Full Terms & Conditions of access and use can be found at
http://www.tandfonline.com/action/journalInformation?journalCode=uawm20 ISSN: 1047-3289 (Print) (Online) Journal homepage: http://www.tandfonline.com/loi/uawm20
Medical Waste Treatment and Disposal Methods
Used by Hospitals in Oregon, Washington, and
Idaho
Pornwipa Klangsin & Anna K. Harding
To cite this article:
Pornwipa Klangsin & Anna K. Harding (1998) Medical Waste Treatment and
Disposal Methods Used by Hospitals in Oregon, Washington, and Idaho, Journal of the Air &
Waste Management Association, 48:6, 516-526, DOI: 10.1080/10473289.1998.10463706
To link to this article:
http://dx.doi.org/10.1080/10473289.1998.10463706
Published online: 27 Dec 2011.
Submit your article to this journal
Article views: 1101
View related articles
Copyright 1998 Air & Waste Management Association
Medical Waste Treatment and Disposal Methods Used by
Hospitals in Oregon, Washington, and Idaho
Pornwipa Klangsin
Department of Public Health, Oregon State University, Corvallis, Oregon
Anna K. Harding
Department of Public Health, Oregon State University, Corvallis, Oregon
ABSTRACT
This study investigated medical waste practices used by hospitals in Oregon, Washington, and Idaho, which in-cludes the majority of hospitals in the U.S. Environmen-tal Protection Agency’s (EPA) Region 10. During the fall of 1993, 225 hospitals were surveyed with a response rate of 72.5%. The results reported here focus on infectious waste segregation practices, medical waste treatment and disposal practices, and the operating status of hospital incinerators in these three states. Hospitals were provided a definition of medical waste in the survey, but were que-ried about how they define infectious waste. The results implied that there was no consensus about which agency or organization’s definition of infectious waste should be used in their waste management programs. Confu-sion around the definition of infectious waste may also have contributed to the finding that almost half of the
IMPLICATIONS
The disposal and treatment of medical waste continues to be a topic of controversy and concern, particularly since air pollution standards have forced the closure of many hospital incinerators. This research provides the first com-prehensive overview of medical waste treatment and dis-posal practices being used by the majority of hospitals in EPA Region 10, and updated information about the ef-fect clean air regulations have had in forcing these hos-pitals to consider alternative medical waste management strategies. As the overall volume and costs associated with treatment continue to increase, this information is important to generators of medical waste, hospitals out-side this region, state agencies that are involved in the regulatory processes, and waste management compa-nies that treat medical waste generated by any type of healthcare facility.
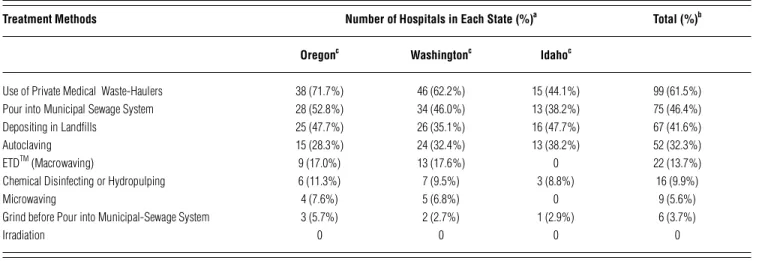
hospitals are not segregating infectious waste from other medical waste. The most frequently used practice of treat-ing and dispostreat-ing of medical waste was the use of private haulers that transport medical waste to treatment facili-ties (61.5%). The next most frequently reported techniques were pouring into municipal sewage (46.6%), depositing in landfills (41.6%), and autoclaving (32.3%). Other meth-ods adopted by hospitals included Electro-Thermal-Deac-tivation (ETD), hydropulping, microwaving, and grind-ing before pourgrind-ing into the municipal sewer. Hospitals were asked to identify all methods they used in the treat-ment and disposal of medical waste. Percentages, there-fore, add up to greater than 100% because the majority chose more than one method. Hospitals in Oregon and Washington used microwaving and ETD methods to treat medical waste, while those in Idaho did not. No hospitals in any of the states reported using irradiation as a treat-ment technique. Most hospitals in Oregon and Washing-ton no longer operate their incinerators due to more strin-gent regulations regarding air pollution emissions. Hos-pitals in Idaho, however, were still operating incinerators in the absence of state regulations specific to these types of facilities.
INTRODUCTION
During the 1980s, several incidents involving the dis-posal of medical waste caused significant public con-cern in areas of the United States.1–6 The public
associ-ated these incidents with the AIDS and Hepatitis B vi-rus (HBV) epidemics and responded with fear. This widespread outcry effectively forced Congress and sev-eral other fedsev-eral agencies, including the U.S. Envi-ronmental Protection Agency (EPA), the Centers for Disease Control and Prevention (CDC), the Occupa-tional Safety and Health Administration (OSHA), and
the Nuclear Regulatory Commission (NRC), to develop regulations and standards for the disposal and treat-ment of medical waste.7–10 In addition, the majority of
states, including Oregon, Washington, and Idaho, have passed state-specific laws regarding the management of medical waste.11–14
Hospitals comprise only 2% of all medical waste gen-erators, but generate as much as 77% of the total annual volume of regulated medical waste in the United States— approximately 8,400 lbs/month/hospital.15 Additional
medical waste is produced by clinics, laboratories, physi-cians’ offices, dentists’ offices, veterinarians’ offices, long-term healthcare facilities, freestanding blood banks, fu-neral homes, residential care facilities, and illegal drug use.16 The amount of medical waste produced by
hospi-tals may vary due to a number of factors, including the hospital type and size, occupancy rate, in- and out-patient ratio, geographic location, state and local waste handling regulations, and hospital waste disposal poli-cies.16,17
The terminology applied to medical waste and medi-cal waste management in hospitals is neither universal nor consistent. The CDC, the EPA, the Joint Commission on Accreditation of Healthcare Organizations (JCAHO), the American Hospital Association (AHA), and the Agency for Toxic Substances and Disease Registry (ATSDR) all have different definitions for “hospital,” “medical,” “infec-tious,” and “regulated medical” wastes. These terms are often mistakenly interchanged.18,19 In general, hospital
waste refers to all waste, biological and non-biological, that is discarded and not intended for further use.19,20 It
consists of infectious and non-infectious solid waste, haz-ardous waste, and low-level radioactive waste.21
In contrast, medical waste, infectious waste, and regu-lated medical waste are all subsets of hospital waste. Medi-cal waste is defined in Section 3 of the MediMedi-cal Waste Tracking Act of 1988 as “any solid waste that is generated in the diagnosis, treatment, or immunization of human beings or animals, in research pertaining thereto, or in the production or testing of biologicals.”16 Medical waste
