90 Int J Res Med. 2015; 4(4)90-95 e ISSN:2320-2742 p ISSN: 2320-2734
Surgical site infections in abdominal surgeries (surgeons nightmare) : a
prospective study
Kota Sreedhar Rao 1*, Khant shahil Rameshbhai2, Perugu Venkateshwar3
1
M.S. Professor and former Hod,Upgraded department of general surgery, Osmania medical collage,Osmania general hospital, Hyderabad , Telangana. 2 M..S. DNB Urology Resident, Department of urology and advanced urodynamic centre , Ruby Hall Clinic , Pune , Maharashtra , 3 M.S. M Ch ( Pediatric surgery ) , 4Associate professor, Upgraded department of general surgery, Osmania medical collage, Osmania general hospital,Hyderabad, Telangana.
INTRODUCTION
Infections that occur in the wound created by an invasive surgical procedure are generally referred to as surgical site infections (SSIs). SSIs are one of the most important causes of healthcare – associated infections (HCAIs),
*Author for correspondence Dr kota Seedhar Rao
Plot no 60 road no 3,Srk puram, Saroor nagar post,
Hyderabad 500035 drsrkota@gmail.com
second only to urinary tract infections (UTI) in incidence. A prevalence survey suggested that approximately 8% of patients in hospital in the UK have HCAI. SSIs accounted for 14% of these infections and nearly 5% of patients who had undergone a surgical procedure were found to have developed an SSI.1 SSI develops in at least 5 % of hospitalised patients undergoing an operative procedure in developed countries, raising the costs of healthcare both to the public
ORIGINAL ARTICLE
ABSTRACT
BACKGROUND: Surgical site infections (ssi) are the third most commonly reported nosocomial infection and they account for approximately a quarter of all nosocomial infections. It has an adverse impact on the hospital as well as on the patient. It is responsible for increasing length of stay of patient which results in social and economic loss to the patients and family. Host factors, wound factors and surgery related factors are implicated in the causation of ssi.
AIMS AND OBJECTIVES: 1) To study the incidence of ssi in our hospital.2)To study the risk factors of ssi in our
hospital.3)To identify any change in the bacteriology of ssi .MATERIALS AND METHODS: 450 operated cases in
surgery were included in this study. Certain risk factors like – type of surgical wound, elective or emergency surgery, antibiotic prophylaxis, duration of surgery, presence or absence of drain and any underlying or predisposing conditions were noted. Swabs were obtained from the post operative infected wounds and processed by the conventional microbiological methods. Antimicrobial susceptibility testing was done by kirby-bauer disc diffusion method and interpretation was done according to clsi guidelines.Statistical analysis was done by applying student t- test and the
chi – square test of significance. RESULTS: The incidence of ssis following laparotomies is 22.2%. .emergency
laparotomies were statistically more likely to develop ssi than elective laparotomies.a large share of abdominal ssis was occupied by surgeries with clean-contaminated wounds, which is similar to other studies. It reflects the higher proportion of such cases in laparotomies.diabetes mellitus was the most common co-morbidity encountered.increase in age, smoking , diabetes mellitus, obesity, hb < 10 gm %, copd, cancer , hiv/aids,asa grade,duratio of surgery > 2hrs,wound irrigation with saline,pre op stay > 5 days were the risk factors identified. The most common organism implicated in the development of abdominal ssi was mrsa, which is different
from that noted in literature. CONCLUSION: Increased awareness among hospital staff with regard to
infection control and strict adherence to the aseptic precautions is the need of the hour. The high rate of ssi with relative preponderance of mrsa strain calls for intensive infection control practices and routine surveillance of ssi in all hospital.
