Low Back Pain: Epidemiology of Consultations
ANNA JO
¨ UD,
1INGEMAR F. PETERSSON,
1ANDMARTIN ENGLUND
2Objective. Low back pain (LBP) affects most people at some stage in life. However, the burden on the health care system is unclear. We studied: 1) the 1-year consultation prevalence, 2) the rate of first-time consultation for LBP and the relationship of the frequency to other musculoskeletal conditions, and 3) the health care utilization of patients with LBP compared to the general population.
Methods. Using the health care register in Southern Sweden (population 1.2 million), including diagnoses (International Statistical Classification of Diseases and Related Health Problems, Tenth Revision) by physicians, we identified all patients who in 2009 were diagnosed with LBP, defined as lumbago with sciatica, low back pain, or other/unspecified dorsalgia. We defined first-time consultation as a consultation in 2009 without a record of an LBP diagnosis in 2004 –2008. Standardized health care utilization ratios were calculated for LBP patients compared to the general population seeking care.
Results. The 1-year consultation prevalence of LBP in the population was 3.8% (4.3% for women, 3.3% for men) and increased with age. LBP had been recorded in 17.1% of all patients (16.5% for women, 18.0% for men) who had been diagnosed with any musculoskeletal condition. The rate of first-time consultation was 238 per 10,000 adults (265 for women, 209 for men). The health care utilization ratios in female and male patients with LBP were 1.74 (95% confidence interval [95% CI] 1.73–1.75) and 1.81 (95% CI 1.80 –1.82), respectively.
Conclusion. LBP, diagnosed in every sixth patient who consulted due to a musculoskeletal problem, is a public health concern that needs structured management. Patients with LBP consume close to twice as much health care as the general population and this warrants more awareness.
Introduction
Low back pain (LBP) is one of the most frequent symptoms in adults within the western world. However, estimates of the occurrence based on subjects’ self-report differ drasti-cally, with a prevalence for a 1-year period between 2% and 65%, depending on the definitions and other meth-odologic aspects (1–3). Studies have indicated that ap-proximately 40 –70% of those experiencing back pain seek health care for their back pain at some stage in life (4,5), often due to more severe pain (4 – 6). This may result in a greater cost to society, which is why this is an important
group to study. The objectives of this study were to inves-tigate 1) the 1-year consultation prevalence, 2) the rate of first-time consultation for LBP and the relationship of the frequency to other musculoskeletal conditions, and 3) the health care utilization of patients with LBP compared to the general population. The consultation prevalence and first-time consultation rate are standardized to the 2000 US standard population.
Materials and Methods
Skåne Health Care Register (SHCR). In Sweden, the responsibility for providing health care is decentralized to the county councils. Both public and private health care providers have the same tax-based financing system and apart from a small co-pay, the residents are entitled to free health care. By law, and to be eligible for free health care, a 10-digit personal identification number, a unique num-ber automatically assigned to the population, is recorded. Within the county of Skåne, the southernmost part of Sweden with a population of 1.2 million inhabitants (representing one-eighth of the total Swedish population), all types of both inpatient and outpatient services are offered for the entire population. Each health care consul-tation generates data entries that transfer to central data-bases, such as the SHCR, and these constitute the basis for reimbursement. Similar regulations apply to both public
Supported by grants from the regional health service au-thorities in Skåne County (Region Skåne), the Swedish So-cial Insurance Agency, the Swedish Research Council, and the Faculty of Medicine, Lund University, Lund, Sweden.
1
Anna Jo¨ud, MPH, Ingemar F. Petersson, MD, PhD: Lund University and WHO Collaborating Centre for Evidence-Based Healthcare in Musculoskeletal Disorders, Lund, Sweden;2Martin Englund, MD, PhD: Lund University and
WHO Collaborating Centre for Evidence-Based Healthcare in Musculoskeletal Disorders, Lund, Sweden, and Boston University School of Medicine, Boston, Massachusetts.
Address correspondence to Anna Jo¨ud, MPH, Department of Orthopedics, Klinikgatan 22, Skåne University Hospital, SE 221 85 Lund, Sweden. E-mail: anna.joud@med.lu.se.
Submitted for publication September 9, 2011; accepted in revised form February 8, 2012.
DOI 10.1002/acr.21642
© 2012, American College of Rheumatology
BRIEF REPORT
and private alternatives, with the only difference that di-agnostic codes in private care are not transferred automat-ically. The register data are continuously and prospec-tively ascertained, and there is very limited selection bias with respect to social class or income.