is, therefore, defined more broadly than infectious waste or regulated medical waste, but less broadly than hospital waste.20,22
The portion of medical waste capable of producing an infectious disease is considered to be infectious waste. In order for waste to be infectious, the four conditions necessary for infection to occur (a virulent pathogen, suf-ficiently high dose, portal of entry, and host resistance) must be present.16,19 CDC considers microbiological waste
(e.g., cultures and stocks), blood and blood products, pathological waste, and sharps to be infectious waste.16
Regulated medical waste refers specifically to the seven different classes of medical waste required by the EPA to
be tracked under the demonstration program, which are similar to that recognized by the CDC as being infectious waste.16,23 The classes include laboratory cultures and
stocks, pathological wastes, human blood and blood prod-ucts, used sharps, animal wastes, isolation wastes, and unused sharps.16
The various definitions yield significant differences in the amounts of waste identified as infectious, and there-fore affect the costs of managing infectious wastes. For example, 3–6% of a hospital’s total waste might qualify as infectious waste using CDC definitions, whereas 7–15% of hospital waste would be considered infectious waste using the broader EPA definitions.18,24 Because the cost of
infectious waste disposal can be as much as 6–20 times higher than that of solid waste disposal, hospitals are wise to use as narrow a definition of infectious waste as pos-sible, taking care to identify the components of the waste stream that are truly capable of transmitting disease.25
In addition to discrepancies in definitions about medi-cal and infectious waste, hospitals have also faced ambi-guities in regulations, guidelines, and standards that ap-ply to these waste streams, which has led to confusion among the hospital industry and waste managers about proper management procedures. Medical waste is not uniformly regulated at the state level throughout the United States; in some states, regulations have not yet been adopted. At the same time, federal regulations (such as air pollution and solid/hazardous waste laws) have also limited alternatives to on-site treatment methods of medi-cal waste. For example, as states enforce the Clean Air Act of 1990, many uncontrolled on-site hospital incinerators have been required to be renovated, replaced, or even closed down, and waste that was once incinerated must now receive alternative treatment.26 Regulations have also
forced hospitals to change either medical waste or infec-tious waste management practices. For example, in many states infectious waste must be treated before being bur-ied in a landfill, or it is required to be segregated and la-beled before being hauled to a commercial facility.27
Nev-ertheless, an estimated 60% of the nation’s medical waste is still disposed of in small to medium-sized incinerators located on-site at hospitals and other medical facilities.28
In addition to these facilities are commercial incinerators that accept medical wastes from a variety of sources. Com-mercial units, which are much larger than on-site hospi-tal incinerators, burn an estimated 20% of the nation’s medical waste.29 The remaining 20% is autoclaved and
either directly placed in a landfill, or fired in a municipal waste incinerator and then placed in a landfill.28
During the past five years, various aspects of medical and infectious waste management have been researched. Studies have included a survey of infectious waste practices in Washington,30 a biomedical waste survey in Oklahoma,31
a review of current legal requirements,32 public health
implications of medical waste,33 occupational exposure
to infectious waste,34 current practices and risks posed by
infectious waste disposal,35 and medical waste practices
in small facilities.18 Although an earlier study on
infec-tious waste disposal was conducted in American Hospital Association (accredited) hospitals, only 7% of U.S. hospi-tals were represented in this study.36 Since that time,
regu-lations have expanded and changed. Information is still lacking about the regulations hospitals follow with regard to medical waste management, and about specific waste handling practices and disposal methods that are used to comply with federal and state mandates. No studies have comprehensively investigated the medical waste practices of hospitals in the contiguous states of EPA Region 10, which comprise the majority of hospitals in this region. The purpose of this study, therefore, was to investigate medical waste treatment and disposal practices in hospi-tals in Oregon, Washington, and Idaho. The study also sought to answer questions about which regulations and standards these hospitals follow in their medical waste management plans, as well as gather information about the operating status of hospital incinerators.
METHODS
Sampling
The study population included all hospitals (N = 225) in Oregon, Washington, and Idaho listed in the 1992 AHA
Guide to the Healthcare Field.37 This group included 70
hos-pitals in Oregon, 107 hoshos-pitals in Washington, and 48 hospitals in Idaho. Each hospital was sent a letter of invi-tation to participate in the study, and asked to respond to the survey. Prior to mailing the surveys, each hospital was contacted to obtain the name and the title of the person responsible for medical or infectious waste management at that facility. The surveys were then mailed specifically to the person with that responsibility. The majority of these people occupied positions in infection control, en-vironmental services, nursing, maintenance, and facility personnel management. The first set of surveys was mailed in September 1993. Non-respondents were sent a second mailing one month later. All responses were collected until November 1993, one month after the follow-up mailing.
Survey Instrument
The survey instrument consisted of a four-page question-naire divided into sets of questions pertaining to a par-ticular aspect of medical waste management. The results of several sets of questions are reported in this paper. The first set included questions regarding definitions of in-fectious waste used by hospitals in their waste manage-ment programs, categories of medical waste considered infectious, and segregation practices. A second set of
questions requested information regarding incinera-tion and other medical waste treatment techniques currently applied in these facilities.
The survey was revised and critiqued by staff at the Oregon State University Survey Research Center. Sampling and consent procedures were approved by the Oregon State University Institutional Review Board for the Pro-tection of Human Subjects. The final draft was then pretested by medical or infectious waste managers in three different hospitals, and edited according to their suggestions.
