169
Chapter 6
Accounts Receivable (A/R)
Management
T
he objective of this chapter is to provide an overview ofpatient account transactions and accounts receivable management. Hospitals provide services to patients for treatment of conditions utilizing highly specialized equip-ment and personnel. It is critical for hospitals to maintain an efficient cash flow by obtaining timely compensation for resources utilized in order to provide services in the hospital environment. Claim forms and patient statements are prepared to bill for services rendered on an outpatient and inpatient basis. Once the claim is submitted or patient statement is sent, the hospital must monitor outstanding accounts to ensure that payment is received within an appropriate time frame. This function is critical to maintaining a positive cash flow for the hospital. This chapter provides a brief overview of the life cycle of a hospital claim. A discussion of the payer’s review of a claim and the remittance advice will provide an understanding of communications from the payer regarding a claim. Payer determinations are reviewed to provide an overview of issues handled by the Patient Financial Services and the Credit and Collection Departments. The chapter will close with a discussion of accounts receivable follow-up and the appeals process to provide a greater understanding of aspects involved in managing accounts receivable.
Chapter Objectives
■ Define terms, phrases, abbreviations, and acronyms related to patient account transactions and accounts receivable follow-up.
■ Demonstrate an understanding of the life cycle of a hospital claim.
■ Discuss elements related to patient transactions. ■ Provide an overview of key information found on an explanation of benefits or remittance advice.
■ List common reasons for claim denials and delays. ■ Demonstrate an understanding of A/R management. ■ Provide an overview of the purpose and function of an accounts receivable report.
■ Describe the process of monitoring and follow-up of outstanding accounts.
■ Demonstrate an understanding of the appeals process.
Outline
LIFE CYCLE OF A HOSPITAL CLAIM HOSPITAL BILLING PROCESS
Insurance Claims and Patient Statements Third-Party Payer (TPP) Claim Processing Remittance Advice (RA)
PATIENT TRANSACTIONS
Patient Payments
Third-Party Payer Payments Adjustments
Balance Billing Secondary Billing
ACCOUNTS RECEIVABLE (A/R) MANAGEMENT
Accounts Receivable Reports Accounts Receivable Procedures
LOST, REJECTED, DENIED, AND PENDED CLAIMS
Lost Claim Rejected Claim Denied Claim Pended Claim
COLLECTION ACTIVITIES
Prioritizing Collection Activities
Patient and Third-Party Follow-up Procedures Uncollectible Patient Accounts
Insurance Commissioner Inquiries
CREDIT AND COLLECTION LAWS
Statute Of Limitations Fair Credit Billing Act
Fair Debt Collection Practices Act
OUTSTANDING PATIENT ACCOUNTS
Patient Statements Patient Phone Contact Collection Letters
OUTSTANDING THIRD-PARTY CLAIMS
Prompt Pay Statutes
Insurance Telephone Claim Inquiry Insurance Computer Claim Inquiry Insurance Claim Tracer
THE APPEALS PROCESS
Claim Determinations That Can Be Appealed Who Can Request an Appeal
Time Requirement for Appeal Submission Levels of Appeals
LIFE CYCLE OF A HOSPITAL CLAIM
The life cycle of a hospital claim begins when the patient arrives at the hospital for diagnosis and treat-ment of a condition(s) and ends when the claim is paid, as illustrated in Figure 6-1. As discussed in previous chapters, the Admissions Department is responsible for obtaining required demographic, financial, and insurnce information from the patient. Another function that is equally important is obtaining appropriate referrals and authorizations. Information obtained by the Admissions Department is entered into the computer on the patient’s account. Patient care services are rendered and docu-mented by various departments within the hospital, and charges are generated. Most charges are posted at the department level through the chargemaster during the patient stay (Figure 6-2). Charges posted through the chargemaster are automatically dropped to the claim and submitted after the patient is discharged. Generally the hospital does not submit a claim or send a patient statement for inpatient services until after the patient is discharged. On discharge, the Health Information Man-agement (HIM) Department receives the patient’s chart for review and coding. The HIM Department codes services, procedures, and items that were not postedKey Terms
Accounts receivable (A/R)
Accounts receivable (A/R) aging report Accounts receivable ratio (A/R ratio) Adjustment
Advance Beneficiary Notice (ABN) Aging Appeal Balance billing Clean claim Contractual adjustment CMS-1450 (UB-92) CMS-1500
Days in accounts receivable (A/R) Denied claim
Dun message
Electronic remittance advice (ERA) Explanation of benefits (EOB) Fair Credit Billing Act
Fair Debt Collection Practices Act Financial class
Hospital Issued Notice of Noncoverage (HINN) Insurance claim tracer
National Correct Coding Initiatives (CCI) Outstanding accounts
Payer data files Pended claim
Prompt pay statutes Rejected claim
Remittance advice (RA) Statute of Limitations Unbundling
Write-off
Acronyms and Abbreviations
ABN—Advance Beneficiary Notice APC—Ambulatory payment classifications A/R—Accounts receivable
CCI—National Correct Coding Initiatives
CMS—Centers for Medicare and Medicaid Services COB—Coordination of benefits
DRG—Diagnosis Related Group EOB—Explanation of Benefits
EOMB—Explanation of Medicare Benefits EMC—Electronic media claim
ERA—Electronic remittance advice HIM—Health Information Management HINN—Hospital Issued Notice of Noncoverage MCE—Medicare Code Editor
OCE—Outpatient Code Editor PFS—Patient Financial Services RA—Remittance advice TPP—Third-party payer
Patient presents for diagnosis and treatment of conditions. (Patient admission) Information referral/ authorization obtained at admission Payer determination Reimbursement (payment processed) Patient services rendered (documentation) Charge capture (chargemaster) HIM chart review/ coding (APC/DRG assignment) Claim submission (CMS-1450/ CMS-1500) Accounts receivables (A/R) management Payer determination (denial or pended) Resubmit/appeal
Community General Hospital
Charge Description Master (CDM) Chargemaster Number/ Department #/ General Ledger # Procedure/ Item Code HCPCS/ NDC and Modifier Item/Service Description Revenue Code Quantity/ Dose Charge Room C532 Cefepime inj 2 G Tray hyperal dre ABD/KUB flatplat Oximeter Prothrombin time CBC with diff Blood culture Basic metabolic Dopp-venous lowe X-ray chest X-ray chest fluoroscopy 100/977 200/164 300/116 300/169 400/137 700/138 700/138 700/139 700/140 700/167 700/169 700/169 J0692 A4550 74470 S8105 85210 85025 87040 80048 93303 71020 71090 0110 0250 0270 0320 0410 0300 0300 0300 0300 0400 0320 0320 1 2 g 1 1 1 1 1 1 1 1 1 1 1042 133 33 148 49 57 68 121 53 583 185 185
Figure 6-2 Charge Description Master (CDM), commonly referred to as the chargemaster.
Life Cycle of a Hospital Claim
Information obtained at admission
Patient care services rendered and documented Charges captured through chargemaster
HIM review, coding, and APC or DRG assignment Process and submit insurance claims and patient
statements
Payer review and determination—remittance advice
BOX 6-1 KEY POINTS
Hospital Encoder and GROUPER Programs
An encoder program is computer software that allows the HIM professional to enter specified information regarding patient care services and the patient’s condition. The program utilizes data entered to identify potential codes.
A GROUPER program is software that allows the HIM professional to enter specified information regarding the patient’s care including condition(s) and procedure(s). The program utilizes the information to assign an APC or DRG.
BOX 6-2 KEY POINTS
Admission Registration Admitting department Reimbursement Post transactions Patient Financial Services
(PFS) Reimbursement Paid PFS Reimbursement Denied PFS–Collections A/R Management Monitor and follow-up on outstanding claims PFS–Credit and collections
Payer review Payment determination
Third-party payers
Charge submission Claims process Claim preparation (scrubber) Patient Financial Services (PFS)
Claim submission CMS-1500 CMS-1450 manual/electronic Patient Financial Services (PFS) Patient care Order entry Ancillary/clinical departments Charge capture Charge Description Master
(CDM) – HCPCS Codes Department personnel
Chart reviewing/coding Post discharge procedures Health Information Management
(HIM) Charge submission Patient invoice/ statement PFS
Figure 6-3 Hospital billing process highlighting charge submission, payer review, A/R management, and reimbursement functions.
through the chargemaster, such as surgeries. The patient’s diagnoses are also coded by the HIM Depart-ment. Coding is generally performed through an encoder program, which utilizes information entered by the HIM coder to assign procedure and diagnosis codes. The codes and other information entered are also used to assign a Diagnosis Related Group (DRG) or ambulatory payment classification (APC) to the hospital case.
HOSPITAL BILLING PROCESS
As discussed in previous chapters, the hospital billing process involves a series of functions required to submit charges for services rendered. The process involves collection of all financial, insurance, and medical information during the patient visit. Information obtained during the patient visit is utilized to submit charges to payers and patients. A critical part of the billing process is charge submission, which involves preparation of insurance claims and patient statements (Figure 6-3).
