Int J Clin Exp Pathol 2013;6(10):2112-2120 www.ijcep.com /ISSN:1936-2625/IJCEP1308017
Original Article
Clinicopathological significance of PTEN and
PI3K/AKT signal transduction pathway
in non-small cell lung cancer
Fen Yun1, Yongfeng Jia1, Xiuxia Li1, Li Yuan2, Qinnuan Sun1, Huiling Yu1, Lin Shi1, Hongwei Yuan1
1Department of Pathology, The First Affiliated Hospital of Inner Mongolia Medical University, Huhhot, 010059, China; 2Shandong Heze Medical College, Heze, Shandong 274000
Received August 8, 2013; Accepted September 3, 2013; Epub September 15, 2013; Published October 1, 2013
Abstract: A high frequency of mutations at the PTEN locus has been noticed in carcinoma of lung. However, the role of PTEN alternations and its association with outcome variables in the genesis of lung carcinoma are not
un-derstood fully. The purpose of our study was to examine the impact of EGFR, TGF-α, P-AKT and PTEN in the genesis of non-small cell lung cancer (NSCLC). Total numbers of 66 histopathologically confirmed cases of NSCLC and 10 cases of benign control samples embedded with wax were studied. We assessed EGFR, TGF-α and P-AKT by the use of specific antibody through immunohistochemistry as directed by the manufacturer, and detected PTEN expres
-sion by in situ hybridization. There were progressive loss of PTEN expres-sion and significant increasing in EGFR, TGF-α, P-AKT expression from benign samples to NSCLC (p<0.05). The overexpression of EGFR, TGF-α, P-AKT and
loss of PTEN expression were correlated to differentiation extent of cancer tissue, metastasis of lymph nodes and
histological classification. Thus, alteration of EGFR, TGF-α, P-AKT and PTEN are likely important molecular events in
pathogenesis and carcinogenesis of NSCLC.
Keywords: Non-small cell lung cancer (NSCLC), P-AKT, TGF-α, EGFR, PTEN
Introduction
Non-small Cell Lung Cancer (NSCLC) is one of the most formidable health problems in terms of morbidity and mortality facing the mankind today. It is the most common cancer worldwide accounting for 80% of all lung cancer in men and women. Premalignant lesions of tissue show features of epithelial, moderate and severe epithelial dysplasia carry the highest risk for malignant transformation. Identification of high risk premalignant lesions with increased susceptibility to NSCLC and consequent aggressive follow up for early detection and treatment may help in down staging of the can-cer and better prognosis [1]. Human NSCLCs show a variety of genetic changes, with differ-ent changes in differdiffer-ent tumors [2]. PTEN (phosphatase and tensin homolog deleted on chromosome TEN), is a tumor suppressor gene mutated in a variety of human cancers includ-ing prostate, breast, brain, endometrial, glio-blastoma, and melanoma [3-6]. PTEN
expres-sion has been down regulated in many malignancies including lung carcinoma [7], oral carcinoma colorectal adenocarcinoma [8, 9], breast cancer, colon cancer, and renal cell car-cinoma [10, 11].
PTEN and PI3KAKT pathway in non-small cell lung cancer
Figure 1. PTEN showing cytoplasmic expression in NSCLC and benign samples of lung (A: Positive sion of PTEN in lung normal tissue; B: Positive expres-sion of PTEN in lung Squamous carcinoma tissue; C: Positive expression of PTEN in lung adenocarcinoma
[image:2.612.95.517.73.391.2]tissue. Original magnification ×400).
Table 1.Loss of PTEN expression in NSCLC and benign samples
Tissue PTEN X2 P-value*
+ - Positive ratio (%)
NSCLC 22 44 33.30% 6.083 0.014
Benign sample 8 2 80%
Note: *Chi-square test.
Table 2.Correlation between PTEN and clinicopathological factors
Factors PTEN X2 P-value*
- +~+++
Age
≤53 12 5 0.158 0.691
>53 32 17
Sex
Male 32 18 0.66 0.417
Female 12 4
Lymph node metastasis
Positive 28 7 5.961 0.015
Negative 16 15
Pathological pattern
adenocarcinoma 20 4 4.714 0.03
Squamous carcinoma 24 18
Differentiation grade
Moderate-well 24 20 8.727 0.003
Poor 20 2
Note: *Chi-square test.
