www.wjpr.net Vol 8, Issue 12, 2019. 1072
PRESCRIBING PATTERN OF DRUGS IN THE TREATMENT OF
HYPERTENSION IN A TERTIARY CARE TEACHING HOSPITAL: A
PROSPECTIVE OBSERVATIONAL STUDY
Dr. Nazish Fathima*, Haran Prasad H. J., Hephzibha S. Mathew, Jasmin Seira Jose and
Jemimah V. Cherian
Department of Pharmacy Practice, Bapuji Pharmacy College Davangere, Karnataka.
ABSTRACT
Background: Hypertension is a common chronic medical condition
which is identified as the 3rd leading risk factor for global burden of
diseases. According to Joint National Committee guidelines,
hypertension is defined as elevated systolic blood pressure of
≥140mmHg or diastolic blood pressure of ≥ 90mmHg. Objective: The
objective of this study is to analyse the prescribing pattern associated
with antihypertensives. Materials and Methods: A Prospective
Observational study was carried out for a period of 6 months in an
inpatient department in Shamanur Shivashankarappa Institute of
Medical Science and Research Centre, a tertiary care teaching hospital,
Davangere. The data was collected from case sheets of all inpatients taking at least one
antihypertensive. Results: A total of 150 prescriptions were analysed, out of which,
88(58.66%) were males and 62(41.33%) were females. The mean age group of study
population was found to be 60-80 years (52%). The most commonly reported co- morbidity
along with hypertension was Diabetes mellitus 80 (53.33%). Monotherapy was most
preferred therapy which was given in almost 76 (50.66%) followed by combination therapy.
In monotherapy Calcium channel blockers 35(46.04%) was most commonly prescribed.
Conclusions: The present study confirms that the Prescribing patterns of antihypertensive
drugs were in concordance with joint national committee 8 guidelines for patients with
different compelling indications. The most frequently prescribed class of drug as
monotherapy was Calcium Channel Blockers, followed by diuretics, which was also the most
commonly used class of drugs in combination therapy.
KEYWORDS: Hypertension, Prescribing pattern, Anti-hypertensives, JNC-8.
Volume 8, Issue 12, 1072-1089. Research Article ISSN 2277– 7105
Article Received on 30 August 2019,
Revised on 19 Sept. 2019, Accepted on 09 Oct. 2019,
DOI: 10.20959/wjpr201912-16064
*Corresponding Author
Dr. Nazish Fathima
INTRODUCTION
Hypertension (HTN) also known as high blood pressure (BP) is a common chronic medical
condition.[1] According to Joint National Committee (JNC 8) guidelines, HTN is defined as elevated systolic BP of ≥140mmHg or diastolic BP of ≥90mmHg.[3]
According to JNC 8, BP in adults is classified into[7]
Categories of HTN Systolic BP (mmHg) Diastolic BP (mmHg)
Normal Pre HTN Stage I HTN Stage II HTN
<120 120-139 140-159 >160 <80 80-89 90-99 >100
The GBD Study found HTN as the third most preventable cause of death worldwide and the
second most common condition in Western countries.[8] For rational planning of health
services accurate estimates of the worldwide prevalence of this condition are essential as a
source of primary information.[2] Worldwide prevalence for HTN is estimated to be in 1
billion individuals, in which approximately 7.1 million deaths per year may be attributable to
HTN and its complications.[9] Approximately 40% of adults aged 25 and above had been
diagnosedwith HTN; the number of people with the condition increased from 600 million in
1980 to1 billion in 2008.[4] The prevalence of HTN is highest in the African Region in 46%
of adults aged 25 and above, while the lowest prevalence is in America in 35% of adults.