Diagnoses are those made since 1998, classified accord-ing to the Swedish translation of the International Statis-tical Classification of Diseases and Related Health Prob-lems, Tenth Revision (ICD-10) system, available online (www.who.int/classifications/icd/en/).
Swedish population register. In Sweden, everyone can seek health care wherever they want to. For this study we were only interested in identifying patients residing in Skåne County. Therefore, SHCR data were linked by per-sonal identification numbers with the Swedish population register. The register is the civil registration of vital events (e.g., births, deaths, marriages, change of residential ad-dress), administered by the Swedish Tax Agency.
Criteria for LBP. We defined LBP as a diagnostic code (ICD-10) in the SHCR for any of the following diagnoses: lumbago with sciatica (M54.4), low back pain (M54.5), other dorsalgia (M54.8), dorsalgia unspecified (M54.9), and an ICD-10 code referred to as dorsalgia not specified (M54.9P), specifically used by general practitioners. These diagnoses were agreed upon after discussions with general practitioners and specialists working in the clinical field. Patients agesⱖ20 years diagnosed by a physician in 2009 were included.
Statistical analysis. Annual consultation prevalence. Diagnostic codes from private health care providers are not forwarded to the SHCR, although other data are, e.g., the personal identification number, date of visit, and informa-tion on the health care provider. In 2009, 28% of a total 3,823,535 outpatient doctor consultations were within pri-vate care and we needed to compensate for this loss in the calculation of period prevalence and the rate of first-time consultation. Therefore, to compensate for the individuals only seeking private care for their LPB (not captured with diagnosis in the SHCR), we reduced the denominator by 30%.
Rate of first-time consultation for LBP. For consultation rates, we were interested in subjects with first- or
new-onset symptoms of LBP, rendering their first consultation. We identified adults with an LBP diagnosis in 2009 that did not have a previous consultation record with a physi-cian due to LBP in the prior 5 calendar years (2004 –2008). Health care contacts. Health care contacts in this study are considered visits to any health care professional, in-cluding physicians, nurses, physiotherapists, etc. (exclud-ing practitioners of alternative or integrative medicine).
A standardized health care utilization ratio was calcu-lated by dividing the observed number of health care
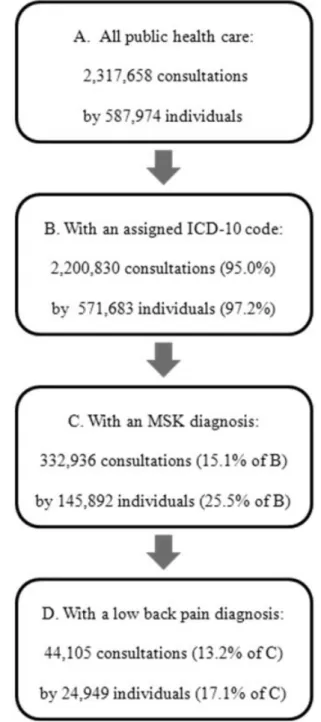
con-Figure 1. Flow chart detailing the number (percentage) of doctor consultations and patients within public care in 2009 in Skåne County, Sweden (with a total population of 1.2 million). ICD-10⫽ International Statistical Classification of Diseases and Related Health Problems, Tenth Revision; MSK ⫽ musculoskeletal or connective tissue (ICD-10, chapter XIII).
Significance & Innovations
● Epidemiologic findings from Swedish health care registries reveal the burden on the health care sys-tem from people diagnosed with low back pain.
● People diagnosed with low back pain consume twice as much health care as the general popula-tion.
● Common other diagnoses among patients with low back pain were depression, respiratory infections, and chronic obstructive pulmonary disease.
tacts in 2009 by the expected number based on data from the general population, stratified by age and sex. This ratio describes the burden on the health care system by the patients with LBP in relation to persons in general. Since the patients with LBP had had at least 1 consultation with a physician (in order to be included in the LBP cohort), we reduced the number of observed contacts in 2009 for LBP patients by 1 per subject.
We also calculated a standardized morbidity prevalence ratio (SMR). The SMR was calculated by dividing the observed prevalence of other common diagnostic codes in the LBP cohort by the expected prevalence based on data from the general population seeking care, standardized for age and sex. The SMR was calculated for the 20 most common diagnoses among the patients with LBP.
In addition to the methodology described above, we also present consultation prevalence and first-time consulta-tion rates standardized to the 2000 US standard popula-tion with 95% confidence intervals (95% CIs). Statistical analyses were performed using SAS software, version 9.2. The study was approved by the Institutional Review Board of Lund University.
