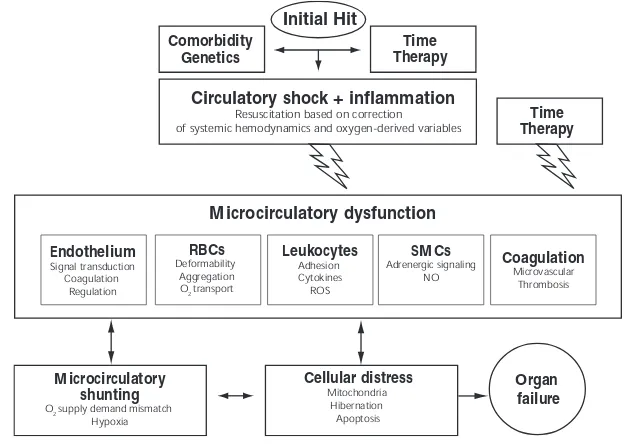
The microcirculation is the motor of sepsis
Full text
Figure
Related documents
Five of the seed selections were obtained from commercial seed companies, while one seed selection was sourced from Trout Lake Farm (Trout Lake, WA, USA), a commercial herb farm that
Analogous to FAB assays, correlations of inhibition of IgE-Bet v 1 binding and previously determined antibody levels revealed significant values for IgG4 and IgE/IgG4 ratios
The stability designation (stability point backup) and the work tool (mulcher) arm load designation were made using real data about.. the tractor with the hydraulic arm in
IL-23 measured by qPCR from RNA extracted from 24 h PPD-J stimulated PBMC isolated from HAV vaccinated (triangles) or Sham vaccinated (squares) calves, taken immediately prior to
Increased expression of VEGF and the degree of tube formation (angiogenesis) by GSNO were reduced after the inhibition of HIF-1 α by 2-ME in an endothelial cell culture model..
By formulating the video denoising problem to a low-rank matrix completion problem, our proposed algorithm does not assume any specific statistical properties
Linear Functional Operations on Functions Having Discontinuities of the First Kind, Bulletin of A.M.S. St.-Nagy Lecons d’analyse fonctionelle, 3rd edition, Budapest Akademiai
The aims of this study are (i) investigate the genetic diversity for MRSA strains obtained from different Iraqi patients using RAPD-PCR, and (ii), the assessment