Overall, high-income countries have a lower prevalence of HTN 35% than other groups at
40%.[4] The prevalence of compelling indication was high among stage II HTN patients
(59.45%).[10]
According to WHO health statistics 2012, the prevalence of HTN in adults ≥25 years of age
was 23.1% in men and 22.6% in women.[11] Overall in 2000, 26·4% of the world’s adult
population had HTN- 26·6% in men and 26·1% in women, and 29·2% were predicted to have
HTN by 2025- 29·0% in men and 29·5% in women.[2] According to the data published in
United States, the prevalence of HTN is 28.7%, but the same rises to 65.4% in those above 65
years of age.[12] The estimated total number of adults with HTN in 2000 was 972 million; 333
million in economically developed countries and 639 million in economically developing
countries.[7] In India, the overall prevalence for HTN was estimated to be 29.8%.[11] The
overall occurrence of HTN is similar between both men and women but it differs with age.
older people they were higher in women than in men.[5] The lowest estimated prevalence of HTN for both men and women was in the region “other Asia and islands”.[2]
Uncontrolled HTN leads to severe long term complications such as stroke, heart failure,
congestive heart disease and end-stage renal disease.[6] Generally, HTN is commonly
associated with diabetes and chronic renal failure.[13] The higher prevalence of HTN is the
major cause for more than half of the cardiovascular diseases (CVD) and is a leading risk
factor for foetal and maternal deaths in pregnancy, dementia.[14] HTN attributes to 29% of
Stroke, 24% of Acute MI, 21% of peripheral vascular disease and 10% of ischemic heart
disease.[15] Worldwide, complications of HTN accounts for 9.4 million deaths every year.
HTN is responsible for 51% of deaths due to stroke (total stroke mortality) and 45% of deaths
due to heart disease (total ischemic heart disease mortality).[4] If HTN left untreated about
50% of the patients will die of coronary artery disease, 33% of cerebrovascular stroke, 20%
of diabetes and 10-15% chronic renal failure.[16] Hence, lifelong management and lifestyle
modification, and pharmacotherapy are needed for its treatment and management. The main
goal is to reduce morbidity and mortality through a reduction in hypertensive associated
complications.[17]
Rational use of drug is important for the wellbeing of the patient.[20] Prescribing pattern is a
component of medical review, which seeks monitoring, evaluation and necessary
modification in prescribing practices of prescribers to achieve rational and effective medical
care.[21] Prescribing pattern in HTN is complex and many factors make this group a high risk
such as polypharmacy, comorbid conditions, pharmacokinetic and pharmacodynamics
variability, and noncompliance.[4] The choice of drugs for a particular patient changes at short
intervals because of factors like efficacy, side effects, cost and development of newer
drugs.[22] Medication quality and patient safety requires a rational prescription of medication
and avoidance of inappropriate prescribing patterns.[18] In medicine practice, there is growing
concern regarding the irrational prescription pattern and use of antihypertensive drugs.[8]
Irrational prescribing of drugs is of common occurrence in the clinical practice, important
reasons being lack of knowledge about drugs, unethical drug promotions and irrational
prescribing habits of clinicians.[23] Inappropriate prescribing habits lead to ineffective and
unsafe treatment, prolongation of illness, distress and unnecessary economic burden to the
patient.[19] Prescribing pattern helps to assess whether the current usage is rational or in
use of least number of drugs to obtain the best possible effect in shortest period.[25] A
prescription-based survey is considered to assess and evaluate the prescribing attitude of
physicians and dispensing practice of pharmacists.[8] The prescribing pattern of
antihypertensive with or without co-morbidities is assessed based on drug class, dosage,
frequency, route, generic, duration and severity of HTN. A large number of antihypertensive
drugs are available, either as alone or in various combinations with other drugs. Monitoring