Analysis
To facilitate the data entry process, the completed ques-tionnaires were separated into groups by states. Data from the surveys were analyzed using Statgraphics 5.0.38 The
level of significance for analysis was set at α = 0.05. RESULTS AND DISCUSSION
Response Rate
A total of 161 surveys were returned for a response rate of 72.5%. The response rates for hospitals in Oregon, Wash-ington, and Idaho were similar: 75.7, 71.5, and 70.8%, respectively. This overall rate is markedly higher than the 46% response rate for a study of U.S. hospitals conducted in 1987, and a 51% response rate obtained with a 1989 Washington Department of Ecology study.30,36
Definitions Used for Medical and Infectious Waste
The survey asked that respondents use the standard medical waste definition, which included solid waste generated in the diagnosis, treatment, or immuniza-tion of human beings.27 Respondents were also asked
to consider hazardous solid waste and hospital waste produced from the laboratory and in testing as medi-cal waste.39 In addition, the respondents were reminded
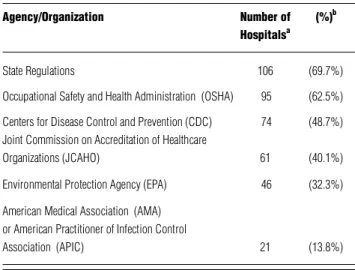
that medical waste also included infectious waste. In-fectious waste was, however, purposefully not defined for the respondents, as the researchers were interested in finding out whether or not there is a consensus among these hospitals about the definition of infec-tious waste. Table 1 shows the percentages of hospi-tals that use a particular agency or organization’s defi-nition of infectious waste in their medical waste man-agement program. The majority of hospitals adopted the state’s definition (69.7%) and/or OSHA’s definition (62.5%) of infectious waste. Slightly fewer than half used CDC’s definition (48.7%) and JCAHO’s definition (40.1%). It was also noted that the vast majority of hospitals (90.1%) indicated they used definitions pro-vided by more than one agency or organization. These definitions are dissimilar because they were issued for
different purposes. For example, CDC published uni-versal precautions to guard against disease transmis-sion; EPA’s purpose was to regulate the medical waste stream; and OSHA, with its Bloodborne Pathogens Standards, sought to protect workers from occupational exposure to bloodborne pathogens. In addition, hos-pitals are often members of several accrediting organi-zations (JCAHO or AHA) or professional associations (AMA or American Practitioner of Infection Control [APIC]), and must meet the standards imposed by each. A healthcare institution, therefore, may be required to comply with state regulations regarding medical waste management as well as standards that are re-quired for accreditation purposes.
These results support previous research indicating that the basis for a hospital’s definition of infectious waste may be extremely variable, based on regulations from different federal agencies, standards of accreditation groups or professional associations, or local regula-tions,23,30 and is confusing at best. One author
recom-mends that the term “potentially infectious waste” be uniformly adopted by all parties as standard terminol-ogy, referring to that portion of hospital-generated waste which, if not contained and managed properly, could result in the transfer of infection.23
Respondents were next asked to select the catego-ries of medical waste that were considered to be infec-tious waste in their hospitals. Overall in the three states, blood specimens and blood products (96.9%), all sharps (93.7%), microbiology laboratory waste (89.9%), patho-logical waste (89.9%), body parts (80.4%), and waste from surgery (77.2%) were most commonly considered to be infectious waste. Table 2 shows that a greater number of categories of medical waste are considered
to be infectious by hospitals than are required by state regulatory agency definitions. For example, more than 50% of hospitals choose to designate contaminated equipment as infectious waste, even though contami-nated equipment is not required to be regulated as infec-tious waste by any agency or organization.
In addition, chemotherapy waste is not categorized as infectious waste in either state regulations and other agencies’ standards,12–14 but was nevertheless treated by
more than 50% of hospitals in Washington and Idaho as infectious waste. One of the reasons that hospitals con-sidered this waste to be infectious may be that chemo-therapy waste sometimes contains antineoplastic drugs and cytotoxic agents.40 Although antineoplastic drugs are
included in the “U” list of hazardous wastes defined by the EPA, antineoplastic drugs used in chemotherapy are regulated as hazardous waste only when they enter the waste stream in unemptied, discarded source contain-ers.41 The results from this study suggest, therefore, that
hospitals in these states that treat chemotherapy waste or contaminated equipment as infectious waste may be inadvertently overly managing these wastes because nei-ther are officially classified as infectious waste.
Waste Segregation Practices
Respondents were asked if their hospital segregated in-fectious waste from medical waste. The results indicated that 89 hospitals (55.3%) reported segregating infectious waste from medical waste, with Idaho reporting the high-est percentage of hospitals segregating waste (64.7%). Per-centages in Washington and Oregon were lower at 54.1 and 51.0%, respectively.
Table 1. Sources of definitions of infectious waste used by hospitals (N = 152). Agency/Organization Number of (%)b
Hospitalsa
State Regulations 106 (69.7%)
Occupational Safety and Health Administration (OSHA) 95 (62.5%) Centers for Disease Control and Prevention (CDC) 74 (48.7%) Joint Commission on Accreditation of Healthcare
Organizations (JCAHO) 61 (40.1%) Environmental Protection Agency (EPA) 46 (32.3%) American Medical Association (AMA)
or American Practitioner of Infection Control
Association (APIC) 21 (13.8%)
a
Many hospitals (90.1%) chose more than one source.
b
Row percentages based on N = 152.
Table 2.Categories of medical waste considered to be infectious.
Waste Categories Oregon Washington Idaho Waste from Communicable Disease Units
(Isolation Waste) 71.2 % 78.4 % 84.4 % Culture and Stock (Microbiology
Laboratory Waste) 90.4 % 89.2 % 90.0 % Pathological Waste 90.4% 90.6 % 87.5 % Blood Specimens and Blood Products 94.2 % 97.3 % 100 % Sharps 94.2 % 93.2 % 93.8 % Only Contaminated Sharps 3.9 % 0.7 % 6.3 % Body Parts 84.6 % 78.4 % 78.1 % Waste from Surgery Rooms 71.2 % 78.4 % 78.1 % Animal Carcasses 21 .2 % 25.1 % 18.8 % Dialysis Unit Waste 36.5 % 23.0 % 8.1 % Contaminated Equipment 69.2 % 52.7 % 59.4 % Chemotherapy Waste 3.5 % 59.5 % 53.1 % Note: Waste categories and numbers in bold indicate infectious waste categories defined by state regulations.
Two previous studies reported much higher percent-ages of hospitals segregating infectious waste from medi-cal waste. The first, a medimedi-cal waste study conducted in 1989 by the Washington Department of Ecology, reported that 85% of hospitals in Washington segregated infectious waste from medical waste.30 A second survey of 955
hos-pitals nationwide reported that 95.4% of hoshos-pitals segre-gated out infectious waste.36
The lower rate of waste segregation reported by hos-pitals in these three states may be partially explained by the high proportion of non-responses to this question. Overall, 39 hospitals (24.2%) did not answer the ques-tion, with hospitals in Oregon having the highest non-response rate (30.0%). The non-non-response rate for hospi-tals in Washington was 22.9%, and the non-response rate for Idaho hospitals was 17.7%. This is surprising because most of the hospitals had at least one advisory commit-tee that was responsible for overseeing medical or infec-tious waste management, and a third of the hospitals also had a committee providing advice on the management of radioactive, chemotherapy, and/or chemical waste. We would have expected that with these committees in place, waste segregation would be routinely practiced and in-formation about the extent to which it is practiced would be widely known.
