on Long-Term Renal Function
Fahed Kouli, MD, Christopher H. Morrell, PhD, Lloyd E. Ratner, MD, and Edward S. Kraus, MD ● This study describes renal function at multiple points in time after transplantation and the influence of donor and recipient factors independent of rejection on this function. Donor and recipient records for 83 consecutive cadaveric renal transplants performed between 1992 and 1994 at Johns Hopkins Bayview Medical Center were reviewed retrospectively. Donor age, gender, weight, terminal serum creatinine (Cr), intensive care unit days, blood pressure, presence of cardiac arrest, kidney only versus multiple organ donation, and cold ischemia time and recipient age, gender, weight, pretransplant pregnancy status, and rejection episodes were recorded. The influ-ences of each of these parameters on changes in recipient Cr clearance over time (derived using the Cockcroft-Gault formula from recipient serum Cr at 3 months and annually up to 5 years) were analyzed first individually, then together in an analysis with multiple explanatory variables. Parameters indicative of donor ischemia (ie, donor blood pressure, pressor administration, and occurrence of cardiac arrest) were not predictive of the course of recipient Cr clearance. With the inclusion of rejection, this analysis shows the magnitude of the independent effects that donor age, donor Cr clearance, and recipient gender have on the subsequent time course of recipient Cr clearance (P<0.05). Recipient gender and the presence of rejection appear to have a fixed effect on the level of Cr clearance, whereas donor age and donor Cr clearance appear to influence the level and the time course of recipient Cr clearance. Of all these factors, donor age appears to have the greatest impact on recipient Cr clearance at all times. Analyzing renal function in this way may prove to be a more sensitive indicator than actuarial survival analysis for evaluating the early effects of changes in transplantation protocols and pharmacologic interventions. ©2001 by the National Kidney Foundation, Inc.
INDEX WORDS: Kidney transplant; renal function; creatinine clearance; donor, rejection.
T
HE APPLICATION of actuarial analysisbased on annual survival rates to clinical decision making in renal transplantation has two major limitations. First, because 1-year survival rates exceed 90%,1 the impact of therapeutic
advances may not be apparent without long-term follow-up based on these criteria. Second, these data represent the pooled consensus of different centers with different demographics and may not be applicable directly to individual programs. An approach to evaluation based on criteria other than patient and graft survival is needed.
A series of studies showed that donor and recipient nonimmunologic parameters influence short-term and long-term graft survival and that these factors correlate with renal function when
measured at discrete points in time. Chertow et al2 showed in a multivariate analysis of the
UNOS database (October 1987 through Decem-ber 1991) that after adjusting for immunologic factors (panel-reactive antibodies, transfusions, and HLA mismatch), the relative risk of graft failure is associated significantly with donor age, gender, and race and recipient body surface area. Terasaki et al,3also evaluating the UNOS
regis-try for the years 1987 through 1994, corrobo-rated this impact of nonimmunologic parameters on long-term graft survival. Their study showed that renal function at the time of discharge (re-flected by serum creatinine [Cr]) significantly affects 1-year graft survival and long-term half-life of the allograft. Discharge serum Cr in turn was influenced significantly by donor age, donor sex, mode of donor death, recipient size, and recipient cold ischemia time. Within the first year, this effect was independent of and additive to the effect of matching. Other investigations4,5
showed further the importance of HLA antigen-independent determinants on graft function by comparing outcome at various time intervals (6 months and 2 years) between paired recipients of allografts from the same donor with recipients of allografts from different donors. Cosio et al4
attributed 64% of the variability in renal func-tion, as manifested by serum Cr at 6 months, to From the Johns Hopkins Comprehensive Transplant
Cen-ter, Departments of Medicine and Surgery, Johns Hopkins Bayview Medical Center; The Johns Hopkins Hospital; and Mathematical Sciences Department, Loyola College in Mary-land, Baltimore, MD.
Received February 28, 2000; accepted in revised form September 1, 2000.
