Self-directed Versus Traditional Classroom Training
for Neonatal Resuscitation
WHAT’S KNOWN ON THIS SUBJECT: The educational efficiency of the neonatal resuscitation course needs to be increased to allow time for simulation and debriefing. Video self-instruction with a personal mannequin has been used to teach adult basic life support.
WHAT THIS STUDY ADDS: Self-directed education successfully shifts the acquisition of cognitive and basic procedural skills outside the classroom, which allows instructors to shorten the course while adding simulation and debriefing activities.
abstract
OBJECTIVE:Neonatal Resuscitation Program instructors spend most of their classroom time giving lectures and demonstrating basic skills. We hypothesized that a self-directed education program could shift acquisition of these skills outside the classroom, shorten the duration of the class, and allow instructors to use their time to facilitate low-fidelity simulation and debriefing.
METHODS:Novice providers were randomly allocated to self-directed ed-ucation or a traditional class. Self-directed participants received a text-book, instructional video, and portable equipment kit and attended a 90-minute simulation session with an instructor. The traditional class included 6 hours of lectures and instructor-directed skill stations. Out-come measures included resuscitation skill (megacode assessment score), content knowledge, participant satisfaction, and self-confidence.
RESULTS:Forty-six subjects completed the study. There was no signif-icant difference between the study groups in either the megacode assessment score (23.8 [traditional] vs 24.5 [self-directed];P⫽.46) or fraction that passed the “megacode” (final skills assessment) (56% [traditional] vs 65% [self-directed];P⫽.76). There were no significant differences in content knowledge, course satisfaction, or postcourse confidence. Content knowledge, years of experience, and self-confidence did not predict resuscitation skill.
CONCLUSIONS:Self-directed education improves the educational effi-ciency of the neonatal resuscitation course by shifting the acquisition of cognitive and basic procedural skills outside of the classroom, which allows the instructor to add low-fidelity simulation and debrief-ing while significantly decreasdebrief-ing the duration of the course. Pediatrics2011;127:713–719
AUTHORS:Gary M. Weiner, MD,a,bKarin Menghini, MSN,
RNC, NNP-BC,aJeanette Zaichkin, MN, RN, NNP-BC,c
Ann E. Caid, BSN, RN,aCarrie J. Jacoby, ADN, RN,aand
Wendy M. Simon, MA, CAEd
aDepartment of Pediatrics, Neonatal Intensive Care, St Joseph Mercy Hospital, Ann Arbor, Michigan;bDepartment of Pediatrics, Neonatal-Perinatal Medicine, Wayne State University School of Medicine, Detroit, Michigan;cNeonatal Outreach Program, Seattle Children’s Hospital, Seattle, Washington; anddDivision of Life Support Programs, American Academy of Pediatrics, Elk Grove Village, Illinois
KEY WORDS
resuscitation, education, newborn
ABBREVIATIONS
NRP—Neonatal Resuscitation Program VSI—video self-instruction
S-NRP—self-directed Neonatal Resuscitation Program C-NRP—classroom Neonatal Resuscitation Program MAS—megacode assessment score
Dr Weiner contributed to the conception, design, data
acquisition, analysis and interpretation of data, and drafting and revision of the manuscript and approved the version to be published; Ms Menghini and Ms Zaichkin contributed to the conception, design, data acquisition, and drafting and revision of the manuscript and approved the version to be published; Ms Caid and Ms Jacoby performed the educational interventions, contributed to data acquisition and revision of the manuscript, and approved the version to be published; and Ms Simon contributed to the conception of the project and revision of the manuscript and approved the version to be published. www.pediatrics.org/cgi/doi/10.1542/peds.2010-2829 doi:10.1542/peds.2010-2829
Accepted for publication Dec 22, 2010
Address correspondence to Gary M. Weiner, MD, Department of Pediatrics, St Joseph Mercy Hospital, 5301 E Huron River Dr, Ann Arbor, MI 48106. E-mail: weinerg@trinity-health.org
PEDIATRICS (ISSN Numbers: Print, 0031-4005; Online, 1098-4275). Copyright © 2011 by the American Academy of Pediatrics
FINANCIAL DISCLOSURE:The American Academy of Pediatrics and Laerdal Medical Corporation provided materials for the completion of this study. Dr Weiner and Ms Zaichkin are consultants for the Neonatal Resuscitation Program Steering Committee and Laerdal Medical Corporation; they receive no compensation for the sale of educational materials. Ms Simon is the director of Life Support Programs at the American Academy of Pediatrics. Ms Menghini, Ms Caid, and Ms Jacoby have indicated they have no financial relationships relevant to this article to disclose.