of prescription components helps identifying the problems while prescribing and provide
feedback to the prescribers.[22] Recommendations regarding the choice of drugs are available
as treatment guidelines to reduce practice variability, cost and improve rational
pharmacotherapy. Implementation of these guidelines is effective in raising the quality of
antihypertensive therapy.[9]
According to the updated 2014 JNC-8 guidelines on HTN, evidence from clinical trials
indicate that antihypertensive medications (BP medication) should be initiated in patients less
than 60 years old if the systolic BP is persistently >140 mmHg and the diastolic BP is
persistently >90 mmHg despite non pharmacologic therapy. If a patient is 60 years or older,
antihypertensive therapy should be initiated if the systolic BP is >150mmHg and the diastolic
BP is >90 mmHg.[5]
With the increasing prevalence of HTN, there is an increase in the use of antihypertensive
drugs, which to a far extent can improve the quality of life and decrease the attributed
morbidity and mortality.[15] The JNC-8 is considered the “gold standard” consensus
guidelines for the management of HTN. A 2014 JNC8 report suggests that in patients aged
≥60 years, BP should be targeted to <150/90 mm Hg.[4]
The updated JNC8 guidelines
treatment is addressed separately based on ethnicity and it also consider first –line and
later-line treatments to be limited to 4 classes of medications: Thiazide type diuretics, CCB, ACE
inhibitors, and ARBs followed by second- and third- line alternatives included higher doses
or combinations of ACE inhibitors, ARBs, Thiazide – type diuretics and CCBs.[13]
MATERIALS AND METHODS
A prospective observational study was conducted in SSIMS&RC, a tertiary care teaching
hospital, Davangere, for a period of 6 months. Before commencement of the study, ethical
clearance was obtained from Institutional Ethical Committee. A total of 150 patients were
included in the study. All patients admitted above 18 years of age who are diagnosed with
Patients who are not willing to participate in the study, pregnant and lactating women with
hypertension were excluded from the study. A suitably relevant patient data collection form
was developed containing patient demographics, co-morbidities, past and present medication,
HTN complication, BP and other monitoring parameters. Collected data was then analysed.
The summarized findings were rearranged and tabulated in a graphical and table form.
RESULTS
Gender distribution
Among 150 individuals 58.67% (88) of males and 41.34% (62) females received anti-HTN
[image:5.595.135.458.298.610.2]drugs. Table 1 shows the gender distribution in the study population.
Table 1: Gender distribution, n=150.
GENDER NUMBER OF
PATIENTS(n)
PERCENTAGE (%)
MALE 88 58.67
FEMALE 62 41.33
Figure 1.1: Gender Distribution.
Age distribution
Out of 150 patients enrolled, majority of subjects fall under the age group of 60-80 years 52%
(78) followed by 39-59 years 40.66% (61). The mean age group of the study population was
found to be 58.97±12.42 years. The table 2 shows the age distribution in the study
Table 2: Age Distribution. n=150.
AGE(YEARS) NUMBER OF PATIENTS(n) PERCENTAGE (%)
18-38 9 6
39-59 61 40.66
60-80 78 52
[image:6.595.88.493.81.414.2]>80 2 1.34
Figure 2.1: Age Distribution.
Distribution of co morbidities in study population
Among 150 patients, the most commonly occurred co morbid condition was found to be
Diabetes mellitus followed by cardiovascular diseases. Table 3 shows the distribution of co-
morbidities in the study population.
Table 3: Distribution of Comorbidities in Study Population. n=150.
SL NO CO MORBID
CONDITION FREQUENCY(n)
PERCENTAGE (%)
1 Diabetes mellitus 80 53.33
2 Cardiovascular diseases 53 35.33
3 Respiratory disorder 41 27.33
4 Cerebrovascular attack 33 22
5 Chronic kidney disease 25 16.66
Figure 3.1: Distribution of Comorbidities in Study Population.
Stages of hypertension in the study population
Among the 150 patients, 33.33% (50) were suffering with stage 2 hypertension followed by
31.33% (47) stage 1 hypertension and 19.33% (29) pre-hypertension. The details of stages of
HTN in the study population is shown in table 4.
Table 4: Stages of Hypertension in Study Population, n=150.