Address reprint requests to Edward S. Kraus, MD, Divi-sion of Renal Medicine, B-2, Johns Hopkins Bayview Medi-cal Center, 4940 Eastern Avenue, Baltimore, MD 21224. E-mail: ekraus2@jhmi.edu
© 2001 by the National Kidney Foundation, Inc. 0272-6386/01/3702-0015$35.00/0
doi:10.1053/ajkd.2001.21307
American Journal of Kidney Diseases, Vol 37, No 2 (February), 2001: pp 356-365 356
donor factors. Donor age was important but could not account for the entire effect. Other donor factors could not be elucidated because of the study design.
In this study, we analyzed the course of renal function as a continuum over time after transplan-tation. Our data show that effects on recipient Cr clearance of nonimmunologic factors (ie, donor age, donor Cr clearance, and recipient gender) independent of the impact of rejection are strong enough to be shown within a single center. Dis-playing renal function longitudinally in this man-ner allows a better appraisal of the influence these parameters have on the magnitude and stability of renal function. This methodology serves as a foundation for the early appraisal of new donor selection and recipient protocols and therapeutic interventions.
MATERIALS AND METHODS
Donor and recipient records for 83 consecutive cadaveric renal transplants performed between 1992 and 1994 at Johns Hopkins Bayview Medical Center were reviewed retrospec-tively. Donor factors recorded included age, gender, weight, serum Cr just before declaration of death, number of inten-sive care unit days, blood pressure (systolic, diastolic, dura-tion of lowest blood pressure), pressor administradura-tion, pres-ence of cardiac arrest, whether the patient was a kidney-only or multiple organ donor, and cold ischemia time. Recipient factors recorded included age; gender; weight; pregnancy status before transplantation for women; rejection (single or multiple episodes); and serum Cr at 1 and 3 months and 1, 2, 3, 4, and 5 years. All rejection episodes were diagnosed by pathologic criteria. Cr clearance, as a measure of glomerular filtration rate (GFR), was estimated using the Cockcroft-Gault formula. If allografts failed, Cr clearance was consid-ered 0 at the next time point, then the patient was censored from further analysis. If patients died or were lost to follow-up, they were censored from analysis after the last available Cr clearance measurement.
Descriptive statistics are presented for donor and recipient factors. These statistics are evaluated further according to the gender of the recipient. For numerical variables, the means were compared by applying the two-sample t-test, whereas for categorical variables, the percent in each group were tested for equality by using a chi-square test.
To evaluate the course of Cr clearance as a continuous parameter after transplantation, a linear mixed-effects regres-sion analysis with a quadratic time trend was used.6-8This statistical methodology differs from conventional multiple linear regression by allowing for the evaluation of the effects of multiple variables on changes in Cr clearance as mea-sured repeatedly in the same individual over a prolonged time rather than on single Cr clearance per individual and accounts for variability among individuals. The effects of each donor and recipient factor on the course of Cr clearance through time initially were evaluated separately (univariate
analysis). The parameters that by these analyses were found to have a significant impact on the level and the time course of recipient Cr clearance were included in an analysis with multiple explanatory variables. Factors losing statistical sig-nificance when analyzed together were eliminated. Data are displayed for individual factors found to be significant by the univariate analyses and for the final multiple variable statistical analysis. To derive graphs, variables are fixed at the median and first and third quartiles for donor weight and donor Cr clearance and for age groups corresponding with ideal and extended donor criteria.
RESULTS
The patients included in this study were recipi-ents of 83 consecutive cadaveric renal trans-plants performed by a single surgeon (L.E.R.) at Johns Hopkins Bayview Medical Center be-tween January 1, 1992, and December 31, 1994. Baseline maintenance immunosuppression con-sisted of prednisone, cyclosporine, and imuran during this time period. Donor and recipient characteristics are listed in Table 1.
