Discrepancies Between Direct and Indirect Blood Pressure Measurements
Using Various Recommendations for Arm Cuff Selection
Jeff A. Clark, MD, FAAP; Mary W. Lieh-Lai, MD, FAAP; Ashok Sarnaik, MD, FAAP, FCCM; and Tej K. Mattoo, MD, DCH, FRCP (UK), FAAP
ABSTRACT. Objective. The current recommendation for choosing an appropriate size cuff for measuring blood pressure (BP) is a bladder width to equal 40% of the upper arm circumference (UAC). However, most phy-sicians use the older two-thirds or three-fourths upper arm length (UAL) recommendations to choose a cuff. The aim of this study was to verify the disparity in cuff size by using two-thirds UAL, three-fourths UAL, and 40% UAC criteria for cuff selection and to compare the indi-rectly measured BP by these criteria with diindi-rectly mea-sured radial intra-arterial BP.
Methods. A prospective, cross-sectional, observa-tional study was conducted in 65 hemodynamically sta-ble patients, aged 5 days to 22 years. Direct BP measure-ments were obtained from a radial intra-arterial catheter. Indirect BP measurements were taken from the same arm as the arterial catheter with a mercury sphygmomanom-eter and standard-size arm cuffs. UAL and UAC of each patient were measured, and the 3 cuffs closest to two-thirds and three-fourths UAL and 40% UAC were used. For each cuff, 3 direct and 3 indirect BP measurements were taken. Student t test was used to compare mean systolic and diastolic BP for direct and indirect measure-ments.
Results. A total of 172 observations were recorded, including 56 by two-thirds UAL, 55 by three-fourths UAL, and 61 by 40% UAC criteria. There was no signif-icant difference between the means of the ideal cuff size by 40% UAC criterion and the actual cuffs used from the available standard cuffs. However, because of an un-availability of the larger cuffs for UAL criteria, the actual cuffs used were significantly smaller than ideal. Compar-ison of direct and indirect BP measurements revealed no significant difference in systolic BP when the latter was obtained by 40% UAC criterion. However, the difference in diastolic BP was significant. With available cuffs, a significant difference in systolic as well as diastolic BP was seen with both UAL criteria.
Conclusions. Practitioners are likely to use signifi-cantly larger arm cuffs when following the two-thirds and three-fourths UAL criteria than when following the 40% UAC criterion. Of the 3 criteria for cuff selection, systolic BP by 40% UAC criterion most accurately reflects directly measured radial arterial pressure. However, the
40% UAC cuff significantly overestimates the diastolic pressure. Using available cuffs for indirect measure-ments by two-thirds and three-quarters UAL criteria sig-nificantly underestimates systolic as well as diastolic BP when compared with radial intra-arterial BP.Pediatrics
2002;110:920 –923;blood pressure, measurement, radial ar-tery, cuff size, children.
ABBREVIATIONS. BP, blood pressure; UAL, upper arm length; UAC, upper arm circumference; BMI, body mass index; SBP, systolic blood pressure; DBP, diastolic blood pressure.
B
lood pressure (BP) measurement is an integral part of the physical examination. In 1977, the National Heart, Lung, and Blood Institute Task Force on Blood Pressure Control in Children1de-fined normal BP in children and the proper methods for its measurement. It suggested using a cuff whose width was approximately two thirds of the upper arm length (UAL), from acromion to the tip of the olecranon process, but ultimately recommended us-ing the largest cuff that snugly fit the upper arm without obscuring the antecubital fossa. In 1987, the task force updated its recommendations, stating that the arm cuff should be wide enough to cover three fourths of the UAL.2In 1996, the task force revised its
recommendations, stating that the arm cuff width should equal approximately 40% of the upper arm circumference (UAC).3
Our previous study revealed that 59% of the health care practitioners use two-thirds UAL criterion for arm cuff selection.4The study also revealed that by
using three-fourths UAL criterion, the large adult cuff should be appropriate for a 6-year-old child with UAL at the 25th percentile for age. Using two-thirds UAL as criterion, that same cuff should be appropri-ate for an 8-year-old child. On the contrary, by using 40% UAC criterion, the small adult cuff should be appropriate for an average 16-year-old boy and a 25-year-old woman. These observations demonstrate considerable discrepancies in cuff size when selected by different criteria. The aim of this study was to validate our observations by actual measurement of arm and cuff sizes required by various criteria and to compare indirectly measured BP using two-thirds UAL, three-fourths UAL, and 40% UAC cuff criteria with directly measured intra-arterial BP.
