Recruitment and Retention of
Community Preceptors
Michael S. Ryan, MD, MEHP, a Lisa E. Leggio, MD, b Christopher B. Peltier, MD, c Archana Chatterjee, MD, d Steven Arenberg, MS, e
Julie S. Byerley, MD, f Julia L. Belkowitz, MD, g Gerard P. Rabalais, MD, MHA, h Michael A. Barone, MD, MPHi
BACKGROUND: Recruiting and retaining community-based pediatricians for teaching medical
students has been explored through the lens of preceptors and educational leaders. The purpose of this study was to explore the perspective of pediatric department chairs, a key stakeholder group charged with maintaining teaching capacity among a faculty.
METHODS: In 2015, members of the Association of Medical School Pediatric Department Chairs
and Council on Medical Student Education in Pediatrics joint task force disseminated a 20-item survey to pediatric department chairs in the United States and Canada. Topics included demographics, incentives offered to community pediatricians, and the perceived value and feasibility of such incentives. Data were analyzed using descriptive statistics and
χ2 to compare categorical variables.
RESULTS: Pediatric department chairs from 92 of 145 (63% response rate) medical schools
returned the survey. Sixty-seven percent reported difficulty recruiting or retaining preceptors, and 51% reported high-reliance on preceptors for the ambulatory portion of the pediatrics clerkship. Almost all (92%) cited competition from other programs for the services of community preceptors. The provision of incentives was correlated with perceived feasibility (R2 = 0.65) but not their perceived value (R2 = 0.12). Few (21%) chairs
reported providing financial compensation to preceptors. The provision of compensation was not related to reliance but did vary significantly by geographical region (P < .001).
CONCLUSIONS: Pediatric departments rely heavily on community-based pediatricians but face
competition from internal and external training programs. The perspective of department chairs is valuable in weighing interventions to facilitate continued recruitment and retention of community preceptors.
abstract
aDepartment of Pediatrics, School of Medicine, Virginia Commonwealth University, Richmond, Virginia; bDepartment of Pediatrics, Medical College of Georgia, Augusta University, Augusta, Georgia; cDepartment of Pediatrics, College of Medicine, University of Cincinnati, Cincinnati, Ohio; dDepartment of Pediatrics, Sanford School of Medicine, University of South Dakota, Vermillion, South Dakota; Departments of iPediatrics and eMarketing and Communications, School of Medicine, Johns Hopkins University, Baltimore, Maryland; fDepartment of Pediatrics, University of North Carolina at Chapel Hill, Chapel Hill, North Carolina; gDepartment of Pediatrics, Miller School of Medicine, University of Miami, Miami, Florida; and hDepartment of Pediatrics, School of Medicine, University of Louisville, Louisville, Kentucky
Dr Ryan conceptualized and designed the study, designed the data collection instrument, conducted data analysis, drafted the initial manuscript, critically reviewed the manuscript for important intellectual content, and revised the manuscript; Dr Barone conceptualized and designed the study, designed the data collection instrument, coordinated and supervised data collection, conducted data analysis, drafted the initial manuscript, critically reviewed the manuscript for important intellectual content, and revised the manuscript; Mr Arenberg designed the data collection instrument, collected data, coordinated and supervised data collection, carried out the initial analyses, critically reviewed the manuscript for important intellectual content, and revised the manuscript; Drs Leggio, Peltier, Chatterjee, Byerley, Belkowitz, and Rabalais conceptualized and designed the study, designed the data collection instrument, drafted
WHAT’S KNOWN ON THIS SUBJECT: The challenges of increased clinical productivity demands and the electronic health record have caused volunteer community clinical preceptors to limit or eliminate their teaching commitment, resulting in a critical shortage of available community faculty to teach trainees.
WHAT THIS STUDY ADDS: The scope of the preceptor crisis is further defined from the perspective of pediatric department chairs. Perceptions of the perceived value and feasibility of interventions will allow departments to employ effective strategies in dealing with a critical shortage of community teachers.
