Original Article
Effectiveness of pharmacist intervention in the
management of coronary artery disease after
index percutaneous coronary intervention: a
single center randomized controlled trial
Nongzhang Xu1,2*,, Cuihong Wang2*, Jianwei Wan2, Xiaoqing Liu2, Zhongdong Li1, Min Chen2
1Department of Pharmacy, Fudan University Huashan Hospital, Shanghai, China; 2Department of Pharmacy,
Shanghai University of Medicine & Health Sciences Zhoupu Hospital, Shanghai, China. *Equal contributors.
Received December 14, 2018; Accepted April 9, 2019; Epub June 15, 2019; Published June 30, 2019
Abstract: Objective: This study aimed to explore the effect of pharmacist intervention on medication adherence, risk factor control, 6 months prognosis, and 2 years prognosis in patients with coronary artery disease (CAD) after the index percutaneous coronary intervention (PCI). Methods: From January 2015 to December 2015, 200 CAD patients were treated with PCI at our hospital. The control group was given routine treatment and nursing care. In addition to routine treatment and nursing care, the intervention group was given direct pharmacist intervention including medication program optimization, formulated pharmaceutical care, medication education, health educa-tion, and outpatient follow-up. The two groups were followed for two years. Readmission rate, incidence of major adverse cardiac events (MACE), readmission expense, awareness rate of secondary prevention drugs, medication adherence, and emotion management were compared between the two groups at 6 months and 2 years after the index procedure. Risk factors in the two groups at 2 years were compared. Results: At 2 years, the risk factors in
the intervention group were significantly improved in comparison with the control group [smoking: 3.1% vs. 12.6%,
P = 0.012; normal blood glucose rate: 79.6% vs. 62.1%, P = 0.007; normal blood pressure rate: 74.5% vs. 53.7%,
P = 0.003; normal blood lipid rate: 84.7% vs. 57.9%, P < 0.001]. The readmission rate, MACE incidence, and
read-mission expense in the intervention group were significantly lower than the control group at 6 months and 2 years [47.7% vs. 72.6%, P = 0.001; 17.3% vs. 28.8%, P < 0.001; 7512.5 ± 10269.6 RMB vs. 22172.6 ± 24413.2 RMB,
P = 0.025]. Conclusion: Pharmacist intervention can effectively improve medication adherence, reduce
postopera-tive risk factors, MACE incidence, medical expenses in patients after the index PCI. These beneficial effects were increasingly more significant along with time.
Keywords:Coronary artery disease, percutaneous coronary intervention, pharmaceutical care, medication adher-ence
Introduction
Percutaneous coronary intervention (PCI) is a cornerstone in the treatment of coronary artery disease (CAD). PCI can effectively reopen clogged vessels, improve myocardial ischemia, and relieve symptoms. However, it has been shown that poor risk factor control and poor medication adherence are associated with increased incidence of major adverse cardiac events (MACE) after PCI, such as stent throm-bosis, restenosis, and myocardial infarction [1, 2].
Guidelines for the prevention and treatment of CAD indicate that the incidence of post-PCI
MACE can be significantly reduced with long-term use of anti-platelet drugs, β-blockers, angiotensin converting enzyme inhibitors/ angiotensin receptor blockers (ACEI/ARB), cal-cium blockers, statins, and other secondary prevention drugs, as well as control of CAD-related risk factors, such as smoking, obesity, hypertension, hyperglycemia, and dyslipidemia [3, 4]. Therefore, medication adherence is criti -cal for successful secondary prevention of CAD after PCI [5].
on the long-term medication adherence in pa- tients with CAD after PCI [8]. This study aimed to investigate the effect of pharmacist interven-tion on risk factor control, medicainterven-tion adher-ence, and short-term and long-term prognosis in patients with CAD after the index PCI. Materials and methods
Patients
The study was conducted at Zhoupu Hospital, Shanghai University of Medicine and Health Sciences, Shanghai, China. The study protocol was approved by the Ethics Committee of the hospital. All patients provided written informed consent.