METHODS
A prospective, cross-sectional observational study was con-ducted on patients who were admitted to the pediatric intensive
From the Department of Pediatrics, Children’s Hospital of Michigan, Wayne State University School of Medicine, Detroit, Michigan.
This work was presented in part at the American Society of Nephrology, October 14, 2000, Toronto, Canada; and at the Annual Scientific Meeting of the American Academy of Pediatrics, October 21, 2001, San Francisco, CA. Received for publication Dec 7, 2001; accepted Apr 8, 2002.
Reprint requests to (T.K.M.) Division of Pediatric Nephrology, Children’s Hospital of Michigan, 3901 Beaubien Blvd, Detroit, MI 48201-2196. E-mail: tmattoo@med.wayne.edu
care unit at Children’s Hospital of Michigan. Each patient had an in situ radial artery catheter, which was placed as part of the routine intensive care. Inclusion criteria were age⬎1 day after term delivery, BP variation within 10% of the baseline, and ade-quate peripheral perfusion, which was defined as a peripheral temperature ⱖ32°C and adequate peripheral pulses. Exclusion criteria were morbid obesity (body mass index [BMI]⬎40 kg/m2)
and being on extracorporeal membrane oxygenation or hemodi-alysis. Informed consent was obtained before enrollment. Data were collected on patient age, weight, BMI, height, UAL, and UAC. UAL was defined as the distance from the acromion to the tip of the olecranon, and the UAC was measured at the midpoint of the UAL. Standard disposable arterial pressure transducers and high-pressure transducer tubing (Abbott Critical Care Systems, Chicago, IL) were used, and arterial pressure was recorded from a standard patient monitor (Solar 8000, Marquette Electronics Inc, Milwaukee, WI).
Before pressure measurement, the arterial catheter system was inspected for the presence of air or clots. The quality of the wave form was evaluated for a sharp up-slope and down-slope of the arterial wave form. The natural frequency and damping coeffi-cient of the pressure-monitoring system was evaluated using the standard snap test described by Gardner5and others.6,7All
sys-tems were suitable for pressure measurement. With the patient in the supine position, the entry site of the radial arterial catheter was taken as the 0 reference point. All measurements were obtained with the catheter and the upper arm in the same plane.
Indirect BP measurement was made with a mercury sphygmo-manometer (Omron Healthcare Inc, Vernon Hills, IL). Three arm cuffs that most closely approximated two-thirds UAL, three-fourths UAL, and 40% UAC were used on each patient. These were selected from standard-size cuffs with bladder widths mea-suring 4.5 cm (“newborn”), 6 cm (“infant”), 9 cm (“child”), 12 cm (“adult”), 15 cm (“large adult”), and 18 cm (“thigh”). In the absence of an ideal-size cuff for each criterion, the closest available size, smaller or larger, was used. The BP was measured 3 times using each cuff, with approximately 1 minute between each mea-surement. A direct intra-arterial measurement was taken immedi-ately before each indirect measurement.
Systolic BP (SBP) was taken as Korotkoff sound I, and diastolic BP (DBP) was taken as Korotkoff sound IV. The Institutional Review Board of Wayne State University approved this study.
Statistical Analysis
Sample size calculation was conducted assuming a 7-mm Hg difference in SBP to be clinically significant, with a power of 80% and an ␣ of 0.05. The averages of the 3 systolic and diastolic measurements for both direct and indirect BP were calculated. Blood pressures obtained by indirect measurement were com-pared with intra-arterial BP using the Studentttest.