For >100 years, third-year medical students have been taught by community pediatricians in the ambulatory setting.1 This setting
affords learners many opportunities beyond the inpatient or university-based model of education, including exposure to primary care, the
business of medicine, continuity of care, and the medical home model.1–4
The value of community-based ambulatory experiences has been TABLE 1 Characteristics of Respondents’ Departments by AAMC Region
Characteristics AAMC Region
Northeast (n = 20) Central (n = 28) South (n = 27) West (n = 10) Canadian (n = 5) Total (n = 90)
Response rate, % 53 64 57 45 45 59
No. full-time faculty, n (%)
<50 1 (5) 10 (36) 7 (26) 0 (0) 1 (20) 19 (21)
50–99 5 (25) 5 (18) 7 (26) 1 (11) 0 (0) 18 (20)
100–149 5 (25) 5 (18) 3 (11) 1 (11) 1 (20) 15 (17)
≥150 9 (45) 8 (29) 10 (37) 7 (78) 3 (60) 37 (42)
Class size, mean (SD) 148 (46) 126 (69) 144 (48) 137 (55) 195 (82) 142 (59)
Pediatrics residency
Present, % 100 86 93 100 100 94
Size, mean (SD)a 21.2 (13) 17.6 (11) 15.0 (6.4) 25.0 (9.3) 12.6 (4.5) 18.0 (10)
High reliance on community preceptors, %
65 64 30 50 40 51
Difficulty recruiting or retaining preceptors, %
60 75 64 67 60 67
Total programs competing for preceptors, %
0 14 4 9 11 0 8
1–3 21 32 27 22 100 32
3–5 29 48 50 67 0 44
>5 36 16 14 0 0 16
Provides a stipend to preceptors, %b 20 25 5 0 100 20
The number of responses to each question varied because of omissions from respondents. No other comparisons were statistically significant.
a Analysis of variance between groups was statistically significant for the residency program size (F = 2.7; P = .04). b Pearson’s χ2 was statistically significant for the provision of stipends to preceptors (χ2 = 24.9; P < .001).
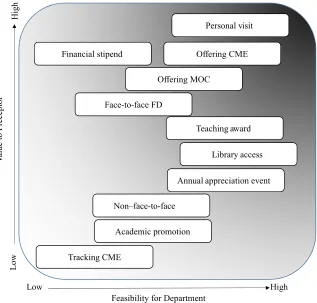
FIGURE 1
further endorsed by the Association of American Medical Colleges (AAMC) and the Liaison Committee on Medical Education (LCME), each of which require institutions to provide these opportunities for students.5, 6
Despite the advantages of community-based ambulatory experiences, growing concern has been expressed over the continuation of this model of education.4, 7 The
term “community preceptor crisis, ”4
has been used to reflect increasing competition for clinical sites, 7 the
proliferation and burden of the electronic health record, 4, 8 and an
increased administrative educational burden to complete meaningful assessment of learners, 4, 9 all of
which threaten the sustainability of relationships between medical education programs and community physicians.
To describe the scope of this problem, the AAMC in conjunction with other professional organizations recently surveyed deans of programs that grant Doctor of Medicine (MD) degrees in the United States. Pediatrics was cited as the field in which they reported the greatest difficulty in finding core clinical sites. Commenting specifically about preceptor shortages in all specialties, 84% of respondents shared that they were moderately to very concerned
about the supply of primary care preceptors.7
Recently, the Alliance for Clinical Education proposed several strategies to maintain or improve teaching opportunities
in community-based settings.4
Two key strategies involve the provision of financial compensation or faculty development for
preceptors who engage in teaching.4
There is substantial literature FIGURE 2
Relationship between feasibility and provision of each incentive. 1, Financial stipend; 2, Offer MOC; 3, Track CME; 4, Annual event; 5, Non face-to-face faculty development; 6, Face-to-face faculty development; 7, Offer CME; 8, Promotion; 9, Personal Visit; 10, Teaching award; 11, Library access.