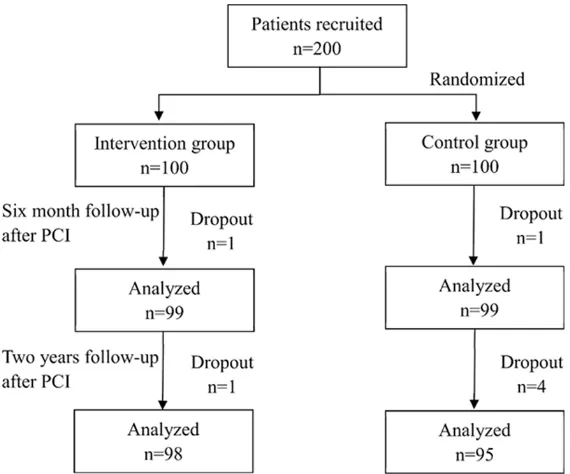
From January 2015 to December 2015, 200 patients with CAD underwent their index PCI at our hospital. The patients were randomly divid-ed into the intervention group or the control group using a random number table. The inclu-sion criteria were: (1) aged 45 to 75 years, male or female; (2) underwent the index PCI for CAD; (3) able to read and understand the test ques-tionnaire; (4) signed the informed consent. Patients with the following conditions were excluded: (1) liver and kidney dysfunction or malignant tumor; (2) mental disorders; (3) unable or unwilling to complete the follow-up. Intervention protocol
Patients in the control group were given routine treatment and nursing care. No pharmacist intervention was involved in the treatment. The patients were followed with telephone inter-view after the discharge.
In addition to routine treatment and nursing care, pharmacists participated in the whole process of treatment of patients in the inter-vention group. The pharmacist interinter-vention was implemented during hospitalization to develop individualized pharmaceutical care program. The pharmacists evaluated and optimized the medication treatment plan and formulated the pharmaceutical care plan, considering the specific needs of a patient. Pharmacists also explained the disease-related knowledge, such as risk factors, clinical manifestations, compli-cations, and treatment of CAD. Medication knowledge was introduced to the patients, such as treatment objective, mechanism of action, route of administration, adverse effects,
anti-platelet drugs, anti-hypertensive drugs, lipid-regulating drugs. The importance of taking medicine according to the instruction was emphasized. Lifestyle intervention was imple-mented including smoking cessation, alcohol abstinence, salt restriction, low-fat diet, weight loss, and exercise. Psychological counseling was used to reduce anxiety and other negative emotions. Before discharge, patients were given individualized medication and lifestyle education, and were asked to be followed by the pharmacists once a month. The pharma-cists assessed risk factors and adherence of the patients at each follow-up and adjusted the medication accordingly. If necessary, further medication education was given to correct non-standard medicine use. The pharmacists also optimized the pharmaceutical care program. Outcome evaluation
Risk factors such as blood pressure [9], blood glucose [10], and blood lipids [11] were con -trolled according to the latest relevant guide-lines in China. Medication adherence was eval-uated using the Morisky Medication Adherence Scale. The highest score of the scale was 8 points. A score less than 6 points indicated low adherence. A score of 6-7 points indicated moderate adherence. An 8-point sore showed high adherence. The primary endpoints were readmission rate, MACE, and readmission expense. MACE included recurrent angina pec-toris, fatal or nonfatal myocardial infarction, and revascularization.
Statistical analysis
Statistical analysis was performed using the SPSS 17 software. Descriptive analysis was used for continuous variables, and frequency analysis was used for categorical variables. Enumeration data were compared using the Chi-square test, and measurement data were compared using the one-way ANOVA or the non-parametric test. P < 0.05 was considered sta-tistically significant.
Results
Baseline data
analysis due to relocation or lack of clinical data (Figure 1). The mean age of our patients was 62.6 ± 7.0 years. The baseline clinical data of the two groups are shown in Table 1. There was no significant difference in gender, age, blood glucose level, blood pressure, heart rate, and blood lipid level between the two groups (all P > 0.05).
MACE after PCI
At 6 months and 2 years after the index PCI, the intervention group had significantly lower read
-mission rate, cumulative MA- CE, revascularization, and re- admission expense in compar-ison with the control group (Tables 2, 3; all P < 0.05). There was no significant differ -ence in recurrent angina pec-toris and nonfatal myocardial infarction between the two gr- oups.
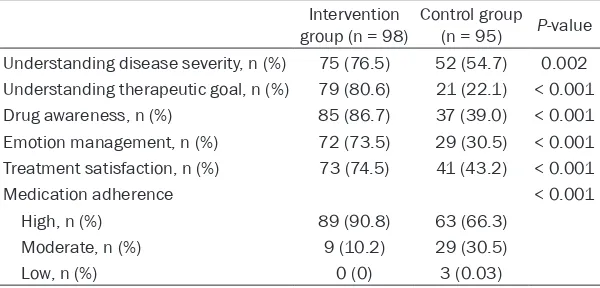
Cognitive management and medication adherence
At 6 months and 2 years after the index PCI, the intervention group had significantly better understanding of the disea- se, treatment goals, medica-tion, related knowledge, emo-tion management and higher satisfaction of treatment in comparison with the control group (Tables 4, 5; all P < 0.05). However, there was no significant difference in me-dication adherence between the two groups at 6 months. At 2 years, medication adher-ence of the intervention gr- oup was significantly higher than that of the control group (90.8% vs. 66.3%, P < 0.01).
