Int J Clin Exp Med 2017;10(8):11710-11716 www.ijcem.com /ISSN:1940-5901/IJCEM0053132
Original Article
CT and MRI imaging characteristics of unexpected
splenic autotransplantation after splenectomy
Zhihao Ren1, Qianjiang Ding1, Jianhua Wang1, Can Tu1, Siqi Wang1, Chao Cheng2, Changjing Zuo2
1Department of Radiology, The Affiliated Hospital of Medical College of Ningbo University, Ningbo, China; 2 Depart-ment of Nuclear Medicine, Changhai Hospital, the Second Military Medical University, Shanghai, China
Received March 17, 2017; Accepted April 28, 2017; Epub August 15, 2017; Published August 30, 2017
Abstract: Objective: To discuss the imaging characteristics of splenosis for improving its diagnostic accuracy. Meth-ods: Twelve patients with splenic autotransplantation were diagnosed by surgical pathology or needle biopsy. Pa-tients underwent CT and MRI plan and enhanced scanning, 2 cases also underwent 99mTc-DRBC scanning, and the
imaging data were collected. Results: Multiple nodules were found in 8 cases and single nodule was found in 4 cases. The nodules were detected in splenic recess (10 cases), in tail of the pancreas (5 cases), in right liver (3 cas-es), and in other parts of abdominal cavity (3 cases). The size of nodules was different, and the maximum diameter of 94.57% of the nodules were less than 3 cm. The nodules were all homogeneous and soft without cystic change, calcification or necrosis. Slightly short T1 and short T2 signal were shown in tail of the pancreas in 1 case. Long T1 and long T2 signal were shown in the rest cases. In CT arterial phase, blood supply from abdominal aorta was shown in nodule of right liver in 1 case. The nodules were surrounded by thin layer of low density ring, which showed long T1 and long T2 signal. Homogeneous or inhomogeneous enhancement was shown in the arterial phase, continu-ous homogenecontinu-ous enhancement was shown in portal vencontinu-ous phase, and the decline degree of enhancement was significant in delayed phase. The findings of 99mTc-DRBC scanning were obviously strong radioactive concentrations
in nodules. Conclusion: Multiple nodules were found in abdominal cavity with homogeneous density or signal and clear boundary. The enhanced features were consistent with spleen. The possibility of splenosis should be consid-ered by the history of splenic trauma or splenectomy.
Keywords: Splenosis, CT, MRI, 99mTc-DRBC, splenic trauma
Introduction
Splenosis is an autotransplantation of spleen, which is caused by splenic trauma or splenec-tomy [1]. The spleen tissue usually implants in the abdominal cavity or outside the abdominal cavity, and establishes blood supply for its development. Ectopic growth of spleen tissue debris form space-occupying lesions, so sple-nosis is also called ectopic spleen planting [2, 3]. Ectopic spleen can be divided into congeni-tal accessory spleen and acquired splenosis [3]. Splenosis has essential difference from accessory spleen and surgery autologous spl- enic planting [4].
Splenosis secondary to splenic trauma is com-mon, and the incidence rate is 26-67% [1, 5, 6]. The shortest interval time of spleen planting after trauma is 5 months, and the longest
inter-val time is 32 years (average time 10 years) [3]. When the tissue of spleen implantation and organ are closely related, it is easy to misdiag-nose as tumors and result in clinical misdiagno-sis [7]. On 99mTc-DRBC scanning, multiple
radio-active lesions can be seen in abdominal cavity, and the locations of multiple masses are con-sistent with CT results. The theory [8] is that
heat-denatured red blood cells (RBC) are first
captured by spleen, then are the liver and mar-row. The red blood cells are damaged in spleen, and heme in red blood cells are digested and metabolized. Hence, radioactive concentration of the spleen is 2-4 times higher than liver.
99mTc-DRBC has a higher sensitivity and
speci-ficity for the diagnosis of splenosis [9].
CT and MRI imaging characteristics of splenosis
data were collected for improving its diagnostic accuracy and avoid unnecessary surgeries.
Materials and methods General information
From April 2008 to May 2016, information of
12 patients confirmed by surgical pathology or
needle biopsy were collected. There were 8 males and 4 females aged 18 to 69 years (median age of 43.7). There were no symptoms in 8 patients, who were detected by abdominal ultrasound or CT reexamination. The other 4 patients were detected by abdominal CT because of jaundice, hematuria, haemateme-sis and black stool. Six patients underwent splenectomy because of traumatic spleen rup-ture, and the other six because of cirrhosis and portal hypertension. The splenectomy time was 5 months to 7 years with an average time of 3.5
years. Six patients were confirmed by surgical
pathology and the other six were by needle biopsy.