Hospitals in Oregon reported a surprisingly low rate of waste segregation, given that state law requires healthcare facilities generating infectious waste to segre-gate this waste from other waste at the point of genera-tion.12,42 One factor contributing to this low rate may be
that approximately 72% of hospitals in Oregon used pri-vate waste haulers to transport medical waste to off-site treatment facilities. Because these companies often pro-vide auxiliary services, such as waste segregation and re-packaging, hospitals in Oregon may be depending on waste haulers to segregate the waste rather than actively practicing in-house segregation.
One of the reasons hospitals should be encouraged to segregate infectious waste from other waste is that this practice is likely to lower a hospital’s waste disposal costs. Segregation methods help hospitals eliminate the higher costs associated with special handling, treatment, and disposal of infectious waste.43 In addition, waste
segrega-tion is one of the methods used to reduce the amount of mixed waste. Mixed waste presents special problems in waste management, due to the difficulty in finding meth-ods that are compatible with all hazards.40
Treatment and Disposal Techniques Two groups of questions were used to collect data related to waste treatment and disposal techniques. One set pertained to incineration and a second set inquired about other practices.
Hospital incineration. Incineration has traditionally been a
hospital’s primary method of treating and disposing of cal waste. A 1994 report stated that approximately 6,700 medi-cal waste incinerators were still operating in U.S. hospitals,24
and a recent article reported 2,400 on-site hospital medical waste incinerators in the United States.44 When questioned
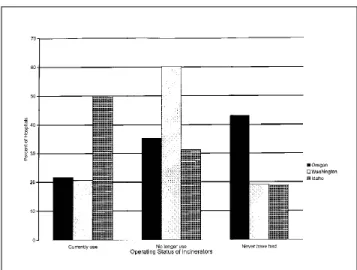
about the operating status of their hospital incinerators (cur-rently in use, no longer in use, never had), 45.7% overall in the three states reported that they had stopped operating their in-cinerators, 27.2% indicated they currently use their incinera-tors, and 27.2% reported they never had incinerators. Infor-mation about the operating status of incinerators in each of the states is presented in Figure 1. The greatest number of hos-pitals reporting that they had discontinued use of their incin-erators occurred in Washington (60.3%). This information updates the EPA report that stipulates that 60% of Washing-ton hospitals operate on-site incinerators.24 Fairly equal
num-bers of hospitals in Oregon (35.3%) and Idaho (31.2%) indi-cated that they had also discontinued use.
Hospitals were also asked to indicate the primary rea-son they were no longer operating their incinerators. Those that had stopped operating their incinerators were most likely to have taken this action within the past five years, for one of the following reasons: air pollution control re-quirements (31.3%), cost of redesigning (26.2%), federal and state waste disposal regulations (23.1%), and expen-sive maintenance (15.9%). For example, one reason con-tributing to the closure of 60.3% of Washington hospital incinerators may be due to the recent passage of stringent state regulations, such as the requirement that hospital in-cinerators may not produce any visible combustible mate-rials in incineration ash.45 In addition, local authorities in
several areas have enacted biomedical waste incineration regulations that are stricter than the state’s requirements. For example, the Puget Sound Air Pollution Control Agency requires the use of multiple chamber incinerators to burn
Figure 1. Operating status of hospital incinerators in Oregon, Washington, and Idaho.
biomedical waste.46 A third reason may be that many
in-cinerators in Washington were installed during the 1970s, and half of these incinerators had no emission control sys-tems.30 Hospitals in Washington, therefore, have been forced
to install expensive air emission control equipment to meet local and state regulations.
Similarly, hospital incinerators in Oregon must meet the specific infectious waste or crematory incinerators’ requirements that were promulgated in 1990 by the Or-egon Department of Environmental Quality.46 These
regu-lations stipulate that hospitals that operate or plan to op-erate existing incinerators constructed or modified prior to March 13, 1990, and new incinerators constructed or modified on or after March 13, 1990, must comply with several requirements, such as using Best Available Con-trol Technology (BACT) to maintain the overall highest air quality levels. The regulations also regulated air emis-sions, such as particulate materials, hydrogen chloride, sul-fur dioxide, carbon monoxide, nitrogen oxide, and opac-ity. In addition, the regulations put restrictions on the types of waste that was allowed to be incinerated; for example, no radioactive and hazardous waste was allowed to be burned in infectious waste incinerators.46 It appears,
there-fore, that the implementation of regulations may have con-tributed to a substantial reduction in the number of oper-ating on-site hospital incinerators in Oregon.