Univariate Analysis
Donor race, blood pressure, steroid and pres-sor administration (vasopressin, dopamine, and epinephrine), and occurrence of cardiac arrest; cold ischemia time; and recipient age, race, weight, and pretransplant pregnancy status did not influence significantly the level or time course of recipient Cr clearance. The mean Cr clearance
Table 1. Donor and Recipient Characteristics Variable Donor Recipient
Age (y) 32.6⫾20.0 44.5⫾11.4 (2-67) (21-73) Sex (% women) 45% 45% Race (% not white) 22% 59% Weight (kg) 61.6⫾27.7 75.4⫾18.4 (8-136) (35-121) Donor Cr clearance (mL/min) 103.5⫾41.0 (17.5-232.6) Cold ischemia time 24.4⫾12.3
(5-49) No. days in ICU 3.3⫾2.9
(1-17) Systolic blood pressure
(low)
72.1⫾22.9 (30-155) Multiple organ donors 48.0% Pressor administration 92.0% Cardiac arrest 26.8%
Rejections 50%
of recipients from multiple organ donors was a constant 11.2 mL/min greater than that of recipi-ents of allografts from kidney-only donors over the entire follow-up period (P⫽0.05).
Recipient gender influenced the course of Cr clearance after transplantation. At any given time, the mean Cr clearance for female recipients was 14.1 mL/min less than that of male recipients (P ⫽ 0.01). Donor gender tended to influence outcome, but its effect was not statistically signifi-cant (P ⫽ 0.07). Recipients of allografts from female donors had a mean Cr clearance 10.0 mL/min less than that of recipients from male donors. This trend in donor/recipient gender mis-match was additive with female donors to male recipients having a mean Cr clearance 24.1 mL/ min less than male donors to female recipients.
This influence of recipient gender on the course of Cr clearance after transplantation could not be explained by any of the factors examined. Donor and recipient characteristics separated by recipi-ent gender are listed in Table 2. Male and female recipients did not differ with regard to donor characteristics and cold ischemia time. Male and female recipients were similar with regard to age, race, weight, and incidence of rejections.
For female recipients, pregnancy before trans-plantation did not influence the posttransplant course of Cr clearance (P⫽0.70).
Donor age significantly (P⬍0.05) influenced the time course of recipient Cr clearance; this is depicted graphically in Fig 1. For purposes of display and comparison, results of the analysis are divided into four groups. Age cutoffs were selected to reflect young pediatric (ⱕ12 years), adolescent (12 to 20 years), ideal adult (20 to 55 years), and older adult donors (ⱖ55 years). Do-nor weight, doDo-nor-to-recipient weight ratio, and donor Cr clearance also influenced Cr clearance individually after transplantation (P⬍ 0.05) as shown in Fig 2. When these analyses were con-fined to donors aged 20 to 55 years, significant influences of these parameters were lost.
After a first rejection episode, the mean Cr clearance fell 11.3 mL/min (P⫽0.01). Mean Cr clearance fell another 9.4 mL/min after a second rejection episode, but this effect was not quite statistically significant (P⫽0.09).
Analysis Using Multiple Explanatory Variables Full data sets were available from 62 allograft recipients for inclusion in the final analysis. In
Table 2. Donor and Recipient Characteristics Separated by Recipient Gender
Variable
Donor Recipient
Male Recipient Female Recipient Male Recipient Female Recipient
Age (y) 29.9⫾18.4 35.9⫾21.9 44.3⫾10.0 44.7⫾13.1 (2-66) (2-67) (23-65) (21-73)
Sex (% women) 43% 49%
Race (% not white) 21% 23% 58% 60%
Weight (kg) 61.0⫾26.6 62.2⫾29.3 77.8⫾18.2 72.1⫾18.4 (8-136) (11-132) (44-121) (35-115) Donor Cr clearance (mL/min) 109.7⫾48.6 95.5⫾27.3
(17.5-232.6) (51.3-143.6) Cold ischemia time 23.5⫾12.1 25.6⫾12.6
(5-46) (7-49) No. days in ICU 3.3⫾3.2 3.3⫾2.6
(1-17) (1-12) Systolic blood pressure (low) 72.0⫾27.0 72.4⫾17.6
(30-155) (40-110) Multiple organ donors 55% 40% Pressor administration 92.7% 91.2% Cardiac arrest 27.6% 25.9%
Rejections 51% 49%
Pregnancy 63%
NOTE. Values are SD (range) or percent. No comparison between male and female recipients in either the donor or recipient columns was statistically significant using the two-samplet-test for numerical values and the chi-square test for categorical values.
this final analysis, only donor age, donor Cr clearance, recipient gender, and presence of a rejection episode retained significant indepen-dent influences on subsequent recipient Cr clear-ance (Table 3). This analysis showed that after a first rejection episode, a recipient’s Cr clearance fell by 12.5 mL/min but, apart from this change in level, continued with the same pattern of change over subsequent time as if no rejection occurred.
