Staying on Target
TMMy Doctor Says:
“Pattern Management
Will Help Me...”
TARGET THERAPY
S T A Y
IN G
O N
T
A R
G
E T
Taking Care of Your Diabetes
You check your blood glucose several times a day and record them in a logbook. When you visit your healthcare provider, he or she always asks to see your logbook. What is he looking for and what does he find in those records? Your doctor is looking for a pattern of blood glucose numbers. For instance, your blood glucose may be higher before lunch than the rest of the day.
He will then try to determine what may be the cause of the high readings at lunch. By looking at these “patterns“ your health care provider will make changes to your treatment plan. Looking at blood glucose records and determining a treatment plan based on those records is called pattern management.
Pattern Managementis a skill that you can learn in order to manage your diabetes. The following information will help you learn about this important method of diabetes care.
Insulin Dose Changes:
Changing your insulin dose may seem difficult and confusing. Health care professionals may ask you to make two different kinds of changes: Correction doses and pattern changes. If your blood glucose before lunch is almost always normal, but today it is high,
you may take 1 or 2 extra units of insulin to “correct” the high reading. This is called a correction dose. This is a temporary change in your dose. If your blood glucose tomorrow before lunch is normal you will not need a correction dose. In contrast, if your blood glucose results before lunch are high for more than 3 days in a row, you will need to make a pattern change. This is a permanent change in your insulin dose. Once you have made a pattern change you continue to take this dose of insulin until you see that it is no longer keeping your blood glucose “in target” and you then make another pattern change.
YOU Can Make a Big Difference
With some diseases you can take a pill, forget about it and go about your daily routine. Diabetes is different.
When you have diabetes, you must take a lot of responsibility for your treatment. Studies have actually proved you can prevent or delay eye, kidney, heart, blood vessel, and nerve complications
of diabetes by 10 years or more just by keeping your blood glucose levels as close to normal as possible!1
Taking the time and effort to learn how to care for your diabetes can really help reward you with long-term health and well-being. Your goal is to keep your blood glucose as close to normal as possible. To do this you should develop “Stay Healthy Goals.”
Your Stay-Healthy Goals
To take care of yourself, you will need to: 1. Develop healthier eating habits. 2. Stay at a healthy weight.
3. Get regular exercise.
4. Monitor your blood glucose (blood sugar). 5. Take medication such as insulin.
Skills You Will Need
To succeed at your stay-healthy goals you will learn to: • Analyze the variables that affect your
glucose levels.
• Make changes to avoid glucose levels that are too high or too low.
• Make decisions about exercise, meals, and maybe even insulin doses.
• Keep most blood glucose levels in your target range.
1The Writing Team for the Diabetes Control and Complications Trial/Epidemiology
Pattern Management:
Your Key to Staying in Good Control
Be a DetectivePeople who are in good control of their diabetes learn how to prevent frequent high and low blood glucose levels. If you have diabetes, analyzing the patterns of your blood glucose results that you have recorded over a period of time can help prevent blood glucose levels that are too high or too low. This method of diabetes control is called “pattern management.” Detecting certain patterns from your results can help you see when and how to make changes in your daily routine.
Stay on Target
Your blood glucose target is the range of blood glucose that you can safely achieve without having hypoglycemia (low blood glucose). Your blood glucose reading should fall into your target blood glucose range most of the time. Using pattern management will help you to meet your target blood glucose goals.
Learn the Alert Signals
Pattern management works best when you notice a pattern showing that your blood glucose levels were out of your target range over a period of time. Three days is usually a good time period. You should not be making pattern changes in response to just one or two readings. This is your signal to stop and think about what may have affected your blood glucose levels during that specific time frame. Taking these steps will help you understand the changes you can make to bring your
Your Tools for Pattern Management
Written Records:Keep Them Daily
The first step in pattern management is writing down your blood glucose levels in your logbook or recording them with a data management software program on
your computer. There are meters that can also record your readings. The pattern of your blood glucose readings shows you if the balance of your insulin, food, and exercise is working. If your blood glucose levels are in your target range, your balance is working well. But if your numbers are too high, too low, or vary a great deal you are not in balance. You need to consider what is causing your blood glucose to be out of your target range, and what you can do to improve them.
