National Hospitalization Impact of Pediatric All-Terrain Vehicle Injuries
Jeffrey B. Killingsworth, MPH; John M. Tilford, PhD; James G. Parker, MS; James J. Graham, MD; Rhonda M. Dick, MD; and Mary E. Aitken, MD, MPH
ABSTRACT. Objective. All-terrain vehicle (ATV) in-juries among children represent a significant and grow-ing problem. Although state-level analyses have charac-terized some aspects of pediatric ATV-related injuries, little information on the national impact on hospitaliza-tion is available. This study was designed to characterize more fully the patterns of injury, hospital length of stay, and hospital charges associated with ATV-related inju-ries, with a nationally representative sample.
Methods. Analyses were based on the 1997 and 2000 Healthcare Cost and Utilization Project Kids’ Inpatient Database (KID). The KID is the only national, all-payer database of hospital discharges for children. KID data were weighted to represent all discharges from general hospitals in the United States. Discharges with external cause-of-injury codes consistent with off-road ATV-re-lated injuries were selected, and the affected population was described. Nationally representative rates of ATV-related injuries were calculated, and changes between 1997 and 2000 were documented.
Results. An estimated 5292 children were hospital-ized because of ATV-related injuries during the 2-year period, and hospitalizations increased 79.1% between 1997 and 2000. Rates of ATV-related hospitalization were highest among adolescent white male subjects, consis-tent with previous studies. Most patients had hospital lengths of stay of<4 days (68%), but 10% had stays of>8 days. Injury severity varied considerably, with more than one third of patients sustaining moderate to severe inju-ries. Approximately 1% of hospitalizations resulted in in-hospital deaths. Total hospital charges for this injury mechanism were $74 367 677 for the 2-year study period. Most of these charges were paid by private insurers.
Conclusions. This study provides evidence support-ing recent substantial increases in childhood ATV-re-lated injuries. The hospitalization impact of ATV-reATV-re-lated injuries among children is considerable. Our data sup-port the need for ongoing creative attempts to identify effective strategies to decrease ATV injuries among children. Pediatrics 2005;115:e316–e321. URL: www. pediatrics.org/cgi/doi/10.1542/peds.2004-1585; pediatrics, injury, all-terrain vehicle.
ABBREVIATIONS. ISS, injury severity score; ATV, all-terrain ve-hicle; CPSC, Consumer Product Safety Commission; KID, Kids’
Inpatient Database; ICD-9-CM,International Classification of Dis-eases, Ninth Revision, Clinical Modification; E-code, external cause-of-injury code.
P
ediatric all-terrain vehicle (ATV)-related inju-ries represent a significant and growing prob-lem. ATVs have been sold in the United States since 1972 and have experienced a popularity surge in recent years.1Accompanying this increase in pop-ularity is concern regarding the associated risks for children who ride on or drive ATVs. Current discus-sions have centered on appropriate vehicle sizes for children and the potential for legislative and educa-tional measures to decrease the ATV injury burden. ATVs are 3- or 4-wheeled machines designed with motorcycle-style handlebars, a high center of gravity, and large, low-pressure tires intended for off-road use. ATVs typically range in engine size from 50 cm3 to⬎500 cm3of displacement and can weigh as much as 600 pounds. Nearly all ATVs are designed for 1 rider, because precise, quickly executed, weight-dis-tribution adjustments must be performed to main-tain balance and control of the vehicle in turns or in rough-terrain situations.ATVs have proved useful for a wide range of occupational and recreational purposes but are also associated with significant risks for fatalities and injuries. In 1986, emergency departments admitted an estimated 106 000 patients with ATV-related inju-ries, representing a 230% increase from 1983 esti-mates. In addition, there was an 18% increase in estimated ATV-related deaths from 1985 to 1986.2
Recognizing the growing problem of ATV-related injuries, public health organizations have attempted to prevent injuries through policy recommendations. The US Consumer Product Safety Commission (CPSC) developed a consent decree with ATV man-ufacturers and distributors, which began in 1988. The decree banned the sale of new 3-wheeled ATVs, es-tablished a nationwide ATV training program, im-proved warning materials such as labels to inform the public about the hazards associated with ATV use, and required age recommendations based on the size of the ATV. Specifically, ATVs with engines of ⬎90 cm3 were not recommended for children ⬍16 years of age.3In addition, the American Academy of Pediatrics issued a policy statement discouraging ATV use for children ⬍16 years of age4 and pro-duced a model ATV safety bill that prohibits children ⬍16 years of age from operating ATVs, mandates license, insurance, and registration requirements for all ATV operators, and bans operation of ATVs on From the Department of Pediatrics, University of Arkansas for Medical
Sciences College of Medicine and Arkansas Children’s Hospital, Little Rock, Arkansas.