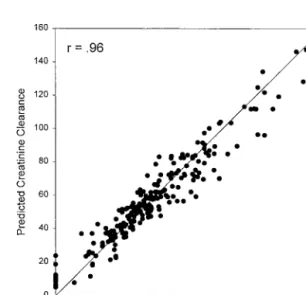
Figure 3 shows the correlation (r ⫽ 0.96) between the Cr clearance values predicted from this analysis and the Cr clearance values ob-served for each patient. The high correlation shows that the factors included in this analysis account for most of the observed variability of Cr clearance over time after transplantation in this study.
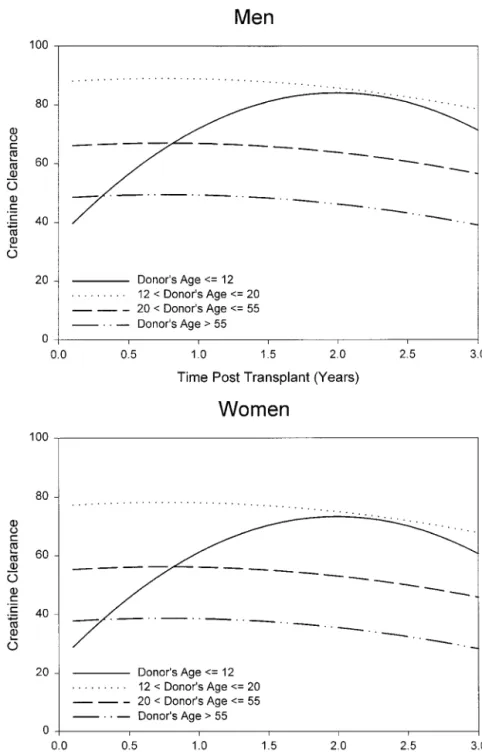
The calculated courses of Cr clearance for rejection-free recipients separated into the four donor age groups as predicted by this analysis are shown in Fig 4. The curves are derived using mean donor Cr clearance and depicted by ent gender. Cr clearance values for female recipi-ents are shifted uniformly downward across time by 10.8 mL/min for all donor age groups.
This analysis further shows that the Cr clear-ance of recipients of kidneys from pediatric donors, although initially lower than for
recipi-ents of kidneys from the other age groups, in-creases steadily with time. By 18 months, renal function in this group appears as good as that of recipients of allografts from adolescent and young adult donors. The two older groups (20 to 55 years and⬎55 years) have Cr clearance values that are 21.9 and 39.5 mL/min lower than the 12 to 20 years age group.
DISCUSSION
Nonimmunologic factors related to the donor organ and to donor/recipient characteristics influ-ence short-term and long-term renal allograft function and survival as shown by single center experience4-5,9-12and analysis of the UNOS data
registry.1-3,13Studies such as these have defined
less than ideal traits for allograft longevity, includ-ing mode of donor death; extremes of donor age; and donor and recipient gender, race, and size. Although many of these nonimmunologic param-eters have been identified, the degree of influ-ence of each factor on long-term allograft func-tion independent of rejecfunc-tion has been difficult to assess.4,9,11,13
In this study, using a single-center experience of 83 consecutive cadaveric renal transplant re-cipients, we analyzed the course of renal func-tion as a continuum over time using a series of mixed-effects regression analyses. This
ap-Fig 1. The effect of donor
age on the subsequent
course of recipient creati-nine clearance. Data for indi-vidual patients are shown. The bold line in each panel is the mean time course as derived from the univariate
mixed-effects regression
analysis using donor age groups as indicated. The ef-fect of age is significant at
Fig 2. The effect of donor weight (A), donor-to-recipi-ent weight ratio (B), and do-nor Cr clearance (C) on the subsequent course of recipi-ent creatinine clearance. The curves depicted are the mean time course as derived from the univariate mixed-effects regression analysis using the median and first and third quartile of donor values as indicated. The ef-fects of these factors are
proach allowed not only for the determination of which donor and recipient factors significantly influenced recipient Cr clearance after transplan-tation over prolonged periods of time, but also for the determination of the magnitude of their effects. Outcomes are depicted graphically in Figs 1 and 2 for univariate analyses and in Fig 4 for the final analysis using multiple explanatory variables. Most of the variability of observed re-cipient Cr clearance after transplantation is ex-plained by this final analysis using these factors; this is shown in Fig 3 by the excellent correlation (r ⫽ 0.96) between the observed recipient Cr clearance and the recipient Cr clearance pre-dicted by this analysis.