CLASSIFICATION NUMBER OF PATIENTS(n) PERCENTAGE (%)
Normal 24 16.01
Pre-hypertension 29 19.33
Stage 1 HTN 47 31.33
Stage 2 HTN 50 33.33
[image:7.595.86.509.415.741.2]PRESCRIBING PATTERN
Prescribing Pattern of Antihypertensives
Among 150 patients, monotherapy was given in almost 50.66% (76) patients, dual therapy
was indicated in 38.66% (58) patients, and triple therapy was used only in 8% (12) patients.
Quadruple therapy is the least preferred combination therapy which accounts only in 2.66%
[image:8.595.99.495.222.522.2](4) patients.
Table 5: Prescribing Pattern of Antihypertensives. n=150.
TREATMENT NO. OF PATIENTS(n) PERCENTAGE (%)
Monotherapy 76 50.66
Dual Therapy 58 38.66
Triple Therapy 12 8
Quadruple Therapy 4 2.68
Figure 5.1: Prescribing Pattern of Antihypertensives.
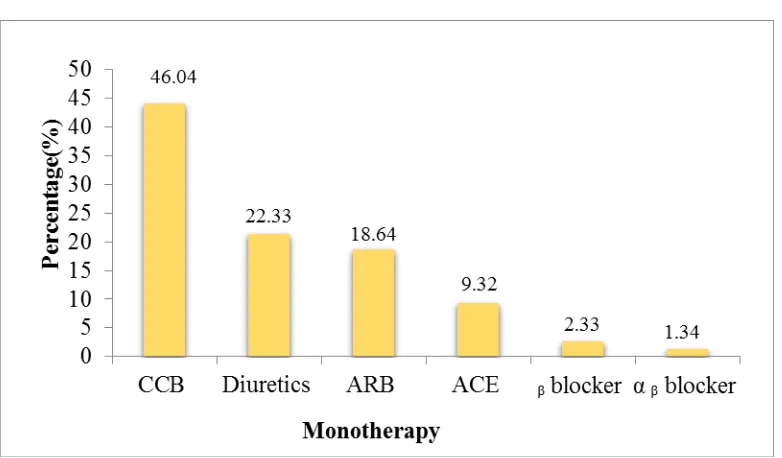
Prescribing Pattern of Antihypertensives as Monotherapy
In monotherapy Calcium channel blockers 46.04% (35) were most commonly prescribed
anti- hypertensive followed Diuretics 22.33% (17) and ARB’s 18.64% (14).
Table 6: Prescribing Pattern of Antihypertensives as Monotherapy. n=76.
CLASS NUMBER OF PATIENTS(n) PERCENTAGE (%)
CCB 35 46.04
Diuretics 17 22.33
ARB 14 18.64
ACE 7 9.32
ᵦ blocker 2 2.33
Figure 6.1: Prescribing Pattern of Antihypertensives As monotherapy.
Commonly Prescribed Antihyperytensives as Monotherapy
Among the Calcium channel blockers, amlodipine (46), among Diuretics, Furosemide (28)
and among ARB, Telmisartan (23) were most commonly prescribed.
Table 7: Commonly Prescribed Antihypertensive as Monotherapy.
SL NO DRUGS NO.OF PATIENTS(n)
1 Amlodipine 47
2 Furosemide 28
3 Telmisartan 23
4 Spironolactone 10
5 Torsemide 9
6 Ramipril 7
7 Carvedilol 7
8 Metoprolol 6
9 Atenolol 2
10 Hydrochlorothiazide 2
11 Losartan 2
12 Cilnidipine 2
13 Propranolol 1
14 Labetalol 1
15 Enalapril 1
16 Felodipine 1
Figure 7.1: Commonly prescribed antihypertensive as monotherapy.
Prescribing Pattern of Antihypertensives as Dual Therapy
In dual therapy calcium channel blockers + diuretics 24.13% (14) were mostly prescribed
followed by ARB + diuretics 20.68% (12) and CCB+ ᵦ blocker 18.96% (11).