Information about the closure of incinerators in Washington and Oregon confirms studies by others who have noted that many of the smaller hospital incinera-tors built in the last decade (or even earlier) may have no pollution control devices and were designed solely to de-stroy medical pathological wastes (body parts and tis-sues).16 These units rarely meet the new federal and state
air pollution control requirements, and hospitals may be required to add air pollution control systems, or to use regional incinerators.15,43 Pollution control devices are
expensive, and the EPA is estimating that its new regula-tions will more than double the cost of medical waste disposal.29 For example, costs at existing incinerators will
sharply increase, from $168 to $390/ton.29
In addition, toxic emissions produced by incinera-tors have generated widespread public health concerns. The EPA estimates that uncontrolled medical waste in-cinerators accounted for 45% of dioxin emissions from all identified sources and approximately 25% of the total polychlorinated dibenzo-p-dioxin (PCDD) or dioxin, and polychlorinated dibenzofuran (PCDF) or furan, flux that enters the U.S. environment.29 Although these statistics
have been challenged, other dioxin-release inventories have confirmed the EPA’s finding that uncontrolled medi-cal waste incinerators have been major dioxin sources.29
Uncontrolled medical waste incinerators have also been documented to be the largest known source of mercury
emissions in the United States and significant contribu-tors of lead and cadmium emissions.29 Additional
pollut-ants emitted from these incinerators are respirable par-ticulate matter, hydrogen chloride, and other products of incomplete combustion, such as vinyl chloride, polychlo-rinated biphenyls (PCBs), chlorobenzenes, chloroform, chlorophenols, and carbon tetrachloride.29 Modern
medi-cal waste incinerators are equipped with high-efficiency Air Pollution Control Equipment (APCE) that has been demonstrated to capture particulates, neutralize acid gases, and effectively reduce toxic emissions.28 As a result,
re-sidual ash produced from the combustion system and resi-dues from APCE generally test below regulatory toxic lev-els.28 If the ash and residues, however, exceed regulatory
levels, the incineration process can be modified to chemi-cally and physichemi-cally stabilize toxic materials in the ash, thereby rendering the ash suitable for landfill disposal.28
In 1995, the EPA proposed new regulations under the Clean Air Act to reduce dioxin and heavy metal emis-sions from medical waste incinerators. The rules require medical waste incinerators to install pollution control equipment and to upgrade equipment so that combus-tion condicombus-tions meet minimum requirements for furnace temperature and residence time.47
Although we neglected to ask hospitals about the influence of public perception with regard to incin-eration closures, negative public perception associated with hospital incinerators has also made it more diffi-cult for hospitals to operate existing or install new well-controlled incinerators. Hospitals have faced many challenges in meeting stringent state (and often local) regulations and in satisfying public demands for lower emissions coming from their facilities. Thus, during the time of this study, many hospitals had switched to alternative methods. Experts supporting the use of properly designed and well-maintained, high-effi-ciency APCE systems have suggested, however, that waste disposal by alternative methods may incur risks a nd addit io nal lia bili t y.28 Fo r exa mple, off-sit e
landfilling may incur more pollution than regulated incineration facilities when transportation and final disposal are considered. When worker safety, energy, and other costs associated with waste transportation are considered, modern incinerators with APCE may be a more desirable option in terms of limiting the negative impacts on human health and improving the overall process of medical waste disposal.28
Idaho had the largest percentage of operating hospi-tal incinerators. One reason for this may be that at the date of this study, specific regulations regarding medical waste incinerators in Idaho were still being developed. Although hospitals in Idaho were required to comply with federal government requirements regarding toxic
air emissions and ambient air standards, these were usu-ally mandated only for municipal solid waste incinerators. Another factor that might have influenced these results is that hospitals in Idaho tended to be smaller in terms of average number of beds/hospital (n = 51) compared with those in Oregon (n = 72) or Washington (n = 91). It is pos-sible that less waste is generated in Idaho hospitals, which means that incinerating waste on-site remains to be a legal and cost-effective method as long as hospital incinerators are not required to update their units.48 It was suggested,
however, that the number of operating hospital incinera-tors would likely decrease when the state or federal govern-ment promulgates new medical waste incinerator require-ments.48
Other treatment and disposal techniques. Many medical
waste treatment technologies have emerged since the beach wash-up events in the late 1980s. No single tech-nology is suitable for all types of medical waste, and it is crucial for hospitals to individually select the most suit-able technologies for treatment and disposal at their fa-cilities. Important factors to be considered when choos-ing technologies include state regulatory considerations, availability of treatment and disposal methods, occupa-tional hazards, environmental impacts, effectiveness of the methods, and cost.40 Of these factors, regulatory
con-siderations and choice of methods were the main inter-ests in this study.
In all three states in this study, regulatory provisions were in place designating the state agency which had the responsibility for approval of each alternative technology for either medical or infectious waste. In Oregon, the Health Division handles issues pertaining to the storage and treatment of infectious waste, whereas the Depart-ment of EnvironDepart-mental Quality oversees the disposal of
this waste.42 In Washington, the Department of Health,
in consultation with the Department of Ecology and lo-cal health departments, is authorized to evaluate the en-vironmental and public health impacts of medical waste treatment technologies.14 Hospitals in Idaho must adhere
to regulations issued by the Department of Health and Welfare pertaining to infectious waste treatment, storage, and disposal methods, and alternative technologies may be used with the approval of the licensing agency.13
Certain alternative technologies are limited in their capacity to treat medical waste. For example, microwaving may not be used to treat body parts and animal carcasses.49
In addition, only liquid or semi-solid waste may be dis-posed of into the sewage system, under the condition that the wastewater treatment system provides secondary treat-ment and is not a combined sanitary-storm sewage sys-tem.40 The volume of waste reduced may also differ
be-tween treatments. For example, microwaving and Electro-Thermal-Deactivation(ETD) are as effective as incinera-tion in reducing the waste volume, whereas autoclaving decreases only 30% of the weight, and irradiation does not reduce the volume or weight of waste.21,40,50 In
addi-tion, several alternative technologies (such as microwaving and hydropulping) involve processes such as shredding, crushing, and steam-moistening that render the medical waste unrecognizable.21,40 The appearance of medical waste
when treated with autoclaving and irradiation, however, remains unchanged.40
Table 3 presents a range of options other than incin-eration that hospitals might use to treat medical waste, and the choices made by hospitals in the three states. Hospitals were asked to identify all methods they used in the treatment and disposal of medical waste. Per-centages, therefore, add up to greater than 100% be-cause the majority chose more than one method. The Table 3. Medical waste treatment methods, other than incineration, used by hospitals in Oregon, Washington, and Idaho.
Treatment Methods Number of Hospitals in Each State (%)a Total (%)b
Oregonc Washingtonc Idahoc
Use of Private Medical Waste-Haulers 38 (71.7%) 46 (62.2%) 15 (44.1%) 99 (61.5%) Pour into Municipal Sewage System 28 (52.8%) 34 (46.0%) 13 (38.2%) 75 (46.4%) Depositing in Landfills 25 (47.7%) 26 (35.1%) 16 (47.7%) 67 (41.6%)
Autoclaving 15 (28.3%) 24 (32.4%) 13 (38.2%) 52 (32.3%)
ETDTM (Macrowaving) 9 (17.0%) 13 (17.6%) 0 22 (13.7%)
Chemical Disinfecting or Hydropulping 6 (11.3%) 7 (9.5%) 3 (8.8%) 16 (9.9%)
Microwaving 4 (7.6%) 5 (6.8%) 0 9 (5.6%)
Grind before Pour into Municipal-Sewage System 3 (5.7%) 2 (2.7%) 1 (2.9%) 6 (3.7%)
Irradiation 0 0 0 0
a
Hospitals were asked to identify all treatment methods used, and therefore column totals for percentages are greater than 100%; b Row percentages reflect the total number of hospitals using each method (N = 161); c Column percentages reflect the total number of hospitals in each state using each method (Oregon, n = 53; Washington, n = 74; Idaho, n = 34).
most frequently reported method for all states was the use of private haulers that transport medical waste to treat-ment facilities (61.5%). The next most frequently reported techniques were pouring into municipal sewage (46.6%), depositing in landfills (41.6%), and autoclaving (32.3%). This regional information differs dramatically from the national data presented in a 1994 EPA report stating that 60% of waste was treated with on-site incineration, 20% with on-site steam sterilization, and 20% off-site treat-ment.24 Other methods adopted by hospitals included
ETD, hydropulping, microwaving, and grinding before pouring into the municipal sewer. Hospitals in Oregon and Washington used microwaving and ETDmethods to treat medical waste, while those in Idaho did not. No hospitals in either of the states reported using irradiation as a treatment technique.