Insurance Claims and Patient
Statements
Patient Financial Services (PFS) may also be referred to as the Business Office or the Patient Accounts Depart-ment. PFS is responsible for managing the hospital’s patient financial transactions, which include charge sub-mission, patient transactions, and accounts receivable (A/R) management. Charge submission involves prep-aration of insurance claims and patient statements (Figure 6-4). Board of Directors Operations Finance Administration Marketing Purchasing Compliance Accounting Admitting Patient Financial Services (PFS) Credit and Collections Human Resources Support Services Central supply Plant Operations Grounds and maintenance Quality assurance Medical/ attending staff Ancillary Services Pathology/ laboratory Physical rehabilitation Respiratory therapy Radiology Pharmacy Nursing in various areas Medical Surgical Unit, Labor/ Delivery, OR, ER Other clinical services Surgery Medicine Anesthesia Pulmonary Cardiology Emergency department Risk Management Medical staff credentialing Social services Satellite Development Outpatient clinics Utilization Management (Utilization review) Health information management Volunteer Services Public Relations Legal Services Clinical
Finance Departments — Responsibilities
• Record, monitor, and analyze financial transactions and prepare reports as required.
• Perform tasks to receive a patient in the hospital including: obtain and enter information in the computer, obtain consents and authorizations, prepare a chart, assign a room and bed, where appropriate.
• Prepare claim forms and patient statements for charge submission. • Record charges, payments, adjustments, and write-offs.
• Provide assistance to patients in understanding their account and resolving billing issues.
• Monitor and follow-up on accounts receivables.
Figure 6-4 Hospital organizational chart illustrating the finance departments and their responsibilities.
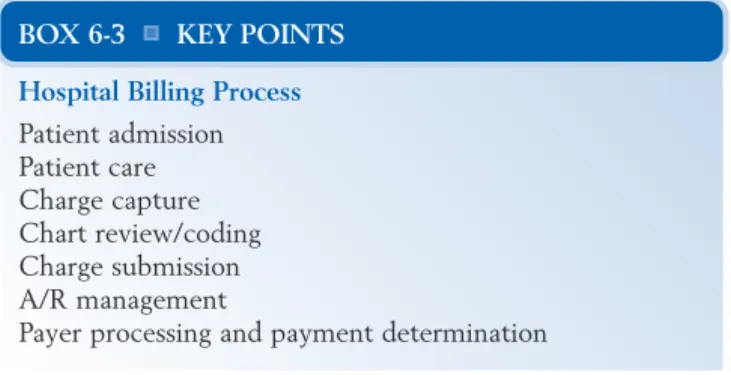
Hospital Billing Process
Patient admission Patient care Charge capture Chart review/coding Charge submission A/R management
Payer processing and payment determination
Insurance Claim Forms
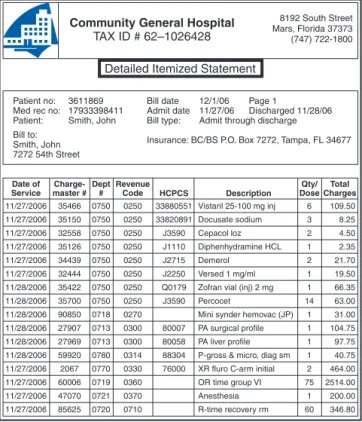
A claim form is prepared for submission of charges to a third-party payer. The goal is to submit a clean claim the first time. A clean claim is defined as one that does not need to be investigated by the payer. The claim passes all internal billing edits and payer-specific edits and is paid without need for additional intervention. Claims that do not meet clean claim status may be denied, rejected, or pended. Preparation of insurance claim forms involves the following steps:
• A detailed itemized statement that outlines each
item and service charged is prepared (Figure 6-5).
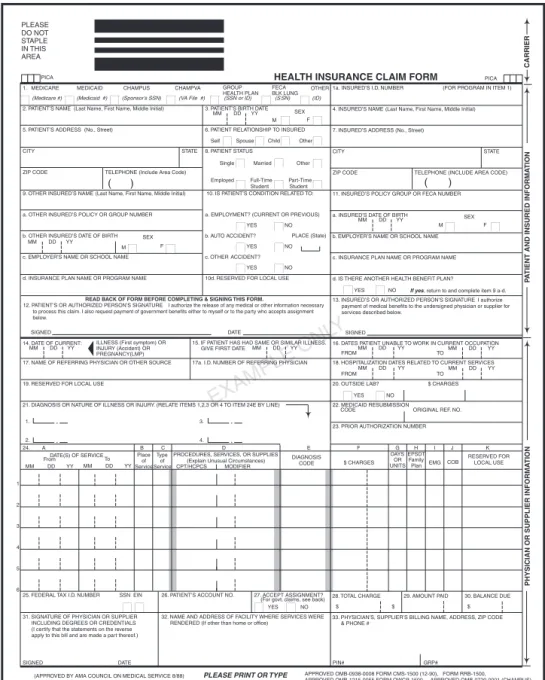
• The appropriate claim form is prepared. As
discussed previously, claim form requirements vary by payer.
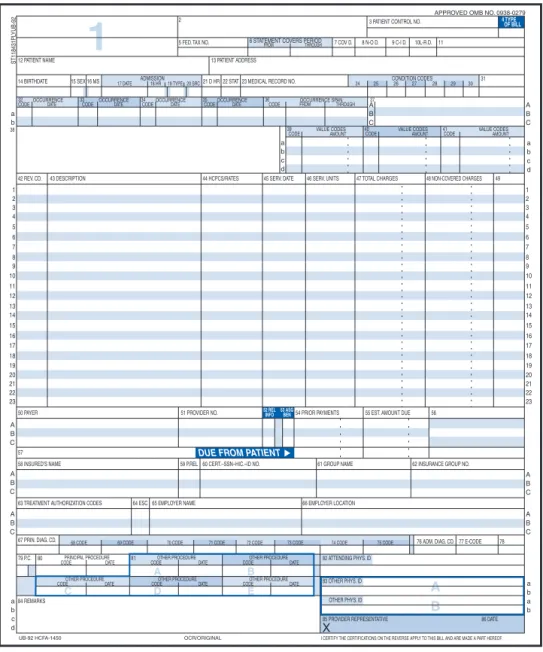
• The universally accepted claim form for submission
of charges for physician and outpatient services is the CMS-1500 (Figure 6-6).The CMS-1450
(UB-92)is the universally accepted claim used to submit facility charges for hospital outpatient and inpatient services (Figure 6-7).
• The claim forms are submitted to respective payers
electronically or manually. Claim forms submitted electronically are referred to as electronic media claims (EMCs). Manual claims are printed on paper and mailed. A detailed itemized statement is generally included with paper claims. Payers receiving electronic claims may request a detailed itemized statement after initial review of the claim. Copies of insurance claims are filed for follow-up.
Patient Statements
Patient statements are generated and sent to the patient. The hospital generally has a schedule for batch
Patient Financial Services (PFS) Responsibilities Charge Submission
• Insurance claim forms • Patient statements
Patient Transactions
• Payments, adjustments, and write-offs
Accounts Receivable (A/R) Management
• Monitoring of and follow-up on outstanding accounts
BOX 6-4 KEY POINTS
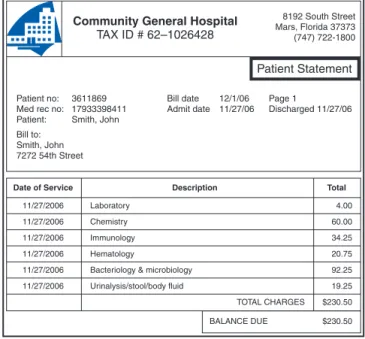
Community General Hospital TAX ID # 62–1026428
Detailed Itemized Statement
8192 South Street Mars, Florida 37373 (747) 722-1800
Patient no: 3611869 Med rec no: 17933398411 Patient: Smith, John Bill to:
Smith, John 7272 54th Street
Bill date 12/1/06 Page 1
Admit date 11/27/06 Discharged 11/28/06 Bill type: Admit through discharge
Insurance: BC/BS P.O. Box 7272, Tampa, FL 34677
Date of Service Charge-master # Revenue Code HCPCS Dept # Description Total Charges Qty/ Dose Vistaril 25-100 mg inj Docusate sodium Cepacol loz Diphenhydramine HCL Demerol Versed 1 mg/ml Zofran vial (inj) 2 mg Percocet
Mini synder hemovac (JP) PA surgical profile PA liver profile P-gross & micro, diag sm XR fluro C-arm initial OR time group VI Anesthesia R-time recovery rm 11/27/2006 11/27/2006 11/27/2006 11/27/2006 11/27/2006 11/27/2006 11/28/2006 11/28/2006 11/28/2006 11/28/2006 11/28/2006 11/28/2006 11/27/2006 11/27/2006 11/27/2006 11/27/2006 35466 35150 32558 35126 34439 32444 35422 35700 90850 27907 27969 59920 2067 60006 47070 85625 0750 0750 0750 0750 0750 0750 0750 0750 0718 0713 0713 0780 0770 0719 0721 0720 0250 0250 0250 0250 0250 0250 0250 0250 0270 0300 0300 0314 0330 0360 0370 0710 6 3 2 1 2 1 1 14 1 1 1 1 2 75 1 60 33880551 33820891 J3590 J1110 J2715 J2250 Q0179 J3590 80007 80058 88304 76000 109.50 8.25 4.50 2.35 21.70 19.50 66.35 63.00 31.00 104.75 97.75 40.75 464.00 2514.00 200.00 346.80
Figure 6-5 Detailed itemized statement.