This study attempts to study the differential expression pat-tern of EGFR, TGF-α and P-AKT and PTEN protein for its rele-vance in development and pro-gression of NSCLC.
Materials and methods
Study population
[image:2.612.89.374.430.476.2] [image:2.612.91.369.517.713.2]Histopathologic-PTEN and PI3KAKT pathway in non-small cell lung cancer
ally, the NSCLCs were cate-gorized as well differentiat-ed and moderately diffe- rentiated -44 cases and poorly differentiated -22 cases, 35 cases with and 31 cases without lymph node metastasis. The be- nign samples of lung (males and females), 31-65 years of age (median age, 48 years) were taken as control.
The protocol of this study was approved by the Protocol Review Committee and the Bioethics Commi- ttee of Inner Mongolia Medical University.
PTEN in situ hybridization
In order to detect PTEN expression, in situ hybrid-ization assays were
per-Figure 2. EGFR expression in NSCLC and benign samples of lung (A: Negative expression of EGFR in lung normal tissue; B: Positive expression of EGFR in Squamous car-cinoma tissue; C: Positive expression of EGFR in lung
[image:3.612.96.519.74.392.2]ad-enocarcinoma tissue. Original magnification ×400).
Table 3. EGFR expression in NSCLC and benign samples
Tissue EGFR X2 P-value*
+ - Positive ratio (%)
NSCLC 46 20 69.70% 4.367 0.037
Benign sample 3 7 30.00%
Note: *Chi-square test.
Table 4. Correlation between EGFR and clinicopathological factors
Factors EGFR X2 P-value*
- +~+++
Age
≤53 6 11 0.27 0.603
>53 14 35
Sex
Male 16 34 0.047 0.828
Female 4 12
Lymph node metastasis
Positive 4 31 12.569 0.001
Negative 16 15
Pathological pattern
adenocarcinoma 8 16 0.164 0.686
Squamous carcinoma 12 30
Differentiation grade
Moderate-well 18 26 7.03 0.008
Poor 2 20
[image:3.612.90.389.427.476.2] [image:3.612.91.388.515.713.2]PTEN and PI3KAKT pathway in non-small cell lung cancer
formed on serial 5 microns thick sections from the orig -inal blocks and the TMA block, using a kit for in situ hybridization (MK1276, Bo-ster Biotech Co, Wuhan, China), according to the provider’s specifications as described in detail else-where. The poly-A probe, used as an indicator of the preservation of mRNA in the cells (positive control), resulted mainly in dark brown nuclear staining and less in a cytoplasmic one.
Immunohistochemical
analysis
[image:4.612.94.519.74.393.2]Formalin fixed paraffin-embedded tissue blocks were cut in 5 microns thick serial sections. The sec-tions were deparaffinized, rehydrated and rinsed in
[image:4.612.91.389.432.477.2]Figure 3. TGF-α expression in NSCLC and benign samples of lung (A: Negative expression of TGF-α in lung normal tissue; B: Positive expression of TGF-α in lung Squamous carcinoma tissue; C: Positive expression of TGF-α in lung adenocarcinoma tissue. Original magnification ×400).
Table 5. TGF-α expression in cytoplasm of NSCLC and benign samples
Tissue TGF-α X2 P-value*
+ - Positive ratio (%)
NSCLC 47 19 71.20% 4.850 0.028
Benign sample 3 7 30.00%
Note: *Chi-square test.
Table 6.Correlation between TGF-α and clinicopathological factors
Factors TGF-α X2 P-value*
- +~+++
Age
≤53 6 11 0.142 0.706
>53 13 36
Sex
Male 14 36 0 1
Female 5 11
Lymph node metastasis
Positive 5 30 7.645 0.006
Negative 14 17
Pathological pattern
adenocarcinoma 9 15 1.396 0.237
Squamous carcinoma 10 32
Differentiation grade
Moderate-well 16 28 3.695 0.055
Poor 3 19
[image:4.612.92.390.518.714.2]PTEN and PI3KAKT pathway in non-small cell lung cancer
[image:5.612.94.519.74.390.2]phosphate buffer saline (PBS). An Immunohistoche-mical assay for EGFR, TGF-α, P-AKT was performed on consecutive paraffin sec -tions using streptavidin-bio-tin method. Monoclonal mouse antihuman EGFR antibody (ZM0093, Beijing ZSGB Company, China), monoclonal rabbit antihu-man TGF-α antibody (ZA2-54, Beijing ZSGB Company, China) and monoclonal mouse antihuman P-AKT antibody (sc16646, Beijing ZSGB Company, China) were used as primary anti-bodies respectively. After antigen retrieval slides were incubated with primary anti-body, followed by second-ary biotinylated antibody. Sections were washed in PBS and then incubated
Table 7. P-AKT expression in cytoplasm of NSCLC and benign samples
Tissue P-AKT X2 P-value*
+ - Positive ratio (%)
NSCLC 50 16 75.80% 10.048 0.002
Benign sample 2 8 20.00%
Note: *Chi-square test.