Risk factors
[image:3.612.91.376.72.309.2]The intervention group had significantly improved risk fac -tors of blood pressure, blood glucose level, and blood lipid level in comparison with the control group (Table 6).
Figure 1. Diagram of patient allocation. PCI, percutaneous coronary inter-vention.
Table 1. Patient general information
Intervention
group (n = 98) Control group (n = 95) P-value
Male, n (%) 59 (60.2) 62 (65.2) 0.468
Age (years) 62.69 ± 11.00 62.38 ± 11.23 0.859 Smoker, n (%) 19 (19.4) 25 (26.3) 0.251 Heart rate (beat/min) 70.7 ± 6.9 70.1 ± 6.7 0.793 Diabetes, n (%) 28 (28.6) 29 (30.5) 0.766 Hypertension, n (%) 62 (63.3) 61 (64.2) 0.891
Renal insufficiency, n (%) 7 (0.07) 6 (0.06) 0.819 TG, mmol/L 1.52 ± 0.78 1.61 ± 0.78 0.755 LDL-C, mmol/L 2.51 ± 1.36 2.7 ± 0.58 0.651 HDL-C, mmol/L 1.03 ± 0.28 1.09 ± 0.23 0.457
TG, triglyceride; LDL-C, low density lipoprotein cholesterol; HDL-C, high density lipoprotein cholesterol.
Discussion
[image:3.612.90.374.374.531.2]im-proved the long-term prognosis in patients with CAD after PCI.
Secondary prevention drugs are an essential part of the comprehensive treatment of CAD
armacist intervention can improve medication adherence and patient cooperation [16]. Ph-armacists can enhance patient confidence to the treatment, reduce anxiety, and promote heart health by providing psychological coun-Table 3. Comparison of endpoints at 2 years
Intervention group (n = 98) Control group (n = 95) P-value
Readmission, n (%) 47 (48.0) 69 (72.6) 0.001
Recurrent angina pectoris, n (%) 39 (39.8) 64 (67.4) < 0.001 Revascularization, n (%) 13 (13.3) 34 (35.8) < 0.001
[image:4.612.89.525.87.165.2]Nonfatal myocardial infarction, n (%) 1 (1.0) 7 (7.4) 0.027 Readmission expense, RMB 7512.5 ± 10269.6 22172.6 ± 24413.2 0.025
Table 4. Comparison of therapeutic cognition and management at 6 months
Intervention
group (n = 98) Control group (n = 95) P-value
Understanding disease severity, n (%) 84 (85.7) 68 (71.6) 0.022
Understanding therapeutic goal, n (%) 87 (88.8) 33 (34.7) < 0.001
Drug awareness, n (%) 91 (92.9) 46 (48.4) < 0.001
Emotion management, n (%) 75 (76.5) 49 (51.6) < 0.001
Treatment satisfaction, n (%) 89 (90.8) 75 (79.0) 0.026
Medication adherence 0.065
High, n (%) 93 (94.9) 76 (87.4)
Moderate, n (%) 5 (5.1) 12 (12.6)
Low, n (%) 0 (0) 0 (0)
Table 5. Comparison of therapeutic cognition and management at 2 years
Intervention
group (n = 98) Control group (n = 95) P-value
Understanding disease severity, n (%) 75 (76.5) 52 (54.7) 0.002
Understanding therapeutic goal, n (%) 79 (80.6) 21 (22.1) < 0.001
Drug awareness, n (%) 85 (86.7) 37 (39.0) < 0.001
Emotion management, n (%) 72 (73.5) 29 (30.5) < 0.001
Treatment satisfaction, n (%) 73 (74.5) 41 (43.2) < 0.001
Medication adherence < 0.001
High, n (%) 89 (90.8) 63 (66.3)
Moderate, n (%) 9 (10.2) 29 (30.5)
[image:4.612.92.523.201.281.2]Low, n (%) 0 (0) 3 (0.03)
Table 2. Comparison of endpoints at 6 months
Intervention group (n = 98) Control group (n = 95) P-value
Readmission, n (%) 13 (9.2) 19 (20.0) 0.041
Recurrent angina pectoris, n (%) 11 (11.2) 15 (15.8) 0.053
Revascularization, n (%) 2 (2.0) 8 (10.5) 0.015
Nonfatal myocardial infarction, n (%) 0 (0) 1 (1.1) 0.309
Readmission expense, RMB 4545.8 ± 1096.7 15055 ± 5352.2 0.057
[image:4.612.91.392.326.470.2] [image:4.612.91.391.516.660.2]Ph-seling, medication education, and health guid-ance [17-19].