Results
Annual consultation prevalence for LBP patients. In 2009, 24,949 individuals (57.3% women) agesⱖ20 years were diagnosed with LBP. The mean⫾SD age was 55.3⫾ 18.3 years. The 1-year consultation prevalence of LBP in the adult population was 3.8% (4.3% for women and 3.3% for men). Standardized to the 2000 US standard popula-tion, the figure was 3.57% (95% CI 3.52–3.61), for women
Figure 2. A,Rate of first-time doctor consultations due to low back pain (LBP) in 2009 (first time defined as the number of unique individuals without consultation with a physician for LBP between 2004 and 2008; n⫽15,601).B,Standardized health care utilization ratios for patients with LBP (n⫽24,949) compared to the general population (n⫽938,397) in 2009 in Skåne County, Sweden. A value of 1 indicates no difference.
Table 1. SMRs for the 20 most common other diagnostic codes (listed in decreasing order) among patients with low back pain compared to the general population*
Diagnosis (ICD-10 code)
Women, SMR (99% CI)
Men, SMR (99% CI)
Essential (primary) hypertension (I10) 0.91 (0.86–0.96) 0.87 (0.81–0.93) Other soft tissue disorder (M79) 1.91 (1.80–2.02) 1.83 (1.68–1.98) Abdominal and pelvic pain (R10) 1.71 (1.60–1.83) 1.50 (1.35–1.65) Acute upper respiratory infection of multiple sites (J06) 1.23 (1.14–1.33) 1.07 (0.95–1.19) Cystitis (N30) 1.34 (1.25–1.44) 1.16 (0.95–1.40) Depressive episode (F32) 1.29 (1.18–1.40) 1.33 (1.17–1.51) Pain not elsewhere classified (R52) 2.36 (2.15–2.57) 2.37 (2.10–2.66) Type 2 diabetes mellitus (E11) 0.99 (0.89–1.10) 1.01 (0.91–1.12) Other joint disorders, not elsewhere classified (M25) 1.47 (1.34–1.61) 1.36 (1.20–1.54) Other intervertebral disc disorders (M51) 8.93 (8.00–9.92) 8.71 (7.78–9.69) Pain in throat and chest (R07) 1.48 (1.33–1.64) 1.40 (1.24–1.57) Other anxiety disorders (F41) 1.38 (1.25–1.52) 1.26 (1.08–1.45) Chronic ischemic heart disease (I25) 1.04 (0.91–1.18) 1.04 (0.93–1.16) Atrial fibrillation and flutter (I48) 0.93 (0.81–1.05) 0.94 (0.83–1.06) Disorders of glycoprotein metabolism (E78) 0.88 (0.78–1.00) 0.79 (0.69–0.90) Senile cataract (H25) 0.98 (0.88–1.10) 0.97 (0.83–1.12) Dizziness and giddiness (R42) 1.31 (1.17–1.47) 1.26 (1.07–1.47) Other spondylopathies (M48) 5.01 (4.43–5.63) 6.20 (5.34–7.13) Unspecified acute lower respiratory infection (J22) 1.23 (1.09–1.38) 1.19 (1.02–1.39) Other chronic obstructive pulmonary disease (J44) 1.33 (1.17–1.50) 1.19 (1.01–1.39) * SMR⫽standardized morbidity prevalence ratio; ICD-10⫽International Statistical Classification of Diseases and Related Health Problems, Tenth Revision; 99% CI⫽99% confidence interval.
was 3.94% (95% CI 3.87– 4.01), and for men was 3.18% (95% CI 3.12–3.24). For every 10,000 adults consulting a physician in 2009, 436 were diagnosed with LBP, 446 per 10,000 women and 424 per 10,000 men.
LBP accounted for 13.2% of all consultations with a musculoskeletal or connective tissue (MSK) diagnosis, and of all patients with an MSK diagnosis, 17.1% had received an LBP diagnosis (Figure 1).
Rate of first-time consultation. A total of 15,601 indi-viduals were identified as having their first-time consul-tation for LBP in 2009 (56.9% women). The mean⫾ SD age at diagnosis was 54.6⫾18.8 years (55.4⫾19.3 years for women and 53.6 ⫾ 18.1 years for men). The 2009 first-time consultation rate was 238 per 10,000 adults, 265 for women and 209 for men (Figure 2A). Adjusted to the 2000 US standard population, the figures were 219 per 10,000 persons (95% CI 189 –5,249), 242 per 10,000 women (95% CI 196 –287), and 196 per 10,000 men (95% CI 156 –236).