As shown in Table 3, almost two-thirds (71.7%) of hospitals in Oregon indicated they used private haulers, and nearly half (47.7%) also stated their waste was depos-ited in landfills. It is not clear from the results if respon-dents knew how private haulers actually disposed of medi-cal waste once it was treated, but we assume that hospi-tals in Oregon were aware that landfills no longer accept untreated infectious waste.12,13,45 A large quantity of
medi-cal waste, therefore, is hauled to regional municipal solid waste (MSW) incinerators, and the resultant ash is depos-ited in a monofill. Respondents who were aware of this entire process may have (accurately) indicated that both methods were used.
Landfill disposal, which was also a common choice for hospitals in all three states, is considered to be a vi-able option to dispose of general solid waste, such as in-cineration ash, sharps, pathological waste, red bags, and hazardous chemical waste.40 Many commercially operated
landfills treat medical waste as “special waste” with han-dling practices similar to requirements for asbestos.16
Al-though concerns have arisen about groundwater contami-nation from medical waste contained in a landfill, be-cause medical waste is neither a major portion of solid waste deposited in sanitary landfills, nor does it contain significantly higher numbers of microorganisms than municipal solid waste, reports have concluded that addi-tional microorganism loading to aquifer systems from properly managed landfills is unlikely if the leachate is collected and controlled.16 An alternative method that
some hospitals may have used is to first treat medical waste on-site by autoclaving and then have it transported to a MSW landfill.
Pouring waste into the municipal sanitary sewer sys-tem has also been demonstrated to be a convenient and inexpensive technique for liquid and semi-liquid medical wastes, and as evidenced in Table 3, was used by 46.4% of the hospitals. This particular method was more popular
among hospitals in Oregon (52.8%) and Washington (46.0%), and less frequently used in Idaho (38.2%). Be-cause hospitals were asked to identify all treatment meth-ods used, these percentages reflect the total number of hospitals in each state using this method, and therefore add up to greater than 100%. Medical waste typically dis-charged to the sanitary sewer system by hospitals includes blood and blood products and pathological wastes. These materials constitute a small portion of the sanitary sewer discharges, and are diluted by the large amounts of resi-dential sewage to well below the concentration needed for bloodborne disease transmission.16 Sewage treatment
facilities accepting medical waste must meet the regula-tory requirements of local sewer authorities, including provision of secondary treatment followed by disinfec-tion.7,12,32, In addition, these plants may not function as
combined sewage systems.7,40
Approximately a third (32.3%) of the hospitals con-tinue to use “traditional” medical waste treatment tech-niques, such as steam sterilization (autoclaving) to disin-fect or dispose of some types of waste.7,21,40 Steam
steril-ization (using an autoclave or a retort) is a process in which pressurized steam is heated to a high temperature (240– 280 °F) for a period of time sufficient to kill infectious agents.7 Despite low rates of waste reduction, steam
ster-ilization is commonly used as either a backup treatment, or as a pretreatment technique prior to transportation to incineration facilities or disposal in sanitary landfills. A recent report, however, indicates that autoclaving and microwaving are fully adequate disinfection technologies, and that these techniques, if followed by shredding, can reduce volume by 60–80%.29
ETD(also called macrowaving) is a relatively new waste treatment technology in which waste is placed in sealed, insulated containers and then exposed to a high strength oscillating electrical field generated by low-fre-quency radiowaves.50,51 Medical waste directly absorbs the
energy and heat at a temperature of 90–100 °C. Even though the heating process of ETDis similar to that of microwaving, electrical wave lengths of ETDare longer, making the preshredding processes unnecessary. After medical waste is treated with ETD, recyclable plastics and syringes are separated and transported to plastics recy-cling companies. Non-recyclable materials are shredded and disposed of in landfills as regular solid waste.50,51 The
ETDtechnique offers several advantages in that plastics from treated sharps can be recycled, and ETDmay be ap-plied to nearly all types of medical waste. ETDis a copy-righted technology owned by Stericycle Company and is available in limited geographical areas.50,51
Approximately 10% of the hospitals used hydropulping as a treatment method. Hydropulping is an oxidation technique in which solid and liquid waste
are first mixed together; the waste is then shredded and pulverized by a hammer mill, and finally sprayed with disinfecting agents such as chlorine.16,21 The ground solid
waste is then disposed of in landfills and the chlorine in the liquid waste is extracted before discharge into the sewer.22 This technique reduces the volume of solid waste
by 30%.22
As seen in Table 3, microwave technology was used by fewer than 6% of hospitals in Oregon and Washing-ton, and none in Idaho. This technique has also only re-cently been introduced into the U.S. medical waste treat-ment market as a decontamination process for waste con-taining blood, secretions, bandages, and hypodermic needles.16 Waste material is crushed, shredded and
steam-moistened so that it is reduced to small wet particles which are then exposed to microwaves until decontamination temperatures are achieved. As with hydropulping and grinding, this treatment must be conducted under nega-tive pressure to avoid producing aerosols.16 The resulting
materials are disposed of in landfills or used as fuel. Microwaving usually reduces the volume (by a ratio of 8:1), but not weight, of waste material.21 It has also been
touted to present no air emission problems.21,52
No hospitals reported using irradiation, which is con-sistent with other reports that suggest that irradiation is seldom used to treat medical waste and equipment in hospitals because it is more expensive than other tech-niques and poses serious disadvantages. For example, ul-traviolet (UV) light sterilizes the surface area but does not penetrate most materials.40 On the other hand,
irradia-tion using Cobalt-60 is more penetrative, but also gener-ates radioactive wastes and is a technology requiring highly trained operators.7,16,40
In summary, and as others have noted, we found that hospitals appeared to select the technologies most suit-able for their particular facilities, considering such fac-tors as regulatory requirements, operating concerns, ap-plicability, effects of treatment on the waste, occupational hazards, environmental impacts, and costs.40
On-site and off-site methods. Figure 2 shows that certain
methods appear as on-site treatments while others were more apt to be performed at off-site locations. For example, conventional methods, such as autoclaving, using chemi-cal disinfectants or hydropulping, and pouring into the municipal sewage system, were often performed on-site in hospitals. On the other hand, new treatment techniques (such as microwaving and ETD) were shipped to off-site facilities.