You will find that you will feel better overall when your blood glucose is within your target range. To stay in your range, you need to understand what happens to your blood glucose levels when you take insulin, exercise, eat or drink.
Variables:
Know What Makes Blood Glucose Go Up and Down
There are many different causes or events that can make your blood glucose go too high or too low. These are called “variables” and are the possible causes that influence your blood glucose. With pattern management, you will be looking for patterns of highs and/or lows
to help you know what kind of changes to make. Some variables might be:
• How quickly your insulin is released or absorbed into your blood stream.
• The way you body responds to physical activity. • The effect of stress or illness on your
blood glucose.
• The amount and kind of food that you eat. • How fast your food is digested and changed
into glucose in your stomach.
The best way for you to understand the effect of variables on your blood glucose levels is to keep written records using a logbook or a computer data management system. Either way, it is important to show your records to your health care provider. He or she can provide useful information to guide changes in the variables that affect your diabetes control, including medication, food intake or exercise.
For more information about the relationship between blood glucose and exercise, read the BD Getting Started™ brochure, My Doctor Says I Need to Exercise…which may be found on-line at: www.bddiabetes.com/us/download/download.asp
Variables That Can Change the Level of Your Blood Glucose
What Makes Blood Glucose Rise? What Makes Blood Glucose Fall? Foods or drink with carbohydrates *Exercise
Stress Insulin
2Adapted fromStandards of Medical Care in Diabetes Mellitus-2006,
Diabetes Care, Volume 29, Supplement 1, p. S10-11, January 2006.
Recommended Target Blood Glucose Levels2
ADA Recommended Targets For Blood Glucose (Sugar) Control In Non-Pregnant Individuals With Diabetes
Normal Target
Before eating Less than 100 90 to 130 2 hours after eating Less than 130 Less than 180
A1C Less than 6% Less than 7%
Target Blood Glucose Goals:
What is Your Target?
Normal blood glucose levels are 70 to 120 mg/dl. If you don’t already know your target blood glucose goals, ask your Health Care Provider for assistance. Generally, it is good to keep blood glucose levels as close to normal as possible, but that is often hard to do without having frequent or severe low blood glucose episodes. The American Diabetes Association (ADA) recommends the
following targets as a starting point for most people.
Your Medications:
Learn How They Work
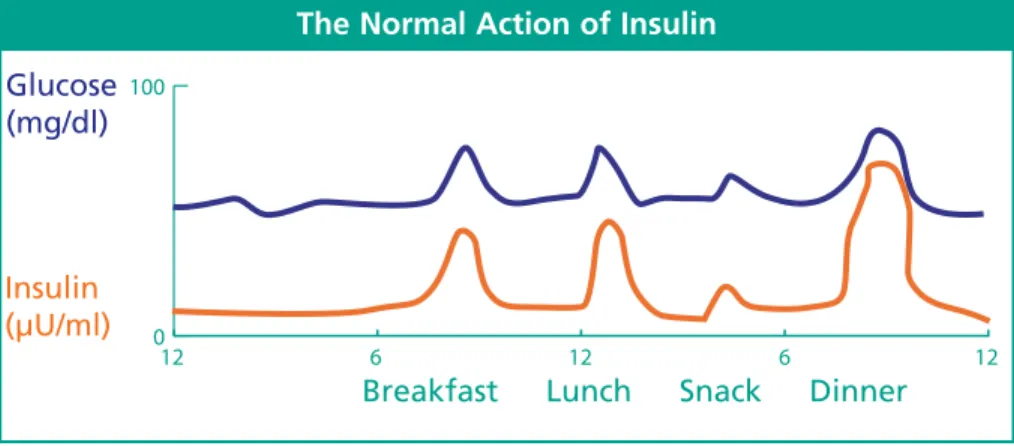
The Action of Insulin in People without Diabetes
In people who do not have diabetes, there is a perfect balance of insulin in response to changes in blood glucose levels. When they eat and their blood glucose rises, their bodies automatically release the right amount of insulin to keep their blood glucose in a normal range.