Health care contacts by LBP patients. In 2009, 45.9% of all contacts by patients with LBP were to a physician, 27.9% were to a physiotherapist, 16.2% were to a nurse, 2.4% were to a psychologist, and the remaining contacts (7.5%) were to other health care providers such as audiol-ogists (1%), chiropractors (0.6%), and others. Of all con-tacts by patients with LBP, 77% were in public care. The proportions were essentially the same among both women and men.
The health care utilization ratio was 1.74 (95% CI 1.73– 1.75) for women and 1.81 (95% CI 1.80 –1.82) for men, i.e., both female and male LBP patients had almost twice as many consultations as women and men in the general population seeking care standardized for age. The ratios declined by increasing age, reaching a ratio closer to 1 in the oldest men and women (Figure 2B). When studying physician contacts, only the physician health care utiliza-tion ratio was 1.50 (95% CI 1.50 –1.51).
The most frequent diagnostic code among the patients with LBP was hypertension (as in the general population). Apart from different pain diagnoses, depressive episodes, anxiety disorders, and dizziness were more frequent in patients with LBP. Also, respiratory tract infections and chronic obstructive pulmonary disease were more fre-quent (Table 1).
Discussion
The 2009 consultation prevalence of LBP in Southern Sweden was 3.8% of the adult population. For every 10,000 persons consulting a physician, 436 were diag-nosed with LBP. Among all patients consulting with an MSK diagnosis (ICD-10, chapter XIII), 17.1% had been diagnosed with LBP in the same calendar year. First-time consultation for LBP was more frequent among women than men and also more frequent with increasing age.
In previous reports, more than 30% of the population has been reported to experience varying degrees of self-reported LBP (2,7,8). However, the pain does not neces-sarily lead to consultation. Studies on consultation pat-terns suggest that people with more severe pain seek
health care more frequently than others (4 – 6). Recent re-search on LBP suggests that elderly persons experience more severe pain (9,10). Our finding that the older popu-lation is overrepresented, both in consultation prevalence and rate of first consultation, corroborates these findings and warrants concern in a steadily aging population. It is plausible that many of these LBP diagnoses reflect pain from more specific conditions such as osteoporosis-related vertebral fractures and spinal stenosis.
Few studies on LBP consultations or equivalent mea-sures of occurrence have been published. However, our rate of first-time consultations (254 per 10,000 women and 200 per 10,000 men) were lower than figures on new episodes of LBP, i.e., 500 and 300 per 10,000 women and men, respectively, reported from the UK (11). An explana-tion could be the fact that the former study used a wider definition of LBP. In a more recent study on consultation rate, defined as the number of patients with an LBP con-sultation of all individuals who consult, Bartholomeeusen et al reported annual consultation estimates of 530 and 499 per 10,000 women and men, respectively (12). These fig-ures are close to ours (446 and 424 per 10,000 women and men, respectively).
As could be expected, we found that patients consulting with LBP consumed substantially more health care than the general population. The total excess health care utili-zation was approximately 2-fold for both women and men. The patients with LBP who consumed the most health care in relative measures were younger patients; the average male LBP patient age 20 –34 years had 2.8 times as many health care contacts compared to the general population in this age category. For both women and men, the health care utilization ratios approached 1 with increasing age, i.e., neither increased nor decreased health care consump-tion for the oldest patients with LBP, suggesting that other symptoms may become more prevalent and concerning with older age in general.
The most notable other common diagnostic code re-corded for the patients with LBP included, as expected, specific back pain diagnoses such as intervertebral disc disorders. However, we also noted more frequent diagnos-tic codes for more generalized pain, e.g., from soft tissues and other sites. Previous data have shown that regional pain such as LBP is a future risk factor for developing generalized pain (13). Further, in accordance with previ-ous studies, we found depression, anxiety, upper and lower respiratory infections (upper only in women), and chronic obstructive pulmonary disease to be more fre-quently diagnosed in patients with LBP (12,14,15).
