EXPERIENCE AND REASON—Briefly Recorded
‘‘In Medicine one must pay attention not to plausible theorizing but to experience and reason together. . . . I agree that theorizing is to be approved, provided that it is based on facts, and systematically makes its deductions from what is observed. . . . But conclusions drawn from unaided reason can hardly be serviceable; only those drawn from observed fact.’’ Hippocrates:Precepts. (Short communications of factual material are published here. Comments and criticisms appear as letters to the Editor.)
Unbound Bilirubin in a Term
Newborn With Kernicterus
ABBREVIATIONS. K, equilibrium association binding constant; ABR, auditory brainstem response; G6PD, glucose-6-phosphate dehydrogenase.
I
n premature newborns, bilirubin-inducedchanges in the auditory brainstem response (ABR) begin at unbound (nonalbumin-bound or “free”) bilirubin levels above .5 g/dL,1 and
ker-nicterus becomes likely at levels between⬃1 and 1.5
g/dL (.017-.026 mol/L).2,3 In term newborns,
however, unbound bilirubin levels between .9 and 2
g/dL, which would be associated kernicterus in premature newborns, produce only subtle, reversible changes in ABR wave latency and amplitude.4
Al-though the unbound bilirubin levels associated with kernicterus in term newborns are unknown, they clearly are greater than the levels associated with kernicterus in premature infants. This indicates that, as with the total bilirubin and total bilirubin/albu-min ratio, the unbound bilirubin levels associated with kernicterus increase as birth weight and gesta-tion increase.1,5
We have been using a Food & Drug Administra-tion-approved method6for measuring unbound
bil-irubin in jaundiced newborns as an adjunct to their clinical care since 1998. We use a weight-based un-bound bilirubin reference value of 1.3g/dL/kg (the level of unbound bilirubin at which exchange trans-fusion should be considered) up to a maximum of 4
g/dL to accommodate the need to increase the reference unbound bilirubin as birth weight in-creases and to incorporate the solubility limits of unbound bilirubin at ph 7.4 (⬃4 g/dL) into the reference criteria.1–5,7–9
We recently encountered a term, jaundiced new-born that developed acute shock and died, appar-ently from kernicterus. This report describes the in-fant’s clinical course and bilirubin-albumin binding data. This case provides insight into the levels of unbound bilirubin associated with kernicterus in term infants as well as the acute changes in
distribu-tion of the bilirubin load (miscible bilirubin pool) between the tissues and the vascular space following the onset of kernicterus.
CASE REPORT
A 110-hour-old (4.5-day-old) Nigerian male newborn presented to the emergency department of our hospital with an 18-hour history of moaning and refusing to feed. He was born at 39 and 5/7 weeks gestation to a 34-year-old gravida 1 woman who had an unremarkable pregnancy except for a questionable bout of malaria during the first trimester in Nigeria. The remainder of her preg-nancy was spent in the United States where she received good prenatal care. Her blood type was B positive with negative anti-bodies, and her vaginal group B streptococcus culture was nega-tive before delivery. Vaginal delivery was uncomplicated with Apgar scores of 7 and 9 at 1 and 5 minutes, respectively. Birth weight was 2609 g (head circumference 34.5 cm, length 48 cm) and the physical examination was normal. The infant was discharged at 42 hours of age weighing 2524 g (weight loss 3.2%), “breast-feeding well,” passing urine and stool, and had “mild jaundice,” but the bilirubin was not measured. Verbal and written instruc-tions were given to the mother to observe the infant for further jaundice and to call her private physician if the jaundice wors-ened. The infant was seen for a routine postpartum visit at⬃86 hours of age (3.5 days of age). At that visit the infant’s vital signs and physical examination were normal except for jaundice to the abdomen. He was observed to be breastfeeding well and making normal “cooing” sounds. The bilirubin was not measured, and the mother and infant were sent home with reassurance. Soon after returning home, the infant became fussy, refused to feed, and started “moaning”. Overnight he became increasingly lethargic and eventually anuric. The following morning he was taken