Table 8. Correlation between P-AKT and clinicopathological factors
Factors P-AKT X2 P-value*
- +~+++
Age
≤53 3 14 0.166 0.683
>53 13 36
Sex
Male 12 38 0 1
Female 4 12
Lymph node metastasis
Positive 4 31 6.662 0.010
Negative 12 19
Pathological pattern
adenocarcinoma 3 21 2.832 0.092
Squamous carcinoma 13 29
Differentiation grade
Moderate-well 14 30 4.125 0.042
Poor 2 20
[image:5.612.91.389.432.478.2]Note: *Chi-square test.
Figure 4. P-AKT immunostaining showing expression in
cytoplasm of NSCLC and benign samples of lung (A:
Neg-ative expression of P-AKT in lung normal tissue; B: Posi
-tive expression of P-AKT in lung Squamous carcinoma tissue; C: Positive expression of P-AKT in lung adenocar
[image:5.612.92.387.518.713.2]PTEN and PI3KAKT pathway in non-small cell lung cancer
Table 9. Correlation between EGFR and TGF-α expression
EGFR TGF-α X2 P-value*
+
-+ 37 9 0.309 0.012
- 10 10
[image:6.612.91.344.188.240.2]Note: *Chi-square test.
Table 10. Correlation between EGFR and P-AKT expression
EGFR P-AKT X2 P-value*
+
-+ 39 7 0.319 0.022
- 11 9
[image:6.612.91.344.290.345.2]Note: *Chi-square test.
Table 11. Correlation between P-AKT and TGF-α expression
P-AKT TGF-α X2 P-value*
+
-+ 41 9 0.421 0.002
- 6 10
Note: *Chi-square test.
with streptavidin peroxidase. Finally chromo-gen Diaminobenzidine (DAB) was used and sec-tion were counterstain with hematoxylin.
Table 12. Correlation between EGFR and PTEN expression
EGFR PTEN X2 P-value*
+
-+ 9 37 -0.443 0.001
- 13 7
Note: *Chi-square test.
Table 13. Correlation between TGF-α and PTEN expression
TGF-α PTEN X2 P-value*
+
-+ 11 36 -0.331 0.007
- 11 8
Note: *Chi-square test.
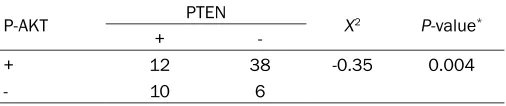
Table 14. Correlation between P-AKT and PTEN expression
P-AKT PTEN X2 P-value*
+
-+ 12 38 -0.35 0.004
- 10 6
Note: *Chi-square test.
Scoring method
Tumors were classified as EGFR, TGF-α, P-AKT and PTEN negative (i.e. low expression) if less than 10% of cells displayed positivity. If equal to or greater than 10% of cells were posi-tive for EGFR, TGF-α, P-AKT and PTEN (i.e. high expression) were considered as positive.
A total of 5-6 fields from each tissue section were chosen, and 100 cells from each field were counted at final magnification at 400X. With every batch of staining a positive and nega-tive control were used to verify the standard of staining.
The percentage of EGFR, TGF-α, P-AKT and PTEN positive cells was calculat-ed independently by two pathologists. The correlations between EGFR, TGF-α, P-AKT and PTEN expression and histological grading were studied. Statistical analysis
Chi-square (X)2 test was performed to
find out the possible correlation among EGFR, TGF-α, P-AKT and PTEN and other clinical parameters in NSCLC and benign samples of lung tissue. We used the SPSS ver. 14.0 (SPSS Inc., Chicago, IL, USA), with P<0.05 being considered as statisti -cally meaningful.