The strength of our study is the large population-based data set encompassing prospectively collected data on all consultations in all levels of health care within a well-defined geographic area. However, there are also several important limitations to acknowledge. First, our case cri-terion, i.e., at least 1 of a selected set of ICD-10 diagnoses, means that the individual has to be diagnosed with LBP. The terminology and diagnostic criteria may vary. We chose to only include 5 ICD-10 codes (M54.4 [lumbago with sciatica], M54.5 [low back pain], M54.8 [other dors-algia], and M54.9 and M54.9P [dorsalgia unspecified]). Different doctors and different clinics may use different
diagnostic codes for the same symptoms and diseases. It is also possible that subjects with LBP receive a myalgia diagnosis, in particular if the LBP is linked to musculo-skeletal pain elsewhere. This would result in an under-estimation of the burden of LBP on the health care system. Second, only diagnoses set by physicians are re-corded. Therefore, patients with LBP who have consulted a physiotherapist without consulting a physician are not captured. The proportion of patients only consulting phys-iotherapists varies locally. Third, although the SHCR in-cludes information on all patients who have used health care, both inpatient and outpatient, the diagnostic codes connected to doctor consultations within private care are not forwarded to the SHCR. However, we have compen-sated for this in order to not substantially underestimate the consultation prevalence and consultation rate.
The present detailed data on consultation patterns war-rant concern in an aging population and could also benefit from benchmarking studies between different countries and systems. A larger proportion of women than men consult, and the increase in consultation prevalence with age suggests that structured management plans are highly needed in the daily clinical setting to distinguish potential chronic inflammatory diseases, malignancies, or other se-rious diseases from the more common and benign condi-tions.
AUTHOR CONTRIBUTIONS
All authors were involved in drafting the article or revising it critically for important intellectual content, and all authors ap-proved the final version to be published. Ms Jo¨ud had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Study conception and design.Jo¨ud, Petersson, Englund.
Acquisition of data.Jo¨ud, Petersson.
Analysis and interpretation of data.Jo¨ud, Englund.
REFERENCES
1. Freburger JK, Holmes GM, Agans RP, Jackman AM, Darter JD, Wallace AS, et al. The rising prevalence of chronic low back pain. Arch Intern Med 2009;169:251– 8.
2. Hoy D, Brooks P, Blyth F, Buchbinder R. The epidemiology of low back pain. Best Pract Res Clin Rheumatol 2010;24: 769 – 81.
3. Rossignol M, Rozenberg S, Leclerc A. Epidemiology of low back pain: what’s new? Joint Bone Spine 2009;76:608 –13. 4. Carey TS, Evans A, Hadler N, Kalsbeek W, McLaughlin C,
Fryer J. Care-seeking among individuals with chronic low back pain. Spine 1995;20:312–7.
5. Carey TS, Evans AT, Hadler NM, Lieberman G, Kalsbeek WD, Jackman AM, et al. Acute severe low back pain: a population-based study of prevalence and care-seeking. Spine 1996;21: 339 – 44.
6. Cote P, Cassidy JD, Carroll L. The treatment of neck and low back pain: who seeks care? Who goes where? Med Care 2001; 39:956 – 67.
7. Loney PL, Stratford PW. The prevalence of low back pain in adults: a methodological review of the literature. Phys Ther 1999;79:384 –96.
8. Walker BF. The prevalence of low back pain: a systematic review of the literature from 1966 to 1998. J Spinal Disord 2000;13:205–17.
9. Baek SR, Lim JY, Park JH, Lee JJ, Lee SB, Kim KW, et al. Prevalence of musculoskeletal pain in an elderly Korean population: results from the Korean Longitudinal Study on Health and Aging (KLoSHA). Arch Gerontol Geriatr 2010;51: e46 –51.
10. Dionne CE, Dunn KM, Croft PR. Does back pain prevalence really decrease with increasing age? A systematic review. Age Ageing 2006;35:229 –34.
11. Jordan K, Kadam U, Hayward R, Porcheret M, Young C, Croft P. Annual consultation prevalence of regional musculo-skeletal problems in primary care: an observational study. BMC Musculoskelet Disord 2010;11:144.
12. Bartholomeeusen S, Van Zundert J, Truyers C, Buntinx F, Paulus D. Higher incidence of common diagnoses in patients with low back pain in primary care. Pain Pract 2012;12:1– 6. 13. Bergman S, Herrstrom P, Jacobsson LT, Petersson IF. Chronic widespread pain: a three year followup of pain distribution and risk factors. J Rheumatol 2002;29:818 –25.
14. Reme SE, Tangen T, Moe T, Eriksen HR. Prevalence of psy-chiatric disorders in sick listed chronic low back pain pa-tients. Eur J Pain 2011;15:1075– 80.
15. Ritzwoller DP, Crounse L, Shetterly S, Rublee D. The associ-ation of comorbidities, utilizassoci-ation and costs for patients iden-tified with low back pain. BMC Musculoskelet Disord 2006; 7:72.