RESULTS
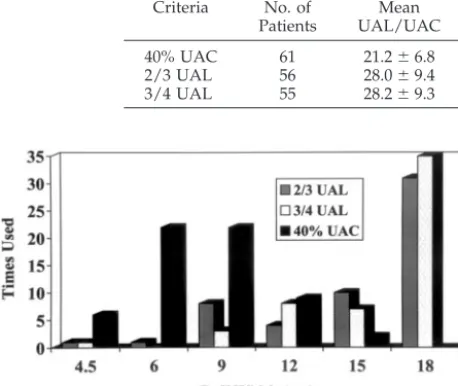
A total of 172 observations were made in 65 pa-tients, aged 5 days to 22 years. Included were 56 measurements by two-thirds UAL criterion, 55 by three-fourths UAL criterion, and 61 by 40% UAC criterion. Fifty-four patients had BP measurements by all 3 criteria. As shown in Table 1, the mean age of the patients was 8.4 (⫾6.5) years, mean weight was 32.8 (⫾24.7) kg, mean UAL was 25.8 (⫾10.3) cm, and mean UAC was 21.0 (⫾6.8) cm.
Table 2 shows the difference between the ideal cuff
size for the patient’s arm using two-thirds UAL, three-fourths UAL, and 40% UAC criteria and the actual cuff size used from our standard repertoire. Using the available cuffs by two-thirds UAL crite-rion, the actual mean cuff size was 15.2⫾3.8 cm, by three-fourths UAL criterion it was 16.0⫾3.2 cm, and by 40% UAC criterion it was 8.1⫾2.7 cm. As shown in Fig 1, by two-thirds UAL and three-fourths UAL criteria, an 18-cm (largest) cuff was used for 28 and 35 measurements, respectively, and it was not used even once by 40% UAC criteria. On the contrary, the 6-cm and 9-cm cuffs were used in 44 of the 61 pa-tients in the 40% UAC group.
The difference between cuff and intra-arterial BP measurements for each of the 3 methods is shown in Table 3. SBP measured by the intra-arterial catheter was similar to that measured using the 40% UAC cuff (P ⫽ .75). Using the available cuffs, the SBP measured by either the two-thirds UAL cuff or the three-fourths UAL cuff significantly underestimated intra-arterial SBP (P⬍.01). These findings were con-sistent throughout the age and size ranges. When comparing DBP, all 3 cuffs showed significant differ-ences from intra-arterial measurements. The 40% UAC cuff significantly overestimated DBP (P⬍.01), whereas both the two-thirds UAL cuff and the three-fourths UAL cuff underestimated DBP (Pⱕ .02). As with SBP, these differences were similar throughout the age and size distribution.
DISCUSSION
The measurement of BP in children is influenced by many factors, including the level of anxiety, state of muscle relaxation, position of the arm in relation to the heart, type of manometer, and size of the arm cuff.8The selection of a proper-size arm cuff is
im-portant because it is widely known that a smaller cuff gives a falsely high BP reading and a larger cuff gives a falsely low reading, the margin of error being smaller with a larger cuff.9 –11This issue is of
partic-ular importance in children because of age-depen-dent differences in arm size.
Our previous study revealed that a majority of health care providers do not follow the published guidelines for arm cuff selection.4The problem is not
confined only to children. In a recent editorial in Blood Pressure Monitoring, Alpert12said, “From
prac-tical experience, I would estimate that improper cuffs are used at least 30% to 50% of the time.” In a study from Great Britain, Wingfield et al13 reported that
only 27% of doctors and 32% of nurses correctly estimated the appropriate coverage of the arm with a BP cuff as per the published British guidelines.