Clean Claim
A claim that does not require further investigation by the payer. The claim passes all of the edits and is processed accordingly without any additional intervention.
BOX 6-5 KEY POINTS
Clean Claim Status
Examples of claims that do not meet clean claim status. • Claims that require additional information
• Claims that require Medicare secondary payer (MSP) screening information
• Claims that require information to determine coverage • Claims that do not pass payer edits
BOX 6-6 KEY POINTS
Universally Accepted Claim Forms and Means of Submission
Claim Form
• CMS-1500 is the form utilized to submit physician and outpatient services
• CMS-1450 (UB-92) is the form utilized to submit facility charges for hospitals and other institutions
Methods for Submission
• Manual submission involves printing a paper claim that is sent by mail
• Electronic claims are submitted utilizing electronic data interchange (EDI)
mailings of patient statements. For example, the hos-pital’s batch schedule may indicate that statements for patient accounts A to M should be mailed on Mondays and Wednesdays and N to Z on Tuesdays and Thursdays. Patient statements include the following information, as illustrated in Figure 6-8.
• Patient name, address, account number, and medical
record number
• Admission and discharge date
• Description of services, including a procedure code
and charge for each
• Payments and adjustments made on the account,
listed along with the balance owed
• Message regarding outstanding balance or claim
submission
Third-Party Payer (TPP) Claim
Processing
Third-party payer claim processing involves entering claim data into the payer’s system, review of the payer’s data file, performance of payer edits, and payment deter-mination (Figure 6-9). Insurance claims can be trans-mitted electronically or sent by mail. Electronic claims are transmitted directly to the payer’s computer system. Paper claims are scanned or entered manually into the payer’s computer system. The payer’s computer system performs a detailed review and electronic edits on each claim. The computerized review and edits are pre-formed to check information on the claim for the pur-pose of identifying potential problems with the claim. First, the computer checks information on the claim
EXAMPLE ONL
Y
1a. INSURED’S I.D. NUMBER (FOR PROGRAM IN ITEM 1)
4. INSURED’S NAME (Last Name, First Name, Middle Initial)
7. INSURED’S ADDRESS (No., Street)
CITY STATE
ZIP CODE TELEPHONE (INCLUDE AREA CODE)
11. INSURED’S POLICY GROUP OR FECA NUMBER
a. INSURED’S DATE OF BIRTH
b. EMPLOYER’S NAME OR SCHOOL NAME
c. INSURANCE PLAN NAME OR PROGRAM NAME
d. IS THERE ANOTHER HEALTH BENEFIT PLAN?
13. INSURED’S OR AUTHORIZED PERSON’S SIGNATURE I authorize payment of medical benefits to the undersigned physician or supplier for services described below.
SEX
F
HEALTH INSURANCE CLAIM FORM
OTHER 1. MEDICARE MEDICAID CHAMPUS CHAMPVA
READ BACK OF FORM BEFORE COMPLETING & SIGNING THIS FORM.
12. PATIENT’S OR AUTHORIZED PERSON’S SIGNATURE I authorize the release of any medical or other information necessary to process this claim. I also request payment of government benefits either to myself or to the party who accepts assignment below.
SIGNED DATE
ILLNESS (First symptom) OR INJURY (Accident) OR PREGNANCY(LMP)
MM DD YY 15. IF PATIENT HAS HAD SAME OR SIMILAR ILLNESS.GIVE FIRST DATE MM DD YY 14. DATE OF CURRENT:
17. NAME OF REFERRING PHYSICIAN OR OTHER SOURCE
19. RESERVED FOR LOCAL USE
21. DIAGNOSIS OR NATURE OF ILLNESS OR INJURY. (RELATE ITEMS 1,2,3 OR 4 TO ITEM 24E BY LINE) 17a. I.D. NUMBER OF REFERRING PHYSICIAN
From MM DD YY To MM DD YY 1 2 3 4 5 6
25. FEDERAL TAX I.D. NUMBER SSN EIN 26. PATIENT’S ACCOUNT NO. 27. ACCEPT ASSIGNMENT? (For govt. claims, see back) 31. SIGNATURE OF PHYSICIAN OR SUPPLIER
INCLUDING DEGREES OR CREDENTIALS (I certify that the statements on the reverse apply to this bill and are made a part thereof.)
SIGNED DATE
32. NAME AND ADDRESS OF FACILITY WHERE SERVICES WERE RENDERED (If other than home or office)
SIGNED MM DD YY FROM TO FROM TO MM DD YY MM DD YY MM DD YY MM DD YY
CODE ORIGINAL REF. NO.
$ CHARGES EMG COB
RESERVED FOR LOCAL USE
28. TOTAL CHARGE 29. AMOUNT PAID 30. BALANCE DUE
$ $ $
33. PHYSICIAN’S, SUPPLIER’S BILLING NAME, ADDRESS, ZIP CODE & PHONE #
PIN# GRP#
PICA PICA
2. PATIENT’S NAME (Last Name, First Name, Middle Initial)
5. PATIENT’S ADDRESS (No., Street)
CITY STATE
ZIP CODE TELEPHONE (Include Area Code)
9. OTHER INSURED’S NAME (Last Name, First Name, Middle Initial)
a. OTHER INSURED’S POLICY OR GROUP NUMBER
b. OTHER INSURED’S DATE OF BIRTH
c. EMPLOYER’S NAME OR SCHOOL NAME
d. INSURANCE PLAN NAME OR PROGRAM NAME
(APPROVED BY AMA COUNCIL ON MEDICAL SERVICE 8/88)
YES NO ■ ■ ■ ■ ( )
If yes, return to and complete item 9 a-d.
16. DATES PATIENT UNABLE TO WORK IN CURRENT OCCUPATION
18. HOSPITALIZATION DATES RELATED TO CURRENT SERVICES
20. OUTSIDE LAB? $ CHARGES
22. MEDICAID RESUBMISSION
23. PRIOR AUTHORIZATION NUMBER MM DD YY
CARRIER
P
A
TIENT AND INSURED INFORMA
TION
PHYSICIAN OR SUPPLIER INFORMA
T ION ■ ■ M ■ ■ ■■ ■ ■ ■■ F YES NO YES NO 1. 3. 2. 4.
DATE(S) OF SERVICE Type of Service Place
of Service
PROCEDURES, SERVICES, OR SUPPLIES (Explain Unusual Circumstances) CPT/HCPCS MODIFIER DIAGNOSIS CODE PLEASE DO NOT STAPLE IN THIS AREA F M SEX MM DD YY YES NO YES NO YES NO PLACE (State) GROUP
HEALTH PLAN FECABLK LUNG
■ ■ ■■ ■ ■ ■■ ■■ ■■ ■ ■
Single Married Other
■ ■ ■■ ■■ ■ ■ ■■ ■ ■ ■■
3. PATIENT’S BIRTH DATE
6. PATIENT RELATIONSHIP TO INSURED
8. PATIENT STATUS
10. IS PATIENT’S CONDITION RELATED TO:
a. EMPLOYMENT? (CURRENT OR PREVIOUS)
b. AUTO ACCIDENT?
c. OTHER ACCIDENT?
10d. RESERVED FOR LOCAL USE■■ ■■
■ ■ ■■
Employed Full-Time Part-Time Student Student Self Spouse Child Other (Medicare #) (Medicaid #) (Sponsor’s SSN) (VA File #) (SSN or ID) (S SN) (ID)
( ) ■ ■ ■ ■ ■■ ■■ ■■ ■■ ■■ ■ ■ M SEX ■ ■ DAYS OR UNITS EPSDT Family Plan F G H I J K 24. A B C D E ■ ■ ■ ■ ■■
PLEASE PRINT OR TYPE APPROVED OMB-0938-0008 FORM CMS-1500 (12-90), FORM RRB-1500, APPROVED OMB-1215-0055 FORM OWCP-1500, APPROVED OMB-0720-0001 (CHAMPUS)
Figure 6-6 CMS-1500 claim form utilized to submit charges for physician and outpatient services.
against the payer’s data files to verify patient coverage and eligibility.