FIGURE 3
that supports the value of both financial compensation9–11
and faculty-development opportunities.12–15 Financial
compensation in particular has become a more common practice7
and may involve direct compensation or, in some cases, tax credits.16
Advantages of such incentive programs have been well described from the perspective of preceptors themselves9–11, 17, 18 and educational
leaders.4, 12, 15 However, in most
medical schools, the implementation of these initiatives requires a collaboration between the medical school and the clinical departmental leadership, often including
the clerkship director and the department chair. In recognition of this collaborative process, the leadership of both the Association of Medical School Pediatric Department Chairs (AMSPDC) and the Council on Medical Student Education in Pediatrics (COMSEP) created a joint task force to address concerns over the sustainability of community preceptorship programs and determine the feasibility of incentive programs. The task force recognized that although substantial literature has been devoted toward describing solutions to this issue from the perspective of many stakeholders, the perspective of department chairs had not been previously described. To assess the feasibility of incentive programs, it is imperative to understand the viewpoint of this key stakeholder group because department chairs often provide direct compensation and/or endorse faculty-development programs. Our purpose in this study was to explore the perspective of pediatric department chairs with respect to recruiting and retaining community-based preceptors. In particular, we were interested in determining current practices and perception of the feasibility and value of providing both financial and faculty-development incentives to improve
the recruitment and retention of community preceptors.
METHODS
AMSPDC and COMSEP Joint Task Force
In 2015, the leadership of AMSPDC and COMSEP recruited a joint task force to address issues that pertain to the recruitment and retention of community-based preceptors. The resultant task force consisted of 11 members: 5 members from AMSPDC and 6 members from COMSEP. The task force was cochaired by 1 member each from AMSPDC (G.R.) and COMSEP (L.E.L.). The task force reviewed the available literature on community preceptors and recently provided a summary of these findings in a manuscript.19
To address a gap in understanding the perspective of department chairs, we developed a survey instrument, which was constructed on the basis of previous studies that were related to preceptor recruitment9–14, 17, 18 as
well as the perspectives of the task force membership.
Instrument
A 20-item survey instrument was developed, which consisted of 4 sections: (1) demographics, (2) benefits and support for teaching, (3) stipends, and (4) faculty development. The demographic section included questions related to program or departmental size, geographic region, and current competition for community-based preceptors. If a participant indicated that he or she did not rely on community preceptors at all, branching logic was used to instruct the participant to submit the survey at that point.
The benefits and support for teaching section provided a list of potential benefits to preceptors
and asked respondents to indicate whether each benefit was currently provided. Specific topics that were addressed in this section included personal visits, faculty development, continuing medical education (CME), incentives, and awards or recognition programs. The term, “personal visits, ” was selected to specifically represent orientation to medical school expectations as previously described by Christner et al4, which
may be provided separately or in conjunction with face-to-face faculty-development efforts. In addition to inquiring about offering CME, the survey asked about tracking CME to recognize how departments may choose to track and provide documentation of attendance in live or recorded local CME offerings, such as grand rounds.
Respondents were then asked to rate each benefit’s relative value to preceptors and feasibility from the departmental perspective. The stipends section asked respondents to indicate their current practice in regard to providing financial support for preceptors. If a
participant responded affirmatively to providing financial support, additional questions were asked to determine the amount of funding and its source. Finally, the faculty-development section provided a list of faculty-development topics (eg, giving feedback, working with a student in difficulty, etc) and asked respondents to indicate whether those opportunities were currently provided. Survey questions were pilot tested with the 20 department chairs from the AMSPDC Education Committee. No formal validation studies were performed beyond pilot testing and subsequent refinement. The final surveys were uploaded to Verint software (Verint Systems, Melville, NY).
Participants and Setting
pediatric department chairs of 145 MD-granting medical schools in the United States and Canada. A cover letter signed by the presidents of AMSPDC and COMSEP was sent with an electronic link to each of the potential participants. Department chairs were encouraged to complete the survey with his or her respective pediatric clerkship director whenever possible to ensure the accuracy of the responses. Participants were able to omit responses to any question(s) at their discretion. The survey was open for 6 weeks, and reminders were sent to nonrespondents at 1- to 2-week intervals until the survey was closed. A maximum of 5 e-mail invitations were sent.