Figure 1:Represents 24-hour action of blood glucose and insulin action in a person without diabetes.
The Body Normally Releases Insulin in Two Ways
Basal (background) insulin: This type of insulin is released every few minutes in small amounts to maintain a stable level of glucose in the blood. Basal insulin keeps blood glucose levels stable between meals and during the night.
Bolus (fast-acting) insulin: When you eat or drink, the food is broken down into glucose and absorbed into the blood stream. The pancreas releases a bolus (burst) of insulin in response to the rapid rise in blood glucose that occurs after a meal.
The Normal Action of Insulin
Glucose (mg/dl)
Insulin (µU/ml)
Injected Insulin Acts at Different Speeds
Intermediate and long-acting insulin: These are NPH, Lantus® (insulin glargine), Levemir®
(insulin detemir) and are used to mimic the basal (background) insulin action.
Rapid-acting and short-acting insulin:
This group includes Humalog®(insulin lispro) Novolog® (insulin aspart),
Apidra®(insulin gluslisine) and/or the short acting Regular insulin. These
are used to imitate the bolus (burst) of insulin action that
acts to “cover” high blood glucose levels that occur
after eating.
*Not commonly used in Flexible Insulin Therapy.
The Timing of Injected Insulin
Name of Insulin Type of Insulin Peak Action Effect on Blood Glucose Humalog®
Novolog® Apidra®
Rapid 30 min. to
1.5 hours 5 hours *Regular Short 2 to 4 hours 6 hours *NPH Intermediate 4 to 12 hours 8 to 14 hours Lantus®
Levemir® Long
No peak
Long-acting (basal) insulin
• NPH insulin peaks or works the hardest at 4 to 12 hours after they are taken. They will continue to work for a total of 8 to14 hours.
• Levemir®(Insulin Detimir) is similar to Lantus® (Insulin Glargine) and both work for a 24-hour period of time with no peak.
Rapid-acting (bolus) insulin
• Humalog®, Novolog®, and Apidra®are rapid acting insulins – used to cover the glucose released from the food eaten or bring down high blood glucose quickly. • Regular insulin works a little slower
and is described as short acting.
Figure 2:Represents the action of three injections of rapid acting insulin before meals and one injection of Insulin Glargine or Detemir at bedtime.
Ask your diabetes educator about the insulin that you are taking and
how it works. For more information about insulin action, read the BD
booklet, Staying on Target™: Your
Insulin Adjustment Workbook. Yes, You Can Do It! It may
be found on-line at:
www.bddiabetes.com/us/down load/download.asp
How Do You Know Your Insulin is Working?
Your blood glucose readings reflect the action on insulin given earlier in the day. When you take blood glucose readings at any given time you are actually checking to see how well the last dose of insulin worked. (See below.)
A Blood Glucose Reading Taken: Matches Insulin Given Earlier: Before Breakfast Dinner or bedtime
background insulin
Before Lunch Breakfast
Before Dinner
Lunch rapid or short-acting insulin or breakfast NPH or Levemir®insulin
Two Hours After Meals Short or rapid acting insulin before that meal
Before Bedtime Dinner rapid or short-acting insulin
3 AM Dinner or bedtime NPH,
Your Plan for Eating
Did You Know That Everything You Eat Affects Your Blood Glucose?
When you have diabetes you need to learn the impact of foods on your blood glucose (remember that glucose is another word for sugar). Over time, everything you eat breaks down into glucose. This causes changes to your blood glucose levels. To better understand this, it is important to know that foods are classified into three major categories: Carbohydrates, Proteins, and Fats.
1. Carbohydrates (carbs)
come from plants (fruits, vegetables, grains, cereal products, and desserts). Carbs convert 100 percent into glucose, 1 to 2 hours after eating!
2. Proteins are from animals (beef, poultry, fish, eggs, cheese) as well as some plants (tofu and peanut butter). Proteins convert 50 to 60 percent into glucose, 3 to 4 hours after eating.
3. Fatsare foods that make everything taste good (butter, margarine, oils, mayonnaise, cream cheese). Fats convert 10 percent into glucose, taking place gradually over six hours after eating.