Resuscitation Program (NRP) is the na-tional standard for teaching neonatal resuscitation.1The provider course
in-cludes a series of lectures, written examinations, practice stations, and a final skills assessment (called the “megacode”).2,3 Although the course
was developed by using adult learning principles, a national survey of NRP in-structors revealed opportunities for improvement.4NRP instructors believe
that lecture is an ineffective teaching method; however, they reported spending the largest percentage of their class time giving lectures and re-viewing textbook material. Most in-structors felt that participants arrived inadequately prepared to learn the technical skills, and few instructors dedicated the majority of time to hands-on training. The focus on pas-sive teaching methodologies may not meet the needs of autonomous, self-directed adult learners.5 The
Interna-tional Liaison Committee on Resuscita-tion recommends that educators use active learning methodologies, and the NRP Steering Committee has advised instructors to use hands-on practice, realistic simulations, and constructive debriefings.6,7 Several barriers may
prevent instructors from adopting these recommendations. Teaching the cognitive components of the course is time-consuming and prevents instruc-tors from introducing additional ac-tivities. Furthermore, students have limited opportunities to practice pro-cedural skills before the course be-cause neonatal resuscitation equip-ment is not generally available outside of the delivery room. The basic instruc-tional design of the course may need to be revised to improve educational effi-ciency and allow instructors time to adopt active methodologies.
Video self-instruction (VSI) has been used to teach basic life support
out-These self-directed programs have compared favorably with traditional classroom courses. They are consis-tent with adult education principles,
because they offer learners flexibility, control over the pace of learning, the ability to repeat portions, and the op-portunity to practice new skills in
private.12 This trial was designed to
evaluate if a self-directed education program in which learners use a text-book, VSI, and a portable equipment kit
could be used to improve the educa-tional efficiency of the NRP course by shifting the acquisition of cognitive and basic procedural skills outside of
the classroom, decrease the total du-ration of the course, and allow instruc-tors to use their time facilitating simu-lations and debriefings.
SUBJECTS AND METHODS
In this randomized controlled trial, we compared a self-directed NRP (S-NRP) course with a full-day classroom (C-NRP) course. Participants were
re-cruited from the postpartum nursing staff at St Joseph Mercy Hospital (Ann Arbor, MI). At the time of the study, nurses working on this unit did not
re-ceive NRP training. Subjects were eligi-ble if they had newborn care responsi-bility but had not participated in an NRP course within the previous 2 years. There were no other exclusion
criteria. Subjects were randomly allo-cated by using a computer-generated table (www.graphad.com/quickcalcs) and assigned a randomly generated
code to mask their identity and alloca-tion from the study personnel who as-sessed outcomes. Two instructors (Ms Caid and Ms Jacoby) taught all courses
in both study groups. The subjects provided written informed consent, and the hospital’s institutional review board approved the study.
S-NRP (Self-directed Education and Simulations)
Subjects in the S-NRP group used the Textbook of Neonatal Resuscitation2
simulation; however, the instructor
limited the session to 90 minutes and required the group to complete each simulation and debriefing at least once.
C-NRP (Traditional Classroom Course)
Subjects who were randomly assigned to the C-NRP group received the text-book 2 weeks before their scheduled course and were advised to read the
relevant chapters. They attended a tra-ditional 6-hour course with lectures and instructor-directed skill stations. The instructor used the standard NRP slide set and speaker notes.3 After
each lecture, participants completed the written knowledge assessments. Subjects then proceeded to a skill sta-tion where they completed the NRP performance checklist by using a
stan-dard neonatal mannequin. Partici-pants worked independently at each skill station and received performance feedback directly from the instructor.
