Improving the Quality of Health Care Systems based on IT Applications
Full text
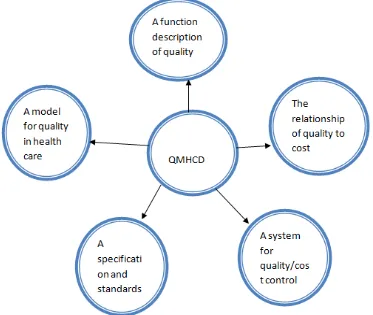
Figure
Related documents
Through both theoretical analysis and empirical analysis ,this paper evaluated and compared the competitiveness of eleven major (or potential) offshore RMB markets, and predict
Equations (13) through (15) represent the effect of changes in trade restrictions (either through a tariff, transport cost, or foreign beachhead cost) on the cutoff firm serving
In Virginia, there are also statutory and practical differences between custody cases heard in Circuit Court (matrimonial ac- tions) versus in Juvenile and
Specific objectives include: (1) to develop a conceptual model of transaction cost theory that explains the outsource decision by rural hospital administrators when
A) Launching our citizens initiative is/was a way of... Strongly Agree Agree Neither Agree nor Disagree Disagree Strongly Disagree.. ...influencing the content and
In a one-sided market, switching costs may intensify or soften first-period price competition depending upon how patient consumers are relative to platforms; but in a two-sided
7 Shrinkage and expansion of the absolute change in peat height (in cm compared to initial peat levels) measured in the field between August 2014 and December 2015 under
Ordinance of municipal adult education (2002:1012) Swedish Statute Book Department/authority: Ministry of Education and Research. www.sweden.gov.se