Accepted for publication Oct 6, 2004. doi:10.1542/peds.2004-1585 No conflict of interest declared.
Reprint requests to (M.E.A.) Department of Pediatrics, Arkansas Children’s Hospital, 800 Marshall St, Slot 512-26, Little Rock, AR 72202-3591. E-mail: aitkenmarye@uams.edu
public roads or with passengers. The bill also en-dorses the use of motorcycle-style helmets, eye protection, and safety clothing, as well as vehicle modifications including seatbelts, roll bars, and automatic headlights.4,5
Despite these efforts, the numbers of pediatric in-juries continue to increase.6–9 The CPSC conducted ATV injury and exposure studies and reported that overall exposure to ATVs increased by 36% (number of drivers) to 50% (number of driving hours) from 1997 to 2001.10The same report showed a dispropor-tionate increase of 104% in ATV-related injuries. The risk of death for children in these studies was 4.5 to 12 times greater than that for adult comparison groups.11,12
Because of this increasing problem, effective meth-ods to prevent ATV-related injuries, particularly among children, are needed. Recent literature has described the benefits of helmet requirements and safety legislation.1,4,6,12–15 The CPSC continues to have an active interest in this problem and held a public hearing in June 2003,16 during which ATV owners and dealers, state legislators, CPSC officials, doctors, researchers, and injury patients and their families discussed ATV injury prevention.
Additional information about the extent and char-acter of ATV-related injuries could inform the debate about these vehicles and might strengthen the efforts of those working to prevent injuries through educa-tion or other activities. This study was designed to determine the impact of ATV-related injuries on the hospital care of children and adolescents. National data were used to assess the numbers of children and adolescents admitted to US hospitals for treatment of ATV-related injuries in 1997 and 2000. Additional analyses determined the distributions of hospitaliza-tions across gender, ethnicity, income, and age cate-gories and the severity of the injuries sustained.
METHODS Study Design and Data
This study was a retrospective analysis of 1997 and 2000 hos-pitalizations based on the Kids’ Inpatient Database (KID).17,18The
KID is a pediatric hospital discharge database developed by the Agency for Healthcare Research and Quality as part of the Health-care Cost and Utilization Project. Data from 22 states in 1997 and 27 states in 2000 are included in the database. A 10% sample of normal newborn discharges and an 80% sample of all other pedi-atric discharges from each US community hospital (short-term, nonfederal, general and specialty hospitals) located in the partic-ipating states are included in the KID.19
The KID is designed to permit the analysis of a broad range of pediatric conditions, such as hospitalizations for treatment of spe-cific injury mechanisms. Information on patient demographic fac-tors, hospital characteristics, diagnosis and procedure codes, and injury severity is included for each hospitalization. Stratification weights are included, which allow the generation of population-based national estimates. This study used the strengths of the KID to develop a national sample of ATV-related hospitalizations.
Childrenⱕ18 years of age with anInternational Classification of Diseases, Ninth Revision, Clinical Modification(ICD-9-CM) external cause-of-injury code (E-code) for an off-road motor vehicle acci-dent were selected for analysis.20The 821 category is described in
the ICD-9-CM codebook as a “nontraffic accident involving other off-road motor vehicles.”20This category specifically excludes
off-road vehicle accidents that occur on public highways. E-codes used in this study for case selection included 821.0, 821.1, 821.8, and 821.9, corresponding to injuries of the driver, a passenger, or
another person injured in an off-road motor vehicle accident. We excluded codes 821.3 through 821.7, because these refer specifi-cally to passengers, occupants, or riders of motorcycles, streetcars, animals, or pedal cycles, as well as pedestrians.