As expected after rejection, Cr clearance fell significantly. Recipients remaining rejection-free had Cr clearance values approximately 10 mL/ min higher at all time points. This effect of rejection was superimposed on and could be separated from the influence of the other factors included in the analysis using multiple explana-tory variables.
Donor hemodynamic instability14and mode of
death (cardiovascular versus trauma)2-3,5 have
been associated with worse allograft outcome. In
our analysis, we could not ascribe any significant influence to these factors as reflected by donor blood pressure (lowest donor systolic pressure), pressor administration, and occurrence of car-diac arrest on the initial and the subsequent course of recipient Cr clearance. When analyzed alone, the number of donor intensive care unit days appeared to have an impact on subsequent recipient Cr clearance. In the final analysis with inclusion of multiple explanatory variables, how-ever, significance for this parameter was lost. Given the lack of standardization of documenta-tion of blood pressure and pressor administradocumenta-tion in the donor records reviewed, this finding may be methodologic.
When analyzed alone (Fig 2) and together with other factors, donor Cr clearance did influ-ence subsequent recipient Cr clearance signifi-cantly (although modestly). This effect is most apparent after 2 to 3 years. No discernible impact was noted on recipient Cr clearance at 3 months. At 3-year follow-up, there is an approximately 10 mL/min difference of recipient Cr clearance between the first and third quartiles of donor Cr clearance. Karpinski et al,10using similar
meth-odology to calculate donor GFR, also reported a modest influence of donor renal function on recipient GFR at 1 year. These investigators further showed that this effect was additive to
Fig 3. The correlation of predicted recipient
creati-nine clearance with recipient creaticreati-nine clearance mea-sured at all time points from the mixed-effects regres-sion analysis using multiple explanatory variables.
Table 3. Final Mixed-Effects Regression Model
With Multiple Explanatory Variables
Variable Parameter Estimate Standard Error P Value Intercept 105.94 11.94 ⬍0.0001 Follow-up time ⫺6.86 5.61 0.222 Follow-up time2 ⫺2.06 0.85 0.016 Donor’s Cr clearance ⫺0.182 0.084 0.031 Recipient’s sex ⫺10.8 5.7 0.059 Reject 1 ⫺12.5 4.1 0.002 Donor’s age 1 ⫺52.9 10.4 ⬍0.0001 Donor’s age 3 ⫺21.9 7.6 0.004 Donor’s age 4 ⫺39.5 9.4 ⬍0.0001 Donor’s Cr clearance ⫻time 0.0996 0.0405 0.014 Donor’s age 1⫻time 46.44 10.47 ⬍0.0001 Donor’s age 1⫻time2 ⫺10.39 2.45 ⬍0.0001
Time⫽the number of years since the transplant. Recipi-ent’s sex⫽0 (1) for man (woman). Reject 1⫽1 (0) after the first rejection (before the first rejection). Donor’s age 1⫽1 (0) if donor’s ageⱕ12 years (otherwise). Donor’s age 2⫽ 1 (0) if donor’s age 12-20 years (otherwise). Donor’s age 3⫽1 (0) if donor’s age 20-55 years (other-wise). Donor’s age 4⫽1 (0) if donor’s age⬎55 years (otherwise).
and not explained fully by the impact of preexis-tent donor disease, as shown in implantation biopsy specimens.