TABLE 1. Anthropometric Data
Age Range n Mean Age
(Years) Mean Weight (kg) Mean Height (cm) Mean BMI (kg/m2)
Mean UAL (cm)
Mean UAC (cm)
⬍1 mo 6 2.5⫾1 wk 3.2⫾0.4 45⫾5 17.0⫾4.9 9.9⫾1.2 10.8⫾1.2
1 mo–4 y 18 1.7⫾1.3 11.6⫾5.7 80⫾21 17.7⫾3.5 15.9⫾3.8 16.5⫾2.7
5 y–9 y 12 7.2⫾1.6 24.2⫾7.3 122⫾14 16.3⫾1.5 25.8⫾2.4 18.5⫾3.0
10 y–14 y 17 12.8⫾1.2 49.5⫾17.7 155⫾15 20.4⫾5.4 33.5⫾5.5 25.8⫾4.8 ⬎14 y 12 17.5⫾2.3 64.5⫾13.4 166⫾10 24.3⫾6.6 37.6⫾3.0 28.5⫾4.3
Total 65 8.4⫾6.5 32.8⫾24.7 120⫾44 19.3⫾5.3 25.8⫾10.3 21⫾6.8
ARTICLES 921
at Viet Nam:AAP Sponsored on August 30, 2020
www.aappublications.org/news
The problem regarding arm cuff selection relates both to the lack of knowledge among health care providers on the current recommendations and to the recommendations themselves. Our study re-vealed that for UAL criteria, we used mostly larger arm cuffs. Of 111 measurements by two-thirds UAL and three-fourths UAL criteria, 95 (86%) required a 12-cm or larger cuff. Included were 66 (59%) subjects who needed the 18-cm (largest) large adult cuff. The mean ideal cuff size by two-thirds UAL and three-fourths UAL criteria were 18.7 cm and 21.2 cm, re-spectively. The results were very different when 40% UAC criterion was used. Of the 61 patients on whom this criterion was used, 50 (80%) required a cuff 9 cm or smaller, and the mean ideal cuff size was 8.5 cm. None of these patients needed the 18-cm cuff. Using two-thirds UAL as criterion, the mean age of patients who required the 18-cm cuff was 9 years, and using three-fourths UAL as criterion, the mean age of pa-tients who required the 18-cm cuff was 8 years. How-ever, using 40% UAC criterion, no patients required the 18-cm cuff. This confirms our previous observa-tion that for UAL criteria we need to use larger cuffs and for 40% UAC criterion we need to use smaller arm cuffs than those commonly used by practitio-ners.4
Our study revealed that for the UAL criteria, a significant difference exists between the ideal and the actual cuff sizes that were used for BP measure-ment; the actual cuffs were significantly smaller than ideal. This is attributable perhaps to a limitation of choice beyond the large adult cuff. On the contrary,
the difference was not significant when 40% UAC criterion was used. This was a result of greater choice among smaller cuffs, which allowed selection of a cuff very close to the ideal size. The anthropometric data in our patients, including gender distribution, age, BMI, UAL, and UAC, were within the normal range for healthy children.14,15
Our study also revealed that arm cuffs by two-thirds and three-fourths UAL criteria give signifi-cantly lower SBP when compared with directly mea-sured radial arterial pressure. The difference is not significant when 40% UAC criterion is used for cuff selection. For DBP, the UAL cuffs significantly un-derestimated radial artery DBP, whereas the UAC cuff significantly overestimated radial artery DBP. These observations indicate that by using the current task force cuff size recommendation of 40% UAC, the indirectly measured BP matches intra-arterial SBP but not the DBP.
The mean SBP and DBP measured by larger cuffs using UAL criteria were, as expected, lower than the directly measured intra-arterial BP. For two-thirds UAL criterion, the mean difference was 14.7 mm Hg for SBP and 5.6 mm Hg for DBP. For three-fourths UAL criterion, the respective numbers were 16.5 mm Hg and 6.6 mm Hg. On the contrary, the use of smaller cuffs by 40% criterion gave higher mean SBP as well as DBP (1.2 mm Hg and 7.1 mm Hg, respec-tively). The margin of error was much lower when 40% UAC criterion was used.