Modifications were made to the dataset to address coding inconsistencies. A small number of records were coded for both an off-road motor vehicle accident and an in-hospital birth, and these cases (n⫽8) were excluded from analysis. The KID is based on hospitalizations and does not use unique identifiers that would enable tracking of individuals over several hospitalizations. To avoid overestimating the ATV-related injury incidence because of double-counting, hospitalizations (n⫽44) that resulted in transfer to another short-term hospital were excluded from analysis.21
Short-term hospital transfers were retained for analysis of charges.
Statistical Analyses
We analyzed ATV-related hospitalizations according to patient demographic variables including age, gender, race, median house-hold income according to zip code, and expected primary payer. Hospital characteristics, including hospital region, hospital type, and hospital bed size, were also considered in our analysis. KID variables used to examine the severity of injury included length of stay, patient disposition at discharge, and total hospital charges. In addition, ICDMAP-90 software was used to calculate injury sever-ity scores (ISSs).22,23
National estimates were calculated with a stratified sampling design and were generated with Stata statistical analysis soft-ware.19,24,25Because a sample size of 70 is required for national
estimates, small categories were combined to produce cells large enough for inclusion in weighted analyses.
RESULTS
The unweighted datasets contained a combined total of 2373 ATV-related hospitalizations for chil-drenⱕ18 years of age across both study years, 1997 and 2000. After weighting, this yielded a national estimate of 5292 cases, with 1896 (SE: 136) hospital-izations in 1997 and 3396 (SE: 147) hospitalhospital-izations in 2000, representing a 79.1% increase from 1997 to 2000.
We calculated the percentages of ATV-related hos-pitalizations that resulted in an in-hospital death for both years. The numbers of deaths for 1997 and 2000 were too small to be used in national estimates of in-hospital mortality rates; therefore, the percent died category is based on unweighted data. The per-cent died results were equal for the 2 years, repre-senting 0.9% of hospitalizations.
Table 1 provides patient demographic characteris-tics. The proportion of hospitalizations experienced by the youngest age category (0 –9 years) decreased from 23.6% to 17.5% between 1997 and 2000, with a corresponding increase in the oldest age category (15–18 years) from 31.6% to 37.7%. Children 10 to 14 years of age experienced ⬃45% of hospitalizations for both years. The proportions of hospitalizations experienced by male and female subjects remained stable over time, at 78% and 22%, respectively. Whites experienced ⬎60% of hospitalizations; how-ever, additional analyses of race were not performed, because race data were missing in⬃25% of cases.
100 000 population in 1997 to 7.41 cases per 100 000 population in 2000. A 103% increase was observed among children 15 to 18 years of age (from 3.91 cases per 100 000 population to 7.95 cases per 100 000 pop-ulation). Male hospitalization rates increased 74%, from 3.91 cases per 100 000 population to 6.81 cases per 100 000 population; female rates increased 63%, from 1.20 cases per 100 000 population to 1.95 cases per 100 000 population.
The distribution of patient income categories changed considerably from 1997 to 2000. The low-income category ($0 –35 000) represented 73.0% of ATV hospitalizations in 1997 but only 46.2% of hos-pitalizations in 2000. A corresponding increase was observed for the high-income category (⬎$35 000), which represented 19.1% of hospitalizations in 1997 and 52.8% in 2000.
The proportions of hospitalizations covered by public insurance, including Medicaid and Medicare, remained relatively equivalent during the study pe-riod, ie, ⬃16% in both 1997 and 2000. The private insurance category, including health maintenance or-ganizations, represented a large majority of hospital-izations for both years, increasing from 70.1% in 1997 to 73.5% in 2000. The third insurance category con-tains all other KID expected-payer designations, in-cluding self-pay, no charge, and other. This category decreased from 12.8% of hospitalizations in 1997 to 10.0% in 2000.