Outcome Measures Primary Outcome Measure
Resuscitation skills were assessed by using the NRP basic megacode3and a
high-fidelity neonatal simulator. Sub-jects received standardized instruc-tions before beginning the megacode. Each subject received the same patient scenario. An assistant who was not otherwise involved in the study partic-ipated in the megacode but was in-structed to perform procedures only if directed by the test subject. The man-nequin provided all necessary visual, tactile, and auditory cues. Each mega-code was video-recorded and subse-quently scored by a single investigator (Ms Zaichkin), blinded to group assign-ment, who used the previously vali-dated megacode assessment score (MAS).13The MAS was modified for use
with the simulator, because subjects do not ask the instructor for the man-nequin’s response. The modified MAS had 14 items; each item was scored
from 0 to 2 (0, not done; 1, done inrectly or out of sequence; 2, done cor-rectly and in sequence). The NRP Steer-ing Committee requires participants to achieve a perfect score on 5 “critical steps” and achieve a minimum MAS of 22 (80%) for successful completion.3
The primary hypothesis was that pro-viders who completed the S-NRP course would achieve a higher mean score on the MAS than those who com-pleted the C-NRP course.
Secondary Outcome Measures
Cognitive skills were assessed by add-ing the scores from the 5 knowledge assessments (maximum: 55 points). At the end of the course, participants completed a course evaluation that in-cluded multiple-choice, Likert-scale, and free-text responses. The re-sponses to the Likert-scale questions were added to create a summary sat-isfaction score (scale: 10 – 46). Two subscores (scale: 3–12) were calcu-lated that reflected (1) the respon-dent’s perception that the course fit his or her learning style and (2) self-confidence in his or her skills at the end of the course.
Statistical Analysis Sample Size
A preliminary estimate of sample size was based on a 12-subject pilot group (n ⫽ 12; mean MAS: 27.2 [SD: 1.4]). Most of the participants in the pilot group had previous NRP experience, and we assumed that MASs in our study would have greater variability (estimated SD: 2). A 2.5-point mean dif-ference was prospectively identified as clinically significant by consensus among the investigators. To detect this difference, 11 subjects would need to be enrolled in each group (2-tailed␣⫽ .05,⫽.80 [estimated SD: 2]).14An
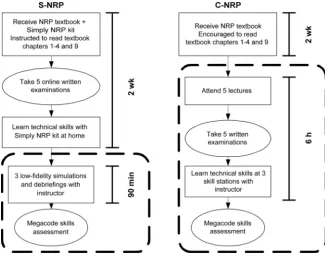
in-terim evaluation after the first 24 sub-jects showed that the SD for the study population was likely to be near 3.0. En-FIGURE 1
Summary of the curriculum for each study group. Components included within the dotted rectangles were completed in a classroom setting with an instructor’s supervision. Solid rectangles represent learning activities, and ovals represent assessments.
Analysis
Continuous data are described as the mean⫾SD. Differences between con-tinuous variable were analyzed by the independent samplettest and are de-scribed as the mean difference rela-tive to the C-NRP group. Differences be-tween categorical variables were analyzed by Fisher’s exact test and are described as the risk ratio relative to the C-NRP group. Multivariate linear regression was used to assess the re-lationship between psychomotor skills (MAS, dependent variable), cognitive skills (knowledge assessment sum-mary score), experience (years), and self-confidence (self-confidence sub-score). All statistical analyses were conducted by using GraphPad InStat 3.0 (GraphPad Software, San Diego, CA). All comparisons were 2-tailed and considered statistically significant ifP was⬍.05.