Rastam et al16 reported that as arm cuff size
in-creases, BP decreases until the cuff width is approx-imately equal to 40% of the UAC. However, to our knowledge, this observation has not been examined in children. In a recent study in adult intensive care unit patients, Marks and Groch17 compared
indi-rectly measured BP using cuff widths of 30% to 55% UAC to radial intra-arterial BP in the contralateral arm. They found that there was not a single cuff width/arm circumference ratio that was optimum in all patients. As arm circumference increased, the op-timum ratio decreased. For the group as a whole, a cuff width/arm circumference ratio of 46% produced no error when comparing intra-arterial and cuff SBP. On the basis of extrapolation, they determined that a cuff width/arm circumference ratio of 74% would produce no error when comparing intra-arterial to
TABLE 3. Indirect Versus Direct BP Measurements
Criteria No. of Patients
Mean Cuff SBP (mm Hg)
Mean Direct SBP
(mm Hg)
SBP Difference
(mm Hg)
P Mean
Cuff DBP (mm Hg)
Mean Direct DBP
(mm Hg)
DBP Difference
(mm Hg) P
40% UAC 61 114⫾18 115⫾22 ⫺1⫾12 .75 69⫾16 62⫾12 7⫾12 ⬍.01
2/3 UAL 56 103⫾16 118⫾19 ⫺15⫾11 ⬍.01 58⫾13 64⫾11 ⫺6⫾13 .02
3/4 UAL 55 102⫾17 119⫾19 ⫺17⫾12 ⬍.01 58⫾14 65⫾11 ⫺7⫾12 ⬍.01
TABLE 2. Mean Ideal Versus Mean Actual Cuffs Used for BP Measurement
Criteria No. of Patients
Mean UAL/UAC
Mean Ideal BP Cuff Size (cm)
Mean Actual BP Cuff Size (cm)
P
40% UAC 61 21.2⫾6.8 8.5⫾2.7 8.1⫾2.7 .5
2/3 UAL 56 28.0⫾9.4 18.7⫾6.3 15.2⫾3.8 ⬍.001
3/4 UAL 55 28.2⫾9.3 21.2⫾7.0 16.0⫾3.2 ⬍.0001
cuff DBP. Our findings that a larger cuff than 40% UAC is necessary for accurate measurement of DBP is in agreement with these results.
Direct measurement of BP by radial artery cannu-lation is a standard practice in the intensive care setting. The radial artery is preferred because of its well-developed collateral circulation, safety, and ease of access. However, the pressure measured may not be an accurate representation of brachial artery pressure. As the arterial pulse wave form travels distally from the aortic valve, SBP is exaggerated relative to more proximal arteries because of incident and reflected wave amplification and because of a decrease in overall compliance in the smaller arteries compared with the aorta.18 –20A number of adult and
animal studies have shown that radial SBP is higher than aortic SBP, but mean BP and DBP are simi-lar.18 –21 No study has been done to determine
whether it is any different in children who have a normal vascular tone, and what, if any, the degree of increase in BP is from brachial to radial arteries is not known.
CONCLUSION
The current repertoire of commercially available arm cuffs is inadequate when using UAL as cuff selection criteria. Larger arm cuffs are required for BP measurement by UAL criteria and smaller cuffs are required for BP measurement by UAC criterion. Furthermore, indirect BP measurement by the cur-rent task force recommendation of 40% UAC is com-parable only to systolic and not diastolic radial artery pressure. It is not clear whether additional cuffs sizes or alternative selection criteria would yield a single cuff that is accurate for measuring SBP as well as DBP.
REFERENCES
1. Blumenthal S, Epps RP, Heavenrich R, et al. Report of the task force on blood pressure control in children.Pediatrics. 1977;59:797– 820
2. Task Force on Blood Pressure Control in Children, National Heart Lung and Blood Institute (NHLBI). Report of the second task force on blood pressure control in children.Pediatrics. 1987;79:1–25
3. National High Blood Pressure Education Program (NHBPEP) Working Group on Hypertension Control in Children and Adolescents. Update on the 1987 task force report on high blood pressure in children and adolescents.Pediatrics. 1996;88:649 – 658
4. Arafat M, Mattoo TK. Measurement of blood pressure in children: recommendations and perception on cuff selection. Pediatrics. 1999; 104(3). Available at: www.pediatrics.org/cgi/content/full/104/3/e30 5. Gardner RM. Direct blood pressure measurement: dynamic response
requirements.Anesthesiology. 1981;54:227–236
6. Kleinman B, Powell S, Kumar P, Gardner RM. The fast flush test measures the dynamic response of the entire blood pressure monitoring system.Anesthesiology. 1992;77:1215–1220