91 Int J Res Med. 2015; 4(4)90-95 e ISSN:2320-2742 p ISSN: 2320-2734 and the healthcare delivery system.
According to a report by the International Nosocomial Infection Control Consortium (INICC) in 2012, overall 1.4 million people worldwide were suffering from nosocomial infections, and in India alone, the rate was over 25 per cent, with SSI occupying a significant share. The incidence is likely underestimated because of inadequate surveillance and incomplete post-discharge data. Extensive surveys have shown that SSIs are associated with considerable morbidity and it has been reported that over one - third of postoperative deaths are
related, at least in part, to SSIs.2 SSI can
range from a fairly minor wound discharge with no other complications to a life- threatening condition. Other outcomes include poor scars that are cosmetically unacceptable and cause psychological
stress.3 SSI is, in most scenarios, a
preventable HCAI, that can double the length of hospital stay and thereby increase the costs of healthcare, attributable to re-operation, extra nursing care and interventions, and drug treatment costs. There are, in addition, indirect costs due to loss of productivity, patient dissatisfaction
and litigation, and reduced quality of life.4,5
Abdominal surgical site infections are among the most common infectious complications in hospitalised patients and are associated with serious consequences for outcomes and costs. They account for up to 14 % of SSIs in studies conducted in developing countries, where there is no organised surveillance system to describe routine nosocomial infections. The present study aims to determine the frequency of surgical site infections in patients undergoing various abdominal surgical procedures, the associated risk factors, the organisms implicated and their sensitivity patterns, and the outcomes observed after treatment among inpatients in the general surgical wards.
MATERIALS AND METHODS
Study Design : Clinico-bacteriological
follow-up of 450 post-operative cases of abdominal surgeries to the development of SSI, as per the
CDC criteria (1991). Incidence was expressed as the infection rate per 100 operations. Antibiotic sensitivity testing was done using the disc diffusion method.
Method of collection of data :Details of the patients who developed SSI following abdominal surgeries were recorded in a proforma which included relevant information with regard to history, clinical examination and perioperative management. Data regarding the organisms isolated and their sensitivity patterns were included.
Statistical Significance :Statistical significance of the various parameters affecting SSI were being tested using CHI SQUARE TEST ( p < 0.05 ) .
Inclusion criteria : 1. Patients who
underwent abdominal surgeries.
Exclusion criteria :1.Superficial abdominal
surgeries like lipoma. 2.Previous laparotomies.
3. Laproscopic surgeries. RESULTS
Incidence of SSI in our study is 22.2 % ( 100 out of 450 patients).Incidence in emergency surgery is 28.57 % .Incidence in elective surgery is 16.6%.
Risk factors which are associated in our study are increase in age(Table 1), smoking (Table 2) , alcohol ( Table 3) pre operative ASA Score (Table 4).Diabetes mellitus, obesity, hb < 10 gm %, COPD ( Table 5).Cancer , hiv/aids (Table 6),Duration of surgery > 2hrs,wound irrigation with saline,pre op stay > 5 days (Table 7).Most common surgery to get SSI is operation for late intestinal perforation (48.27 %) .Most common associated co morbidity with SSI is diabetes mellitus (46.6%). Among types of wound dirty infected wound have maximum incidence (35.4 %)(Table 8). 65 % are superficial incisional SSI, 22 % are deep incisional SSI and 13 % are organ space SSI.(Table 9). The most commonly implicated organism in this study was
MRSA (Methicillin Resistant Staphylococcus Aureus), accounting for 25 % of the cases of
SSI, followed by E.Coli and Klebsiella
species, each of which accounted 23% and 18% respectively . Other commonly
encountered organisms were Proteus species
92 Int J Res Med. 2015; 4(4)90-95 e ISSN:2320-2742 p ISSN: 2320-2734
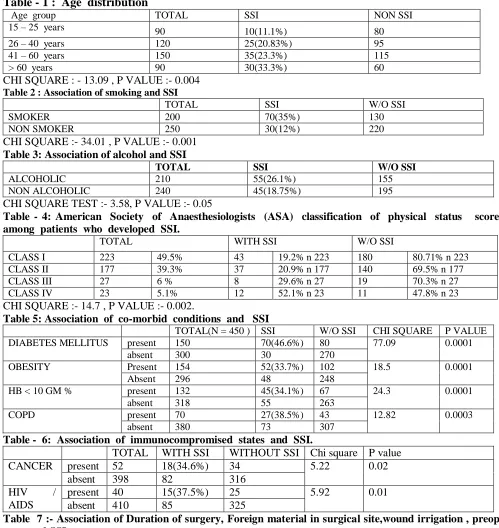
Table - 1 : Age distribution
Age group TOTAL SSI NON SSI
15 – 25 years 90 10(11.1%) 80
26 – 40 years 120 25(20.83%) 95
41 – 60 years 150 35(23.3%) 115
> 60 years 90 30(33.3%) 60
CHI SQUARE : - 13.09 , P VALUE :- 0.004
Table 2 : Association of smoking and SSI
TOTAL SSI W/O SSI
SMOKER 200 70(35%) 130
NON SMOKER 250 30(12%) 220
CHI SQUARE :- 34.01 , P VALUE :- 0.001
Table 3: Association of alcohol and SSI
TOTAL SSI W/O SSI
ALCOHOLIC 210 55(26.1%) 155
NON ALCOHOLIC 240 45(18.75%) 195
CHI SQUARE TEST :- 3.58, P VALUE :- 0.05
Table - 4: American Society of Anaesthesiologists (ASA) classification of physical status score among patients who developed SSI.