RESULTS
Forty-eight subjects were enrolled and randomly allocated to the study groups. One subject in each group dropped out before beginning the pro-gram, which left a total of 46 subjects. Few of the participants had ever previ-ously completed an NRP course (Table 1). Most of the subjects were experi-enced nurses with an average of⬎15 years caring for newborns in a post-partum or nursery setting. Fewer than half of them had ever worked in a de-livery room or NICU setting in which they would have been exposed to neo-natal resuscitations. There was no dif-ference between the groups in these measures of previous experience. Sub-jects in the S-NRP group reported spending an average of 2 more hours (P⬍.01) preparing at home for their classroom activity.
There was no difference between study groups in the mean MAS (23.8⫾
3.1 [C-NRP] vs 24.5⫾3.6 [S-NRP]) or in the fraction of participants who passed the megacode (0.56 [C-NRP] vs 0.65 [S-NRP]) (Table 2). Individually, each of the 5 critical steps was per-formed correctly by the majority of participants (range: 0.83–1.0) (Table 3). There was no difference in the frac-tion of participants who correctly per-formed all 5 critical steps (0.65 [C-NRP] vs 0.65 [S-NRP]). Similarly, there was no difference between study groups in the mean knowledge-assessment score (49.8⫾3.1 [C-NRP] vs 51.5⫾3.0 [S-NRP]) (Table 2) or in the fraction of
participants who passed all 5 tests on
their first attempt (0.74 [C-NRP] vs 0.96 [S-NRP]; risk ratio: 1.3 [95% confidence interval: 1.0 –1.7];P⫽.09).
Both groups were satisfied with their course. There was no difference
be-tween groups with respect to their cu-mulative satisfaction score or the sub-score for the learning-style evaluation (Table 2). There was a trend, not quite
significant, that favored the C-NRP group for the subscore that reflected self-confidence in their skills at the conclusion of the course (10.9 ⫾1.2
Experience, y
Mean⫾SD 15.3⫾10.1 15.4⫾10.0
Median (IQR) 12 (8–22) 10 (8–22)
Previous NRP experience,n(%) 4 (17) 6 (26) Previous labor-and-delivery experience,n(%) 9 (39) 10 (43) Previous NICU experience,n(%) 5 (22) 8 (35) Preparation time, mean⫾SD, h 4.0⫾1.5 6.3⫾1.5a
IQR indicates interquartile range.
aP⬍.01.
TABLE 2 Primary and Secondary Outcome measures C-NRP (N⫽23)
S-NRP (N⫽23)
Mean Difference or RR (95% CI)
P
MAS, mean⫾SD (maximum score: 28) 23.8⫾3.1 24.5⫾3.6 0.7 (⫺1.2 to 2.7) .46 Passed megacode,n(%) 13 (56) 15 (65) 1.15 (0.72 to 1.84) .76 Knowledge-assessment score, mean⫾SD
(maximum score: 55)
49.8⫾3.1 51.5⫾4.0 1.7 (⫺0.1 to 3.5) .06
Cumulative satisfaction score, mean⫾SD (maximum score: 46)
42.4⫾4.0 41.4⫾3.9 ⫺1.0 (⫺3.4 to 1.4) .40
Learning-style subscore, mean⫾SD (maximum score: 12)
11.2⫾1.0 10.8⫾1.2 ⫺0.4 (⫺1.0 to 0.3) .30
Self-confidence subscore, mean⫾SD (maximum score: 12)
10.9⫾1.2 10.1⫾1.3 ⫺0.8 (⫺1.5 to 0.0) .05
RR indicates relative risk; CI, confidence interval.