It has been hypothesized that implantation of a small kidney into a large recipient has a negative impact on long-term allograft outcome as a result of the burden of an increased metabolic demand and the requirements of organ hypertrophy.
Inves-tigations of this hypothesis have yielded conflict-ing results. In a sconflict-ingle-center experience, Vi-anello et al15reported no difference in allograft
GFR, proteinuria, and survival over 4 years when comparing transplant recipients grouped by size disparity with their donors. Several studies of the UNOS database do support this proposed effect of body size disparity, however. A worse 1-year
Fig 4. The predicted
course of creatinine clear-ance derived from the final
mixed-effects regression
analysis using multiple ex-planatory variables for rejec-tion-free male and female re-cipients using the median donor creatinine clearance and donor ages grouped as indicated. Each variable re-tained a statistical
graft outcome was found when excessive height and weight differences occurred between donor and recipient (recipients of grafts from smaller donors faring worse).16-18 Terasaki et al3 and
Chertow et al2found when analyzing this same
registry that allografts transplanted into larger recipients had a lower 1-year survival and a shorter long-term half-life.
Conclusions drawn from our analyses do not confirm the effect of donor/recipient size dispar-ity on renal function observed in these previous investigations. When evaluated as individual fac-tors in the univariate analyses, small donor weight and small donor-to-recipient weight ratio favor-ably influence recipient Cr clearance at 1, 2, and 3 years of follow-up. Three-month Cr clearance does not appear to be affected by donor size. This discrepancy between our observations and those of earlier studies may be due to differences in the demographics of our donor population. As dis-cussed subsequently, Cr clearance for recipients of allografts from pediatric donors in this study sample increased with time. Because approxi-mately 20% of our donors compared with less than 6% in the UNOS registry were ⬍7 years old,19this could bias our conclusions about the
effect of donor/recipient size match when com-pared with studies comprising predominantly adult donors. When we repeated the analysis excluding these young donors, this advantageous impact of size was no longer significant.
Although in the final multiple variable analy-sis donor weight (as described earlier) did not appear to influence recipient Cr clearance, recipi-ent gender, a possible surrogate marker for size, did retain significance. Cr clearance was 14.1 mL/min less in female recipients than in male recipients with female-to-female transplants hav-ing the lowest subsequent Cr clearance values.
In the analysis using multiple explanatory vari-ables, only the presence of rejection, recipient gender, donor Cr clearance, and donor age retain significant independent influences on the subse-quent course of recipient Cr clearance. As shown in Fig 4, of all these factors, donor age appears to have the greatest impact on recipient Cr clear-ance at all time points. As expected, this analysis shows that recipients of kidneys from older do-nors had a lower Cr clearance when compared with recipients of kidneys from ideal adult
do-nors aged 20 to55 years.2-5,20-28Our data are
con-sistent with findings documented in analyses of the UNOS registry showing a progressive de-cline of recipient GFR with increasing donor age
⬎20 years.2,26,27This effect of donor age could
be due to disease demonstrable by biopsy at the time of transplantation. In a group of transplant recipients of organs from high-risk, predomi-nantly older donors, Karpinski et al10correlated
increased 1-year serum Cr with donor vascular pathology. In another single-center prospective study of recipients from donors of all ages, Pokorna et al12could not confirm this finding,
however. These investigators observed using uni-variate analysis that the degree of donor glomer-ulosclerosis but not vascular disease influenced renal function at 1 and 2 years. In their final multivariate analysis, however, only donor age but not donor pathology retained a significant influence on GFR at 1 and 2 years.
Use of kidneys from very young donors (⬍5 years) remains controversial with programs re-porting decreased,2,3,23,24 normal,29-32 and
vari-able33graft function and survival. In this study,
for recipients of kidneys from donors⬍12 years old (only 1 donor of the 19 in this group was⬎6 years old), Cr clearance increased gradually over the first 1.5 years to levels seen in adolescent donors. Although this increase in Cr clearance may predispose to hyperfiltration injury promot-ing the development of focal sclerosis, we have not noted this as yet.31We continue to follow-up
these patients.