TOTAL WITH SSI W/O SSI
CLASS I 223 49.5% 43 19.2% n 223 180 80.71% n 223
CLASS II 177 39.3% 37 20.9% n 177 140 69.5% n 177
CLASS III 27 6 % 8 29.6% n 27 19 70.3% n 27
CLASS IV 23 5.1% 12 52.1% n 23 11 47.8% n 23
CHI SQUARE :- 14.7 , P VALUE :- 0.002.
Table 5: Association of co-morbid conditions and SSI
TOTAL(N = 450 ) SSI W/O SSI CHI SQUARE P VALUE
DIABETES MELLITUS present 150 70(46.6%) 80 77.09 0.0001
absent 300 30 270
OBESITY Present 154 52(33.7%) 102 18.5 0.0001
Absent 296 48 248
HB < 10 GM % present 132 45(34.1%) 67 24.3 0.0001
absent 318 55 263
COPD present 70 27(38.5%) 43 12.82 0.0003
absent 380 73 307
Table - 6: Association of immunocompromised states and SSI.
TOTAL WITH SSI WITHOUT SSI Chi square P value CANCER present 52 18(34.6%) 34 5.22 0.02
absent 398 82 316 HIV /
AIDS
present 40 15(37.5%) 25 5.92 0.01 absent 410 85 325
Table 7 :- Association of Duration of surgery, Foreign material in surgical site,wound irrigation , preop stay and SSI.
Factor Total SSI W/O SSI CHI SQUARE P VALUE
Prophylactic antibiotic Given 450 100 (22.2%) 350
Duration of surgery < 2 hours 224 41(18.3%) 183 3.96 0.04
> 2 hours 226 59(26.1%) 167
Foreign material in
surgical site
Suture only 207 47(22.7%) 160 0.05 0.8
Suture + Drain 243 53(21.8) 190
Wound irrigation Povodine Iodine 274 37 (13.5%) 237 30.8 0.0001
Saline 176 63 (35.7%) 113
Pre op stay < 5 days 130 14 (10.7%) 116 7.1 0.007
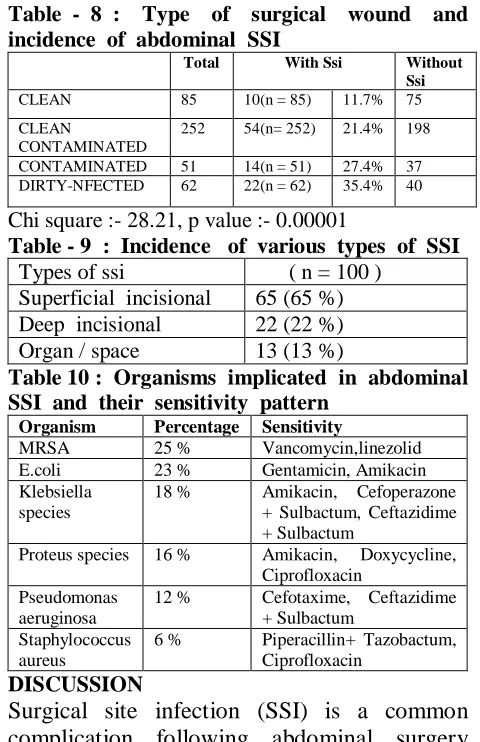
93 Int J Res Med. 2015; 4(4)90-95 e ISSN:2320-2742 p ISSN: 2320-2734 Table - 8 : Type of surgical wound and
incidence of abdominal SSI
Total With Ssi Without
Ssi
CLEAN 85 10(n = 85) 11.7% 75
CLEAN
CONTAMINATED
252 54(n= 252) 21.4% 198
CONTAMINATED 51 14(n = 51) 27.4% 37 DIRTY-NFECTED 62 22(n = 62) 35.4% 40
Chi square :- 28.21, p value :- 0.00001
Table - 9 : Incidence of various types of SSI
Types of ssi ( n = 100 ) Superficial incisional 65 (65 %) Deep incisional 22 (22 %) Organ / space 13 (13 %)
Table 10 : Organisms implicated in abdominal SSI and their sensitivity pattern
Organism Percentage Sensitivity
MRSA 25 % Vancomycin,linezolid
E.coli 23 % Gentamicin, Amikacin
Klebsiella species
18 % Amikacin, Cefoperazone
+ Sulbactum, Ceftazidime + Sulbactum
Proteus species 16 % Amikacin, Doxycycline,
Ciprofloxacin Pseudomonas
aeruginosa
12 % Cefotaxime, Ceftazidime
+ Sulbactum Staphylococcus
aureus
6 % Piperacillin+ Tazobactum,
Ciprofloxacin
DISCUSSION
Surgical site infection (SSI) is a common complication following abdominal surgery and is the third most frequent health-care associated infection, accounting for serious consequences in terms of morbidity and increased health-care costs. The overall incidence of SSI for all surgeries performed in this study was 22.2 %. Different studies from various parts of India have shown rates ranging from 6.09 to 38.7 %, with the majority of studies having a rate of 14 – 17 %, hence the rate of SSI for all surgeries in the present study was slightly higher than that seen in most other hospitals in India. In similar studies conducted in other developing countries, one in Kosovo and another in Iran, the incidence of abdominal SSI was 12 % and 17 % respectively. Hence the incidence of abdominal SSI was slightly higher than that of other developing countries, but much higher than that observed in developed countries like United Kingdom (3.1%) and the Netherlands (4.3%). The most common age group developing