TABLE 3 Participants Correctly Performing 5 “Critical” NRP Steps C-NRP (N⫽23),n(%)
S-NRP (N⫽23),n(%)
RR (95% CI) P
Prepare bag, mask, and oxygen 19 (83) 22 (96) 1.2 (0.9–1.4) .35 Identify need for PPV 21 (91) 23 (100) 1.1 (0.9–1.2) .49 Provide PPV with correct rate and technique 23 (100) 21 (91) 0.9 (0.8–1.0) .49 Take corrective action for ineffective ventilation 23 (100) 20 (87) 0.9 (0.7–1.0) .23 Provide compressions with correct rate and
technique
20 (87) 19 (83) 1.0 (0.7–1.2) .99
Perform all 5 critical steps correctly 15 (65) 15 (65) 1.0 (0.6–1.5) .99 No. of “critical steps” performed correctly
(maximum: 115)
106 (92) 105 (91) 1.0 (0.9–1.1) .99
[C-NRP] vs 10.1⫾1.3 [S-NRP];P⫽.05). All participants responded that they would recommend their course to a colleague. The C-NRP group identified the interactive skill stations as the most valuable component (Table 4). The S-NRP group did not identify a sin-gle most valuable component. Similar fractions of the participants selected the textbook, Simply-NRP kit, and prac-tice simulations.
In multiple regression analysis, the knowledge score, self-confidence sub-score, and years of experience were not predictive of resuscitation skill as measured by the MAS (R2⫽0.073;P⫽
.36). This finding was true when con-sidering all 3 independent variables to-gether and simplified models in which each variable was omitted 1 at a time.
DISCUSSION
The NRP Steering Committee has an-nounced a strategic plan to emphasize active learning by adding simulation and debriefing exercises to the pro-vider course.7To achieve this goal,
in-structors will need to improve their educational efficiency. One strategy would be to shift the acquisition of cog-nitive and basic procedural skills out-side of the classroom. Results of our study confirm that this strategy is suc-cessful. Participants in the S-NRP group compared favorably with those in the C-NRP group on both the psy-chomotor and cognitive assessments, and there was a trend favoring the S-NRP group for both outcome
mea-sures. Although the mean difference between groups for the MAS was insuf-ficient to reject the null hypothesis, the
lower limit of the 95% confidence inter-val is fully contained within the pre-specified range of indifference (2.5 points) and, therefore, supports a con-clusion of noninferiority.15 This is an
important finding, because the proto-col would have been expected to bias the study against the self-directed
method. The subjects were novices with little previous neonatal resuscita-tion experience, and the S-NRP group’s interaction with an instructor was strictly limited to 90 minutes. Outside of the study, instructors would be ex-pected to adjust the duration of their hands-on practice on the basis of the learner’s needs. Less experienced
learners, and those who are learning advanced skills, would likely require more time. The increased efficiency of the self-directed curriculum would al-low instructors the flexibility to allo-cate additional time to hands-on prac-tice without extending the duration of the course. By decreasing the instruc-tor time required to complete an NRP
course, the self-directed program has the potential to yield significant re-source savings. Given that the new method is not inferior, allows the addi-tion of simulaaddi-tion and debriefing, shortens the course, and decreases the instructor’s time commitment, we believe that it is preferable to the tra-ditional curriculum.
Our findings are consistent with those of other studies that have compared self-instruction with traditional class-room training for adult basic life sup-port. In these studies, brief self-instruction with VSI performed as well or better than a traditional classroom course.8–10,16–19It is important to note
that self-instruction was effective only if hands-on practice with a personal mannequin was incorporated with VSI. Simply watching videotape without hands-on practice was not found to be effective.20,21The materials included in
the Simply-NRP kit allow synchronous hands-on practice with the instructor and alleviate the equipment barrier that has previously limited opportuni-ties to practice NRP skills outside of the classroom.
Poor skill retention is a consistent problem for resuscitation programs.22
Currently, the NRP requires providers to repeat the course every 2 years; however, investigators have shown that resuscitation knowledge and skills deteriorate within 3 to 8 months.23,24 Previous investigators
have shown that adults trained with a single exposure to VSI experience a similar decline in skills compared with those trained in the classroom.18,19
Al-though our study was not designed to assess skill retention, providers could potentially use the self-directed pro-gram to refresh their skills between NRP courses without additional ex-pense or increasing the demand on instructors.