At baseline, approximately 80% of our patients were not aware of the drugs they were taking in terms of treatment goals, precautions during medication, and possible adverse effects. A majority of our patients were on multiple drugs, and often missed a dose or discontinued a medication. Pharmacist intervention and medi-cation edumedi-cation, as well as outpatient follow-up, helped our patients to better understand their own medication and the importance of secondary prevention for CAD, resulting in improved medication adherence. In the inter-vention group, 90% of the patients took the medicines on time, showing significantly improved medication adherence in comparison with the control group. Medication adherence level of CAD patients at postoperative 1 year was significantly lower than that at discharge, and decreased significantly along with time [20]. The study also found that in the control group patients with good medication adher-ence were 21.1% less at postoperative 2 years than postoperative 6 months. Follow-up by pharmacists for 2 years still had significant beneficial on medication adherence, indicating that long-term follow-up is effective to improve medication adherence of patients with CAD after PCI.
Abundant evidence has shown that CAD is closely related to smoking, obesity, high blood pressure, diabetes mellitus, and dyslipidemia [14]. Intervention for controlling these risk fac -tors of CAD also plays an important role in improving long-term prognosis and reducing mortality of patients with CAD. Long-term
Acknowledgements
The study was supported by the Shanghai Health and Family Planning Commission, 2018 Shanghai Clinical Pharmacy Key Specialist Construction project and the Important Weak Discipline Construction Project of the Pudong New Area Health System (NO. PWZbr2017-17). We also thank the patients and investigators who participated in the study.
Disclosure of conflict of interest
None.
Address correspondence to: Zhongdong Li, De- partment of Pharmacy, Fudan University Huashan Hospital, Shanghai, China. E-mail: zdgli@126.com; Min Chen, Department of Pharmacy, Shanghai University of Medicine & Health Sciences Zhoupu Hospital, Shanghai, China. E-mail: zply_89@163. com
References
[1] Ho PM, Magid DJ, Shetterly SM, Olson KL, Maddox TM, Peterson PN, Masoudi FA and Rumsfeld JS. Medication nonadherence is as-sociated with a broad range of adverse out-comes in patients with coronary artery dis-ease. Am Heart J 2008; 155: 772-779.
[image:5.612.91.359.86.228.2][2] Yusuf S, Islam S, Chow CK, Rangarajan S, Da-genais G, Diaz R, Gupta R, Kelishadi R, Iqbal R, Avezum A, Kruger A, Kutty R, Lanas F, Lisheng L, Wei L, Lopez-Jaramillo P, Oguz A, Rahman O, Swidan H, Yusoff K, Zatonski W, Rosengren A, Teo KK; Prospective Urban Rural Epidemiology (PURE) Study Investigators. Use of secondary prevention drugs for cardiovascular disease in the community in high-income, middle-income, and low-income countries (the PURE Study):
Table 6. Comparison of risk factor control at 2 years
Intervention
group (n = 98) Control group (n = 95) P-value Smoker, n (%) 3 (3.1) 12 (12.6) 0.012
Normal blood glucose, n (%) 78 (79.6) 59 (62.1) 0.007 Glycosylated hemoglobin 5.8 ± 0.24 6.5 ± 0.43 < 0.001
Normal blood pressure, n (%) 73 (74.5) 51 (53.7) 0.003
High cholesterol diet, n (%) 5 (5.1) 21 (22.1) < 0.001 TG, mmol/L 0.79 ± 0.02 1.36 ± 0.03 < 0.001 LDL-C, mmol/L 2.01 ± 0.05 2.44 ± 0.02 < 0.001 HDL-C, mmol/L 1.06 ± 0.23 1.16 ± 0.18 < 0.001
Normal blood lipid, n (%) 83 (84.7) 55 (57.9) < 0.001
TG, triglyceride; LDL-C, low density lipoprotein cholesterol; HDL-C, high density lipoprotein cholesterol.
health education can effectively reduce the risk factors, as well as the incidence and mortality of patients with CAD after PCI [13].
a prospective epidemiological survey. Lancet 2011; 378: 1231-43.