Payer’s Data File
The computerized payer data files contain information regarding covered individuals, including a history of past claims submitted for the patient. Information sub-mitted on the claim regarding the patient, the insurance,
and the services billed is compared with information in the payer’s data files to verify that the patient is covered under the plan, is eligible to receive benefits, and that all plan requirements are met. The following data are checked against the payer’s data file:
• Patient name and identification number are checked
to confirm that the patient is covered under the policy
• The date of service is checked to ensure that the
services were provided within the benefit period and that the patient is eligible to receive benefits
• Preauthorization information is reviewed to ensure
that plan requirements are met
• Dates of admission and discharge are checked
against the plan coverage details to ensure that length of stay is appropriate
A B A D B E C
1
12 PATIENT NAME ST118431PL Y UB-92 13 PATIENT ADDRESS 14 BIRTHDATE 42 REV. CD. 50 PAYER 5758 INSURED’S NAME 59 P.REL60 CERT.–SSN–HIC.–ID NO. 61 GROUP NAME 62 INSURANCE GROUP NO.
63 TREATMENT AUTHORIZATION CODES
67 PRIN. DIAG. CD.
84 REMARKS
UB-92 HCFA-1450 OCR/ORIGINAL I CERTIFY THE CERTIFICATIONS ON THE REVERSE APPLY TO THIS BILL AND ARE MADE A PART HEREOF.
79 P.C. 82 ATTENDING PHYS. ID 83 OTHER PHYS. ID 85 PROVIDER REPRESENTATIVE X 86 DATE OTHER PHYS. ID 80 81
76 ADM. DIAG. CD. 77 E-CODE 78 65 EMPLOYER NAME 66 EMPLOYER LOCATION
64 ESC
68 CODE
CODE DATE CODE DATE
69 CODE 70 CODE 71 CODE 72 CODE 73 CODE 74 CODE 75 CODE
51 PROVIDER NO.
DUE FROM PATIENT
54 PRIOR PAYMENTS 55 EST. AMOUNT DUE 56
43 DESCRIPTION 44 HCPCS/RATES 45 SERV. DATE 46 SERV. UNITS 47 TOTAL CHARGES 48 NON-COVERED CHARGES 49
32 CODE
38
33
CODE 34CODE 35CODE 36CODE
39
CODE 40CODE 41CODE 37
ADMISSION CONDITION CODES A B C A B C A B C A B C a b c d a b a b a b c d a b a b c d 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 19 20 21 22 23 A B C A B C A B C 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 19 20 21 22 23 15 SEX OCCURRENCE
DATE OCCURRENCEDATE OCCURRENCEDATE OCCURRENCE OCCURRENCE SPAN
PRINCIPAL PROCEDURE OTHER PROCEDURE
CODEOTHER PROCEDURE DATE
CODEOTHER PROCEDURE DATE CODEOTHER PROCEDURE DATE
CODEOTHER PROCEDURE DATE
VALUE CODES DATE
16 MS 21 D HR 22 STAT 23 MEDICAL RECORD NO. 31
4 TYPE OF BILL
52 REL INFO 53 ASGBEN
17 DATE 18 HR 19 TYPE
FROM THROUGH
AMOUNT VALUE CODESAMOUNT VALUE CODESAMOUNT
20 SRC 24 25 26 27 28 29 30
5 FED. TAX NO. FROM THROUGH 7 COV D. 8 N-O D. 9 C-I D. 10L-R.D. 11
APPROVED OMB NO. 0938-0279 3 PATIENT CONTROL NO.
6 STATEMENT COVERS PERIOD 2
Figure 6-7 CMS-1450 (UB-92) claim form utilized to submit facility charges for hospital services.
Third-Party Payer Claim Processing
Claim data entered into payer system Review of claim information
Payer edits
Payment determination
• Procedure code data are reviewed to identify covered and noncovered items
• Services on the claim are also checked against the
common data file to identify duplicate services
Computer Edits
The payer’s system performs computerized edits on the claim for the purpose of identifying problems relating to services billed such as coding errors or issues involv-ing medical necessity. Payer computer edits vary accord-ing to the payer’s criteria and system setup. For example, Medicare’s system contains an Outpatient Code Editor (OCE) and a Medicare Code Editor (MCE). The OCE
Community General Hospital TAX ID # 62–1026428 Patient Statement 8192 South Street Mars, Florida 37373 (747) 722-1800 Patient no: 3611869 Med rec no: 17933398411 Patient: Smith, John Bill to:
Smith, John 7272 54th Street
Bill date 12/1/06 Page 1
Admit date 11/27/06 Discharged 11/27/06
Date of Service Description Total
Laboratory Chemistry Immunology Hematology
Bacteriology & microbiology Urinalysis/stool/body fluid TOTAL CHARGES BALANCE DUE 11/27/2006 11/27/2006 11/27/2006 11/27/2006 11/27/2006 11/27/2006 4.00 60.00 34.25 20.75 92.25 19.25 $230.50 $230.50
Figure 6-8 Sample patient statement.
Claim Data Entered into the payer’s system
Electronic claims
transmitted directly into the payer’s system Manual claims
scanned or manually keyed into the payer’s system
Payer Computerized Edits
are performed to identify problems related to services billed including coding errors
✔ Procedures that are inappropriate based on gender
✔ Procedures that are inappropriate based on age
✔ Procedures that are not medically necessary
✔ Packaged services that are unbundled
Payment Determination
✔ Determination of allowed charges—APC or DRG rate
✔ Determination of deductible—co-insurance or co-payment
✔ Remittance advice is prepared and forwarded to the hospital
✔ Patient coverage is active
✔ Services were provided within coverage period – patient eligible to receive benefits
✔ Preauthorization requirements are met
✔ Length of stay is within plan criteria
✔ Services provided are covered and not duplicate Review Claim Information against the Payer’s Data File to ensure
Figure 6-9 Phases of the third-party payer claims process.
Payer Data Files
Patient coverage is active.
Services were provided within coverage period and the patient is eligible to receive benefits.
Preauthorization requirements are met. Length of stay is within plan criteria.
Services provided are covered and not duplicated.
BOX 6-9 KEY POINTS
Medicare Outpatient Code Editor
(OCE)
Coding Edits
✔ Inpatient only procedure
✔ Invalid diagnosis or procedure code
✔ Age conflict
✔ Sex conflict
✔ Correct coding initiative edits Coverage Edits ✔ Non-covered procedures ✔ Questionable covered procedure Clinical Edits ✔ Invalid age ✔ Invalid sex Claim Edits ✔ Invalid date
✔ Date out of range
✔ Units of service edits
✔ Observation edits
Inpatient Coding Edits
✔ Invalid diagnosis or procedure code
✔ Invalid fourth or fifth digit for diagnosis codes
✔ E code used as a principal diagnosis
✔ Duplicate of the principal diagnosis ✔ Age conflict ✔ Sex conflict ✔ Manifestation code as principal diagnosis ✔ Nonspecific principal diagnosis ✔ Questionable admission ✔ Unacceptable principal diagnosis Coverage Edits ✔ Non-covered procedures ✔ Limited coverage ✔ Open biopsy
✔ Medicare secondary payer (MSP) alert
Inpatient Clinical Edits
✔ Bilateral procedure
✔ Invalid age
✔ Invalid sex
✔ Invalid discharge status
Medicare Code Editor
(MCE)
Figure 6-10 Medicare Outpatient Code Editor (OCE) and Medicare Code Editor (MCE) computer edits are incorporated into Medicare’s system. OCE is for outpatient claims, and MCE is for inpatient claims.
and MCE are used to identify data inconsistencies on hospital outpatient and inpatient claims. The OCE con-tains edits for hospital outpatient claims. The MCE contains edits for hospital inpatient claims (Figure 6-10). The following are examples of computer edits:
• Procedure conflicts with patient’s sex. The
procedure code is checked against the patient’s sex to determine whether the procedure is appropriate. For example, a hysterectomy would not be
performed on a male.
• Procedure conflict with patient’s age. The procedure
code is checked against the patient’s age to verify that the procedure is age appropriate. For example,
a hysterectomy would not normally be performed on a 10-year-old.
• Medical necessity. All services and items provided
must be considered medically necessary to obtain third-party reimbursement. Diagnosis codes are checked against procedure codes to identify problems involving medical necessity.
• Bundled (packaged) services. Services and items
billed are reviewed to identify cases of unbundling. Unbundling is the process of coding multiple codes to describe services that should be described with one code.
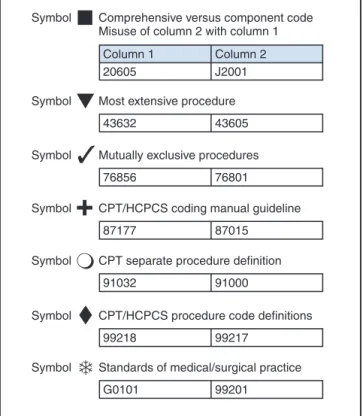
Many payers incorporate the National Correct Coding Initiatives edits into their system. The National Correct
Coding Initiatives (CCI) was developed by CMS for
the purpose of promoting national coding guidelines and preventing improper coding. CCI outlines code combinations that are inappropriate (Figure 6-11).