CT and MRI examinations
Eight patients underwent CT and MRI plain scanning and dynamic enhanced scanning. In addition, two of them underwent 99mTc-DRBC
scanning, which had higher sensitivity and
specificity for diagnosis of splenosis [8, 10].
Four patients only underwent CT plain scanning and dynamic enhanced scanning. 16-slice
[image:2.612.325.524.70.399.2]spi-ral CT (SIEMENS, Sensation) was used in 5 cases, and 256-slice spiral CT (Philips iCT) was used in 7 cases. Tube voltage was 120 kV, tu- be current was 220-250 mAs, and the layer thickness was 5 mm. Non-ionic contrast agent (iohexol) was used in CT examinations. The injection dose was 80-100 ml with injection rate of 2.5-3.0 ml/s. Arterial phase, portal venous phase and delayed phase scanning were conducted at 25-30 s, 60 s, 180 s after drug injection, respectively. Siemens 1.0T Harmony MRI scanner was used in 5 cases, and GE SignaHDxt 1.5T double gradient mag-netic resonance scanner was used in 3 cases. T1WI and T2WI axial scanning were used, and the three-phase dynamic enhanced scanning of MRI was consistent with CT. The contrast agent was Gd-DTPA in MRI examination. The injection dose was 0.2 mmol/kg with injection Figure 1. Splenosis of a 44-year-old man after
sple-nectomy for trauma. On CT scanning, oval nodules in tail of the pancreas and round nodules in spleen fossa showed soft and compact tissue with clear boundary and homogeneous density.
[image:2.612.89.290.72.239.2]CT and MRI imaging characteristics of splenosis
rate of 2.5 ml/s. Two patients underwent 99m
Tc-DRBC examination.
Results
CT and MRI characteristics
Thirty-eight nodules were found in the 12 patients. Twenty-one of 38 nodules were found in the left inferior phrenic splenic recess in 10 cases. The nodules were found in tail of the pancreas in 5 cases, and there was only a nod-ule in each case. The nodnod-ules were found in right liver in 3 cases, and there was a nodule in right posterior lobe of liver and 5 nodules in the surface of right liver. The nodules were found in other parts of abdominal cavity in 3 cases, there were 2 nodules in kidney, a nodule in iliac fossa and 3 nodules in posterior peritoneum. Multiple nodules were found in 8 cases, and each case had 2-8 nodules. Single nodule was found in 4 cases, and the 4 patients underwent
splenectomy because of liver cirrhosis and por-tal hypertension. The shape of nodules was round or oval with clear boundary (Figure 1). The size of nodules was different, and the maxi-mum diameter was 0.5-3.6 cm. 94.57% of the nodules were less than 3 cm. The nodules were all homogeneous and soft without cystic
change, calcification or necrosis. CT values
were 32.3-52.8 HU. In MRI scanning, slightly short T1 and short T2 signal were shown in tail of the pancreas in 1 case (Figure 2). Long T1
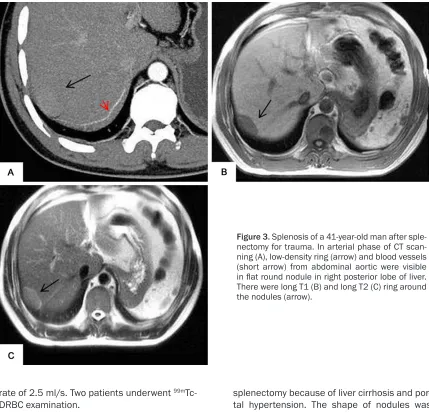
and long T2 signal were shown in the rest cases. In arterial phase of enhanced CT
[image:3.612.91.520.70.483.2]scan-ning, most nodules were significantly homoge -neous enhancement, and only 6 nodules were heterogeneous enhancement and showed plaque-like enhancement with CT values of 53.3-90.5 HU. Blood supply from abdominal aorta was shown in nodule of right posterior lobe of liver in 1 case. The nodule was sur-rounded by thin layer of low density ring, which showed long T1 and long T2 signal (Figure
CT and MRI imaging characteristics of splenosis
3A-C). Homogeneous enhancement was shown in portal venous phase with CT values of 92.2-115.6 HU, which were higher than arterial phase. The decline degree of enhancement
was significant in delayed phase with CT values
of 67.5-83.7 HU (Figure 4A-C). The enhanced features of MRI were similar to CT (Figure 5A-C).
Radionuclide imaging
Strong radioactive concentrations in nodules were detected in splenic recess, tail of the pan-creas and the surface of right liver with clear boundary and homogeneous nuclides (Figure 6).