Table 2 provides characteristics of the hospitaliza-tions of children with ATV-related injuries. The length of stay remained relatively stable from 1997 to 2000. Approximately 70% of hospitalizations for both years resulted in a length of stay of 0 to 3 days. TABLE 1. Demographic Characteristics for Children and Adolescents Hospitalized for Treatment
of ATV-Related Injuries
Characteristic 1997 2000
No. SE %* Rate† No. SE %* Rate†
Total hospitalizations 1896 136 100 2.59 3396 147 100 4.45
Age
0–9 y 447 98 23.6 1.15 593 38 17.5 1.49
10–14 y 850 50 44.8 4.45 1521 90 44.8 7.41
15–18 y 599 35 31.6 3.91 1280 58 37.7 7.95
Gender
Male 1469 83 77.5 3.91 2664 123 78.4 6.81
Female 427 68 22.5 1.20 727 36 21.4 1.95
Race
White 1183 76 62.4 2291 122 67.5
Not white 173 22 9.1 264 21 7.8
Median income
$0–35 000 1384 116 73.0 1538 81 45.3
More than $35 000 363 32 19.1 1793 92 52.8
Insurance status
Public 309 32 16.3 538 33 15.8
Private 1329 92 70.1 2496 131 73.5
Other 242 29 12.8 341 21 10.0
* May not equal 100% because of missing data.
† Rates are expressed per 100 000 children 0 to 18 years of age in each of the strata.
TABLE 2. Injury Severity for Children and Adolescents Hospitalized for Treatment of ATV-Related Injuries
Characteristic 1997 2000
No. or Mean SE %* No. or Mean SE %*
Total hospitalizations 1896 136 100 3396 147 100
Length of stay
0–3 d 1291 104 68.1 2302 97 67.8
4–7 d 405 32 21.4 764 49 22.5
ⱖ8 d 199 19 10.5 328 29 9.7
Disposition
Routine 1772 129 93.5 3146 142 92.6
Other 120 16 6.3 249 28 7.3
ISS
0–8 1189 108 62.7 1999 90 58.9
9–16 528 39 27.8 981 60 28.9
17–75 173 18 9.1 406 31 12.0
Hospital charges (by insurance status),† $
Public 5 078 482 589 697 19.8 8 461 127 633 399 17.4
Private 18 065 457 1 135 532 70.4 36 354 816 2 437 718 74.7
Other 2 341 486 259 089 9.1 3 489 026 376 657 7.2
Total hospital charges,† $ 25 669 637 1 505 100 48 698 040 2 775 839
Mean ISS 7.50 0.42 8.29 0.20
Mean hospital charges, $ 13 336 654 13 823 430
Approximately 20% of hospitalizations involved a length of stay of 4 to 7 days, and the remaining 10% had a length of stay of ⬎7 days. Most hospitaliza-tions (4918 patients; 93.5%) resulted in routine dis-charge to home. The remaining 6.3% of patients died in the hospital, were discharged against medical ad-vice, or were transferred to a skilled-nursing facility, intermediate-care facility, or home health care.
The proportion of mild injuries (ISS values of 0 – 8) decreased slightly from 1997 to 2000, ie, from 62.7% to 58.9% of ATV-related hospitalizations. The pro-portions of moderate injuries (ISS values of 9 –16) remained approximately equal, at 28% of ATV-re-lated hospitalizations, for the 2 years. The most se-vere injury category (ISS values of ⬎16) increased from 9.1% of ATV-related hospitalizations in 1997 to 12.0% of hospitalizations in 2000. In addition to ex-amination of ISS values according to category, KID weight variables were used to create a national esti-mate of the mean ISS values for the 2 years. The estimated ISS mean increased slightly, from 7.50 (SE: 0.42) in 1997 to 8.29 (SE: 0.20) in 2000.
Hospital charges were calculated from a dataset that included transfers to a short-term hospital. KID weight variables were used to create a national esti-mate of charges for the 2 years. The mean charge per hospitalization remained stable across the years, with charges of $13 336 (SE: $654) in 1997 and $13 823 (SE: $430) in 2000. Estimated total charges associated with these hospitalizations were more than $70 mil-lion for the 2 years studied. The proportions of charges according to insurance type were largely unchanged from 1997 to 2000, with⬃70% and 20% of charges being paid by private insurance and public insurance, respectively.