In conclusion, with the shortage of cadaveric donors, less than ideal donors will need to be used to curtail the ever-increasing waiting time for patients desiring transplantation. Our data show a tradeoff between use of less than ideal donors to alleviate time on the waiting list and subsequent renal allograft function over the first 3 years of follow-up. Independent of rejection, donor Cr clearance, donor age, and recipient gender in our analysis predictively influenced recipient Cr clearance. Of these factors, donor age appears from this analysis to have the great-est clinical impact. Data such as these may support development of selection and allocation strategies to optimize long-term outcome, such as the proposal to match older donors with older recipients.
ACKNOWLEDGMENT
We thank Janet Hiller, RN, MSN, of the Johns Hopkins Comprehensive Transplant Center, and the staff of the Trans-plant Resource Center, Baltimore, MD, for their invaluable assistance in identifying and providing donor records for this study.
REFERENCES
1. Hariharan S, Johnson CP, Bresnahan BA, Taranto SE, McIntosh MJ, Stablein D: Improved graft survival after renal transplantation in the United States, 1988 to 1996. N Engl J Med 342:605-612, 2000
2. Chertow GM, Milford EL, Mackenzie HS, Brenner BM: Antigen-independent determinants of cadaveric kidney transplant failure. JAMA 276:1732-1736, 1996
3. Terasaki PI, Gjertson DW, Cecka JM, Takemoto S: Fit and match hypothesis for kidney transplantation. Transplan-tation 62:441-445, 1996
4. Cosio FG, Qiu W, Henry ML, Falkenhaim ME, Elkham-mas EA, Davies EA, Bumgardner GL, Ferguson RM: Fac-tors related to the donor organ are major determinants of renal allograft function and survival. Transplantation 62: 1571-1576, 1996
5. Bertoni E, Zanazzi M, Rosati A, Nistico A, Cirami C, Bandini S, Carmellini M, Frosini F, Mosca F, Rindi P, Rizzo G, Salvadori M: Fate of kidneys retrieved from the same donor and grafted into different recipients: Do donor related factors influence the graft outcome? Transplant Proc 29:125-126, 1997
6. Laird NM, Ware JH: Random-effects models for longi-tudinal data. Biometrics 38:963-974, 1982
7. Pearson JD, Morrell CH, Fleg J, Brant LJ: Gender differences in a longitudinal study of age associated changes in blood pressure. J Gerontol Med Sci 52A:M177-M183, 1997
8. Morrell CH, Pearson JD, Brant LJ: Linear transforma-tions of linear mixed-effects models. Am Stat 51:338-343, 1997
9. Golconda MS, Whiting JF, Smith R, Hayes R, Alex-ander JW, First MR: Long-term outcome of kidney transplan-tation from expanded criteria donors: A single center experi-ence. Transplant Proc 29:3379-3381, 1997
10. Karpinski J, Lajoie G, Cattran D, Fenton S, Zaltzman J, Cardella C, Cole E: Outcome of kidney transplantation from high risk donors is determined by both structure and function. Transpantation 67:1162-1167, 1999
11. Matas AJ, Gillingham KJ, Humar A, Dunn DL, Suth-erland DER, Najarian JS: Immunologic and nonimmuno-logic factors: Different risks for cadaveric and living donor transplantation. Transplantation 69:54-58, 2000
12. Pokorna E, Vitko S, Chadimova M, Schuck O, Ek-berg H: Proportion of glomerulosclerosis in procurement wedge renal biopsy cannot alone discriminate for acceptance of marginal donors. Transplantation 69:36-43, 2000
13. Ojo AO, Wolfe RA, Held PJ, Port FK, Schmouder RL: Delayed graft function: Risk factors and implications for renal allograft survival. Transplantation 63:968-974, 1997
14. Marshall R, Ahsan N, Dhillon S, Holman M, Yang HC: Adverse effect of donor vasopressor support on
immedi-ate and one-year kidney allograft function. Surgery 120:663-665, 1996