Surgical pathology
There were capsules in nodules. The sections of nodules were dark red or beige, and the
nod-ules were soft and friable. Thick fibrous tissue
capsules were covered on the edge of lesions,
and there were no significant muscle tissue and elastic fibers. Organizational structure in
nodules were similar to spleen, which was mainly consisted of red pulp with hemostasis. There was white pulp consisted of dense
lym-phocytes, too. Lymphatic sheath and splenic
nodules were formed by parts dense lympho-cytes around the small arteries. The structure of white pulp in part region was incomplete. So the structure of hilus of spleen was not seen.
Discussion
In 1910, Von Kuttner first proposed the con -cept of splenic implantation after splenic
trau-ma. In 1912, Von StenbenRouc first proved the
[image:4.612.85.525.70.504.2]CT and MRI imaging characteristics of splenosis
necrosis would happen to other kind of cells.
Once the scaffolds consisted of reticulocytes and fibrous tissues were formed, the cells would differentiate into endothelial sinus, capil-Figure 5. The same patient of capil-Figure 3. In MRI scanning, inhomogeneous enhancement was visible in the arterial phase (A), continu-ous homogenecontinu-ous enhancement was visible in portal venous phase (B), and the decline degree of enhancement was significant in de-layed phase (C).
[image:5.612.88.527.69.643.2]CT and MRI imaging characteristics of splenosis
laries, and lymphocytes, and finally form spleen
tissues. These spleen tissues had the ability of phagocytosis of spleen.
Most patients with spleen planting do not have symptoms, and they are found by autopsy, abdominal surgery or imaging examination for other reasons [11]. There are few reports about the implanted spleen located in special area. If splenosis occurs in gastrointestinal tract, it will cause stomachache, intestinal obstruction and gastrointestinal bleeding [12, 13]. If splenosis occurs in female pelvic cavity, it will cause chronic pelvic pain, dysmenorrheal and deep sexual intercourse pain [14, 15]. When the tis-sue of spleen implantation and organ are close-ly related, it is easy to misdiagnose as tumors and result in clinical misdiagnosis [7]. Splenosis is a compensatory behavior when the body is free from spleen and another form of ectopic spleen. Arroja [12] et al. reported that spleen implanted nodules had compensation function and proliferative function. The common fatal complication after splenectomy was over-whelming infection, and the longest interval time was 40 years, which indicated that patients without spleen might have a lifetime risk of overwhelming infection [2, 16]. For patients had no symptoms, they were
suggest-ed not to receive treatment, which nesuggest-edsuggest-ed defi -nite preoperative diagnosis and differentiate from benign and malignant tumors and acces-sory spleen.
The number of splenic implanted nodules can range from one to hundreds. Even only single nodule was found by imaging examination,
there were a large number of dark red inflam -matory nodules with a size of soybeans distrib-uted in the peritoneum [17, 18]. It is common in splenic recess, and it also can be seen in the tail of pancreas and the right liver. Because the splenic implanted nodules do not have sepa-rated blood supply, so the diameter of 94.57% of the nodules is less than 3 cm [3]. On CT and MRI scanning, the density and signal were simi-lar to normal spleen. The nodules were homo-geneous and soft. Homohomo-geneous or inhomoge-neous enhancement was shown in the arterial phase, continuous homogeneous enhance-ment was shown in portal venous phase, and
the decline degree of enhancement was signifi -cant in delayed phase. If the scanning time in arterial phase was appropriate, plaque-like enhancement could be seen, and the enhanced
characteristics was the same as normal spleen, which were consistent with previous reports [2, 3, 6, 14, 17, 18].
Accessory splenosis usually single, and the sit-uation of more than six is rare [19]. It has big size and locates in mesangium surrounding the spleen. The shape is oval with clear boundary. It has one hilus of spleen and thick capsule. Blood supply is supported by the splenic artery. Splenosis is usually multiple and small [20]. The diameter is usually less than 3 cm. It can locate in internal and external of the abdominal cavity, and the spleen tissue debris can distrib-ute to anywhere. When the growing space is limited by surrounding structures, the shape can be variable. There is no hilus of spleen. It
has fibrous capsule separated from adjacent
organs. A number of blood vessels through thin pseudocapsule can be seen. The difference between accessory spleen and splenosis is that splenosis is almost associated with spleen trauma.
In conclusion, for patients who has splenic trau-ma or splenectomy, the possibility of splenosis should be considered once the homogeneous soft mass with similar density, signal and enhanced characteristics to spleen is found in abdominal cavity. It is important to know the history and imaging characteristics to avoid unnecessary surgeries. 99mTc isotope scanning
and percutaneous puncture of the mass will help to diagnose.