Results
Loss of PTEN expression in NSCLC
[image:6.612.90.344.393.448.2] [image:6.612.91.344.496.547.2] [image:6.612.91.344.596.649.2]PTEN and PI3KAKT pathway in non-small cell lung cancer
speculate that tumor prognostic features cor-related with EGFR, TGF-α P-AKT and PTEN expression in NSCLC.
Discussion
Lung cancers make up 14% of all newly diag -nosed cancers in the USA today, whereas. Though there are many studies on the etiology of cancer but the exact pathogenesis still remains uncertain. The major etiologic factor in the development of lung cancer is smoking, besides, cultural, and genetic differences, hor-monal and possibly infectious factors may also play etiologic roles [18]. The incidence of lung cancer might be due to the cumulative effects of long time exposures to carcinogens, the fail-ings of DNA repair mechanisms and aging [19]. The identification of prognostic and predictive markers is clinically important, because lung cancer is a group of heterogenous diseases with various biological and clinical characteris-tics. Loss of PTEN function and/or overexpres-sion of growth factors and malfunctions in their signal pathways occur frequently in cancers. EGFR, TGF-α and P-AKT have been studied as predictive markers and prognostic factors in prostate, oral, breast and lung cancers [20, 21]. Earlier investigator showed that expres-sion status of EGFR, TGF-α, P-AKT or PTEN in lung cancer. However, to our knowledge, this is the first study to report that EGFR, TGF-α, and P-AKT expression is inversely correlated with PTEN loss in NSCLC. This observation shows that a mechanism by which EGFR, TGF-α, and P-AKT are upregulated in the development and progression of NSCLC. Such a mechanism would include loss of PTEN activity. The upregu-lation of EGFR, TGF-α, and P-AKT might reduce the apoptotic induction thereby contributing to the tumorigenesis. The present study reveals that loss of PTEN expression in NSCLC clinical specimens is significantly correlated with EGFR, TGF-α, and P-AKT overexpression. The study also shows that loss of PTEN expression and EGFR, TGF-α, P-AKT overexpression are signifi -cantly correlated with NSCLC staging, suggest-ing that both of the activities may play an important role in NSCLC development and pro-gression. Earlier investigator showed that loss of PTEN increased remarkably according to dis -ease stage and lymph node metastasis [22, 23]. Our study showing that PTEN gene altera-tion is associated with advanced stage and lymph node involvement, histological classifi
-cation and poor differentiation (Table 2).
Immunohistochemical detection of EGFR
protein
Nuclear immuno reaction for EGFR was consid-ered positive and found in 46/66 cases (69.7%) of NSCLC and 3/10 of benign samples of lung (Figure 2). The result reveals the significant dif -ference between the normal tissue (30%) and cancerous tissue (69.7%) for the EGFR protein (p<0.05). With the progression in lymph node involvement and tumor grade, the rate of EGFR expression significantly increased (Tables 3
and 4).
Immunohistochemical detection of TGF-α
protein
Cytoplasmic and nuclear immuno-reaction for TGF-α was considered positive and found in 47/66 cases (71.2%) of NSCLC and 3/10 of benign samples of lung (Figure 3). In the NSCLC,the overexpression of TGF-α had sig -nificant correlation with the metastasis of lymph nodes (Tables 5 and 6).
Immunohistochemical detection of P-AKT
protein
Nuclear immuno reaction for P-AKT was consid -ered positive and found in 50/66 cases (75.8%) of lung carcinoma and 2/10 of benign samples of lung (Figure 4). The result reveals the signifi -cant difference between the normal tissue (20%) and cancerous tissue (75.8%) for the P-AKT protein (p<0.05). With the progression in lymph node involvement and tumor grade, the rate of P-AKT expression significantly increased (Tables 7 and 8).
The relationship between EGFR, TGF-α, P-AKT and PTEN expression
PTEN and PI3KAKT pathway in non-small cell lung cancer
lymph node metastasis. Our results suggest that PTEN may play an important role in the regulation of tumor progression and metasta-sis during the development of NSCLC. But the exact role of PTEN in the genesis of NSCLC remains unknown. Studies on PTEN in NSCLC showed frequent genetic alterations and loss of expression but still there are a lot of discrepan-cies toward the drawing of the final conclusion [24]. Recent study demonstrates that loss of PTEN was associated to up-regulation of the EGFR gene, thus contributing to survival of can-cer cells in lung and breast cancan-cers [25, 26]. Our results also showed the strong association of loss PTEN expression with not only EGFR, but also TGF-α, and P-AKT positive expression (p<0.05) in NSCLC.