Payment Determination
Determination of payment is conducted after the com-puter edits are performed. It includes the following steps:
• Determination of allowed charges, APC, or DRG
rate
• Determination of deductible, co-insurance, or
co-payment
• Preparation of a remittance advice or explanation of
benefits, which is forwarded to the hospital
Payment determination may result in one of the following actions:
• The claim is paid
• The claim is placed in a pending status (pending
requested information)
• The claim is denied or rejected
Remittance Advice (RA)
A remittance advice (RA) is a document prepared by the payer to provide an explanation of payment
Unbundling
The process of coding multiple codes to describe services that are described with one code. For example, reporting the following laboratory codes for three tests that were performed on one specimen at the same time.
• 82465, Cholesterol • 83718, Lipoprotein • 84478, Triglycerides
These tests should be reported as a Lipid Panel using CPT code 80061.
BOX 6-10 KEY POINTS
Figure 6-11 Examples of edits from the National Correct Coding Initiatives (CCI).
Symbol Comprehensive versus component code Misuse of column 2 with column 1
Column 1 Column 2
20605 J2001
Symbol Standards of medical/surgical practice
G0101 99201
Symbol CPT/HCPCS procedure code definitions
99218 99217
Symbol CPT separate procedure definition
91032 91000
Symbol Mutually exclusive procedures
76856 76801
Symbol Most extensive procedure
43632 43605
Symbol CPT/HCPCS coding manual guideline
87177 87015
National Correct Coding Initiatives (CCI)
Developed by CMS for the purpose of promoting national coding guidelines and preventing improper coding.
CCI outlines code combinations that are inappropriate, including services that are:
• Integral to a more comprehensive procedure • Mutually exclusive
• Included in the surgical procedure • Sequential procedures
• Bundled
determination for a claim. The RA is also known by other payers as an Explanation of Benefits (EOB) or Explanation of Medicare Benefits (EOMB). The RA includes detailed information about the charges submitted and an explanation of how the claim was processed. An RA can include information regarding several claims. It can be forwarded to the hospital electronically or it can be printed and sent to the hospital by mail. An electronic remittance advice
(ERA) is a document that is electronically transmitted to the hospital to provide an explanation of payment determination for a claim.
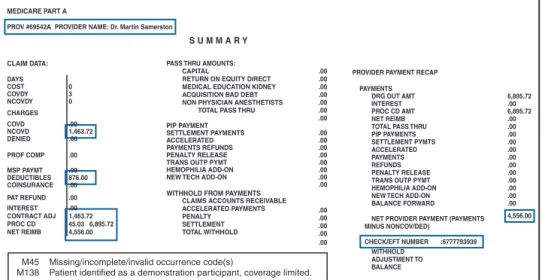
Remittance Advice Data Elements
The design and content of an RA will vary by payer. Most include basic data regarding the patient, service provided, charges submitted, and explanation of the pay-ment determination. Figure 6-12 illustrates the follow-ing data elements listed on a sample Medicare remittance advice:
• Date of the remittance advice and check number
• Patient’s name and identification number
• Name of provider performing services, if not the
same as the hospital
• Claim control number—a number given to the
payer as a reference to the claim when the hospital inquires about a claim
• ICD-9-CM procedure or HCPCS codes and
modifiers describing the billed services or items
• Explanation code or reason code that explains the
claim processing, such as whether the claim is denied or reduced
• The amount of deductible the patient is responsible
to meet
• The co-insurance amount the patient is responsible
to pay
• The payment amount, which is the total amount
paid for all claims outlined on the remittance advice
MEDICARE PART A
P.O. BOX 167953 TEMPE AR 72207 TEL# 800 660 4235 VER# 4010–A1
PROV #69542A PROVIDER NAME: Dr Martin Samerston PART A PAID DATE: 06/26/2006 REMIT#: 7654 PAGE:1 PATIENT NAME PATIENT CNTRL NUMBER ICN
HIC NUMBER NUMBERNACHG HICHG TOB
FROM DT THRU DT COST COVDY NCOVDY CLMSTATUS
SUBTOTAL FISCAL YEAR-$000
SUBTOTAL PART A
TOTAL PART A
RC REM DRG# DRG OUT AMT COINSURANCE PAT REFUND CONTRACT ADJ
RC REM OUTCD CAPCD NEW TECH COVDCHGS ESRD NET ADJ PER DIEM RTE
RC REM PROF COMP MSP PAYMT NCOVD CHGS INTEREST PROC CD AMT
RC REM DRG AMT DEDUCTIBLES DENIED CHGS PRE PAY ADJ NET REIMB
149 6,895.72 1,463.72 .00 4556.00 M 45 .00 .00 .00 .00 M 138 .00 .00 .00 .00 45.03 876.00 5,432.00 .00 4,556.00 .00 .00 .00 .00 .00 .00 .00 .00 .00 .00 .00 .00 .00 876.00 5,432.00 .00 4556.00 Smith John 7 9 4076922738872 084327777A 109876543210 06/01/2005 06/05/2006 3 111 6 00
FIgure 6-12 Sample Medicare RA illustrating data elements (page 1).
Payer Payment Determination
Payment determination is conducted by the payer after the claim passes all computer edits and can result in one of the following actions.
• The claim payment is processed
• The claim is put in a pending status until requested information is received
• The claim is denied or rejected
BOX 6-12 KEY POINTS
MEDICARE PART A
P.O. BOX 167953 TEMPE AR 72207 TEL# 800 660 4235 VER# 4010–A1
PROV #69542A PROVIDER NAME: Dr Martin Samerston PART A PAID DATE: 06/26/2006 REMIT#: 7654 PAGE:1 PATIENT NAME PATIENT CNTRL NUMBER ICN
HIC NUMBER NUMBERNACHG HICHG TOB
FROM DT THRU DT COST COVDY NCOVDY CLMSTATUS
SUBTOTAL FISCAL YEAR-$000
SUBTOTAL PART A
TOTAL PART A
RC REM DRG# DRG OUT AMT COINSURANCE PAT REFUND CONTRACT ADJ
RC REM OUTCD CAPCD NEW TECH COVDCHGS ESRD NET ADJ PER DIEM RTE
RC REM PROF COMP MSP PAYMT NCOVD CHGS INTEREST PROC CD AMT
RC REM DRG AMT DEDUCTIBLES DENIED CHGS PRE PAY ADJ NET REIMB
149 6,895.72 1,463.72 .00 4556.00 M 45 .00 .00 .00 .00 M 138 .00 .00 .00 .00 45.03 876.00 5,432.00 .00 4,556.00 .00 .00 .00 .00 .00 .00 .00 .00 .00 .00 .00 .00 .00 876.00 5,432.00 .00 4556.00 Smith John 7 9 4076922738872 084327777A 109876543210 06/01/2005 06/05/2006 3 111 6 00 1 2 3 4 5 7 8 6
FIgure 6-13 Sample Medicare RA (page 1) illustrating the steps (1 through 8) in analyzing a remittance advice.
Analyzing a Remittance Advice
It is important for hospital billing professionals to under-stand the elements of an RA. Information on the RA is carefully analyzed to ensure that the claim was pro-cessed appropriately. This task is complicated by the
fact that each payer may adopt a different type of form. Information on the RA is used to post payments to the patient’s account. An RA may be several pages long, and it may contain information regarding several patients and several claims (Figures 6-13 and 6-14). Following is an overview of how to analyze the RA.
1. Identify the patient’s name and number for the purpose of opening the correct patient account on the computer system.
2. Match the date of service on the RA to the date of service on the patient’s account.
3. Compare the procedure code indicated on the RA with that listed on the patient’s account to ensure that the claim was paid based on the correct service.
BOX 6-1
LIFE CYCLE OF A HOSPITAL CLAIM: THIRD-PARTY PAYER CLAIM PROCESSING
1. Explain when the life cycle of a hospital claim begins.
2. Discuss the relationship between information obtained by the Admissions Department and the preparation of a claim form.
3. List the steps involved in processing a hospital claim form.
4. State what claim form(s) is used to submit facility charges for hospital outpatient and inpatient services.
5. Provide a brief overview of data found on a patient statement.
6. Discuss the purpose of checking claim information against the payer’s common data file.
7. Explain the two types of review performed on a claim by the payer’s computer system.
8. Explain the difference among the Medicare Code Editor (MCE), the Outpatient Code Editor (OCE), and the National Correct Coding Initiatives (CCI).
9. State what items on the claim are checked to determine medical necessity.
10. List and discuss three steps in payment determination.
Electronic Remittance Advice (ERA)
A document prepared by the payer to provide an explanation of payment determination for a claim. Also referred to as the following.