Table 8: Prescribing Pattern of Antihypertensives as Dual Therapy. n=58
CATEGORY NUMBER OF PATIENTS(n) PERCENTAGE (%)
CCB+ Diuretics 14 24.13
ARB+ Diuretics 12 20.68
CCB + ᵦ blocker 11 18.96
ARB +CCB 6 10.35
ᵦ Blocker+ ARB 3 5.17
Diuretic +αᵦ blocker 3 5.17
ᵦ Blocker + diuretics 3 5.17
ᵦ Blocker + ACE 2 3.45
Diuretics + ACE 1 1.73
ACE + αᵦ blocker 1 1.73
ARB +αᵦ blocker 1 1.73
Figure 8.1: Prescribing Pattern of Antihypertensives as Dual Therapy.
Prescribing Pattern of Antihypertensives as Triple Therapy
In triple therapy, diuretics + CCB+ ARB 4(33.36%) was most commonly prescribed followed
by CCB+ ARB+ ᵦ blocker 25% (3).
Table 9: Prescribing Pattern of Antihypertensives as Triple Therapy. n=12.
CATEGORY NUMBER OF PATIENTS(n) PERCENTAGE (%)
Diuretic+ CCB+ ARB 4 33.36
CCB +ARB+ᵦ blocker 3 25.00
Diuretics+ ARB+αᵦ blocker 2 16.66
Diuretics+ CCB +ᵦ blocker 1 8.33
ARB +Diuretic +α2 agonist 1 8.33
αᵦ blocker + diuretic + ACE 1 8.33
[image:11.595.76.520.382.735.2]Prescribing Pattern of Antihypertensives as Quadruple Therapy
In quadruple therapy, ARB+ CCB+ Diuretics+ ᵦ blocker 75% (3) was commonly prescribed
[image:12.595.76.521.155.402.2]followed by ARB+ ACE+ Diuretics+ ᵦ blocker 25% (1).
Table 10: Prescribing Pattern of Antihypertensives as Quadruple Therapy.
CATEGORY NO OF PATIENTS(n) PERCENTAGE (%)
ARB+ CCB+ Diuretics+ ᵦ Blocker 3 75
Diuretic + ᵦ Blocker+ ARB+ ACE 1 25
Figure 10.1: Prescribing Pattern of Antihypertensives as Quadruple Therapy.
DISCUSSION
Increased life expectancy and high global prevalence of HTN and its complication render
treatment of this condition a lifelong personnel and social burden. The increasing prevalence
of HTN along with world’s ageing population places an increasing burden on health care
system. Antihypertensives plays an important role in improving, preserving and restoring
health. Prescribing pattern helps to assess whether the current usage is rational or in
concordance with current treatment guidelines for HTN.
This study was carried out in a tertiary care hospital for a period of 6 months. During the
study period, general prescribing pattern of antihypertensives, prescribing pattern of
antihypertensives as monotherapy, dual therapy, triple therapy and quadruple therapy were
done. A total of 150 cases of patients who were receiving antihypertensives were
prospectively monitored during the study of which 88 (58.67%) were males and 62 (41.33%)
were females which is in concordance with the study carried out by Yadav et.al where a male
patients in the age group 60-80 years have more incidence of HTN followed by 39-49 years,
and this incidence is less observed in other study.[4]
Altogether 143 (95.33%) patients in our study were found to have concomitant comorbidities
and Diabetes Mellitus (27.02%) was highly prevalent comorbidity followed by
cardiovascular disease (17.90%), respiratory disorders (13.86%), Cerebrovascular
accidents(11.15%), CKD (8.44%). Other comorbidities found were metabolic
encephalopathy, anemia, hypothyroidism, deep vein thrombosis, Urinary tract infection etc.
majority of the patients were comorbid with Diabetes Mellitus which was in accordance with
study conducted by Abegaz et al.[26]
About 50 (33.33%) patients had stage II HTN followed by 47 (31.33%) patients had stage I
HTN and 29 (19.33%) patients had pre-HTN respectively, as per JNC 8 classification, was
found to be similar to the study conducted by Nwaka et al where 115 (56.9%) patients had
stage II HTN, 75 (37.1%) patients had stage I HTN and 12 (5.9%) patients had pre HTN.[17]
In the present study monotherapy was given in almost 76 (50.66%) patients prescribed with
CCB (46.04%) followed by diuretics (22.33%), ARB (18.64 %), ACE inhibitors (9.32%).