Acknowledgements
This project was supported by science fund for young scholars of Inner Mongolia Medical University (NY2007QN007).
Disclosure of conflict of interest
There is no conflict of interest among all the authors in this study.
Address correspondence to: Dr. Yongfeng Jia,
Department of Pathology, The First Affiliated
Hospital of Inner Mongolia Medical University, NO.1, Northern Tongdao Street, Huhhot, 010059, China. E-mail: yfjia0479@163.com
References
[1] Keith RL, Miller YE. Lung cancer chemopreven -tion: current status and future prospects. Nat Rev Clin Oncol 2013; 10: 334-43.
[2] Kadara H, Wistuba II. Field cancerization in
non-small cell lung cancer: implications in dis-ease pathogenesis. Proc Am Thorac Soc 2012; 9: 38-42.
[3] Salvesen HB, Werner HM, Krakstad C. PI3K
Pathway in Gynecologic Malignancies. Am Soc
Clin Oncol Educ Book 2013; 2013: 218-21.
[4] Cancer Genome Atlas Research Network, Kan
-doth C, Schultz N, Cherniack AD, Akbani R, Liu
Y, Shen H, Robertson AG, Pashtan I, Shen R, Benz CC, Yau C, Laird PW, Ding L, Zhang W,
Mills GB, Kucherlapati R, Mardis ER, Levine
DA. Integrated genomic characterization of en-dometrial carcinoma. Nature 2013; 497: 67-73.
[5] Daniilidou K, Frangou-Plemenou M, Grammati
-kakis J, Grigoriou O, Vitoratos N, Kondi-Pafiti A.
Prognostic significance and diagnostic value of
PTEN and p53 expression in endometrial carci-noma. A retrospective clinicopathological and immunohistochemical study. J BUON 2013; 18: 195-201.
[6] Duman BB, Sahin B, Acikalin A, Ergin M, Zorlu
-demir S. PTEN, Akt, MAPK, p53 and p95 ex -pression to predict trastuzumab resistance in HER2 positive breast cancer. J BUON 2013; 18: 44-50.
[7] Boespflug A, Couraud S, Bringuier PP, Isaac S,
Gérinière L, Perrot E, Edery P, Durieu I, Sou-quet PJ. Primary lung adenocarcinoma occur-ring in a PTEN related syndrome (Cowden’s disease): routine EGFR sequencing also high-lights two rare somatic mutations S768I and V769L. Lung Cancer 2013; 79: 318-20. [8] Rahmani A, Alzohairy M, Babiker AY, Rizvi MA,
Elkarimahmad HG. Clinicopathological signifi -cance of PTEN and bcl2 expressions in oral squamous cell carcinoma. Int J Clin Exp Pathol 2012; 5: 965-71.
[9] Ghiţă C, Vîlcea ID, Dumitrescu M, Vîlcea AM, Mirea CS, Aşchie M, Vasilescu F. The prognos -tic value of the immunohistochemical aspects of tumor suppressor genes p53, bcl-2, PTEN
and nuclear proliferative antigen Ki-67 in re -sected colorectal carcinoma. Rom J Morphol Embryol 2012; 53: 549-56.
[10] Abdulkareem IH, Blair M. Effects of indometha -cin on expression of PTEN tumour suppressor in human cancers. Niger Med J 2013; 54: 100-6.
[11] Cheng T, Zhang JG, Cheng YH, Gao ZW, Ren XQ. Relationship between PTEN and Livin expres-sion and malignancy of renal cell carcinomas. Asian Pac J Cancer Prev 2012; 13: 2681-5. [12] Li LQ, Li XL, Wang L, Du WJ, Guo R, Liang HH,
Liu X, Liang DS, Lu YJ, Shan HL, Jiang HC. Ma-trine inhibits breast cancer growth via miR-21/
PTEN/Akt pathway in MCF-7 cells. Cell Physiol
Biochem 2012; 30: 631-41.