We anticipated that adult learners would prefer the flexibility of the self-directed curriculum.5,25Participants in
both groups indicated a high level of satisfaction; however, there was a trend for subjects in the C-NRP group to report greater self-confidence in their skills. Early in an educational ex-perience, learners may adopt a more dependent, passive learning style and feel more comfortable in a controlled, TABLE 4 Most and Least Useful Components of the NRP Course
Most Useful,n(%) Least Useful,n(%)
C-NRP (N⫽20)
S-NRP (N⫽22)
C-NRP (N⫽18)
S-NRP (N⫽19)
Textbook 2 (10) 8 (36) 5 (28) 2 (10)
Textbook DVD 0 (0) 2 (9) 13 (72) 13 (68)
Lectures 0 (0) NA 0 (0) NA
Simply-NRP kit NA 5 (23) NA 4 (21)
Skill stations or simulations 15 (75) 6 (27) 0 (0) 0 (0)
Megacode 3 (15) 1 (4) 0 (0) 0 (0)
Sample size varied on the basis of the number of subjects who responded to each question. NA indicates not applicable.
felt less prepared by the self-directed program because they had less inter-action with the instructor. The in-creased self-confidence expressed by those in the traditional C-NRP group did not, however, translate into im-proved performance. This finding is consistent with those from previous investigators who have found little cor-relation between self-perceived confi-dence,16,24,26–28 cognitive scores,24,28,29
and objective measures of resuscita-tion skills.
Strengths of our study include the randomized design, standardized out-come measures, and masked assess-ment of skills with a high-fidelity simu-lator. Limitations include the small sample size, homogeneity of the study population, and measurement of the primary outcome in a simulator rather
taking the basic NRP course. The Simply-NRP kit does not review ad-vanced technical skills such as intuba-tion, laryngeal mask placement, or emergency intravascular access. Addi-tional studies are required to evaluate the role of self-directed education among experienced providers and those taking the advanced NRP course. Finally, resuscitation skills were mea-sured in both groups by using a high-fidelity simulator. Although evaluation during an actual resuscitation would have been ideal, there is evidence sup-porting the correlation between per-formance during simulation and ac-tual clinical practice.30
Although these data indicate that nov-ice participants can acquire cognitive and basic procedural skills by using the self-directed curriculum, they
We believe that the interpersonal inter-action between instructor and learner remains a critical component of the NRP course. Ideally, the improved effi-ciency of the self-directed curriculum will allow instructors to use their time more constructively.
CONCLUSIONS
A self-directed education program us-ing the NRP textbook, online knowledge assessment, and VSI with a portable equipment kit can successfully im-prove the educational efficiency of the neonatal resuscitation course by shift-ing the acquisition of cognitive and ba-sic procedural skills outside of the classroom, which allows the instruc-tor to add low-fidelity simulation and debriefing activities while significantly decreasing the duration of the course.
REFERENCES
1. Halamek LP. Educational perspectives: the genesis, adaptation, and evolution of the Neonatal Resuscitation Program. Neor-eviews. 2008;9(4):e142– e149
2. Kattwinkel J, ed.Textbook of Neonatal Re-suscitation. 5th ed. Elk Grove Village, IL/ Dallas, TX: American Heart Association/ American Academy of Pediatrics; 2006 3. Zaichkin J, ed.Instructor’s Manual for
Neo-natal Resuscitation. 5th ed. Elk Grove Vil-l a g e , I L / D a Vil-l Vil-l a s , T X : A m e r i c a n H e a r t A s s o c i a t i o n / A m e r i c a n A c a d e m y o f Pediatrics; 2006
4. Weiner GM. NRP 2007: what it is and isn’t, what works and doesn’t. Presented at: American Academy of Pediatrics National Conference and Exhibition; October 26, 2007; San Francisco, CA. Available at: www. aap.org/nrp/pdf/NRPToday.pdf. Accessed February 2, 2011
5. Knowles MS, Holton EF, Swanson RA.The Adult Learner: The Definitive Classic in Adult Education and Human Resource Develop-ment. 6th ed. Burlington, MA: Elsevier; 2005 6. Chamberlain DA, Hazinski MF. Education in resuscitation. Resuscitation. 2003; 59(1):11– 43
7. Zaichkin J, McGowan JE. The “new” NRP instructor: 2011 and beyond. Available at: w w w . c p s . c a / E n g l i s h / P r o E d u / N R P /
FallWinter2008.pdf. Accessed February 2, 2011
8. Todd KH, Braslow A, Brennan RT, et al. Ran-domized, controlled trial of video self-instruction versus traditional CPR training.