Data Analysis
We calculated descriptive statistics for the demographic variables, faculty-development opportunities, and presence of benefits and stipends. An analysis was performed on all responses even if surveys were returned incomplete. This was done to accommodate for branching logic omission (eg, if a participant did not use community preceptors, the survey concluded) and/or participant-driven omission of responses to individual questions. A Pearson’s χ2 analysis was performed to make
comparisons between categorical variables by volume of learners and faculty, geographic region (by using AAMC regions as reference), financial stipends, difficulty recruiting and retaining preceptors, and reliance on preceptors. Geographic region (as designated by AAMC) was chosen as an important variable on the basis of a possible correlation with population size and/or educational program density and therefore a potential factor in competition for preceptors. Significance was set at
P < .05. All analyses were performed by using IBM SPSS Statistics Premium version 23 (IBM SPSS Statistics, IBM Corporation, Armonk, NY). This study was deemed exempt by the Johns
Hopkins University School of Medicine Institutional Review Board.
RESULTS
Department chairs from 92 of the 145 surveyed medical schools represented by AMSPDC returned the survey (63% response rate). The response rate for individual questions varied on the basis of omission of response(s) to individual questions that resulted from either automated or branching logic or participant-driven omission. Because of this, the denominator for individual responses varied.
Chairs were asked to designate their department’s region (on the basis of AAMC), and 98% of respondents did so (90 of 92). A summary of major findings by region is presented in Table 1. We received the highest response rate from those pediatric departments that are affiliated with AAMC central medical schools (64%). These schools tended to have smaller mean class sizes than schools in other regions, although this difference was not statistically significant (P = .18). Most departments (94%) reported the presence of an internally supported residency program. Canadian and Southern departments had significantly smaller residency program sizes compared with other regions (P = .04).
Overall, 51% (46 of 90) of
department chairs stated that they were highly reliant on community preceptors in the ambulatory portion of their pediatric clerkship. When viewed by region, there was a trend toward schools in the Southern region reporting that they had less reliance on community preceptors in their pediatric clerkship (P = .06). No statistically significant differences were found with respect to reliance when analyzing medical schools by class size (P = .54), provision of financial stipends (P = .59), or
competition from other programs (P = .32). Among departments with residency programs, nearly 50% of chairs stated that they were heavily reliant on community preceptors for pediatric clerkship teaching. There were no significant differences on the basis of residency class size (P = .16). Overall, 67% of department chairs responded, “Yes” to the question, “Is your program having difficulty recruiting or retaining community preceptors in the pediatric
clerkship?” There was no significant difference by region (P = .87).
reported competition from students attending non–LCME-accredited medical schools, including offshore medical schools, those in the Central region were most likely to state this competition. Overall, 92% (69 of 75) of responding chairs cited competition from other programs. We explored the provision of incentives to preceptors for teaching. The provision of financial incentives differed significantly by region (P < .001). All Canadian schools reported the granting of stipends whereas no responding schools in the West reported doing so. There were no other significant differences in the provision of stipends to community preceptors on the basis of difficulty in recruiting or retaining preceptors (P = .69), medical student class size (P = .48), or number of full-time departmental faculty (P = .43). Of stipends provided, respondents reported that these ranged from $15 per student per day to as much as $500 per student per week. Of those who reported providing a stipend, 13 indicated a particular funding stream, 77% of which came from the school of medicine exclusively or in combination with the department. Among the reasons cited for not providing a stipend, responses such as limited resources and setting a precedent that would be difficult to maintain were noted. Nearly 50% (27 of 57) of respondents reported that competing programs offered a stipend. In the survey item, it was not specified whether financial stipends to preceptors were more frequent from internal or external competitive programs.