SSI was > 60 years,for both males and females. Most studies in literature show an increase in the incidence of SSI with
increasing age6, probably reflecting the
deteriorating immune status and
development of co-morbidities as age advances. SSI rates among males is 24% and among females is 20%.There is no statistical significance different of SSI among males and females. Among the patient-related risk factors observed in this study, incidence of SSI among smokers is 35% and among non smokers is 12 % with statistically significance
difference7.The incidence of SSI among
alcoholics is 26.19% and among non alcoholics is 18.75% with no statistical significance difference. The most common co-morbidity was Diabetes Mellitus,the rate of SSI among diabetics is 46.6% and among non diabetics is 10% which is statistical significance difference. The other risk factors which were included were Obesity,Hb < 10 gm%, COPD all of which showed statistical significance SSI rates.The two immunocompromised states included in the studies was cancer and hiv/aids which both showed statistical signifante higher
rates of SSI8-10 . Incidence of SSI increases
with an increase of the ASA score, but in the present study, majority of the patients had an ASA score of I and II, which was probably due to the fact that most of the patients with ASA score III or IV were either not taken up for surgery .
Of the 450 patients studied, 240 underwent elective laparotomies and 210 underwent emergency laparotomies. The incidence for SSI was 16.6 % for elective laparotomies and 28.57 % for emergency abdominal surgeries, which shows that emergency laparotomies were statistically far more likely to develop SSI than elective procedures (p value < 0.0001). This is in conformity with another study conducted at an Indian teaching hospital by Mahesh C B
94 Int J Res Med. 2015; 4(4)90-95 e ISSN:2320-2742 p ISSN: 2320-2734 the greater frequency of contaminated or
dirty wounds in emergency surgeries. 56 %(252 out of 450) of laparotomies were classified by the CDC wound classification system as clean-contaminated. These cases accounted for 54 %(54 out of 100) of SSI in this study. This may be due to the fact that a high proportion of laparotomies is occupied by clean-contaminated cases. Most common surgery to be infected are laparotomy for late intestinal perforation (48.27%), open cholecystectomy (48%), open appendicectomy (44.7 %).Incidence of SSI for these surgeries was far higher than any noted in literature. This was probably due to the associated co-morbidities that rendered patients unfit for laparoscopic cholecystectomy and the late presentation of patients with duodenal ulcer perforation in these parts, which converts a contaminated wound to a dirty wound, thus increasing the risk of SSI. A review of literature suggests that the risk of infection increases when the duration of surgery exceeds 2 hours, although the type of surgery may vary. Use of drain to reduce the incidence of SSI rates is not recommended as there is no statistical significant difference in reduction of SSI rate with use of drain. Wound irrigation was regularly practised for wounds with a greater risk of contamination, which
theoretically reduces the risk of SSI11-13.