Figure 3:The speed at which the three nutrients convert to blood glucose.
‘Flexible’ Insulin Therapy and the Food You Eat
Flexible insulin therapy provides most people with diabetes with
a better match between their insulin and food. This therapy is called “flexible” because it can help give you more freedom and flexibility in your lifestyle. The key is to learn how to bolus (give rapid or short-acting insulin) before your meals in combination with basal (long-acting) insulin at other times. Deciding on the correct bolus dose you should take before meals will depend on the amount of carb you have eaten.
Carbohydrate (Carb) Counting
Carbohydrate is the nutrient that most affects your blood glucose. It is important to remember that 100 percent of the carb you eat appears in your bloodstream as blood glucose within a few hours after you have eaten! When you use the carb counting method of meal planning, you add up all the carb that you eat for a period of time.
Your Carb-to-Insulin Ratio
Once you know the amount of carb you have eaten in a specific time frame, you can figure out the amount of insulin that you will need to “cover” a specific amount of carbohydrate. This is called your carb : insulin (carb-to-insulin) ratio. Knowing your ratio will help you decide how much insulin you need to take to match the amount of carbohydrate that you are planning to eat. The carb : insulin ratio can be different for each meal.
Your carb : insulin ratio should help you keep your blood glucose in its target range after meals. Since the grams of carb you have eaten determine the amount of insulin to be given, you will need to learn to weigh and measure your foods – especially when you are beginning to use this method. Reference charts and nutrition labels will also help you find out the grams of carbohydrate in the food you eat.
Learn About Bolus Insulin Dosing
You will learn how to practice bolus insulin dosing by writing down your blood glucose and your carb intake. This will help your healthcare team develop the right carb : insulin ratio for you. This ratio will tell you the amount of rapid acting insulin (Humalog®, Novolog®, Apidra®) you should take for a specific amount of carb that you plan to eat. The example below shows how a carb : insulin ratio is used.
Example:
Question:
Jane’s Carb : Insulin Ratio is 15:1.
She has eaten 60 grams of carbohydrate. How much insulin should Jane take?
Answer:
Since 1 unit of insulin covers 15 grams of carbohydrate, Jane should take 4 units of rapid acting insulin. She will know that this ratio is working if she checks her blood glucose two hours after the meal and finds that it is within 20-40 mg/dl of her before-meal glucose level.
For more information about determining carb : insulin ratios, read the BD booklet, Staying on Target™: Your
Insulin Adjustment Workbook. Yes, You Can Do It! May be found on-line at: www.bddiabetes.com/us/ download/download.asp
Jane’s Breakfast Carb
Food Grams of
Carbohydrate 1/2 cup branflakes 15
1 cup 2% milk 15
1/2 banana 15
1 slice toast 15
1 egg 0
Know Your Carb!
Once you know how to count carb you should also be aware that the type of carb selected might impact your blood glucose levels two hours after eating. Here is how it works.
If your carbohydrate choices are:
• Refined or Processed Carb (white rice, mashed
potatoes, desserts, white flour grain products, fruit juices, etc.) and if they are more then 10 percent of the total amount of carbohydrate you have eaten, your blood glucose may rise too quickly for your insulin dose to “match” the glucose “rise.”
• High Fiber Carb(whole grains, brown rice,
potato with skin, soy protein, or whole fruits) your blood glucose will rise more slowly. When you choose high fiber foods
combined with protein and fat – and spread food portions throughout the day – this will usually result in better blood glucose readings two hours after a meal.
Balance Your Total Nutrients
Carbohydrate has a dramatic effect on your blood glucose levels, while protein and fat play a minor role in the rise of your blood glucose levels after meals.
When you eat protein and fat in reasonable amounts (3 to 6 ounces of protein and 1 to 3 servings of fat), then your basal (background) insulin (NPH, Lantus®, Levemir®) and your daily activity levels will usually compensate for the glucose you get from these foods. However, if you eat very large protein and fat portions, your blood glucose may be within target range at 2 hours after your meal, but will be too high 4 to 6 hours after the meal.