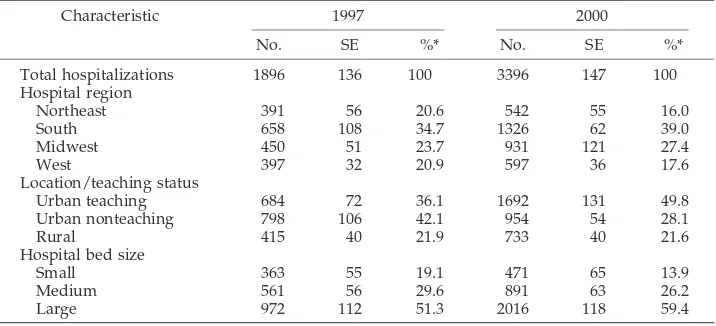
Table 3 provides hospital characteristics for ATV-related hospitalizations. The Northeast and West re-gions showed small decreases in hospitalizations from 1997 to 2000, and the South and Midwest re-gions showed corresponding increases. Overall, the South had the highest percentage of hospitalizations (39%) in 2000, followed by the Midwest (27.4%). ATV-related hospitalizations are much less frequent in the West and Northeast (⬍20%).
Hospital location (urban versus rural) and
teach-ing status are recorded in the KID. Rural hospitals received relatively equal percentages of hospitaliza-tions (⬃21%) in 1997 and 2000. The representation of urban nonteaching hospitals decreased considerably, from 42.1% of hospitalizations in 1997 to 28.1% of hospitalizations in 2000. A corresponding increase was seen in the representation of urban teaching hospitals, from 36.1% in 1997 to 49.8% in 2000.
Hospital size (measured as the number of avail-able beds) is described in the KID as small, medium, or large. Small and medium-sized hospitals had de-creased representation of ATV-related hospitaliza-tions from 1997 to 2000, whereas that of larger hos-pitals increased from 51.3% to 59.4%.
DISCUSSION
The CPSC 1997 and 2001 ATV injury studies, with a random-digit-dialing survey design, have pro-vided the most comprehensive, nationally represen-tative data demonstrating the recent increase in ATV-related injuries among children. Those studies were limited to the reports of survey respondents and lacked clinically important information about the nature of the injuries sustained. Our study ex-tends those findings by using a large, nationally representative, pediatric discharge database. Results provide evidence supporting the increasing number of ATV-related injuries experienced by children. The study period is significant; the study used KID data collected in the years surrounding the end of the initial CPSC 10-year consent decree in 1998, which allows us to substantiate the subsequent increase in ATV-related injuries suggested in the CPSC injury reports.
Use of the KID data enabled a more detailed look at the hospital impact of ATV-related injuries at a national level than had been possible previously. The estimated number of ATV-related hospitalizations in our sample increased nearly 80%, to⬎3300 hospital-izations in 2000, which was even more dramatic than the CPSC report of a 56.5% increase in emergency department-treated injuries during the same time period. This larger change in admissions may reflect increasing severity of injuries, necessitating
hospital-TABLE 3. Characteristics of Hospitals Treating Children and Adolescents for ATV-Related Inju-ries
Characteristic 1997 2000
No. SE %* No. SE %*
Total hospitalizations 1896 136 100 3396 147 100
Hospital region
Northeast 391 56 20.6 542 55 16.0
South 658 108 34.7 1326 62 39.0
Midwest 450 51 23.7 931 121 27.4
West 397 32 20.9 597 36 17.6
Location/teaching status
Urban teaching 684 72 36.1 1692 131 49.8
Urban nonteaching 798 106 42.1 954 54 28.1
Rural 415 40 21.9 733 40 21.6
Hospital bed size
Small 363 55 19.1 471 65 13.9
Medium 561 56 29.6 891 63 26.2
Large 972 112 51.3 2016 118 59.4
ization, or other factors not accounted for in the available data.