7. Heimann PA, Murray WB. Construction and use of catheter manometer systems.J Clin Monit.1993;9:45–53
8. Bailey RH, Bauer JH. A review of common errors in the indirect mea-surement of blood pressure.Arch Intern Med.1993;153:2741–2748 9. Lum LG, Jones MD. The effect of cuff width on systolic blood pressure
measurements in neonates.Pediatrics. 1977;91:963–966
10. Whincup PH, Cook DG, Shaper AG. Blood pressure measurements in children: the importance of cuff bladder size. J Hypertens. 1989;7: 845– 850
11. Gilman MW, Cook NR. Blood pressure measurement in childhood epidemiologic studies.Circulation. 1995;92:1049 –1057
12. Alpert BS. Cuff width and accuracy of the measurement of blood pressure.Blood Press Monit.2000;5:151–152
13. Wingfield D, Pierce M, Feher M. Blood pressure measurement in the community: do guidelines help.J Hum Hypertens.1996;10:805– 809 14. Hall JG, Froster-Iskenius U, Allanson J.Handbook of Normal Physical
Measurements. Oxford, England: Oxford University Press; 1995:229 –231, 271–276
15. Snyder RG, Spencer ML, Owings CL, Schneider LW.Physical Character-istics of Children as Related to Death and Injury for Consumer Product Safety Design. Washington, DC: National Institutes of Health; 1975 16. Rastam L, Prineas RJ, Gomez-Marin O. Ratio of cuff width-arm
circum-ference as a determinant of arterial blood pressure measurements in adults.J Intern Med.1990;227:225–232
17. Marks LA, Groch A. Optimizing cuff width for noninvasive measure-ment of blood pressure.Blood Press Monit.2000;5:153–158
18. Pauca AL, Wallenhautt SL, Kon ND, Tucker WY. Does radial artery pressure accurately reflect aortic pressure?Chest. 1992;102:1193–1198 19. O’Rourke MF. What is blood pressure?Am J Hypertens.1990;3:803– 810 20. Carroll GC. Blood pressure monitoring.Crit Care Clin.1988;4:411– 434 21. Bazaral MG, Welch M, Golding LAR, Badhwar K. Comparison of
bra-chial and radial arterial pressure monitoring in patients undergoing coronary artery bypass surgery.Anesthesiology. 1990;73:38 – 45
COPING WITH UNCERTAINTY
“Medicine’s ground state is uncertainty. And wisdom for both patients and doctors is defined by how one copes with it.”
Gawande A.Complications A Surgeon’s Notes on an Imperfect Science. Metropolitan Books; 2002
Submitted by Student
ARTICLES 923
at Viet Nam:AAP Sponsored on August 30, 2020
www.aappublications.org/news
DOI: 10.1542/peds.110.5.920
2002;110;920
Pediatrics
Jeff A. Clark, Mary W. Lieh-Lai, Ashok Sarnaik and Tej K. Mattoo
Various Recommendations for Arm Cuff Selection
Discrepancies Between Direct and Indirect Blood Pressure Measurements Using
Services
Updated Information &
http://pediatrics.aappublications.org/content/110/5/920
including high resolution figures, can be found at:
References
http://pediatrics.aappublications.org/content/110/5/920#BIBL
This article cites 18 articles, 2 of which you can access for free at:
Subspecialty Collections
http://www.aappublications.org/cgi/collection/standard_of_care_sub
Standard of Care
_management_sub
http://www.aappublications.org/cgi/collection/administration:practice
Administration/Practice Management
following collection(s):
This article, along with others on similar topics, appears in the
Permissions & Licensing
http://www.aappublications.org/site/misc/Permissions.xhtml
in its entirety can be found online at:
Information about reproducing this article in parts (figures, tables) or
Reprints
http://www.aappublications.org/site/misc/reprints.xhtml
DOI: 10.1542/peds.110.5.920
2002;110;920
Pediatrics
Jeff A. Clark, Mary W. Lieh-Lai, Ashok Sarnaik and Tej K. Mattoo
Various Recommendations for Arm Cuff Selection
Discrepancies Between Direct and Indirect Blood Pressure Measurements Using
http://pediatrics.aappublications.org/content/110/5/920
located on the World Wide Web at:
The online version of this article, along with updated information and services, is
by the American Academy of Pediatrics. All rights reserved. Print ISSN: 1073-0397.
the American Academy of Pediatrics, 345 Park Avenue, Itasca, Illinois, 60143. Copyright © 2002 has been published continuously since 1948. Pediatrics is owned, published, and trademarked by Pediatrics is the official journal of the American Academy of Pediatrics. A monthly publication, it
at Viet Nam:AAP Sponsored on August 30, 2020
www.aappublications.org/news