The most common incentives that were offered were access to the library (84%), eligibility for teaching awards (75%), personal visits (74%), and sponsoring faculty for academic advancement (72%). The least common incentives that were offered were financial stipends (21%), Maintenance of Certification (MOC)
(28%), tracking CME (35%), and annual appreciation event(s) (40%). Finally, we asked respondents to comment on both the perceived value and feasibility of various incentives. Financial stipends and offering MOC were rated as the highest value incentives but were also depicted as those with the lowest feasibility. Incentives such as a personal visit, eligibility for a teaching award, and access to the university library scored highest in terms of both their relative perceived value and feasibility. A summary of these findings is depicted in Fig 1.
Figure 2 illustrates the relationship between percentage of department chairs who report providing each incentive and the percentage of chairs who report the incentive as high value or high feasibility, respectively. As shown on this figure, there was a moderate to strong positive correlation (R2 = 0.65) between the current
provision of incentives and high perceived feasibility. There was a weak negative to no correlation (R2 = 0.12) between the provision of
incentives and high perceived value.
DISCUSSION
A task force of representatives from COMSEP and AMSPDC undertook this study to examine how pediatric department chairs recruit and retain the valued resource of preceptors to teach medical students. We also aimed to assess the value and feasibility for different methods to be considered, with the goal of supporting the development of organizational guidelines to address this challenge. Although authors of several previous studies have similarly described the reliance on community preceptors4, 7 and have
identified the value of incentives to preceptors themselves, 9–11, 20, 21
we are the first to address the
feasibility of such incentives from the perspective of the departmental leaders: a group often responsible for providing or supporting such incentive programs. Combined with the perspectives of medical education leaders and preceptors themselves, these findings may offer additional insight into the relative merit of recruitment and retention programs.
In this survey, half of pediatric department chairs reported a heavy reliance on community preceptors, although this finding varied by region. The regional variation may be secondary to the relatively close geographical proximity and therefore to the increased competition between medical schools within the northeast and central regions when compared with other regions. Overall,
many chairs endorsed significant competition for these preceptors from multiple sites, both within and outside of their institutions, and over two-thirds of the chairs in this study acknowledged having difficulties in recruiting and retaining preceptors. Given the growing number of medical students through new medical schools, the expanded class sizes and regional medical campuses, 22
and the intentional increased use of the community-based distributive medical education model in an effort to train future physicians to meet the demands of the changing health care delivery system, 23 the perceived
competition will likely intensify with time. An understanding of both the motivating factors for preceptor participation and the realities of what medical schools can deliver are key to developing solutions to address this issue.
In our study, chairs reported that providing financial stipends was the least common incentive offered but may be of the highest value to preceptors. Whether preceptors themselves agree with this sentiment is unclear. Several previous
compensation may be less important to preceptors than intrinsic rewards (eg, personal satisfaction, feedback from learners, etc).17, 24–27 However,
more recent studies contradict those findings.9, 10, 21, 28 These more recent
findings coupled with the perspective of department chairs from our study may suggest a shift in perceived value of compensation for modern community preceptors.
Despite the high perceived value of financial stipends, chairs reported that financial stipends were the least feasible benefit. Although this study did not identify the rationale for the chairs’ rankings of feasibility and value of preceptor rewards, we hypothesize that the low feasibility of financial reward for preceptors is due to the tight financial constraints faced by many pediatric departments. Other costly incentives, such as departments offering MOC, were also less likely to be currently provided, as shown in Fig 2. On average, pediatrician salaries are lower than all other physician salaries.29 To compensate
for paying community preceptors, pediatric department chairs could be faced with shifting scarce resources, which could have a negative impact on departmental salaries and educational programming. The decision to fund community preceptors directly (through medical school tuition dollars) is often not within the purview of pediatric department chairs. The arguments that surround justified payment (or not) to the critical teaching workforce of community preceptors reveal the high cost structure and competing demands for resources within academic medical centers. Interestingly, more pediatric department chairs in this study report that their competitors offered stipends rather than provide stipends themselves. It is unclear whether this is a misperception by department chairs about the rewards offered to preceptors in a community,
a sign of the strong competition from non–medical school training programs, or a result of response bias. Existing literature suggests that this is indeed a real finding. Whereas deans from MD programs have reported only rarely providing financial support, 71% of deans from osteopathic medical school programs and 20% of deans from of physician assistant programs in the United States report providing financial support for community-based sites. In addition to these competitors, 30% of MD programs reported competition from off-shore medical schools as well.7 One solution to this
issue could involve collaboration between institutions to distribute resources within a community. However, this is increasingly complex given the geographical diversity (local, regional, and abroad), and institutions may seek the services of the same preceptor(s).