Check your Ratio
To make sure that your insulin : carb ratio is correct, you should check your blood glucose before meals and two hours after meals. If your blood glucose rises 20-40 mg/dl after your meal compared to the reading before the meal, then your insulin dose matched. However, if your blood sugar is greater than 20-40 mg/dl, then your insulin dose did not match your blood glucose. In this case you might consider the following actions:
1. Decrease your total amount of carb. 2. Decrease the amount of refined
foods you eat.
3. Replace the refined foods with high fiber food, or
4. Increase the amount of insulin to match the amount of carb. For more information about
carbohydrate counting and carb : insulin ratios, read the booklet, BD Staying on Target™, Carb Counting: Eat to Win! May be
Your Plan for Exercise
Did You Know That Your Physical Activity Affects Your Blood Glucose?
Physical activity is important for everyone, but is especially important for people with diabetes because it can help lower your blood glucose. The best way to be physically active is to stick to a regular routine and do something you like. Even routine chores can be counted as physical activity. Moving your muscles in any way is considered physical activity. Make sure that you check with your doctor before starting any exercise or physical activity that is more than what you are doing now.
When You Are More Active Than Usual
When you increase the amount of exercise you are getting, you may need to make some adjustments in your food or schedule to prevent hypoglycemia (low blood glucose). The cells in your muscles use glucose at an increased rate with activity. Sometimes, blood glucose levels can drop too low. The low blood glucose can also happen hours after exercise or physical activity, as there is a sustained increased uptake of glucose by the muscles.
Regular physical activity helps to lower your blood glucose because it helps insulin work better. This means that when you are exercising, you may need to:
• Eat or drink more. • Take less insulin.
If you are more active than usual, it is also wise to check blood sugar levels at 3:00 AM to make sure that you are not having a low blood glucose reaction at that time. Protecting Against Low Blood Glucose
To prevent low blood glucose reactions (hypoglycemia) during activity, make sure that you have eaten enough carbohydrate to balance the amount of activity or exercise you plan to do. Carb provides the glucose that your muscles will need to use for energy.
When You Are Involved in Unexpected Exercise
During unplanned physical activity, carb replacement may be needed to prevent low blood glucose when:
• Insulin adjustments are not made
• Exercise occurs several hours after a meal
• Exercise lasts for a long time
The amount of extra carb you will need depends on the amount of time spent exercising related to your:
• Medication; • Meal;
• Type, intensity and duration of exercise; and • Pre-exercise glucose level.
Use the following guide to help decide how much carb to eat before you exercise.
Carbohydrate Replacement During Exercise3 Intensity of
Exercise
Duration (minutes)
Carbohydrate
Replacement Frequency Mild to
Moderate < 30
May not be needed
Moderate 30 to 60 15 grams Each hour
High 60+ 30 to 50 grams Each hour
3Leborvitz, H.E., ed. Therapy for Diabetes Mellitus and Related Disorders.Fourth
If you are watching your weight, it may be advisable to decrease the amount of insulin you take before the exercise or activity. Check with your health care provider.
Check Your Blood Glucose Levels Before and After Activity
By doing so you will be able to see how well your adjustment of insulin or carb worked. Making note of your pattern of glucose levels after your adjustments can help guide your future insulin doses and pre-activity carb intake. Be sure to record your blood glucose results, amount of carb eaten, insulin dose and type of activity in a logbook. It can be very helpful to download the memory feature
of your meter to a computer program for this purpose.
Using Pattern Management
Step 1:Write down your blood glucose numbers over a period of days.
Use columns according to time of day and relationship to meals or snacks.
Step 2:Look at the numbers for general patterns.
Note the time of day (before breakfast, before lunch, before dinner and at bedtime). Step 3:Identify readings above or below
your target levels.
Use a highlighter pen to clearly mark out-of-target readings. Step 4:Once you have identified the pattern, decide which variables may have caused readings outside your targets.
Step 5:Making sure you only adjust one
variable at a time, take the following actions:
• Change the amount or timing of the carb eaten.
• Increase or decrease the length of time or day that you exercise.
• Adjust the dose of insulin or the time the insulin is given.
Step 6:If the insulin dose needs to be adjusted, decide which insulin needs to be changed.