Ann Emerg Med. 1998;31(3):364 –369 9. Todd KH, Heron SL, Thompson M, Dennis R,
O’Connor J, Kellermann AL. Simple CPR: a randomized, controlled trial of video self-instructional cardiopulmonary resuscita-tion training in an African American church congregation.Ann Emerg Med. 1999;34(6): 730 –737
10. Bjørshol CA, Lindner TW, Soreide E, Moen L, Sunde K. Hospital employees improve basic life support skills and confidence with a personal resuscitation manikin and a 24-min video instruction.Resuscitation. 2009; 80(8):898 –902
11. Lynch B, Einspruch EL, Nichol G, Becker LB, Aufderheide TP, Idris A. Effectiveness of a 30-min CPR self-instruction program for lay responders: a controlled randomized study.
Resuscitation. 2005;67(1):31– 43
12. Grow GO. Teaching learners to be self-directed.Adult Educ Q. 1991;41(3):124 –149 13. Lockyer J, Singhal N, Fidler H, Weiner G, Aziz
K, Curran V. The development and testing of a performance checklist to assess neonatal resuscitation megacode skill.Pediatrics.
2006;118(6). Available at: www.pediatrics. org/cgi/content/full/118/6/e1739 14. Dupont WD, Plummer WD Jr. Power and
sample size calculations: a review and com-puter program.Control Clin Trials. 1990; 11(2):116 –128
15. Motulsky H.Intuitive Biostatistics: A Non-mathematical Guide to Statistical Thinking.
2nd ed. New York, NY: Oxford University Press; 2010
16. Braslow A, Brennan RT, Newman MM, Bircher NG, Batcheller AM, Kaye W. CPR training without an instructor: development and evaluation of a video self-instructional system for effective performance of cardio-pulmonary resuscitation. Resuscitation. 1997;34(3):207–220
17. Batcheller AM, Brennan RT, Braslow A, Urru-tia A, Kaye W. Cardiopulmonary resuscita-tion performance of subjects over forty is better following half-hour video self-instruction compared to traditional four-hour classroom training.Resuscitation. 2000;43(2):101–110
19. Isbye DL, Rasmussen LS, Lippert FK, Rudolph SF, Ringsted CV. Laypersons may learn ba-sic life support in 24min using a personal resuscitation manikin.Resuscitation. 2006; 69(3):435– 442
20. Clark LJ, Watson J, Cobbe SM, Reeve W, Swann IJ, Macfarlane PW. CPR ’98: a practical multi-media computer-based guide to cardiopulmo-nary resuscitation for medical students. Re-suscitation. 2000;44(2):109 –117
21. Monsieurs KG, Vogels C, Bossaert LL, et al. Learning effect of a novel interactive basic life support CD: the JUST system. Resuscita-tion. 2004;62(2):159 –165
22. Smith KK, Gilcreast D, Pierce K. Evaluation of staff’s retention of ACLS and BLS skills. Re-suscitation. 2008;78(1):59 – 65
23. Kaczorowski J, Levitt C, Hammond M, et al. Retention of neonatal resuscitation skills and knowledge: a randomized controlled trial.Fam Med. 1998;30(10):705–711 24. Curran VR, Aziz K, O’Young S, Bessell C.