[13] Akca H, Demiray A, Tokgun O, Yokota J. Inva -siveness and anchorage independent growth ability augmented by PTEN inactivation through
the PI3K/AKT/NFkB pathway in lung cancer
cells. Lung Cancer 2011; 73: 302-9.
[14] Koromilas AE, Mounir Z. Control of oncogene
-sis by eIF2α phosphorylation: implications in PTEN and PI3K-Akt signaling and tumor treat -ment. Future Oncol 2013; 9: 1005-15. [15] Dionysopoulos D, Pavlakis K, Kotoula V,
Fountzilas E, Markou K, Karasmanis I, Angouri
-dakis N, Nikolaou A, Kalogeras KT, Fountzilas G. Cyclin D1, EGFR, and Akt/mTOR pathway. Potential prognostic markers in localized laryn -geal squamous cell carcinoma. Strahlenther
Onkol 2013; 189: 202-14.
[16] Pannain VL, Morais JR, Damasceno-Ribeiro O,
PTEN and PI3KAKT pathway in non-small cell lung cancer
immunoreactivity. A study in hepatocellular carcinoma and in non-neoplastic liver tissue. Ann Hepatol 2012; 11: 495-9.
[17] Berg M, Soreide K. EGFR and downstream ge
-netic alterations in KRAS/BRAF and PI3K/AKT
pathways in colorectal cancer: implications for targeted therapy. Discov Med 2012; 14: 207-14.
[18] Egleston BL, Meireles SI, Flieder DB, Clapper ML. Population-based trends in lung cancer incidence in women. Semin Oncol 2009; 36: 506-15.
[19] Grudny J, Kołakowski J, Kruszewski M, Szopiński J, Sliwiński P, Wiatr E, Winek J, Załęska J, Zych J, Roszkowski-Śliż K. Associa -tion of genetic dependences between lung cancer and chronic obstructive pulmonary dis-ease. Pneumonol Alergol Pol 2013; 81: 308-18.
[20] Bettstetter M, Berezowska S, Keller G, Walch
A, Feuchtinger A, Slotta-Huspenina J, Feith M,
Drecoll E, Höfler H, Langer R. Epidermal growth factor receptor, phosphatidylinositol-3-kinase catalytic subunit/PTEN, and KRAS/NRAS/
BRAF in primary resected esophageal adeno-carcinomas: loss of PTEN is associated with worse clinical outcome. Hum Pathol 2013; 44: 829-36.
[21] Takeda H, Takigawa N, Ohashi K, Minami D, Kataoka I, Ichihara E, Ochi N, Tanimoto M, Kiu
-ra K. Vandetanib is effective in EGFR-mutant lung cancer cells with PTEN deficiency. Exp Cell
Res 2013; 319: 417-23.
[22] Krohn A, Diedler T, Burkhardt L, Mayer PS, De Silva C, Meyer-Kornblum M, Kötschau D,
Tennstedt P, Huang J, Gerhäuser C, Mader M,
Kurtz S, Sirma H, Saad F, Steuber T, Graefen
M, Plass C, Sauter G, Simon R, Minner S, Schlomm T. Genomic deletion of PTEN is as-sociated with tumor progression and early PSA recurrence in ERG positive and fusion-negative prostate cancer. Am J Pathol 2012; 181: 401-12.
[23] Im SA, Lee KE, Nam E, Kim DY, Lee JH, Han HS, Seoh JY, Park HY, Cho MS, Han WS, Lee SN. Potential prognostic significance of
p18-5(HER2) overexpression with loss of PTEN ex-pression in gastric carcinomas. Tumori 2005; 91: 513-21.
[24] Panagiotou I, Tsiambas E, Lazaris AC, Kavant
-zas N, Konstantinou M, Kalkandi P, Ragkos V, Metaxas GE, Roukas DK, Vilaras G, Patsouris
E. PTEN expression in non small cell lung carci-noma based on digitized image analysis. J BUON 2012; 17: 719-23.
[25] Kim EJ, Jeong JH, Bae S, Kang S, Kim CH, Lim YB. mTOR inhibitors radiosensitize PTEN-defi -cient non-small-cell lung cancer cells harbor-ing an EGFR activatharbor-ing mutation by inducharbor-ing autophagy. J Cell Biochem 2013; 114: 1248-56.