• Explanation of Benefits (EOB)
• Explanation of Medicare Benefits (EOMB)
4. Review the charge billed on the RA against the charge listed on the patient’s account.
5. Analyze the approved amount and noncovered charges. These amounts indicate what the payer is approving for the service. The payment is
determined based on the approved amount. 6. An explanation of the approved amount is
indicated using some type of coding system commonly referred to as explanation or reason codes. Definitions of the reason codes are listed on the bottom or the back of the RA, as illustrated in Figure 6-15. The reason X2 on the ABC Insurance RA tells the hospital that the allowed amount was determined based on the contract.
7. Information on the RA regarding the deductible and co-insurance explains amounts that are billable to the patient.
M45 Missing/incomplete/invalid occurrence code(s)
M138 Patient identified as a demonstration participant, coverage limited.
CLAIM DATA: DAYS COST 0 COVDY 3 NCOVDY 0 CHARGES COVD .00 NCOVD 1,463.72 DENIED .00 PROF COMP .00 MSP PAYMT .00 DEDUCTIBLES 876.00 COINSURANCE .00 PAT REFUND .00 INTEREST .00 CONTRACT ADJ 1,463.72 PROC CD 45.03 6,895.72 NET REIMB 4,556.00 MEDICARE PART A
PROV #69542A PROVIDER NAME: Dr. Martin Samerston
S U M M A R Y
PASS THRU AMOUNTS:
CAPITAL .00
RETURN ON EQUITY DIRECT .00
MEDICAL EDUCATION KIDNEY .00
ACQUISITION BAD DEBT .00
NON PHYSICIAN ANESTHETISTS .00
TOTAL PASS THRU .00
.00 PIP PAYMENT SETTLEMENT PAYMENTS .00 ACCELERATED .00 PAYMENTS REFUNDS .00 PENALTY RELEASE .00
TRANS OUTP PYMT .00
HEMOPHILIA ADD-ON .00
NEW TECH ADD-ON .00
.00
WITHHOLD FROM PAYMENTS CLAIMS ACCOUNTS RECEIVABLE
ACCELERATED PAYMENTS .00
PENALTY .00
SETTLEMENT .00
TOTAL WITHHOLD .00
.00
PROVIDER PAYMENT RECAP PAYMENTS
DRG OUT AMT 6,895.72
INTEREST .00
PROC CD AMT 6,895.72
NET REIMB .00
TOTAL PASS THRU .00
PIP PAYMENTS .00 SETTLEMENT PYMTS .00 ACCELERATED .00 PAYMENTS .00 REFUNDS .00 PENALTY RELEASE .00
TRANS OUTP PYMT .00
HEMOPHILIA ADD-ON .00
NEW TECH ADD-ON .00
BALANCE FORWARD .00
NET PROVIDER PAYMENT (PAYMENTS 4,556.00
MINUS NONCOV/DED)
CHECK/EFT NUMBER :6777793939 WITHHOLD
ADJUSTMENT TO
BALANCE
Figure 6-14 Sample Medicare RA (page 2) illustrating claim data related to payment.
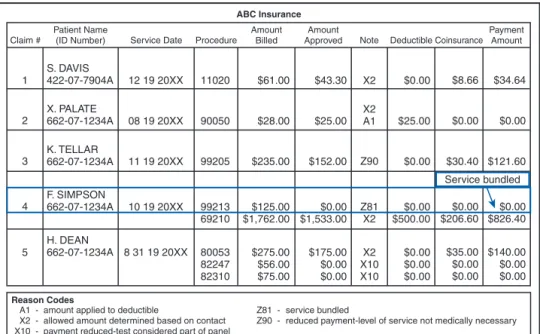
Reason Codes
ABC Insurance
A1 - amount applied to deductible Z81 - service bundled
X2 - allowed amount determined based on contact Z90 - reduced payment-level of service not medically necessary X10 - payment reduced-test considered part of panel
S. DAVIS 422-07-7904A Claim #
Patient Name
(ID Number) Service Date Procedure Amount
Billed
Amount
Approved Reason Deductible
Payment Amount Coinsurance $34.64 $8.66 $0.00 $43.30 $61.00 11020 12 19 20XX X. PALATE 662-07-1234A $0.00 $121.60 $0.00 $25.00 $25.00 $28.00 90050 08 19 20XX K. TELLAR 662-07-1234A 11 19 20XX 99205 $235.00 $152.00 $0.00 $30.40 $0.00 $826.40 F. SIMPSON 662-07-1234A $0.00 $206.60 $0.00 $500.00 $0.00 $1,533.00 $125.00 $1,762.00 99213 69210 10 19 20XX $140.00 $0.00 $0.00 H. DEAN 662-07-1234A $35.00 $0.00 $0.00 $0.00 $0.00 $0.00 $175.00 $0.00 $0.00 $275.00 $56.00 $75.00 80053 82247 82310 8 31 19 20XX X2 X2 A1 Z90 Z81 X2 X2 X10 X10 1 2 3 4 5
Figure 6-15 ABC Insurance RA illustrating reason codes and their explanations.
Patient Transactions
The Patient Financial Services (PFS) Department is responsible for posting transactions to the patient’s account. Patient transactions include the following. • Patient payments
• Third-party payer payments
The account balance will be billed to the patient (balance billing) when appropriate or to a secondary or tertiary insurance (secondary billing).
8. The payment amount on the bottom of the page is the total payment for all claims listed on the RA.
PATIENT TRANSACTIONS
The PFS Department is responsible for processing tran-sactions including payments, adjustments, and other transactions to the patient’s account. Patient payments and third-party payments are posted to the patient’s account by PFS. The process followed is outlined below:
• Payment is posted to the patient’s account
• A contractual adjustment is applied where
applicable
• The balance is billed to the patient or sent to a
secondary or tertiary payer when applicable
• Denials and information requests are researched and
processed as appropriate
• If the claim is denied appropriately, the claim may
need to be submitted to a secondary insurance
Patient Payments
Patient payments are posted to the patient’s account when payment is received. The patient may pay the entire amount or part of the balance owed. When the entire amount is not paid, a statement reflecting the balance will be sent to the patient in the next billing period. Adjustments may be posted to the patient’s account to reflect discounts or amounts that are uncollectible, as discussed later in this section.
Third-Party Payer Payments
Payments from third-party payers are posted to the patient’s account when an RA and check are received from the payer. Payment on a claim is processed in accordance with the payer’s determination. The payer may process payment for the claim as appropriate or the payment amount may be lower than expected by the hospital. This may occur when services are billed separately that are bundled or when medical necessity criteria are not met for a higher level of service. If the correct amount is not paid by the payer, a hospital representative will pursue correction of the claim.
Incorrect Payment Level
When the payer processes a claim at a reduced level or payment is not made for a service reported on the
Patient Transaction Process
Payment is posted to the patient’s account
A contractual adjustment is applied where applicable The balance is billed to the patient or sent to a secondary
or tertiary payer where applicable
Denials and information requests are researched and processed as appropriate
If the claim is denied appropriately, it may be necessary for the claim to be submitted to a secondary insurance
BOX 6-15 KEY POINTS
Reason Codes
A1 - amount applied to deductible Z81 - service bundled
X2 - allowed amount determined based on contact Z90 - reduced payment-level of service not medically necessary X10 - payment reduced-test considered part of panel
S. DAVIS 422-07-7904A Claim #
Patient Name
(ID Number) Service Date Procedure Amount
Billed
Amount
Approved Note Deductible
Payment Amount Coinsurance $34.64 $8.66 $0.00 $43.30 $61.00 11020 12 19 20XX X. PALATE 662-07-1234A $0.00 $121.60 Service bundled $0.00 $25.00 $25.00 $28.00 90050 08 19 20XX K. TELLAR 662-07-1234A 11 19 20XX 99205 $235.00 $152.00 $0.00 $30.40 $0.00 $826.40 F. SIMPSON 662-07-1234A $0.00 $206.60 $0.00 $500.00 $0.00 $1,533.00 $125.00 $1,762.00 99213 69210 10 19 20XX $140.00 $0.00 $0.00 H. DEAN 662-07-1234A $35.00 $0.00 $0.00 $0.00 $0.00 $0.00 $175.00 $0.00 $0.00 $275.00 $56.00 $75.00 80053 82247 82310 8 31 19 20XX X2 X2 A1 Z90 Z81 X2 X2 X10 X10 1 2 3 4 5 ABC Insurance
Figure 6-16 ABC Insurance RA #1 highlighting a service the payer bundled into another service. The hospital cannot balance bill the patient for this amount.
claim, a hospital representative must investigate the reason for the reduced payment or nonpayment. Com-mon situations when a claim may be paid at a reduced level are outlined below:
• The diagnosis code(s) submitted does not meet
medical necessity criteria for the service level billed
• Services are billed with more than one code when
they should be described with a single code
• A service that is considered part of a more
comprehensive service is billed separately
The ABC Insurance RA #1 illustrated in Figure 6-16 highlights a reduced payment situation. The RA reason, code Z81, indicates that the payer did not pay on procedure 99213, “Evaluation and Management” (E/M) service. The reason for nonpayment is that the payer considered the E/M to be part of the surgical package. The surgical package outlines services that are bundled into the surgery code.