Eval-uation of the effect of a computerized train-ing simulator (ANAKIN) on the retention of neonatal resuscitation skills.Teach Learn Med. 2004;16(2):157–164
25. Moore MG.Handbook of Distance Education.
2nd ed. Mahwah, NJ: Erlbaum Associates; 2007 26. Castle N, Garton H, Kenward G. Confidence vs competence: basic life support skills of health professionals. Br J Nurs. 2007; 16(11):664 – 666
27. Marteau TM, Wynne G, Kaye W, Evans TR. Resuscitation: experience without feedback
increases confidence but not skill. BMJ. 1990;300(6728):849 – 850
28. White JR, Shugerman R, Brownlee C, Quan L. Performance of advanced resuscitation skills by pediatric housestaff.Arch Pedi-atr Adolesc Med. 1998;152(12):1232–1235 29. Rodgers DL, Bhanji F, McKee BR. Written evaluation is not a predictor for skills per-formance in an Advanced Cardiovascular Life Support course.Resuscitation. 2010; 81(4):453– 456
30. Gordon JA, Alexander EK, Lockley SW, et al. Does simulator-based clinical performance correlate with actual hospital behavior? The effect of extended work hours on patient care provided by medical interns. Acad Med. 2010;85(10):1583–1588
THE BIRTHPLACE OF WINE MAKING:When I go to the store to purchase wine for dinner, the choices seem almost endless. There are varieties from Europe, North and South America, Australia, New Zealand, and South Africa. It seems as if almost everyone is in the wine making business these days. If wine making and consumption is so ubiquitous, where did it get its start? While many French wine enthusiasts claim that wine production originated in Western Europe, new evi-dence suggests that the true origin may lie quite a bit farther to the east. As reported on CNN (Brian Walker, January 12, 2011) researchers have discovered evidence of wine production in a cave system in southern Armenia close to the border with Iran dating back 6000 years. The pots, vats, and press all suggest an organized effort to press and distill grapes during the copper age. Previously, the oldest known winery was thought to have been in Israel and dated from 1650 BC. The copper age wine makers used a foot-stomping system to make their wine similar to that used by people throughout the region well into the 19th century. Analysis of the residue in the pots suggests that the wine makers of the age used the same grape variety, Vitis vinifera, used to produce the vast major-ity of wine today. What the wine would have tasted like is speculative, although some have hypothesized that it would resemble unfiltered merlot. As the cave was part of an important cemetery site, the wine was probably more for cere-monial purposes than general everyday imbibing. Still, the ability to make wine, more complex than making beer, suggests a high degree of horticultural skill and may have paved the way for trade and exchange of agricultural ideas. It seems likely that wine making spread widely from this region. While I still cannot find wines from Armenia in the store, the next time I have guests and we drink wine, I will raise a toast to those ancient wine makers who began the process.
Noted by WVR, MD
DOI: 10.1542/peds.2010-2829 originally published online March 7, 2011;
2011;127;713
Pediatrics
and Wendy M. Simon
Services
Updated Information &
http://pediatrics.aappublications.org/content/127/4/713
including high resolution figures, can be found at:
References
http://pediatrics.aappublications.org/content/127/4/713#BIBL
This article cites 22 articles, 2 of which you can access for free at:
Subspecialty Collections
http://www.aappublications.org/cgi/collection/neonatology_sub Neonatology
sub
http://www.aappublications.org/cgi/collection/fetus:newborn_infant_ Fetus/Newborn Infant
following collection(s):
This article, along with others on similar topics, appears in the
Permissions & Licensing
http://www.aappublications.org/site/misc/Permissions.xhtml
in its entirety can be found online at:
Information about reproducing this article in parts (figures, tables) or
Reprints
http://www.aappublications.org/site/misc/reprints.xhtml
DOI: 10.1542/peds.2010-2829 originally published online March 7, 2011;
2011;127;713
Pediatrics
and Wendy M. Simon
Gary M. Weiner, Karin Menghini, Jeanette Zaichkin, Ann E. Caid, Carrie J. Jacoby
Self-directed Versus Traditional Classroom Training for Neonatal Resuscitation
http://pediatrics.aappublications.org/content/127/4/713
located on the World Wide Web at:
The online version of this article, along with updated information and services, is
by the American Academy of Pediatrics. All rights reserved. Print ISSN: 1073-0397.