to the emergency department where the vital signs showed a heart rate of 150 beats per minute and a temperature of 37.3°C. His weight had decreased 9% from birth weight to 2400 g. He appeared dehydrated but otherwise responded appropriately and was ad-mitted to the hospital. A sepsis evaluation was undertaken, in-cluding a lumbar puncture, which he tolerated well. Approxi-mately 30 minutes after arrival he was given a bolus of normal saline, antibiotics were started, and he was able to breast feed. He appeared alert, but his axillary temperature had decreased to 33°C (confirmed rectally). The capillary refill time was⬃3 seconds, and additional warming measures were instituted and another saline bolus was given. Admission laboratory data then returned show-ing a white blood count of 2100/mm3 with 24% neutrophiles (absolute neutrophile count 504/mm3) and no band forms. The hematocrit was 34% and the platelet count 85 000/mm3. The se-rum chemistry panel revealed a sodium of 144 meq/L, creatinine of 0.1 mg/dL, glucose of 34 mg/dL, albumin of 2.8 g/dL, total bilirubin of 31.7 mg/dL, and the unbound bilirubin was 7.7g/ dL. The spinal fluid glucose was 11 mg/dL, the protein 91 mg/dL, and the Gram-stain negative for bacteria. After the bilirubin value was reported, intravenous albumin and dextrose were given, but while arrangements were being made to transfer the infant to the newborn intensive care unit for an exchange transfusion, the infant suddenly became apneic, unresponsive, and developed sei-zures. The infant was resuscitated for several hours with mechan-ical ventilation, vasopressors, and blood components, but died 9 hours later without becoming stable enough to receive an ex-change transfusion. Three hours after the initial arrest, the infant’s serum total bilirubin had fallen to 6.9 mg/dL, the albumin to 1.0 g/dL (despite administration of albumin), and the unbound bili-rubin to 1.9g/dL. The total bilirubin and albumin were repeated
Received for publication May 7, 2002; accepted Sep 12, 2002.
Reprint requests to (C.E.A.) Division of Neonatology, Department of Pedi-atrics, California Pacific Medical Center, 3850 California St, San Francisco, CA 94118. E-mail: ligand@centurytel.net
PEDIATRICS (ISSN 0031 4005). Copyright © 2003 by the American Acad-emy of Pediatrics.
and found to be correct. All cultures (blood, cerebral spinal fluid, and urine) were negative for bacteria. The red blood cell glucose-6-phosphate dehydrogenase (G6PD) test showed deficiency of the enzyme. Further history revealed no known drug or chemical exposure that might have induced hemolysis. Genetic analysis performed by Dr E. Beutler at Scripps Research Institute (La Jolla, CA) showed the infant to be hemizygous for G6PD A negative, confirming the diagnosis of G6PD deficiency, and homozygous for (Ta)6/(Ta)6, indicating that the infant did not have Gilbert’s disease.10The carboxyhemoglobin level performed by Dr H. Vre-man at Stanford University (Stanford, CA) was 0.57% (normal).11 At autopsy, kernicterus was present grossly and microscopically. There was inflammation in the spleen suggestive of infection, but no other evidence of infection or hemolysis was found in any of the other organ systems including the meninges.
DISCUSSION
The sudden deterioration in this infant was pre-sumed because of sepsis as supported by the neutro-penia, thrombocytoneutro-penia, hypoglycorrhachia, and splenitis at autopsy. However, the lack of positive blood cultures and the absence of strong evidence for sepsis at autopsy suggest that acute bilirubin enceph-alopathy (kernicterus) played a significant role in the demise of this newborn. Although recovery from acute bilirubin encephalopathy is generally expected, bilirubin encephalopathy can be lethal.10,12
Before the infant’s acute deterioration, the un-bound bilirubin concentration at the total bilirubin of 31.7 mg/dL and albumin of 2.8 g/dL (bilirubin/ albumin molar ratio 1.25) was 7.7g/dL (2.9g/dL per kg) measured using an Arrows UB-analyzer (Ar-rows Co Ltd, Osaka, Japan)6and corrected for rate
limiting dissociation of bilirubin from albumin.13
This is the highest unbound bilirubin concentration measured in several hundred newborns at our insti-tution over the last 3 years and well beyond both our 1.3g/dL per kg and 4g/dL reference value limits for unbound bilirubin.