Estimated gender and race characteristics were similar to those in previous studies, with a large proportion of ATV-related injuries being experi-enced by white male subjects.7,10,12,14,27–30 Despite warnings from manufacturers and policy statements from medical groups regarding the use of ATVs by children, most of these pediatric injuries occurred among younger children; two thirds of the children wereⱕ14 years of age, and approximately one fifth were⬍9 years of age. This underscores the need to intensify efforts to educate parents about ATV risks for children and to identify new strategies that might prevent inappropriate ATV use among young chil-dren.
The proportion of ATV-related hospitalizations as-sociated with a median income of more than $35 000 increased substantially between 1997 and 2000, from 19.1% to 52.8%. In the full KID, this category repre-sented 45.2% of hospitalizations in 1997 and 59.9% of hospitalizations in 2000. The reasons behind this shift to a greater proportion of higher-income hospitaliza-tions are not clear but may reflect, in part, the in-creasing costs associated with purchase of larger, more powerful ATVs over time. The CPSC docu-mented a 202.7% increase in larger ATVs, with en-gine sizes of ⱖ400 cm3, during the same time peri-od.10
We were able to identify 3 other studies in which injury severity was formally assessed with the ISS, all based on data from trauma referral centers in single states. Our severity findings were similar to those found in Ohio when ATV riders were compared with bicyclists.12 Reports with smaller samples from trauma centers in Georgia and Pennsylvania demon-strated mean ISS values of 13 for childrenⱕ16 years of age.7,8Our national data, by comparison, demon-strated mean scores of 7.50 in 1997 and 8.29 in 2000, representing injuries treated in general as well as in trauma referral centers. Although more than one half of ATV-related injuries in our study were associated with ISS values of⬍9, it is notable that many of the patients (⬎10%) sustained very severe injuries, with scores of⬎16 and correspondingly prolonged hospi-tal stays of ⬎1 week in many cases. Although few deaths were reported in our study, these hospitaliza-tions represent substantial injuries. We were unable to characterize the long-term morbidity associated with these injuries using data available in the KID.
The mean charges reported here (more than $13 000 per hospitalization) were substantially higher than those noted in a Utah study ($4240 per hospitalization) in the early 1990s.6The total charges associated with the hospitalizations over 2 years ex-ceeded $70 million, demonstrating an expensive, avoidable, public health problem. The bulk of these hospital expenses were borne by private insurers.
For several reasons, we think that the total cost of ATV-related injuries is underestimated in this study. Physician charges are not included in the KID; there-fore, charge estimates described in this study under-estimate the cost of ATV-related hospitalizations. In addition, we have no follow-up data to characterize
the long-term health care needs of the affected pa-tients. Finally, the KID does not include ATV-related injuries treated in outpatient or emergency depart-ment settings.
The burden of ATV-related injuries is unevenly distributed throughout the country, with injuries be-ing most common in the South and Midwest regions of the country, consistent with previous usage re-ports.27,31 Our results also indicate a shift to hospi-talization in larger, urban, teaching hospitals from 1997 to 2000. Rural hospitals maintained ⬃21% of ATV-related hospitalizations for the 2 years. The no-table change in location/teaching status from 1997 to 2000 was the shift from urban nonteaching hospitals to urban teaching hospitals.
Several limitations should be acknowledged. The use of ICD-9-CM E-codes as selection criteria ex-cluded injuries that occurred on paved roads. ATV crashes occurring on paved roads have been associ-ated with more severe injuries.9,11,31,32Therefore, we think that our findings underestimate both the num-ber and the severity of ATV-related injuries. How-ever, because ATVs are not designed for use on paved roads, this analysis provides an opportunity to describe a population using ATVs in the setting for which they were designed. We attempted, through careful selection of the E-codes, to include only ATV-related hospitalizations in our data. It is possible that some cases of other off-road vehicles might have been included in our results, although the consistency of our data with previously pub-lished ATV injury studies suggests that the degree of misclassification was small.
Data from the KID are currently available only for the years 1997 and 2000, preventing a more detailed analysis of ATV-related hospitalizations over time. The anticipated release of KID data for 2003 will enhance our ability to describe hospitalization trends.