[3] Hillis LD, Smith PK, Anderson JL, Bittl JA, Bridg-es CR, Byrne JG, Cigarroa JE, DiSBridg-esa VJ, Hiratz-ka LF, Hutter AM Jr, Jessen ME, Keeley EC, La-hey SJ, Lange RA, London MJ, Mack MJ, Patel MR, Puskas JD, Sabik JF, Selnes O, Shahian DM, Trost JC, Winniford MD, Jacobs AK, Ander-son JL, Albert N, Creager MA, Ettinger SM, Guy-ton RA, Halperin JL, Hochman JS, Kushner FG, Ohman EM, Stevenson W, Yancy CW; American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. 2011 ACCF/AHA guideline for coro-nary artery bypass graft surgery: executive summary: a report of the American College of Cardiology Foundation/American Heart Asso-ciation Task Force on Practice Guidelines. J Thorac Cardiovasc Surg 2012; 143: 4-34.
[4] Jones K, Saxon L, Cunningham W, Adams P; Guideline Development Group. Secondary pre-vention for patients after a myocardial infarc-tion: summary of updated NICE guidance. BMJ 2013; 347: f6544.
[5] Cordero A, Rodriguez Padial L, Batalla A, López Barreiro L, Torres Calvo F, Castellano JM, Ruiz E, Bertomeu-Martínez V; CAPS study investiga-tors. Optimal pharmacological treatment and adherence to medication in secondary preven-tion of cardiovascular events in Spain: results from the CAPS study. Cardiovasc Ther 2017; 35.
[6] Santschi V, Chiolero A, Burnand B, Colosimo AL and Paradis G. Impact of pharmacist care in the management of cardiovascular disease risk factors: a systematic review and meta-analysis of randomized trials. Arch Intern Med 2011; 171: 1441-53.
[7] Cai H, Dai H, Hu Y, Yan X and Xu H. Pharmacist care and the management of coronary heart disease: a systematic review of randomized controlled trials. BMC Health Serv Res 2013; 13: 461.
[8] Tang F-m and Wang BJCP. Brief Analysis on Status Quo of Domestic and Foreign
Medica-tion EducaMedica-tion for Patients [J]. China Pharmacy
2013, 32: 179-182.
[9] Liu LS; Writing Group of 2010 Chinese Guide-lines for the Management of Hypertension.
[2010 Chinese guidelines for the management
of hypertension]. Zhonghua Xin Xue Guan Bing Za Zhi 2011; 39: 579-615.
[10] American Diabetes Association. Standards of medical care in diabetes--2012. Diabetes Care 2012; 35: S11-63.
[11] Joint Committee for Developing Chinese guide-lines on Prevention and Treatment of
Dyslipid-emia in Adults. [Chinese guidelines on preven -tion and treatment of dyslipidemia in adults]. Zhonghua Xin Xue Guan Bing Za Zhi 2007; 35: 390-419.
[12] Swieczkowski D, Mogielnicki M, Cwalina N, Zuk G, Pisowodzka I, Ciecwierz D, Gruchala M and Jaguszewski M. Medication adherence in pa-tients after percutaneous coronary interven-tion due to acute myocardial infarcinterven-tion: from research to clinical implications. Cardiol J
2016; [Epub ahead of print].
[13] Clark AM, Hartling L, Vandermeer B and McAli-ster FA. Meta-analysis: secondary prevention programs for patients with coronary artery dis-ease. Ann Intern Med 2005; 143: 659-72.
[14] Farkouh ME, Boden WE, Bittner V, Muratov V, Hartigan P, Ogdie M, Bertolet M, Mathewkutty S, Teo K, Maron DJ, Sethi SS, Domanski M, Frye RL and Fuster V. Risk factor control for coronary artery disease secondary prevention in large randomized trials. J Am Coll Cardiol 2013; 61: 1607-1615.
[15] Zhao S, Zhao H, Wang L, Du S and Qin Y. Edu-cation is critical for mediEdu-cation adherence in patients with coronary heart disease. Acta Car-diol 2015; 70: 197-204.
[16] Zhang X and Yang GJCPJ. The effect of medica-tion reconciliamedica-tion in patients with medicamedica-tion errors in cardiology department. 2013; 48: 234-237.
[17] Zhao SJ, Zhao HW, Du S and Qin YH. The im-pact of clinical pharmacist support on patients receiving multi-drug therapy for coronary heart disease in China. Indian J Pharm Sci 2015; 77: 306-311.
[18] Michal M1, Simon P, Gori T, König J, Wild PS, Wiltink J, Tug S, Sterzing B, Unterrainer J, Mün-zel T, Beutel ME. Psychodynamic Motivation and Training program (PMT) for the secondary prevention in patients with stable coronary heart disease: study protocol for a randomized controlled trial of feasibility and effects. Trials 2013; 14: 314.
[19] Kovacs AH and Moons P. Psychosocial func-tioning and quality of life in adults with con-genital heart disease and heart failure. Heart Fail Clin 2014; 10: 35-42.