The hospital cannot balance bill the patient for this amount if it participates with the insurance company. Upon investigation, it may be determined that the service should not have been considered part of the surgical package, and payment should have been made. If the E/M service was not related to the surgery or if the decision for surgery was made during the E/M service, the hospital may request that the claim be reprocessed with a modifier attached to the E/M code, or the hospital may appeal the claim.
Adjustments
An adjustment is the process of reducing the original amount charged by a specified amount. There are several types of adjustments that may be posted to a patient’s account, such as discount, contractual adjustment, or write-off, as outlined below.
Common Reasons for Reduced Claim Payments
Level of service is not supported by the patient’s condition
Service may be bundled, such as services included in the surgical package
Service may be considered an integral part of a larger procedure
BOX 6-16 KEY POINTS
Reason Codes
A1 - amount applied to deductible Z81 - service bundled
X2 - allowed amount determined based on contact Z90 - reduced payment-level of service not medically necessary X10 - payment reduced-test considered part of panel
S. DAVIS 422-07-7904A Claim #
Patient Name
(ID Number) Service Date Procedure Amount
Billed
Amount
Approved Reason Deductible
Payment Amount Coinsurance $34.64 $8.66 $0.00 $43.30 $61.00 11020 12 19 20XX X. PALATE 662-07-1234A $0.00 $121.60 Difference between amount charged and approved amount
$0.00 $25.00 $25.00 $28.00 90050 08 19 20XX K. TELLAR 662-07-1234A 11 19 20XX 99205 $235.00 $152.00 $0.00 $30.40 $0.00 $826.40 F. SIMPSON 662-07-1234A $0.00 $206.60 $0.00 $500.00 $0.00 $1,533.00 $125.00 $1,762.00 99213 69210 10 19 20XX $140.00 $0.00 $0.00 H. DEAN 662-07-1234A $35.00 $0.00 $0.00 $0.00 $0.00 $0.00 $175.00 $0.00 $0.00 $275.00 $56.00 $75.00 80053 82247 82310 8 31 19 20XX X2 X2 A1 Z90 Z81 X2 X2 X10 X10 1 2 3 4 5 ABC Insurance
Figure 6-17 ABC Insurance RA #2 illustrating a contractual adjustment in the amount of $17.70 (the difference between the amount billed and the amount approved).
Adjustments
The original amount charged is reduced by a specified amount. Types of adjustments are as follows.
• Discount
• Contractual adjustment • Write-off
Discount
The original charge may be discounted by a specific amount as an agreement between the patient and the hospital. For example, a hospital may offer a discount to self-pay patients who are responsible for the entire hospital bill. The hospital may offer a 20% discount to the patient for payment of the entire balance. When the payment is received, the adjustment is made to the patient’s account to reduce the original charge by the discounted amount.
Contractual Adjustment
A contractual adjustment is a reduction made to the original charge in accordance with the hospital’s contract with a payer. Payer contracts include provisions regarding the amount the hospital is required to accept as payment in full, commonly referred to as the approved amount. The approved amount may represent a case rate, contract rate, DRG or APC rate, or fee schedule amount. In accordance with the contract, the hospital agrees to follow those provisions and therefore may not bill patients for amounts over the approved amount. The difference between the approved amount and the hospital’s original charge must be adjusted off the patient’s account. The hospital posts a contractual adjustment to the patient’s account to reduce the original charge. Most hospitals program the computer billing system to calculate and deduct the contractual amount as required by agreement with the payer.
The ABC Insurance RA #2 illustrated in Figure 6-17 highlights a contractual adjustment situation. The difference between the billed amount of $61.00 and the approved amount of $43.30 on claim number 1 is $17.70. A contractual adjustment in the amount of $17.70 must be posted to the patient account if the hospital is participating with the insurance company. The reduction of the claim by $17.70 is a contractual adjustment that is made in accordance with the hospital’s contract with the payer.
Write-Off
A write-off is the process of reducing a patient’s balance to zero. Write-offs are made when the balance is deemed uncollectible. In accordance with most contracts, the hospital is not allowed to forgive or write-off a patient deductible, co-insurance, and co-payment amount. The hospital is required to follow the necessary steps required to make every attempt to collect the amount for which the patient is responsible. When all efforts are exhausted to collect the patient’s responsibility, the hospital may then off the balance. These write-offs are considered a bad debt. Hospitals establish policies and procedures regarding write-offs that detail the necessary steps required to collect the patient balance and the criteria for write-offs.
Balance Billing
Balance billingrefers to billing the patient for a balance in excess of the payer’s approved amount in accordance with the payer contract. When the hospital is participat-ing with the payer, the contractual agreement prohibits balance billing a patient for the following amounts:
• The difference between the original charge and the
approved amount
• The amount of hospital charges that are greater
than a DRG payment rate
• The amount of hospital charges that are greater
than an APC payment rate
The hospital is required to bill a patient for amounts related to co-payments, co-insurance, and deductible amounts. In some cases, charges for services that are not covered may also be billed. Medicare requires that beneficiaries be given an Advance notice of services that Medicare may not cover due to medical necessity. The notice required by Medicare is the Advance Beneficiary Notice (ABN) or Hospital Issued Notice of Non-coverage (HINN).
Advance Beneficiary Notice (ABN)
An Advance Beneficiary Notice is a written notice that is presented to a Medicare beneficiary before Medicare
Figure 6-18 Advance Beneficiary Notice (ABN), required for
Part B services are furnished, to inform the beneficiary that the provider believes Medicare will not pay for some or all of the services to be rendered because they are not reasonable and necessary. Figure 6-18 illustrates Medicare’s ABN. Hospitals are required to present this form for signature to the beneficiary before services are rendered. The hospital cannot bill the patient for these services if the ABN is not completed and on file.
Hospital Issued Notice of Noncoverage (HINN)
The HINN is a written notice that is presented to a Medicare beneficiary before Medicare Part A services are furnished to inform the beneficiary that the pro-vider believes that Medicare will not pay for some or all of the services to be rendered because they are not reasonable and necessary. The HINN is required by Medicare for hospital Part A services that may not be covered due to medical necessity. The HINN is written in letter form, and it must be presented and signed by the beneficiary before services are rendered. The content of an HINN varies based on the type of services that may not be covered; for example, an admission. Figure 6-19 illustrates a sample HINN.
Balance Billing
Law prohibits balance billing Medicare patients for the following amounts
• The difference between the original charge and the approved amount
• The amount of hospital charges that are greater than a DRG payment
• The amount of hospital charges that are greater than an APC payment
BOX 6-18 KEY POINTS COMMUNITY HOSPITAL8192 South Street
Mars, Florida 37373 (747) 722-1800 HOSPITAL ISSUED NOTICE OF NONCOVERAGE (HINN)
December 15, 2005 Patient name: Zalma Jerzon Address: 4949 South Street Philadelphia, PA 72929
Admission Date: December 15, 2005 Health Insurance Claim (HIC) Number: 67945221 Attending Physician: Dr. Jason James
YOUR IMMEDIATE ATTENTION IS REQUIRED Dear Ms. Jerson:
The purpose of this notice is to inform you that we find that your admission for (a total knee replacement) is not covered under Medicare for the following reason(s) MEDICAL NECESSITY. This determination was based upon our understanding and interpretation of available Medicare coverage policies and guidelines. You should discuss with your attending physician other arrangements for any further health care you may require. If you decide to (be admitted to/remain in) the hospital, you will be financially responsible for all customary charges for services furnished during the stay, except for those services for which you are eligible under Part B.
This notice, however, is not an official Medicare determination. The QIO Organization is the quality improvement organization (QIO) authorized by the Medicare program to review inpatient hospital services provided to Medicare patients in the State of (Pennsylvania), and to make that determination.
If you disagree with our conclusion: (Select as appropriate) Preadmission:
Request immediately, but no later than 3 calendar days after receipt of this notice, or, if admitted, at any point in the stay, an immediate review of the facts in your case. You may make this request through us or directly to the QIO by telephone or in writing to the address listed below.
Admission:
Request immediately, or at any point during your stay, an immediate review of the facts in your case. You may make this request through us or directly to the QIO by telephone or in writing to the address listed below.
If you do not wish an immediate review:
You may still request a review within 30 calendar days from the date of receipt of this notice by telephoning or writing to the address specified below.
Results of the QIO Review:
The QIO will send you a formal determination of the medical necessity and appropriateness of your hospitalization, and will inform you of your reconsideration and appeal rights. IF THE QIO DISAGREES WITH THE HOSPITAL (i.e., the QIO determines that your care is covered), you will be refunded any amount collected except for any applicable amounts for deductible, coinsurance, and convenience services or items normally not covered by Medicare.