Some concerns might be raised that the increase in ATV-related hospitalizations found in the KID might be an artifact of its design. However, previous stud-ies demonstrated stable KID hospitalization esti-mates for conditions for which no increase should be expected.33,34
CONCLUSIONS
This study provides additional evidence support-ing recent substantial increases in the number of ATV-related injuries among children. The hospital-ization impact of ATV-related injuries among chil-dren is considerable. Our data support the need for ongoing creative attempts to identify effective strat-egies to decrease ATV injuries among children.
ACKNOWLEDGMENTS
This work was supported by grants from the Health Resources and Services Administration, Maternal and Child Health Bureau (grant 1H33 MC 00088 01), and by the Robert Wood Johnson Foundation (Injury Free Coalition for Kids grant 047012).
We thank James M. Robbins, PhD, for helpful review of an earlier version of this manuscript and Suzanne Speaker for manu-script editing.
REFERENCES
1. Scutchfield SB. All-terrain vehicles: injuries and prevention.Clin Orthop.
2. Consumer Product Safety Commission.Annual Report of ATV Deaths and Injuries. Washington, DC: Consumer Product Safety Commission; 2000 3. US District Court for the District of Columbia. United States of America versus American Honda Motor Co., Inc., et al: Final Consent Decree: Civil Action 87-3525. March 14, 1988
4. American Academy of Pediatrics, Committee on Injury and Poison Prevention. All-terrain vehicle injury prevention: two-, three-, and four-wheeled unlicensed motor vehicles.Pediatrics.2000;105:1352–1354 5. American Academy of Pediatrics. All-Terrain Vehicle Regulation Act
[model bill]. In:American Academy of Pediatrics Policy Reference Guide. Elk Grove Village, IL: American Academy of Pediatrics; 1989
6. Cvijanovich NZ, Cook LJ, Mann NC, Dean JM. A population-based assessment of pediatric all-terrain vehicle injuries.Pediatrics.2001;108: 631– 635
7. Lynch J, Gardner M, Worsey J. The continuing problem of all-terrain vehicle injuries in children.J Pediatr Surg.1998;33:329 –332
8. Ross R, Stuart L, Davis F. All-terrain vehicle injuries in children: indus-try-regulated failure.Am Surg.1999;65:870 – 873
9. Bercher D, Staley K, Turner L, Aitken M. Pediatric injuries resulting from use of all-terrain vehicles.J Ark Med Soc.2001;97:351–353 10. Consumer Product Safety Commission.All-Terrain Vehicle 2001 Injury
and Exposure Studies. Washington, DC: Consumer Product Safety Commission; 2003
11. Rodgers GB. The effectiveness of helmets in reducing all-terrain vehicle injuries and deaths.Accid Anal Prev.1990;22:47–58
12. Brown RL, Koepplinger ME, Mehlman CT, Gittelman M, Garcia VF. All-terrain vehicle and bicycle crashes in children: epidemiology and comparison of injury severity.J Pediatr Surg.2002;37:375–380 13. Helmkamp JC. A comparison of state-specific all-terrain vehicle-related
death rates, 1990 –1999.Am J Public Health.2001;91:1792–1795 14. Upperman JS, Shultz B, Gaines BA, et al. All-terrain vehicle rules and
regulations: impact on pediatric mortality. J Pediatr Surg. 2003;38: 1284 –1286
15. Keenan HT, Bratton SL. All-terrain vehicle legislation for children: a comparison of a state with and a state without a helmet law.Pediatrics.
2004;113(4). Available at: www.pediatrics.org/cgi/content/full/113/ 4/e330
16. Consumer Product Safety Commission.35 Witnesses Set to Testify at CPSC Regional ATV Safety Hearing in West Virginia: ATV Injuries Double in 5-Year Period, Deaths Continue to Climb.Washington, DC: Consumer Product Safety Commission; 2003. Publication 03–136.