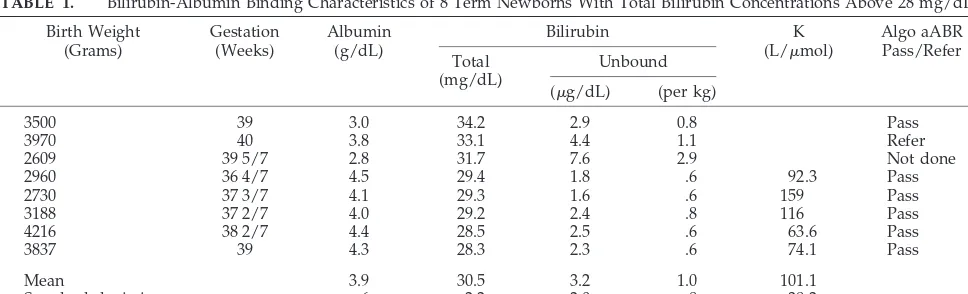
The Table contains bilirubin binding and hearing screening data from 8 term newborns (including this patient) with total bilirubin levels between 28 and 34 mg/dL. The mean unbound bilirubin concentration for the group if this infant is excluded declines to 2.5
g/dL and 0.7g/dL per kg. The only other infant with an unbound bilirubin concentration beyond 4
g/dL (but still below the 1.3g/dL per kg refer-ence value) had a “refer” hearing screening at the
time of admission but passed the hearing screen after receiving an exchange transfusion. It should be noted that infants with unbound bilirubin levels above 1
g/dL may have subtle bilirubin-induced ABR wave latency and amplitude changes that would have been detected by formal ABR testing4but might still pass
an Algo hearing screening test, which only looks for the presence of wave V. All the infants with total bilirubins above 30 mg/dL (except the reported case) received exchange transfusions according to the American Academy of Pediatrics guidelines.14 It is
arguable whether the exchange transfusions were really needed in the infants with unbound bilirubin levels below both the reference levels of 4g/dL and 1.3 g/dL per kg and who passed their hearing screen. Further study of the relationship between bilirubin binding and ABR changes might improve our ability to determine which infants with very high total bilirubins require exchange transfusion in addi-tion to phototherapy.
The total bilirubin spontaneously fell (verified by repeat analysis) to 6.9 mg/dL, the albumin to 1 g/dL (bilirubin/albumin molar ratio .7 vs 1.25 on presen-tation to the hospital), and the unbound bilirubin to 1.9g/dL following the acute onset of bilirubin en-cephalopathy, as has been described previously.15
This paradoxical decline in total bilirubin during acute bilirubin toxicity illustrates how rapidly the total bilirubin may change and how potentially mis-leading it can be as an indicator of the true bilirubin load, which is the primary determinant of the risk of kernicterus.16 Without knowledge of the admission
laboratory values, the role of bilirubin toxicity in this infant would not have been apparent until autopsy. The equilibrium association binding constant (K) for the infant at a total bilirubin of 6.9 mg/dL, albu-min of 1 g/dL, and unbound bilirubin of 1.9g/dL is 110 L/mol, similar to the mean K for the new-borns in the Table. At this level of unbound bilirubin, subtle bilirubin-induced changes in the ABR would be expected although the total bilirubin is quite low.4
Furthermore, it can be shown that at this very low albumin the total bilirubin would only need to rise above 7.5 mg/dL for the unbound bilirubin to ap-proach its solubility level of 4g/dL. At the infant’s
TABLE 1. Bilirubin-Albumin Binding Characteristics of 8 Term Newborns With Total Bilirubin Concentrations Above 28 mg/dL Birth Weight (Grams) Gestation (Weeks) Albumin (g/dL) Bilirubin K
(L/mol)
Algo aABR Pass/Refer Total
(mg/dL)
Unbound (g/dL) (per kg)
3500 39 3.0 34.2 2.9 0.8 Pass
3970 40 3.8 33.1 4.4 1.1 Refer
2609 39 5/7 2.8 31.7 7.6 2.9 Not done
2960 36 4/7 4.5 29.4 1.8 .6 92.3 Pass
2730 37 3/7 4.1 29.3 1.6 .6 159 Pass
3188 37 2/7 4.0 29.2 2.4 .8 116 Pass
4216 38 2/7 4.4 28.5 2.5 .6 63.6 Pass
3837 39 4.3 28.3 2.3 .6 74.1 Pass
Mean 3.9 30.5 3.2 1.0 101.1
Standard deviation .6 2.2 2.0 .8 38.2
aABR indicates automated ABR.
K is the equilibrium association constant, assuming single site bilirubin-albumin binding. Pass or Refer indicates the presence (Pass) or absence (Refer) of ABR wave V at 35 dB SPL as determined by the Algo aABR response system (Natus Medical, San Carlos, CA).