Disclosure of conflict of interest
None.
Address correspondence to: Dr. Jianhua Wang, De- partment of Radiology, The Affiliated Hospital of Medical College of Ningbo University, Ningbo 3150- 20, China. Tel: +86-13586582317; E-mail: wangji- anhua573@163.com
References
[1] Kang KC, Cho GS, Gui AC, Kang GH, Yong JK, Lee MS, Kim HK and Park SJ. Intrahepatic splenosis mimicking liver metastasis in a pa-tient with gastric cancer. J Gastric Cancer 2011; 11: 64-68.
CT and MRI imaging characteristics of splenosis
[3] Berman AJ, Zahalsky MP, Okon SA and Wagner JR. Distinguishing splenosis from renal mass-es using ferumoxide-enhanced magnetic rmass-eso- reso-nance imaging. Urology 2003; 62: 748-748. [4] Ksiadzyna D and Peña AS. Esplenosis
abdomi-nal. Rev Esp Enferm Dig 2011; 103: 421-426. [5] Carobbi A, Romagnani FG and Bianchini M.
Laparoscopic splenectomy for severe blunt trauma: initial experience of ten consecutive cases with a fast hemostatic technique. Surg Endosc 2010; 24: 1325-1330.
[6] Kim K, Choi HJ, Kim YM, Kwon WJ, Lee WC, Suh JH. Thoracic splenosis: a case report and the importance of clinical history. J Korean Med Sci 2010; 25: 299-303.
[7] Ksiądzyna D. A case report of abdominal sple-nosis-a practical mini-review for a gastroenter-ologist. J Gastrointestin Liver Dis 2011; 20: 321-324.
[8] Crivellaro C, Cabrini G, Gay E, Sara R and Ros-setti C. Intrathoracic splenosis: evaluation by 99mTc-labelled heat-denatured erythrocyte SPECT/CT. Eur J Nucl Med Mol Imaging 2010; 38: 412.
[9] Baldari G, Sindoni A, Belletti A, Baldari S and Ruffini L. (99m)Tc disphosphonate uptake due to splenosis: incidental finding 60 years after splenectomy. Clin Nucl Med 2015; 40: 533-535.
[10] Kao PF, Tzen KY, Tsai MF and Lin JN. 99mTc-sulphur-colloid and heat-denatured 99mTc-la-belled red cell scans demonstrating a giant in-trapelvic spleen in a girl after splenectomy. Pediatr Radiol 2001; 31: 283-285.
[11] Fukuhara S, Tyagi S, Yun J, Karpeh M and Reyes A. Intrathoracic splenosis presenting as persistent chest pain. J Cardiothorac Surg 2012; 7: 1030-1030.
[12] Arroja B, Almeida N, Macedo CR, Moreira AP, Oliveira P, Tomé L, Gouveia H and Sofia C. Gas-tric splenosis: a rare cause of digestive bleed-ing. Rev Esp Enferm Dig 2011; 103: 377-378. [13] Obokhare ID, Beckman E, Beck DE, Whitlow CB
and Margolin DA. Intramural colonic splenosis: a rare case of lower gastrointestinal bleeding. J Gastrointest Surg 2012; 16: 1632-1634. [14] Ekong E, Goojha C and Kamencic H. Expect the
unexpected: a case of pelvic splenosis. J Ob-stet Gynaecol Can 2011; 33: 787.
[15] Macario S, Chassang M, Novellas S, Baudin G, Delotte J, Toullalan O and Chevallier P. The value of pelvic MRI in the diagnosis of posteri-or cul-de-sac obliteration in cases of deep pel-vic endometriosis. AJR Am J Roentgenol 2012; 199: 1410-1415.
[16] Javadrashid R, Paak N and Salehi A. Combined subcutaneous, intrathoracic and abdominal splenosis. Arch Iran Med 2010; 13: 436-439. [17] Lake ST, Johnson PT, Kawamoto S, Hruban RH
and Fishman EK. CT of splenosis: patterns and pitfalls. AJR Am J Roentgenol 2012; 199: 686-693.
[18] Kellert B, Caster M, Jean RD and Vaccarello L. Diffuse intra-abdominal splenosis presenting as carcinomatosis exhibiting positron emitted tomography hypermetabolic activity. Gynecol Oncol Case Rep 2013; 5: 46-48.
[19] Ota T and Ono S. Intrapancreatic accessory spleen: diagnosis using contrast enhanced ul-trasound. Br J Radiol 2004; 77: 148-149. [20] Liu Y, Ji B, Wang G and Wang Y. Abdominal