This was in concordance with the study conducted by Prasanna et al where monotherapy was
given in 200 patients followed by dual therapy 166 (42.13%) patients, triple therapy in 24
(6.09%) patients, quadruple therapy in 4 (1.01%) patients.[9] According to JNC 8 on
detection, evaluation, prevention and treatment recommends the use of ACE inhibitors,
ARBs, thiazides, diuretics and CCBs alone or in combination for the management of early
stages of HTN. Thus suggesting that the above trend is in conformity to the recommendation
of JNC8 guidelines. In our study CCB (46.04%) constitutes the most frequently prescribed
antihypertensive drug class followed by diuretics (22.33%), ARB (18.63%), and ACE
Inhibitors (9.32%) which were comparable with the study carried out by Bhandari et al where
CCB (87.34%) were most commonly prescribed followed by diuretics (3.80%), ACE
inhibitors (3.80%), ARBs (2.53%) and beta blocker (1.26%). But in our study the third
commonly prescribed antihypertensive category was diuretics, ACE and beta blocker. In our
study among CCBs amlodipine was most commonly prescribed drug as monotherapy and
among diuretics furosemide was most commonly prescribed. This finding is supported by the
CCB +diuretics combination (24.13%) was mostly used in 2 drug combination therapy
followed by ARB + diuretics (20.68%) and CCB+ beta blocker (18.96%) combination. 3
drug combination as an antihypertensive mainly Diuretics +CCB+ ARB (33.36%) followed
by CCB+ ARB+ beta blocker (25%) and diuretics +ARB + alpha beta blocker (16.66%). In 4
drug combinations, ARB+CCB+ Diuretic+ beta blocker (75%) followed by diuretic+
betablocker + ARB+ACE (25%). In combination therapy CCB+ Diuretics were most
commonly used in our study in accordance with Sharma et al.[3] But the other combinations in
our study is not in compliance with the study done by Sharma et al.[3] In the present study
most of the 3 drug combinations consists of diuretics where the leading drug combinations to
be the most commonly prescribed indicating that diuretics were used more common as
component of multi drug therapy, the use of diuretic in multi drug regimen is recognized as
essential for reduction of blood volume, vascular resistance and hence efficiency of the
combined regimen. This is consistent with the study done by Gupta et al.[27]
CONCLUSION
The present study confirms that the Prescribing patterns of antihypertensive drugs were in
concordance with joint national committee (JNC) 8 guidelines for patients with different
compelling indications. The study also provides the baseline data for similar studies in future,
as the pattern in prescribing antihypertensive drugs keep changing.
In the present study male predominance could be seen. Most of patients were in the age group
of 60-80 years, constituting 52% of total patients. It was also observed that the physicians had
preferred monotherapy more often than the combination therapy. The most frequently
prescribed class of drug as monotherapy was CCBs, on account of its fewer side effects,
followed by diuretics, which was also the most commonly used class of drugs in combination
therapy. In CCBs, most commonly prescribed was amlodipine and Furosemide was most
commonly prescribed in diuretics. Approximately 95.3% of the sample patients had
co-morbidities, in which Diabetes mellitus was the commonly identified co morbid condition.
CCBs were the most commonly prescribed class of drug alone or as part of combination
therapy.