To help you with this decision, please scroll back to the section entitled “Injected Insulin Acts at Different Speeds” and check the chart called “The Timing of Injected Insulin” that lists Names of Insulin, Types, Peak Action and Effect on Blood
Glucose. Your next step is to consult your healthcare team members (physician and certified diabetes educator). They will assist you and answer questions as you learn to do this. It is important to understand why your doctor or diabetes educator recommends the changes. After you analyze a few of your records in this way, you may be comfortable making insulin changes on your own.
Practice Example:
Sam’s blood glucose patterns:
Sam’s Three-Day Blood Glucose Diary Target Blood Glucose: 90-130 mg/dl
Breakfast Lunch Dinner Bedtime
Before Insulin After Before Insulin After Before Insulin After Insulin
158 8 H 215 4 H 117 6 H 78 15 L
173 8 H 226 4 H 135 6 H 63 15 L
Did you notice these patterns?
1. Before-breakfast numbers are somewhat high 2. Before-lunch numbers are very high
3. Before-dinner numbers are in the target range 4. Bedtime readings are low
Breakfast:
Why are Sam’s breakfast numbers high?
Sam needs to think backwards. What did he eat the night before? Did he have a snack before he went to bed? Was it larger than usual? What time did he eat dinner? Did he eat more or less carbs than usual? Eating a larger snack
at night or a larger meal with more carbs or later in the evening will increase the blood glucose level in the morning. Sam should consider the following changes:
1. Eating his snack or meal earlier in the evening. 2. Eating fewer carbs at the evening meal
or snack.
3. Plan to exercise in the evening, this will help the blood glucose remain low overnight.
Lunch:
What could be making Sam’s blood glucose the highest
before lunch? It could be that if he improves his lunch
numbers, which are the highest of the day, the rest of the day will improve automatically.
1. Sam is not getting enough rapid acting insulin (such as Humalog®) before breakfast, or
2. He is eating too much high-carbohydrate, high-fat foods for his breakfast.
Sam should consider the following actions: 1. Take more Humalog® at breakfast or 2. Eat less breakfast, or less
carbohydrate at breakfast, or 3. Exercise in the morning
to help to correct the blood glucose level.
Dinner:
Sam’s dinner numbers are in his target range, so no changes are necessary!
Bedtime:
Sam’s bedtime numbers are low, so he may
need changes. He should consider:
1. Less Humalog® at dinner, or
2. More carbohydrate, orprotein at dinner 3. Orperhaps a snack before evening exercise to
prevent a low blood glucose level at bedtime.
Remember: You must consider all the variables before you make a decision about the action you should take.
Balancing Your Variables
To better control your blood glucose levels, it is best to maintain a regular schedule of daily meal and exercise times. If there are many variables that
change on a daily basis, such as food, meal times, insulin doses, and/or type and duration of exercise, it will take more time to get all these factors balanced. Once you understand how each variable affects your blood glucose, you will be able to vary each, one at a time, to achieve more flexibility in your lifestyle.
Preventing Low Blood Glucose Before it Happens:
When you are having patterns of low blood glucose, try to prevent them before they happen. Some people are able to easily recognize and treat low blood glucose and do not think it is a problem. However, if you often have low blood glucose at certain times of the day or night, you are at risk for having a more severe low blood glucose that may be more difficult to treat.
Be Aware of High Blood Glucose Levels
On the other hand, it is also very common to have a high blood glucose level sometime after a low one because:
1. Your body makes hormones to counteract the low blood glucose.
2. Most people have a tendency to “over-treat” a low blood glucose because they feel uncomfortable.
Troubleshooting your Blood Glucose
Questions to Ask Yourself When You See Patterns Of Low Blood Glucose:
1. Have I been too busy to check my blood glucose before meals so that I am not sure if I am taking the right amount of insulin?
2. Have I been taking too much insulin? 3. Have I been eating
less than usual?
4. Am I eating different types of foods? 5. Are meals being skipped or delayed? 6. Do I have a new activity, or has my
activity increased?
A YES answer to any one of the questions above could cause low blood glucose.