These results are similar to other research that has shown that typical off-site treatment methods include contracting with waste management companies and the use of regional facilities.40 A regional facility is another
type of off-site treatment option for hospitals. With this option, one hospital owns a medical waste treatment fa-cility and accepts waste from other generators in the same area. For example, several hospitals in Oregon and Idaho commented in the survey that they sent medical waste to be incinerated at other hospitals. As was demonstrated by the data in Table 3 and Figure 2, hospitals have in-creasingly chosen to contract the services of a waste man-agement company for off-site treatment and disposal of medical waste. Hospitals may segregate and package the waste; contracted waste companies then transport, store, treat, and dispose of the waste.40 Hospitals, however, are
liable for waste generated and the harm from waste when it is disposed of or treated improperly, so are likely to be very careful when selecting contracted companies.40
CONCLUSIONS AND RECOMMENDATIONS
Numerous federal and state agencies and other organiza-tions have established regulaorganiza-tions and standards pertain-ing to medical waste, and regulate its treatment and dis-posal in Oregon, Washington, and Idaho. The majority of hospitals used state regulations to define and manage their infectious waste, and nearly all also adopted infec-tious waste definitions from other agencies or organizations, such as the EPA, CDC, OSHA, JCAHO, AMA, and APIC.
Hospitals considered more types of medical waste to be infectious than is required by state regulatory defini-tions. Six types of medical waste were generally catego-rized as infectious waste by hospitals in Oregon, Wash-ington, and Idaho: blood specimens and blood products, all sharps, microbiology laboratory waste, pathological waste, body parts, and waste from surgery rooms. The re-sults implied that there was no consensus about which agency or organization’s definition of infectious waste should be used in waste management programs. As a re-sult, hospitals may be treating a portion of the hospital-generated waste as infectious waste, when it might be treated with less rigor and with less cost. Confusion around
Figure 2. Number of hospitals using on-site and off-site treatment methods.
the definition of infectious waste may also have contrib-uted to the finding that almost half of the hospitals are not segregating infectious waste from other medical waste. The most frequently used practice of treating and dis-posing of medical waste was the hiring of private medical waste haulers to treat waste off-site, which usually resulted in off-site incineration at municipal solid waste incinera-tors. Another common practice included the use of off-site landfills. Less frequent off-off-site treatment techniques were microwaving and Electro-Thermal-Deactivation (ETD). Frequently used on-site medical waste treatment techniques included autoclaving and pouring waste into the municipal sewage system. Most hospitals in Oregon and Washington no longer operate their incinerators due to more stringent regulations regarding air pollution emis-sions. Hospitals in Idaho, however, are currently operat-ing incinerators in the absence of state regulations spe-cific to these types of facilities.
We offer the following recommendations based on this study:
• Federal or state agencies should draft universal defi-nitions of infectious waste with input from waste management companies, hospitals, and accredita-tion organizaaccredita-tions. The adopaccredita-tion of a universal defi-nition will likely make the process of separating in-fectious waste from other less regulated medical waste less confusing, and contribute to a decrease in the volume of waste as well as a reduction in waste management costs.
• Waste management hierarchy programs (reduce, re-use, recycle) should be instituted in all hospitals as an overall policy to reduce both the quantity and toxicity of waste generated. We agree with others who have suggested that such programs first con-duct waste audits and then seek to use techniques that satisfy both criteria.23,29 For example,
adminis-trators may promote reuse, recycling, and the use of substitute materials or chemicals in their facilities. Substituting reusable materials for disposable prod-ucts, such as linens, gowns, draping, bedpans, or food service equipment, may be done without compro-mising sanitary concerns, and may result in a con-siderable reduction in waste and costs of treating the waste.29 For example, an innovative material
called OREXproduced by Isolyser Corporation, is used to make products that perform like traditional disposables, but can be dissolved in water after use rather than being deposited in a landfill or inciner-ated.44 OREXis made from hot-water-soluble
poly-vinyl alcohol (PVA), a nontoxic synthetic polymer. PVA is biodegradable in sewage treatment facilities and the final products of degraded PVA are carbon dioxide and water.44
Also, whenever possible and feasible, hospitals should decrease the amount of disposable items and plastics that contribute to toxic emissions of diox-ins, heavy metals, and volatile organic compounds to reduce the volatile organic compounds produced by incinerators. These waste management strategies, however, must balance the need to conserve re-sources with the need to protect against communi-cable disease transmission.
• A similar study might be conducted in other types of healthcare facilities, such as long-term care facili-ties, dentist, and physician offices, which also pro-duce large volumes of medical and infectious waste. Interesting results may arise from a study that com-pares medical waste management and treatment techniques used in different types of hospitals and in other geographic regions of the United States. For example, comparisons about management practices might be made between profit and nonprofit hospi-tals, between research and non-research hospihospi-tals, and between hospitals located in the Pacific North-west and those in other geographical areas. • Finally, it is recommended that the environmental
impact and efficiency of new techniques such as ETD and OREXbe assessed as alternative methods for widespread use.
REFERENCES
1. Council on Scientific Affairs. J. Am. Med. Assoc. 1989, 262, 1669-1671. 2. Gellerman, B. What’s New in Handling Infectious Materials: The Sudden Rise of the Red-Bag Business. The New York Times, March 27, 1988, p 15. 3. Baker, J. Blood in the Water: A Tide of Hospital Waste.” Newsweek,
July 18, 1988, p 35.
4. Bussey, J.; Sheet, K.; Gest, T.; Taylor, R.; Sandford, G. Garbage Out, Garbage In. US News World Rep., July 18, 1988, p 9.
5. Morganthau, T.; Hager, M.; Brown, L.; Kenny, T.; Drew, L. Don’t Go Near the Water. Newsweek, August 1, 1988, pp 43-47.
6. Hershkowitz, A. Tech. Rev. 1990, 93, 35-40.
7. EPA Guide for Infectious Waste Management; U.S. Environmental Protection
Agency. Office of Solid Waste and Emergency Response. U.S. Government Printing Office: Washington, DC, 1986; EPA/ 536-W-86-014.
8. Centers for Disease Control and Prevention. Morbidity and Mortality
Weekly Report 1987, 36(suppl. 2), 1s-18s.