However, further studies are necessary to set up a rationale or pattern for the choice of
medication; taking into consideration the demographic factors involved in the prevalence of
hypertension. Furthermore, physicians should be sensitized to adhere to the standard
health outcome and improvement in quality of life of patients suffering from hypertension
with co-morbidities. Physician should use standard guidelines to treat hypertensive patients
for the effective management of hypertension. The evaluation pattern, patient adherence to
the treatment, physician adherence to hypertension management guidelines, and other data
concerning co morbid conditions have been explored in many clinical studies. In spite of
these data and published guidelines, inconsistencies exist towards treatment approach,
because of which physicians sometime shave to individualize the therapy, based on specific
patient characteristics and response to treatment. In developing countries like India, more
systematic studies are required on the evaluation of prescribing patterns and guideline based
antihypertensive medications’ use, which can be tailored to suit the patients' requirements.
ACKNOWLEDEMENT
We are grateful to our Principal, HOD and Faculties of Pharmacy Practice Department,
Bapuji Pharmacy College for their continuous support and encouragement.
CONFLICT OF INTEREST
There was no conflict of interest between the authors.
REFERENCES
1. Pyarelal. A study of prescription pattern of antihypertensive drugs in a tertiary care
teaching hospital. Indian Journal of Basic and Applied Medical Research, 2015 June;
4(3): 584-8.
2. Kearney P, Whelton M, Reynolds K, Muntner P, Whelton P, He J. Global burden of
hypertension: analysis of worldwide data. The lancet, 2005 Jan 15; 365(9455): 217-23.
3. Sharma A, Dahiya N, Kairi J, Bharati S. Prescription pattern of antihypertensive drugs in
a tertiary care teaching hospital in India. International Journal of basic & Clinical
Pharmaclogy, 2015 Jan; 4(1): 55-9.
4. Romday R, Gupta AK, Bhambani P. An assessment of antihypertensive drug prescription
patterns and adherence to Joint National Committee-8 hypertension treatment guidelines
among hypertensive patients attending a tertiary care teaching hospital. Int J Res Med Sci,
2016; 4(12): 5125-33.
5. Bell K, Twiggs J, Olin BR, Date IR. Hypertension: The silent killer: updated JNC-8
6. Pathmashri VP, Vikranth V, Sundari S. Study on the prescription pattern of
antihypertensive drugs among acute coronary syndrome patients in South Indian
population. Drug Invention Today, 2018 Sep 22; 10(4): 3714-19.
7. Yadav VK, Keshari SS, Pandey K. Prescribing Pattern of Antihypertensive Drugs in a
Tertiary Care Teaching Hospital in Lucknow Region. Indian Journal of Clinical Practice,
2016 Feb; 26(9): 819-21.
8. Neupane GP, Rai M. Adverse drug reaction profile and prescription pattern of
antihypertensive drug monotherapy at tertiary care hospital Nepalgunj, Nepal. Int J Basic
Clin Pharmacol, 2018 Jan; 7(1): 75-9.
9. Rajasekhar DG, Prasanna DG, Chandrakanth P. Prescribing pattern of antihypertensive
drugs based on compelling indications with hypertension. Int J Pharm Pharm Sci, 2016;
8(2): 72-5.
10. Shobana J, Semere M, Sied M, Eyob T, Russom M. Prescribing pattern of
anti-hypertensive drugs among hypertension patients with cardiac complications in Eritrea.
Lat Am J Pharm, 2013 Jun 1; 32(5): 745-8.
11. Gupta R, Malhotra A, Malhotra P. Assessment of rational use of fixed dose combinations
in hypertension in a tertiary care teaching hospital in north India. International Journal of
Advances in Medicine, 2018 Sep; 5(5): 1263.
12. Naidu CD and Vardhan A. A Study of the prescription pattern of antihypertensive drugs
in a tertiary care teaching hospital of Andaman & Nicobar Island. International Journal of
Pharmacological Research, 2017; 7(05): 103-6.
13. Kuriakose NG, Bhandari R, Sai BK, Jayalakshmi E, Teja PR. A Study to Assess and
Evaluate Prescribing Patterns of Antihypertensive Drugs in Medicine Ward of a Tertiary
Care Teaching Hospital at Vijayanagara Institute of Medical Sciences, Ballari, Karnataka.