EXPERIENCE AND REASON 1111
at Viet Nam:AAP Sponsored on August 30, 2020
www.aappublications.org/news
initial albumin of 2.8 g/dL and a K of 110 L/mol, the unbound bilirubin would reach 4 g/dL at a total bilirubin of⬃20 g/dL and 1.3g/dL per kg at total bilirubin of 17 mg/dL. This case is a poignant example of the need to interpret the total bilirubin in the context of the albumin concentration and in par-ticular the unbound bilirubin concentration.3,15,17
The course of the clinical events is consistent with the hypothesis that kernicterus in this particular in-fant began with the unbound bilirubin reaching its solubility limit. Bilirubin precipitation7–9 then
dam-ages the blood brain barrier subsequently allowing both albumin bound and unbound bilirubin to exit the vascular space. The fall in bilirubin/albumin mo-lar ratio from 1.25 on admission to .7 in 3 hours suggests that more bilirubin than albumin exited the vascular space. However, the susceptibility of pre-mature newborns to kernicterus at unbound biliru-bin concentrations well below its theoretical solubil-ity limits1,2 indicates that the pathogenesis of
bilirubin toxicity is complex, and many factors such as the relative maturity of the central nervous system and tissue bilirubin levels may predispose an infant to kernicterus before the solubility of unbound bili-rubin becomes a factor.1–3
For the total bilirubin to have reached 31.7 mg/dL with an unbound bilirubin of 7.7 g/dL an extremely large bilirubin load must have been present. The large bilirubin load does not appear because of greatly increased hemolysis, since the carboxyhemo-globin level was normal and the hematocrit 34%. This supports the hypothesis that poor hepatic con-jugation and excretion of bilirubin may sometimes play an important role in kernicterus associated with G6PD deficiency, although the infant did not have Gilbert’s disease.
It is disconcerting that even with early postnatal hospital discharge follow-up, kernicterus still oc-curred. Clinicians caring for jaundiced newborns must deal not only with the inherent risk in not measuring bilirubin levels when newborns appear jaundiced, but also with the reality that total biliru-bin levels alone can be quite misleading.3,15,17 The
latter is caused in part by the significant variability in bilirubin-albumin binding,18 which reduces the
cor-relation between the risk of bilirubin toxicity (biliru-bin load) and the total biliru(biliru-bin.
Newer methods for predicting bilirubin load such as the age-specific total bilirubin and end tidal car-bon monoxide levels have been disappointing.16
Measuring the unbound bilirubin concentration and albumin concentration, and performing hearing screening can provide critically important additional information about the risk of bilirubin toxicity in jaundiced newborns. Furthermore, the unbound bil-irubin along with the total bilbil-irubin and albumin can be used to estimate the specific total bilirubin at which the unbound bilirubin level reaches reference levels (1.3 g/dL per kg or its solubility limit of 4
g/dL).9Once that specific total bilirubin of concern
has been identified by measuring bilirubin binding in addition to the total bilirubin, a more individual-ized and rational approach to newborn jaundice be-comes possible. This case along with the consider-able body of evidence documenting the potential usefulness of bilirubin binding measurements in jaundiced newborns indicates that further studies of bilirubin binding measurements in the jaundiced newborns are warranted.
Charles E. Ahlfors, MD Oded Herbsman, MD
Department of Pediatrics California Pacific Medical Center San Francisco, California 94118
REFERENCES
1. Amin SB, Ahlfors C, Orlando MS, Daizell LE, Merle KS, Guillet R. Bilirubin and serial auditory brainstem responses in premature infants.
Pediatrics.2001;107:664 – 670
2. Nakamura H, Yonetani M, Uetani Y, Funato M, Lee Y. Determination of serum unbound bilirubin for prediction of kernicterus in low birth weight infants.Acta Paediatr Jpn.1992;34:642– 647
3. Ahlfors CE. Unbound bilirubin associated with kernicterus: a historical approach.J Pediatr.2000;137:540 –544
4. Funato M, Tamai H, Shimada S, Nakamura H. Vigintiphobia, unbound bilirubin, and auditory brainstem responses.Pediatrics.1994;93:50 –53 5. Ahlfors CE. Criteria for exchange transfusion in jaundiced newborns.
