynaecologists (RCOG), 27 Sussex Place, Regent’s Park, London NW1 4RG. Tel: 020 7772 6200, website: www.rcog.org.uk.
Guidelines
Chlamydia – uncomplicated, genital (women) – manage-ment.NHS Clinical Knowledge Summaries. http:// cks.librar y.nhs.uk/chlamydia_uncomplicated_ genital.
Herpes simplex – genital – management.NHS Clinical Knowledge Summaries. http://cks.library.nhs.uk/ herpes_simplex_genital.
Management of genital herpes in pregnancy.RCOG, 2007. www.rcog.org.uk.
National guideline on the management of anogenital warts. BASHH, 2007. www.bashh.org/documents/86/86.pdf.
National guideline for the management of genital tract infec-tion with Chlamydia trachomatis. BASHH, 2006. www.bashh.org/documents/61/61.pdf.
National guideline for the management of genital herpes. BASHH, 2007. www.bashh.org/documents/115/115.pdf. National guideline on the diagnosis and treatment of gonorrhoea in adults.BASHH, 2005. www.bashh.org/ documents/116/116.pdf.
National guideline on the management of Trichomonas vaginalis. BASHH, 2007. www.bashh.org/documents/87/87.pdf Sexually transmitted infections in primary care. BASHH and RCGP, 2006. www.bashh.org/documents/702/702.pdf.
Patient support
The Family Planning Association. The fpa provides a national service in the UK providing information, training, research and publications. www.fpa.org.uk.
Further reading
ABC of sexually transmitted infections.Adler M. London: BMJ Press, 2004.