Outside of providing direct financial support, offering MOC opportunities was viewed as a high value incentive. This is in line with previous studies9
and expert consensus4 and may be of
growing importance for preceptors given the high cost and time burden. Although a third of our respondents reported that the provision of MOC credit was low with respect to feasibility, recent changes in MOC (eg, those that provide credit for educational program improvement) may soon change this. Specifically, the American Board of Pediatrics has recently embraced such changes and the designation of institutions as MOC portfolio sponsors.30 This
designation may represent a new, high-value, and more feasible opportunity for medical education programs to collaborate with community pediatricians.
There were several limitations to this study. First, our response rate was 63%, which may limit the application of these findings across institutions. It is possible that nonrespondents may have been more or less inclined
to share their practice of providing incentives for community-based preceptors. However, a comparison of our data to that of the 2013 joint report7 suggests that our
population was comparable. Second, pediatric department chairs may not be fully aware of programs to support recruitment and retention of community-based pediatricians, particularly those that are available outside of a departmentally managed pediatric clerkship. In some cases, stipends may be provided from a centrally maintained fund within the dean’s office or from state programs that provide formal partnerships between medical schools and community practices.31
Third, we did not explore the experiences of regional campuses and their respective department chairs. We suspect that this group may be even more reliant on community preceptors because of the smaller size of their institutions. It may therefore be worth exploring their unique perspectives more specifically.
Finally, the results of this study are limited to the perspective of department chairs, and the value of incentives is not considered from the viewpoint of the preceptors. The department chair perspective is just 1 of many perspectives that are involved in the complex situation of designing, financing, and delivering medical education, and the department chair’s influence on teaching services may be indirect. Although department chairs may be best suited to comment on the feasibility of various incentives, the value of such incentives must be considered in conjunction with the viewpoints of other key stakeholders.
CONCLUSIONS
depend heavily on the services of community-based pediatricians to support the educational mission of medical education programs in North America. A thoughtful and collaborative relationship between departmental leadership, educational leaders, school of medicine
administration, and preceptors is required to ensure that incentives to recruit and retain the services of community preceptors are both feasible and valuable. Figure 3 provides a summary schematic that incorporates findings from the perspective of the department chairs who were highlighted in this study as well as from the perspective of medical educators and recent
studies of preceptors.4, 20, 21 We
hope this may be useful in promoting alignment between the value and feasibility of incentive programs to improve the recruitment and retention of community pediatricians.
ACKNOWLEDGMENTS
We thank Drs Jerold Stirling and Kenneth Nakamura, who served on the AMSPDC and COMSEP joint task force and contributed to the initial discussions and survey development related to this article, and Dr Lewis First, Chair of the AMSPDC Education Committee, for his support and guidance throughout this project.
portions of the initial manuscript, critically reviewed the manuscript for important intellectual content, and revised the manuscript; and all authors approved the final manuscript as submitted and agree to be accountable for all aspects of the work.
DOI: https:// doi. org/ 10. 1542/ peds. 2018- 0673 Accepted for publication Jun 20, 2018
Address correspondence to Michael S. Ryan, MD, MEHP, Department of Pediatrics, Virginia Commonwealth University School of Medicine, 1201 E. Marshall St, Box 980565, Richmond, VA 23298-0565. E-mail: michael.ryan1@vcuhealth.org
PEDIATRICS (ISSN Numbers: Print, 0031-4005; Online, 1098-4275). Copyright © 2018 by the American Academy of Pediatrics
FINANCIAL DISCLOSURE: The authors have indicated they have no financial relationships relevant to this article to disclose.
FUNDING: No external funding.
POTENTIAL CONFLICT OF INTEREST: The authors have indicated they have no potential conflicts of interest to disclose.