Pediatrics.1994;93:488 – 494
6. Shimabuku R, Nakamura H. Total and unbound bilirubin determina-tion using an automated peroxidase micromethod. Kobe J Med Sci.
1982;28:91–104
7. Brodersen R, Funding L, Pedersen AO, Ro¨igaard-Petersen H. Binding of bilirubin to low-affinity sites of human serum albumin in vitro followed by co-crystallization.Scand J Clin Lab Invest.1972;29:433– 446 8. Hahm J-S, Ostrow JD, Mukerjee P, Celic L. Ionization and
self-association of unconjugated bilirubin, determined by rapid solvent partition from chloroform, with further studies of bilirubin solubility.J Lipid Res.1992;33:1123–1137
9. Ahlfors CE. Bilirubin-albumin binding and free bilirubin.J Perinatol.
2001;21:S40 –S42
10. Slusher TM, Vreman HJ, McLaren DW, Lewison LJ, Brown AK, Steven-son DK. Glucose-6-phosphate dehydrogenase deficiency and carboxy-hemoglobin concentrations associated with bilirubin-related morbidity and death in Nigerian infants.J Pediatr.1995;126:102–108
11. Vreman HJ, Kwong LK, Stevenson DK. Carbon monoxide in blood: an improved microliter blood-sample collection system, with rapid analy-sis by gas chromatography.Clin Chem.1984;30:1382–1386
12. Zuelzer WW, Mudgett RT. Kernicterus: etiologic study based on an analysis of 55 cases.Pediatrics.1950;6:452– 474
13. Ahlfors CE, DiBiasio-Erwin D. Rate constants for dissociation of biliru-bin from its biliru-binding sites in neonatal (cord) and adult sera.J Pediatr.
1986;108:295–298
14. American Academy of Pediatrics, Provisional Committee for Quality Improvement and Subcommittee on Hyperbilirubinemia. Practice parameter: management of hyperbilirubinemia in the healthy term newborn.Pediatrics.1994;94:558 –565
15. Harris RC, Lucey JF, MacLean JR. Kernicterus in premature infants associated with low concentration of bilirubin in the plasma.Pediatrics.
1958;21:875– 883
16. Stevenson DK, Fanaroff AA, Maisels MJ, et al. Prediction of hyperbil-irubinemia in near-term and term infants.Pediatrics.2001;108:31–39 17. Perlman JM, Rogers BB. Kernicteric findings at autopsy in two sick near
term infants.Pediatrics.1997;99:612– 615
18. Cashore WJ. Free bilirubin concentrations and bilirubin-binding affinity in term and preterm infants.J Pediatr.1980;96:521–527
DOI: 10.1542/peds.111.5.1110
2003;111;1110
Pediatrics
Charles E. Ahlfors and Oded Herbsman
Unbound Bilirubin in a Term Newborn With Kernicterus
Services
Updated Information &
http://pediatrics.aappublications.org/content/111/5/1110
including high resolution figures, can be found at:
References
http://pediatrics.aappublications.org/content/111/5/1110#BIBL
This article cites 18 articles, 10 of which you can access for free at:
Subspecialty Collections
sub
http://www.aappublications.org/cgi/collection/fetus:newborn_infant_
Fetus/Newborn Infant following collection(s):
This article, along with others on similar topics, appears in the
Permissions & Licensing
http://www.aappublications.org/site/misc/Permissions.xhtml
in its entirety can be found online at:
Information about reproducing this article in parts (figures, tables) or
Reprints
http://www.aappublications.org/site/misc/reprints.xhtml
Information about ordering reprints can be found online:
at Viet Nam:AAP Sponsored on August 30, 2020
www.aappublications.org/news
DOI: 10.1542/peds.111.5.1110
2003;111;1110
Pediatrics
Charles E. Ahlfors and Oded Herbsman
Unbound Bilirubin in a Term Newborn With Kernicterus
http://pediatrics.aappublications.org/content/111/5/1110
located on the World Wide Web at:
The online version of this article, along with updated information and services, is
by the American Academy of Pediatrics. All rights reserved. Print ISSN: 1073-0397.
the American Academy of Pediatrics, 345 Park Avenue, Itasca, Illinois, 60143. Copyright © 2003 has been published continuously since 1948. Pediatrics is owned, published, and trademarked by Pediatrics is the official journal of the American Academy of Pediatrics. A monthly publication, it
at Viet Nam:AAP Sponsored on August 30, 2020
www.aappublications.org/news