JAMPS, 2018 May 29; 17(1): 1-9.
14. Islam SM, Mainuddin AK, Islam MS, Karim MA, Mou SZ, Arefin S, Chowdhury KN.
Prevalence of risk factors for hypertension: A cross-sectional study in an urban area of
Bangladesh. Global Cardiology Science and Practice, 2015 Nov: 1-9 doi:
10.5339/gcsp.2015.43.
15. Pilakkadavath Z, Shaffi M. Modifiable risk factors of hypertension: A hospital-based
case–control study from Kerala, India. Journal of family medicine and primary care,
16. Do HT, Geleijnse JM, Le MB, Kok FJ, Feskens EJ. National prevalence and associated
risk factors of hypertension and prehypertension among Vietnamese adults. American
journal of hypertension, 2014 May 26; 28(1): 89-97.
17. Nwaka AL, Nduka SO, Osonwa UE, Maureen A, Samuel UU, Ele GN. Evaluation of the
prescription pattern of antihypertensive agents in a tertiary health institution in Nigeria.
African Journal of Pharmacy and Pharmacology, 2015 May 29; 9(20): 540-6.
18. Kumar M, Dahiya V, Mishra S, Sharma D, Mishra N, Lahkar M. Cardiovascular disease
prevalence and drug utilization patterns at a tertiary care hospital in northeastern India. Int
J Pharm Pharm Sci, 2016; 8(6): 116-9.
19. Dawalji S, Venkateshwarlu K, Thota S, Venisetty PK, Venisetty RK. Prescribing pattern
in coronary artery disease: a prospective study. International Journal of Pharma Research
& Review, 2014 Mar; 3(3): 24-33.
20. Amruth Raj V, Gautam A, Ghimire S, Shashidhar G, Mahesh NM, Gyawali S.
Prescribing pattern of antihypertensive drugs and cost analysis in a tertiary care teaching
hospital. World Journal of Pharmacy and Pharmaceutical Sciences, 2015 Feb 24; 4(5):
958-76.
21. Divya G, Devi AR, Lakshmi P, Kishore SR, Prasad TD, Ranganayakulu D. Prescribing
Patterns of Antihypertensive Drugs in Cardiology Department. Inventi Rapid: Pharmacy
Practice, 2014 Jun; 3(1): 976-84.
22. Philip R, Drishyamol KA, Mathew M, Reddy VLT, Mahesh NM and Krishnamurthy MS.
Prescribing pattern of antihypertensive drugs in geriatric population in tertiary care
hospital. International Journal of Pharmacological Research, 2016; 6(03): 114-119.
23. Rakesh B, Suresha BS, Himaja J, Joy ET, Varghese AR. Assessment of prescribing
pattern in coronary artery disease. International Journal of Allied Medical Sciences and
Clinical Research, 2016 Oct; 4(4): 698-715.
24. Shah J, Balraj A. Drug Utilization pattern of antihypertensive agents in patients of
hypertensive nephropathy in a tertiary care hospital: A cross sectional study. International
Journal of Basic & Clinical Pharmacology, 2017; 6(9): 2131-33.
25. Vakade KP, Thorat VM, Khanwelkar CC, Jadhav SA, Sanghishetti VM. A study of
prescribing pattern of drugs in patients of cardiovascular emergencies at a tertiary care
hospital of Western Maharashtra. Int J Res Med Sci, 2016 Feb; 4(2): 556-61.
26. Abegaz TM, Tefera YG, Abebe TB. Antihypertensive drug prescription patterns and their
Integrated Pharmacy Research and Practice. 2017: [Internet]. 2017[Cited 25 Feb 2019].
Available from: http: //www.dovepress.com/
27. Gupta R, Malhotra A, Malhotra P. Study of prescribing pattern of drugs used in the
treatment of hypertension in a tertiary care teaching hospital in North India: an
observational study. Gupta et al. International Journal of Research in Medical Sciences,