17. Healthcare Cost and Utilization Project.Kids’ Inpatient Database (KID), 1997[CD-ROMs]. Rockville, MD: Agency for Healthcare Research and Quality; 2000
18. Healthcare Cost and Utilization Project.Kids’ Inpatient Database (KID), 2000[CD-ROMs]. Rockville, MD: Agency for Healthcare Research and Quality; 2002
19. Healthcare Cost and Utilization Project.2000 Kids’ Inpatient Database (KID) Technical Documentation. Rockville, MD: Agency for Healthcare Research and Quality; 2002
20. US Department of Health and Human Services.International Classifica-tion of Diseases, 9th Revision, Clinical ModificaClassifica-tion. Washington, DC: US Department of Health and Human Services, Public Health Service, Health Care Financing Administration; 1998
21. Westfall JM, McGloin J. Impact of double counting and transfer bias on estimated rates and outcomes of acute myocardial infarction.Med Care.
2001;39:459 – 468
22. ICDMAP-90 [computer program]. Baltimore, MD: Johns Hopkins Uni-versity and Tri-Analytics, Inc; 1998
23. Baker SP, O’Neill B. The injury severity score: an update.J Trauma.
1976;16:882– 885
24. Stata Corp. Stata statistical software: release 7.0. College Station, TX: Stata Corp; 2001
25. Agency for Healthcare Research and Quality.Nationwide Inpatient Sam-ple Technical Documentation. Rockville, MD: Agency for Healthcare Re-search and Quality; 2004
26. US Bureau of the Census.Profile of General Demographic Characteristics: 2000. Washington, DC: US Bureau of the Census; 2002
27. Rodgers GB. The characteristics and use patterns of all-terrain vehicle drivers in the United States.Accid Anal Prev.1999;31:409 – 419 28. Rodgers GB. Risk factors for all-terrain vehicle injuries: a national
case-control study.Am J Epidemiol.2001;153:1112–1118
29. Marciani R, Caldwell G, Levine H. Maxillofacial injuries associated with all-terrain vehicles.J Oral Maxillofac Surg.1999;57:119 –123
30. Lister D, Morgan J III, Denning D, Valentovic M, Trent B, Beaver B. Pediatric all-terrain vehicles trauma: a 5-year statewide experience.
J Pediatr Surg.1998;33:1081–1083
31. Consumer Product Safety Commission. All-Terrain Vehicle Exposure, Injury, Death, and Risk Studies. Washington, DC: Consumer Product Safety Commission; 1998
32. Hargarten SW. All-terrain vehicle mortality in Wisconsin: a case study in injury control.Am J Emerg Med.1991;9:149 –152
33. Holman R, Curns A, Belay E, Steiner C, Schonberger L. Kawasaki syndrome hospitalizations in the United States, 1997 and 2000. Pediat-rics.2003;112:495–501
DOI: 10.1542/peds.2004-1585
2005;115;e316
Pediatrics
M. Dick and Mary E. Aitken
Jeffrey B. Killingsworth, John M. Tilford, James G. Parker, James J. Graham, Rhonda
National Hospitalization Impact of Pediatric All-Terrain Vehicle Injuries
Services
Updated Information &
http://pediatrics.aappublications.org/content/115/3/e316 including high resolution figures, can be found at:
References
http://pediatrics.aappublications.org/content/115/3/e316#BIBL This article cites 17 articles, 3 of which you can access for free at:
Subspecialty Collections
son_prevention_sub
http://www.aappublications.org/cgi/collection/injury_violence_-_poi
Injury, Violence & Poison Prevention
http://www.aappublications.org/cgi/collection/hospital_medicine_sub
Hospital Medicine
following collection(s):
This article, along with others on similar topics, appears in the
Permissions & Licensing
http://www.aappublications.org/site/misc/Permissions.xhtml in its entirety can be found online at:
Information about reproducing this article in parts (figures, tables) or
Reprints
DOI: 10.1542/peds.2004-1585
2005;115;e316
Pediatrics
M. Dick and Mary E. Aitken
Jeffrey B. Killingsworth, John M. Tilford, James G. Parker, James J. Graham, Rhonda
National Hospitalization Impact of Pediatric All-Terrain Vehicle Injuries
http://pediatrics.aappublications.org/content/115/3/e316
located on the World Wide Web at:
The online version of this article, along with updated information and services, is
by the American Academy of Pediatrics. All rights reserved. Print ISSN: 1073-0397.