Questions to Ask Yourself When You See Patterns Of High Blood Glucose:
1. Have I forgotten to check my blood glucose before meals so that I am not sure if I am taking the right amount of insulin?
2. Have I been taking my insulin on time and in the right amount?
3. Have I been eating more then usual?
4. Have I been eating extra snacks or sweets?
5. Has my physical activity been less than usual?
6. Do I have a cold, infection or illness? 7. Am I having more stress in my life?
A “yes” answer to any one of the questions above could cause high blood glucose. A combination of any of the events listed could cause high or low blood glucose.
Pattern Management Guidelines
for Making Adjustments
When you try to fix a problem pattern, do it one step at a time. If you change too many things at once, you will not know what is causing what! It is best to make one change at a time, wait for the result, then make another as needed. A good idea is to wait three days to see if a pattern forms.
1. When you cannot explain a low blood glucose level by too much insulin, inadequate food, or exercise, an insulin dose adjustment should be made before the next dose. Do not wait for a second low blood glucose level! Call your doctor
or health care team for help right away. Always be prepared for a low blood glucose reaction by having carbohydrates such as milk, soda, hard candies or glucose
tablets available.
2. If patternsof “lows” are occurring that can be explained by too much insulin, not enough food, skipping meals, or exercise, then try to change whatever the problem may be. (One high blood sugar, although not desirable, will happen occasionally but is not something you should worry about.)
3. If you do make changes to your insulin dose, do not do so by more than 10 percent of the dose4
unless you are advised to do so by your doctor. For example, if your usual dose is 10 units, you can safely make changes in 1 unit increments, so that you could take 9 units as needed. 4. Make the change that is easiest to do first. 5. If one type of adjustment doesn’t work,
try something else.
6. Always remember to call your diabetes educator, dietitian or doctor for help.
Practice Problems:
Stella’s Blood Sugars Are Usually High At Lunch: What Should She Do?
Pattern: When Stella noticed that she had a pattern
of high blood glucose readings at lunch, she thought about the different ways she could fix the problem.
Possible Adjustments:
Stella considered three possibilities. • Exercise after breakfast.
• Eat less breakfast or morning snack. • Take more insulin at breakfast.
Stella decided that her busy schedule did not give her enough time to exercise after breakfast. She thought that the breakfast she ate was adequate and didn’t
want to change it. But, she decided to omit the mid-morning snack that she sometimes had with her coffee, as she wasn’t really hungry anyway. However, her lunch blood glucose levels were still high even on the days when she didn’t eat a snack.
Solution: Stella decided that the easiest and best thing
to do would be to take more insulin at breakfast. She called her diabetes educator the first few times she made the adjustment, just to be sure she was
doing it correctly.
In the Following Examples See If You Can Recognize A Problem Pattern and Figure Out the Solution
Dave’s Blood Glucose Diary
Target Blood Glucose: Pre-meal: 90-130 mg/dl
Post-meal: Less than 180 mg/dl
Pattern: These blood glucose levels look excellent.
They are in the 90-130 mg/dl target range before meals and under the 180 target after meals.
Solution: No problem! No changes are necessary.
Breakfast Lunch Dinner
Pre Insulin Post Pre Insulin Post Pre Insulin Post
99 12 H 145 133 3 H 178 14 H 144
105 181 81 137 10 L 130
Marita’s Blood Glucose Diary
Target Blood Glucose: Pre-meal: 90-130 mg/dl
Post-meal: Less than 180 mg/dl
Pattern: Blood glucose levels are in target range before
breakfast and lunch and seem to be fine even after dinner. However, blood glucose 1 to 2 hours after breakfast and lunch are quite high.
Consider the Possible Causes:
• Too much food at breakfast and lunch. • Not enough insulin at breakfast and lunch.
(The amount of carbohydrate eaten is not well covered by insulin.)
Solution:
1. Cut the amount of carbohydrate eaten at breakfast and lunch. 2. Increase the Humalog®/Novolog®
insulin at breakfast and lunch
Marita decided to cut 15 g. of carbohydrate from breakfast as she was always in a rush and didn’t have time to enjoy it anyhow. She wanted to eat all of her lunch, however, so she added a unit on to her lunchtime Humalog® dose.