ABBREVIATIONS
AAMC: Association of American Medical Colleges
AMSPDC: Association of Medical School Pediatric Department Chairs
CME: continuing medical education
COMSEP: Council on Medical Student Education in Pediatrics
LCME: Liaison Committee on Medical Education MD: Doctor of Medicine MOC: Maintenance of
Certification
REFERENCES
1. Nagappan S, Doyne EO, Roberts K, Dewitt TG. Pediatric education in office settings. Pediatr Ann. 2010;39(2):67–71 2. Stirling J. Community
pediatric faculty–a valued but endangered resource. J Pediatr. 2014;165(2):220–221
3. McCurdy FA, Beck GL, Kollath JP, Harper JL. Pediatric clerkship experience and performance in the Nebraska Education Consortium: a community vs university comparison.
Arch Pediatr Adolesc Med. 1999;153(9):989–994
4. Christner JG, Dallaghan GB, Briscoe G, et al. The community preceptor crisis: recruiting and retaining community-based faculty to teach medical students-a shared perspective from
the Alliance for Clinical Education.
Teach Learn Med. 2016;28(3):329–336 5. AAMC Generalist Physician Task
Force. AAMC policy on the generalist physician. Acad Med. 1993;68(1):1–6 6. Liaison Committee on Medical
Education. Standards, publications, and notification forms. 2016. Available at: http:// lcme. org/ publications. Accessed February 12, 2017
7. Erikson C, Hamann R, Levitan T, Pankow S, Stanley J, Whatley, M. Recruiting and maintaining US clinical training sites: joint report of the 2013 multi-discipline clerkship/clinical training site survey. 2013. Available at: https:// members. aamc. org/ eweb/ upload/ 13- 225%20 wc%20 report%202 %20 update. pdf. Accessed March 9, 2017
8. Spencer DC, Choi D, English C, Girard D. The effects of electronic health record implementation on medical student educators. Teach Learn Med. 2012;24(2):106–110
9. Ryan MS, Vanderbilt AA, Lewis TW, Madden MA. Benefits and barriers among volunteer teaching faculty: comparison between those who precept and those who do not in the core pediatrics clerkship.
Med Educ Online. 2013;18:1–7 10. Peters AS, Schnaidt KN, Zivin K,
Rifas-Shiman SL, Katz HP. How important is money as a reward for teaching? Acad Med. 2009;84(1): 42–46
incentives do they prefer? Teach Learn Med. 2002;14(2):119–123
12. Drowos J, Baker S, Harrison SL, Minor S, Chessman AW, Baker D. Faculty development for medical school community-based faculty: a council of academic family medicine educational research alliance study exploring institutional requirements and challenges. Acad Med.
2017;92(8):1175–1180
13. Langlois JP, Thach SB. Bringing faculty development to community-based preceptors. Acad Med. 2003;78(2):150–155
14. Roberts KB, Devries JM. APA/HRSA National faculty development scholars program: community-based teaching track. Ambul Pediatr. 2004;4(suppl 1): 92–97
15. Theobald M. STFM tackles preceptor shortage. Ann Fam Med. 2016;14(2):183–184
16. Laff M. Tax incentives aim to attract primary care preceptors. AAFP News. June 14, 2016. Available at: https:// www. aafp. org/ news/ education- professional- development/ 20160614preceptor credits. html. Accessed February 22, 2018 17. Ullian JA, Shore WB, First LR. What
did we learn about the impact on community-based faculty? Recommendations for recruitment, retention, and rewards. Acad Med. 2001;76(suppl 4):S78–S85 18. Scott I, Sazegar P. Why community
physicians teach students (or not): barriers and opportunities for
preceptor recruitment. Med Teach. 2006;28(6):563–565
19. Leggio LE, Ryan MS, Peltier CB, et al. Recruitment and retention: recommendations from the Association of Medical School Pediatric Department Chairs Education Committee and the Council on Medical Student Education in Pediatrics Task Force on Community Preceptors.