IF THE QIO AGREES WITH THE HOSPITAL, you are responsible for payment for all services beginning on December 15, 2005.
ACKNOWLEDGMENT OF RECEIPT OF NOTICE
This is to acknowledge that I received this notice of non-coverage of services from the Community Hospital on 12/15/04 at 8:35 a.m. I understand that my signature below does not indicate that I agree with the notice, only that I have received a copy of the notice.
(Signature of beneficiary or Representative) Date Time cc: QIO and Attending Physician
Figure 6-19 Hospital Issued Notice of Noncoverage (HINN), CMS Hospital Manual required for Medicare Part A services.
(Modified from Centers for Medicare & Medicaid Services:
Hospital-issued notice of noncoverage, new.cms.hhs.gov/BNI/
Downloads/HINNs1to10.pdf, 2005.)
Advance Beneficiary Notice (ABN) and Hospital Issued Notice of Noncoverage (HINN)
ABN
A written notice presented to a Medicare beneficiary before Part B services are furnished to inform the beneficiary that Medicare may not pay for some or all of the services to be rendered because they are not reasonable and necessary.
HINN
A written notice presented to a Medicare beneficiary before Part A services are furnished to inform the beneficiary that Medicare will not pay for some or all of the services to be rendered because they are not reasonable and necessary.
BOX 6-19 KEY POINTS
Coordination of Benefits (COB)
A clause written into an insurance policy or government program plan that defines how benefits will be paid when the member or beneficiary is covered under multiple plans.
Third-party payers combine efforts to coordinate benefits paid by the plan through the coordination of benefits (COB) provisions. These provisions help to ensure the following conditions.
• The plans pay as primary and secondary payers appropriately
• Total payments for the claim do not exceed more than 100% charges
• There is no duplication of payments for health care services
BOX 6-2
REMITTANCE ADVICE (RA): PATIENT TRANSACTIONS
1. Define an electronic remittance advice.
2. List various names used to describe the document provided by the payer that explains how a claim was processed.
3. Explain the process of posting patient and third-party payments to the patient’s account by the PFS.
4. Explain why it is important to compare the procedures listed in a remittance advice with those listed on the patient’s account.
5. Describe the purpose of reason codes.
6. List common reasons why a payer may process payment at an incorrect level.
7. Discuss why it is important for a hospital representative to analyze payment made by an insurance company.
8. Outline the actions required when payment is received at the incorrect level.
9. Provide an explanation of an adjustment.
10. List three types of adjustments a hospital may make to a patient’s account.
11. Describe contractual adjustment and explain when this type of adjustment is made to a patient account.
12. State when a hospital may write off a balance.
13. Provide a brief explanation of balance billing.
14. Explain the purpose of an ABN.
Secondary Billing
Secondary billing may occur when the patient has a supplemental insurance that is designed to cover expenses not covered by the primary insurance. When
payment is processed from the primary payer, the hospital representative may initiate billing to a secondary or ter-tiary payer. Coordination of benefits (COB) provisions for the plan must be followed. Medicare secondary payer guidelines must also be followed. Coordination of benefits and Medicare secondary payer guidelines will be discussed later in this text in the payer chapters.
ACCOUNTS RECEIVABLE (A/R)
MANAGEMENT
Accounts receivable is a term used to describe revenue owed to the hospital by patients and third-party payers. Accounts receivable is commonly referred to as A/R. A/R management is a vital function required to monitor and follow-up on outstanding accounts. The financial stability of a hospital is highly dependent on maintaining a positive cash flow. The hospital must maintain a steady flow of revenue (income) to cover expenses required to provide patient care services. To accomplish this, the hospital monitors the revenue cycle. As illustrated in Figure 6-20, the hospital revenue cycle begins when the patient arrives at the hospital for patient care services and ends when payment is received. The primary objective of A/R management is to minimize the amount of time that accounts are outstanding. Outstanding accounts are accounts that have been billed to the patient or third-party payer but have not received any payment. A/R management involves tracking accounts that have not been paid, assessing action required to secure payment, and implementing procedures to secure payment.
Accounts Receivable (A/R) Reports
Hospitals utilize various computerized reports to monitor accounts that have not been paid, such as an unbilled accounts report, financial class report, denials manage-ment report, and accounts receivable aging reports.Accounts Receivable (A/R) Aging Report
Computer-generated A/R aging reports are utilized to identify and analyze outstanding accounts. The A/R
aging reportis a listing of outstanding accounts based on the age of the account. The term aging refers to the number of days the account has been outstanding. The computer system counts the number of days the account is outstanding from the date the claim or state-ment is sent. A/R reports can be run for specified patient accounts or by payer type. The report cate-gorizes accounts based on aging categories in incre-ments of 30 days, as outlined below:
• 0 to 30 days • 31 to 60 days • 61 to 90 days • 91 to 120 days Transaction posting payments, adjustments, rejections/denial/ pended claims Patient received Billing information obtained Patient care rendered Charges generated and posted Charges billed Patient statements Third-party claims A/R management Patient and third-party follow-up Denial management
Figure 6-20 Hospital revenue cycle.
Accounts Receivable (A/R) Management
Functions required to monitor and follow-up on outstanding accounts to ensure that reimbursement is received in a timely manner.
BOX 6-21 KEY POINTS
Accounts Receivable (A/R) Reports Unbilled Accounts
Listing of patient accounts that have not been billed
Financial Class
Outlines claim information such as charges, payments, and outstanding balances, grouped according to type of payer
Denials Management
Listing of claims that have been denied
Accounts Receivable (A/R) Aging
Outstanding accounts are categorized based on the number of days the balance is outstanding
BOX 6-22 KEY POINTS
Aging
The process of counting the number of days that an account is outstanding from the date billed.
• 121 to 150 days.
• 151 to 180 days.
Table 6-1 illustrates an A/R aging report based on patient billed date. The report includes the account number, patient name, and phone number. Outstanding amounts owed on the patient account are reported in
the column that reflects the aging category of the amount owed. Table 6-2 illustrates an A/R report based on payer type. Payer-based A/R reports include the payer name, payer code, and phone number. Outstand-ing amounts are reported in the appropriate agOutstand-ing category. A/R reports provide a percentage of aging in each of the aging categories.
TABLE 6-1 Community General Hospital Patient A/R Report, December 30, 2005
Days Outstanding
Account Name Phone Current 31-60 61-90 91-120 121-150 151-180 180+ Total
Number Balance 05962 Applebee, Carla (813) 797-4545 724.45 724.45 23456 Borden, Andrew (813) 423-9678 200.00 47.52 247.52 16955 Cox, Anthony (813) 233-7794 175.00 695.00 199.53 1069.53 14355 Freeman, Tina (727) 665-7878 592.14 592.14 00876 Holtsaver, Marshall (727) 874-2945 485.72 400.00 1583.66 2469.38 00023 James, John (813) 201-2054 350.00 963.68 1313.68 10245 Marcus, Xavier (727) 779-3325 2745.21 2745.21 19457 Peters, Samantha (413) 544-2243 1545.23 1022.69 2567.92 99645 Snowton, Michael (941) 333-4325 1314.00 3254.00 4568.00 Report Totals 660.72 2945.21 4304.23 3254 2825.56 0 2308.11 16297.83 % Aged 4.05% 18.07% 26.41% 19.97% 17.34% 0.00% 14.16%
TABLE 6-2 Community General Hospital Third-Party Payer A/R Report, December 30, 2005
Days Outstanding
Payer Payer Phone Current 31-60 61-90 91-120 121-150 151-180 180+ Total
Code Balance
Aetna AETNA (800) 797-4545 724.45 724.45
BlueCross/ BCBS (800) 423-9678 24224.34 29666.59 45987.65 32456.78 15765.12 27459.44 175559.92 Blue Shield
Champus CHMPV (800) 233-7794 6759.25 695.00 199.53 7653.78
Fed Emp FET (800) 665-7878 592.14 592.14
Trust Medicaid MDCD (800) 874-2945 2459.32 1456.00 14245.00 11727.00 1600.00 792.80 1435.00 33715.12 Medicare MDCR (800) 201-2054 34567.00 52000.00 37456.32 64456.00 60797.00 45511.00 27564.88 322352.2 Metropolitan MET (800) 779-3325 16453.22 274.00 6400.00 7329.00 14676.11 22453.29 67585.62 Nationwide NAT (800) 544-2243 1545.23 1022.69 2567.92 Workers WCMP (800) 333-4325 6600.00 47243.00 82899.00 3254.00 64222.00 24214.55 17243.56 245676.11 Comp Report 50385.57 141376.56 166781.14 131824.65 168219.14 100959.58 6880.62 856427.26 Totals % Aged 5.88% 16.51% 19.47% 15.39% 19.64% 0.00% 14.16%