15. Vianello A, Calconi G, Amici G, Chiara G, Pignata G, Maresca MC: Importance of donor/recipient body weight ratio as a cause of kidney graft loss in the short to medium term. Nephron 72:205-211, 1996
16. Lee CM, Scandling JD, Shen GK, Salvatierra O, Dafoe DC, Alfrey EJ: The kidneys that nobody wanted— support for the utilization of expanded criteria donors. Trans-plantation 62:1832-1841, 1996
17. Cho YW, Terasaki PI, Cecka JM, Gjertson DW, Takemoto S: Should excessive height and weight differences between the kidney donor and recipient be avoided? Trans-plant Proc 29:104-105, 1997
18. Mizutani K, Yamada S, Katoh N, Ono Y, Ohshima S, Kinukawa T, Fujita T: Cadaveric kidneys from older donors and their effective use in transplantation: A risk factor for long-term graft survival. Transplant Proc 29:113-115, 1997 19. Bennett LE, Shield CF, Edwards EB: Is there a difference in the quality of kidneys that are offered for payback compared to non-payback kidneys? Transplantation 65:S84, 1998
20. Lloveras J, Arias M, Puig JM, Escallada R, Mir M, Cotorruelo JG, de Francisco AL, Masramon J: Long-term follow-up of recipients of cadaver kidney allografts from elderly donors. Transplant Proc 25:3175-3176, 1993
21. Flechner SM, Modlin CS, Serrano DP, Goldfarb DA, Papajcik D, Mastroianni B, Goormastic M, Novick AC: Determinants of chronic renal allograft rejection in cyclo-sporin-treated recipients. Transplantation 62:1235-1241, 1996 22. Pokorna E, Vitko S, Chadimova M, Schuck O: Do the factors of the renal graft donor have an effect on early graft function and long-term graft survival? Transplant Proc 29: 3278-3280, 1997
23. Valdes F, Pita S, Alonso A, Rivera CF, Cao M, Fontan MP, Carmona AR, Mongalian J, Adeva A, Lorenzo D, Oliver J: The effect of donor gender on renal allograft survival and influence of donor age on posttransplant graft outcome and patient survival. Transplant Proc 29:3371-3372, 1997
24. Busson M, Benoit G: Is matching for sex and age beneficial to kidney graft survival? Clin Transplant 11:15-18, 1997
25. Kumar MS, Mysore S, Panigrahi D, Dezii CM, Abouna GM, Chvala R, Brezia J, Kumar AM, Katz SM, McSorley M, Laskow DA: Long-term function and survival of elderly donor kidneys transplanted into young adults. Transplantation 65:282-285, 1998
26. Terasaki PI, Gjertson DW, Cecka JM, Takemoto S, Cho YW: Significance of the donor age effect on kidney transplants. Clin Transplant 11:366-372, 1997
27. Hariharan S, McBride MA, Bennett LE, Cohen EP: Risk factors for renal allograft survival from older cadaver donors. Transplantation 64:1748-1754, 1997
28. Vivas CA, Gritsch HA, Shapiro R, Scantlebury VP, Hickey DP, Hakala TR, Jordan ML: Cadaveric renal trans-plantation using donors over 60 years old—5 year follow-up. Transplant Proc 29:112, 1997
29. Modlin C, Novick AC, Goormastic M, Hodge E, Mastrioanni B, Myles J: Long-term results with single pediatric donor kidney transplants in adult recipients. J Urol 156:890-895, 1996
30. Al-Bader WE, Landsberg D, Manson AD, Levin A: Renal function changes over time in adult recipients of small pediatric kidneys. Transplantation 62:611-615, 1996
31. Ratner LE, Kraus ES, Magnuson T, Bender JS: Trans-plantation of single and paired pediatric kidneys into adult recipients. J Am Coll Surg 185:437-445, 1997
32. Lackner JE, Wright FH, Banowsky LH: Long-term function of single pediatric kidneys less than 48 months of
age transplanted into adult recipients compared with adult cadaveric and living-related transplants. Transplant Proc 29:3283-3287, 1997
33. Satterthwaite R, Aswad S, Sunga V, Shidban H, Mendez RG, Bogaard T, Asai P, Khetan U, Magpayo M, Mendez R: Outcome of en bloc and single kidney transplan-tation from very young cadaveric donors. Transplantransplan-tation 63:1405-1410, 1997