J Pediatr. 2017;191:4–5.e1
20. Latessa R, Colvin G, Beaty N, Steiner BD, Pathman DE. Satisfaction, motivation, and future of community preceptors: what are the current trends? Acad Med. 2013;88(8):1164–1170 21. Beck Dallaghan GL, Alerte AM, Ryan
MS, et al. Recruiting and retaining community-based preceptors: a multicenter qualitative action study of pediatric preceptors. Acad Med. 2017;92(8):1168–1174
22. Association of American Medical Colleges. A snapshot of the new and developing medical schools in the United States and Canada. 2012. Available at: https:// members. aamc. org/ eweb/ upload/ A%20 Snapshot%20 of%20 the%20 New%20 and%20 Developing%20 Medical%20 Schools%20 in%20 the%20 US%20 and%20 Canada. pdf. Accessed January 23, 2018 23. Farnsworth TJ, Frantz AC, McCune RW.
Community-based distributive medical education: advantaging society. Med Educ Online. 2012;17:8432
24. Lacroix TB. Meeting the need to train more doctors: the role of community-based preceptors. Paediatr Child Health. 2005;10(10):591–594
25. Latessa R, Beaty N, Landis S, Colvin G, Janes C. The satisfaction, motivation, and future of community preceptors: the North Carolina experience. Acad Med. 2007;82(7):698–703
26. Dent MM, Boltri J, Okosun IS. Do volunteer community-based preceptors value students’ feedback?
Acad Med. 2004;79(11):1103–1107 27. Starr S, Ferguson WJ, Haley HL, Quirk
M. Community preceptors’ views of their identities as teachers. Acad Med. 2003;78(8):820–825
28. Anthony D, Jerpbak CM, Margo KL, Power DV, Slatt LM, Tarn DM. Do we pay our community preceptors? Results from a CERA clerkship directors’
survey. Fam Med. 2014;46(3):167–173 29. American Academy of Sleep Medicine. Medscape Physician Compensation Report shows salaries vary by specialty. Available at: https:// aasm. org/ medscape- physician- compensation- report- shows- salaries- vary- by- specialty/ . Accessed July 3, 2018
30. American Board of Pediatrics. Improvement in professional practice MOC part 4: pediatric portfolio sponsor standards. 2017. Available at: https:// assets. mymocam. com/ ABP/ Pediatric%20 Portfolio%20 Sponsor%20 Standards2. pdf. Accessed January 23, 2018
DOI: 10.1542/peds.2018-0673 originally published online August 16, 2018;
2018;142;
Pediatrics
Barone
Arenberg, Julie S. Byerley, Julia L. Belkowitz, Gerard P. Rabalais and Michael A.
Michael S. Ryan, Lisa E. Leggio, Christopher B. Peltier, Archana Chatterjee, Steven
Recruitment and Retention of Community Preceptors
Services
Updated Information &
http://pediatrics.aappublications.org/content/142/3/e20180673
including high resolution figures, can be found at:
References
http://pediatrics.aappublications.org/content/142/3/e20180673#BIBL
This article cites 24 articles, 1 of which you can access for free at:
Subspecialty Collections
b
http://www.aappublications.org/cgi/collection/medical_education_su
Medical Education following collection(s):
This article, along with others on similar topics, appears in the
Permissions & Licensing
http://www.aappublications.org/site/misc/Permissions.xhtml
in its entirety can be found online at:
Information about reproducing this article in parts (figures, tables) or
Reprints
http://www.aappublications.org/site/misc/reprints.xhtml
DOI: 10.1542/peds.2018-0673 originally published online August 16, 2018;
2018;142;
Pediatrics
Barone
Arenberg, Julie S. Byerley, Julia L. Belkowitz, Gerard P. Rabalais and Michael A.
Michael S. Ryan, Lisa E. Leggio, Christopher B. Peltier, Archana Chatterjee, Steven
Recruitment and Retention of Community Preceptors
http://pediatrics.aappublications.org/content/142/3/e20180673
located on the World Wide Web at:
The online version of this article, along with updated information and services, is
by the American Academy of Pediatrics. All rights reserved. Print ISSN: 1073-0397.