9. Bloodborne Pathogens. Code of Federal Regulations, Part 1910, Title 29, Section 1030, 1995.
10. Fed. Regist. 1993, 58, 37778.
11. O’Neale, M. Assoc. of Operating Room Nurses J. 1992, 55(3), 855-860. 12. “Oregon Revised Statute”; Legislative Council Committee: State of
Or-egon, 1995; Vol. 8, Title 39 (Public Health and Safety), Chapter 459.386-459.405 (Infectious Waste Disposal); ORS 459.386-459.386-459.405 (1995). 13. Rules, Regulations, and Minimum Standards for Hospitals in Idaho;
Bu-reau of Facility Standards; Idaho Department of Health and Welfare: Boise, ID, 1990.
14. “Revised Code of Washington”; Statute Law Committee: State of Washington, 1992; Title 70, Chapter 95 (Biomedical Waste), Chapter 95.010; RCW 70.95k.010 (1992).
15. Green, A.E.S. In Medical Waste Incinerators and Pollution Prevention; Green, A.E.S., Ed.; Van Nostrand Reinhold: New York, 1992; pp 107-204. 16. The Public Health Implications of Medical Waste: A Report to Congress;
U.S. Department of Health and Human Services. Agency for Toxic Substances and Disease Registry: Atlanta, GA, 1990.
17. Wagner, W.M. Today’s Operating Room Nurse 1991, 13(4), 24-27. 18. Byrns, G.; Burke, T. J. Environ. Health 1992, 55(3), 12-14. 19. Burke, E.L. J. Environ. Health 1994, 56(9), 11-14.
20. Rutala, W.A. Infection Control Hospital Epidemiology 1992, 13(1), 38-48. 21. Cross, F.L.; Hesketh, H.E.; Rykowski, P.K. Infectious Waste Management;
Technomic Publishing: Lancaster, PA, 1990, pp 1-33. 22. Cross, F.L. Pollut. Eng. 1990, 22, 68-73.
23. Garvin, M.L. Infectious Waste Management: A Practical Guide; Lewis: Boca Raton, FL, 1995; pp 11-15.
24. Medical Waste Incinerators-Background Information for Proposed Standards and
Guidelines: Industry Profile Report for New and Existing Facilities; U.S.
Envi-ronmental Protection Agency. Office of Air Quality Planning and Stan-dards: Research Triangle Park, NC, 1994; EPA-453/R-94-042a.
25. Hagland, M.M. Hospitals 1993, January, 17-24.
26. Cruz, L.D. Assoc. Operating Room Nurses J. 1992, 55(3), 855-862. 27. Medical Waste Tracking Act of 1988. Public Law 100–582, 1988; Code
of Federal Regulations, Section 6992 et seq.
28. Medical Waste Committee, Air & Waste Management Association. J
Air & Waste Manage. Assoc. 1994, 44, 1176-1179.
29. Thornton, J.; McCally, M.; Orris, P.; Weinberg, J. Public Health Rep.
1996, 111, 298-313.
30. Turnberg, W.L. Survey of Infectious Waste Management Practices
Con-ducted by Medical Facilities in Washington State; Washington State
In-fectious Waste Project, Attachment 2; Washington Department of Ecology: Olympia, WA, 1989.
31. Boatright, D.T.; Edwards, A.J.; Shaver, K.A. J. Environ. Health 1995,
57(8), 15-18.
32. Uzych, L. J. Environ. Health 1990, 52(4), 233-235.
33. Rodenbeck, S.E.; Lichtveld, M.Y. J. Environ. Health 1990, 53(1), 30-31. 34. Turnberg, W.L.; Frost, F. Am. J. Public Health 1990, 80(10), 1262-1264. 35. Turnberg, W.L. J. Environ. Health 1991, 53(6), 21-25.
36. Rutala, W.A.; Odette, R.L.; Samsa, G.P. J. Am. Med. Assoc. 1989, 262(12), 1635-1640.
37. 1992 Guide to the Healthcare Field; American Hospital Association: Chicago, IL, 1992.
38. Statgraphics: Statistical Graphics System Version 5.0; Statistical Graphics Corporation: Rockville, MD, 1985.
39. Seminar Publication, Medical and Institutional Waste Incineration:
Regu-lations, Management, Technology, Emissions, and Operations, U.S.
Envi-ronmental Protection Agency. Office of Research and Development. U.S. Government Printing Office: Washington, DC, 1991; EPA/625/ 4-91/030.
40. Reinhardt, P.A.; Gordon, J.G. Infectious and Medical Waste
Management; Lewis: Ann Arbor, MI, 1991.
41. Definition of Hazardous Waste. Code of Federal Regulations, Part 261, Title 40 Section 3, 1995.
42. Oregon Administrative Rules, Division 18-Health Division (Infectious Waste), 1995; Chapter 333-050; OAR 333-18-050 (1995).
43. Fay, M.F.; Beck, W.C.; Fay, J.M.; Kessinger, M.K. Assoc. Operating Room
Nurses J. 1990, 51(6), 1493-1508.
44. Fisher, B.E. Environ. Health Perspectives 1996, 104(7), 708-710. 45. Summary Packet of Information Prepared to Identify Requirements that
Affect Biomedical Waste Management in Washington State; Washington
Department of Ecology: Olympia, WA, 1993.
About the Authors
Pornwipa Klangsin obtained her M.S. degree in Environmen-tal Health Management in 1994 from Oregon State Univer-sity, Corvallis. She is currently a Ph.D. candidate in Environ-mental Health Sciences at the University of Michigan School of Public Health in Ann Arbor. Anna K. Harding is an Associ-ate Professor in Environmental Health in the Department of Public Health, and coordinates the Environmental Health and Safety Program at Oregon State University. Dr. Harding’s re-search is focused on environmental contamination and pub-lic health interventions. Correspondence should be directed to Anna Harding, Department of Public Health, Waldo Hall 309, Oregon State University, Corvallis, OR 97331-6406, or e-mail: hardinga@ccmail.orst.edu.
46. Oregon Administrative Rules, Division 25-Department of Environmen-tal Quality (Incinerator Regulations), 1994; Chapter 850 to 340-905; OAR 340-25-850 (1994).
47. Federal Regist. 1995, 60, 10654-10691.
48. Pitman, D. Idaho Division of Environmental Quality, Boise, ID. Per-sonal communication, 1994.
49. Medical Waste Management and Disposal; U.S. Environmental Protec-tion Agency. Office of Solid Waste. Noyes Data: Park Ridge, NJ, 1991. 50. Johnson, R. Stericycle Company, Pacific Northwest Facility, Morton,
WA. Personal communication, 1994.
51. Spurgin, R.A. Plant Technol. & Safety Manage. Ser. 1991, 2, 13-17. 52. Rubin, D.K.; Buckner, M.; Boyle, B. Eng. News Record 1991, 226(1), 26-27.