Antibiotic prophylaxis was received by all the cases studied, which has consistently proven to reduce SSI rates in various studies world-wide. The most critical factors in the prevention of postoperative infections, the sound judgement and proper technique of the surgeon and surgical team, were difficult to quantify in this study. The most common organism implicated in this study
was MRSA. The Gram-negative organisms
implicated were found to be most sensitive to the aminoglycosides Amikacin or Gentamicin, followed by third generation cephalosporins and penicillins with or without beta-lactamase inhibitors, macrolides like Roxithromycin, quinolones like ofloxacin and to tetracycline and
doxycycline. Drug resistance to the regularly prescribed empiric antibiotics, Ciprofloxacin and Cefotaxime was encountered during initial as well as persistent infection, reflecting the need to re-analyse and design a new empiric antibiotic regimen effective against the resident flora of the hospital. Resistance of enteric organisms to Ciprofloxacin is in conformity with reports of increasing resistance to this drug as reported by
Chand Wattal et al in a study conducted in
a tertiary hospital at New Delhi.Despite the many technological advances, surgical site infections are still persisting. The old adage, “prevention is better than cure” holds true in this respect. A conscious effort at asepsis, in the form of a proper infection control programme, can take us a long way in the fight against infections.
CONCLUSION
Increased awareness among hospital staff with regard to infection control and strict adherence to the aseptic precautions is the need of the hour. The incidence of SSI in our hospital is slightly higher when compared to other studies done in developing countries. The high rate of SSI with relative preponderance of MRSA strain calls for intensive infection control practices and routine surveillance of SSI in all hospital.
REFERENCES
1. Smyth ET, McIlvenny G, Enstone JE, et al.
Four Country Healthcare Associated
Infection Prevalence Survey 2006:
overview of the results. Journal of Hospital
Infection 2008;69:230–48.
2. Astagneau P, Rioux C, Golliot F, et al.
Morbidity and mortality associated with surgical site infections: results from the
1997–1999 INCISO surveillance. Journal
of Hospital Infection 2001;48:267–74.
3. Bayat A, McGrouther DA, Ferguson MW.
Skin scarring. British Medical Journal
2003;326:88–92.
4. Coello R, Charlett A, Wilson J, et al.
Adverse impact of surgical site infections in
English hospitals. Journal of Hospital
95 Int J Res Med. 2015; 4(4)90-95 e ISSN:2320-2742 p ISSN: 2320-2734
5. Plowman R, Graves N, Griffin MA, et al.
The rate and cost of hospital-acquired infections occurring in patients admitted to selected specialties of a district general hospital in England and the national burden
imposed. Journal of Hospital Infection
2001;47:198–209.
6. Kaye KS, Schmit K, Pieper C, et al. The
effect of increasing age on the risk of
surgical site infection. Journal of Infectious
Diseases 2005;191:1056–62.
7. Gravante G, Araco A, Sorge R, et al.
Postoperative wound infections after breast reductions: The role of smoking and the
amount of tissue removed. Aesthetic Plastic
Surgery 2008;32:25–31.
8. Neumayer L, Hosokawa P, Itani K, et al.
Multivariable predictors of postoperative surgical site infection after general and vascular surgery: results from the patient
safety in surgery study. Journal of the
American College of Surgeons
2007;204:1178–87.
9. Scott JD, Forrest A, Feurstein S, et al.
Factors associated with postoperative
infection. Infection Control and Hospital
Epidemiology 2001;22:347–51.
10.Cruse PJ, Foord R. A five-year prospective
study of 23,649 surgical wounds. Archives
of Surgery 1973;107:206–10.
11.Sindelar WF, Mason GR. Irrigation of
subcutaneous tissue with povidone-iodine solution for prevention of surgical wound
infections. Surgery, Gynecology and
Obstetrics 1979;148:227–31.
12.Harihara Y, Konishi T, Kobayashi H, et al.
Effects of applying povidone-iodine just
before skin closure. Dermatology 2006;212
Suppl 1:53–7.
13.Gray JG, Lee MJ. The effect of topical
povidone iodine on wound infection
following abdominal surgery. British