Breakfast Lunch Dinner
Pre Insulin Post Pre Insulin Post Pre Insulin Post
94 5 H 253 129 3 H 299 5 H 138
107 320 86 180 12 L 140
Bill’s Blood Glucose Diary
Target Blood Glucose: Pre-meal: 90-130 mg/dl
Post-meal: Less than 180 mg/dl
Pattern: The breakfast blood sugars are a bit higher
than desired for a 90 to130 target, lunch and dinner are okay, and bedtime numbers are too low.
Possible Causes:
1. Morning highs could be high because too much food is eaten at bedtime, or because more bedtime insulin is needed.
2. Bedtime low blood glucose readings could have several causes (not enough dinner eaten, too much insulin is given at dinner, or exercise after dinner).
Possible Solutions:
1. Reduce amount of bedtime snack or change types of foods.
2. Either eat more dinner or take less insulin. 3. Stop exercising after dinner.
Breakfast Lunch Dinner
Pre Insulin Post Pre Insulin Post Pre Insulin Post
180 10 H 98 5 H 178 10 H 96
156 103 87 15 L 68
201 89 125 70
Bill always took his dog for a long walk after dinner and decided that was the most likely reason that his blood glucose levels dropped in the evening. However, he did not want to give it up (neither did his dog) as he knew that the exercise was good for him. He decided to cut back his dinner insulin a bit. He discovered that when his blood glucose was normal at bedtime, he did not overeat. He realized that he had been “over-treating” his low blood sugars and that made the morning numbers high. Once he no longer had low blood glucose in the evening, his morning blood glucose fell into the target.
Kelly’s Blood Glucose Diary
Target Blood Glucose: Pre-meal: 90-130 mg/dl
Post-meal: Less than 180 mg/dl
Kelly is taking Lantus® insulin at bedtime with Humalog® to cover meals.
Breakfast Lunch Dinner
Pre Insulin Post Pre Insulin Post
(3pm) Pre Insulin Post
112 6 H 134 8 H 59 172 10 H 93
156 98 44 187 12 L 210
85 87 77 122 117
Pattern: Breakfast, lunch and bedtime numbers look generally okay. Although a few are above target, there is no pattern. However, blood glucoses
are generally too low at 3 PM.
Consider the Possible Causes:
1. Kelly isn’t eating enough at lunch.
2. She needs less insulin at lunch. 3. Kelly needs to cover her
afternoon exercise with food.
Solution: Kelly’s lunch was early, at 11AM.
As a schoolteacher, she was busy all day.
Therefore, although she thought that eating more lunch or taking less insulin at lunch time might help, she decided that instead of eating more at lunch time, she would eat some crackers around 2:30 PM, to avoid the mid-afternoon slump.
Keep Up the Good Work!
We hope that this introduction to Pattern Management has helped you understand how to identify problem patterns in your diabetes control and decide on possible ways of fixing the problem. Of course, if you cannot fix the problem yourself, it is most important to call your diabetes health professional for guidance. Do not make insulin adjustments without having learned how to do so or without your doctor’s permission. In time and with a little practice, Pattern Management can help put you on the path to good control.
Educational Information from BD Medical Diabetes Care. BD, BD Logo and Staying on Target are the property of
BD provides this brochure for informational purposes only. It is not intended to be a substitute for professional medical advice, diagnosis or treatment. Always seek the advice of you physician or other qualified healthcare provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay in seeking it because of something you have read in this brochure.
Written by:
Kris Knutson, RN, BSN, CDE Joyce Malaskovitz, PhD, RN, CDE Margaret Riedl, RD, CDE
Las Vegas, NV
We wish to acknowledge the following health professionals for reviewing this publication and providing their valuable insights: Jean E. Betschart Roemer, CPNP, MSN, MN, CDE
Pittsburgh, PA
Linda Urso, APRN, BC-ADM Warren, MI
Kathleen C. Arnold, CS-ANP, BC-ADM, CDE Gulfport, MS
BD Medical Diabetes Care
1 Becton Drive
Franklin Lakes, NJ 07417-1883 1.888.BDCARES (232.2737)