ISSN: 2171-4703 © 2016 SECOIR
Highlights for improving cyclotorsional eye-tracking
success rate in femtosecond laser-assisted LASIK with
WaveLight EX500 excimer laser
Hung-Yuan Lin, MD
1,2,3; Feng-Ju Zhang, MD, PhD
4,5; Ya-Jung Chuang, MD
6;
Pi-Jung Lin, MD, PhD
6; Han-Chieh Yu, MD
7PURPOSE: To present novel techniques for improving the success rate of cyclotorsional eye-tracking and visual and refractive outcomes following LASIK with an IntraLase 150-kHz femtosecond and WaveLight EX500 excimer laser.
SETTING: Universal Eye Center, Zhongli, Taoyuan, Taiwan.
METHODS: A total of 84 eyes of 47 patients with myopia or myopic astigmatism were enrolled. If patients had dense opaque bubble layers (OBLs) and gas accumulation through the pocket in the perilimbal area impeding cyclotorsional eye-tracking, gentle scraping of the surface with a fl ap lifter was used to decrease OBL density and gas in the perilimbal area.
Th e fl ap lifter was also used to cover the gas in the perilimbal area and simulate an enlarged
circle delineating the corneal periphery for comparison with reference images. Adequate adjustment of illumination and infrared light facilitated cyclotorsional eye-tracking. Preoperative and postoperative uncorrected distance visual acuity (UDVA), corrected distance visual acuity (CDVA), manifest sphere and cylinder were analyzed.
RESULTS: Eye-tracking was successfully performed in all eyes. Th e mean ± SD preoperative
spherical equivalent (SE) refraction was −5.43 ± 2.28 diopters (D). Th ree months
postoperatively, all eyes maintained or had improved CDVA. UDVA was 20/20 or better in 85%, and 20/40 or better in 100% of the eyes. Overall, 75% and 93% of the eyes had SE
refraction within ±0.5 D and ±1.0 D, respectively. Th e mean magnitude of cyclotorsion was
2.40 degrees ± 1.89 (range 0.0 to 9.0 degrees).
CONCLUSION: Th e novel methods improved eye registration success and cyclotorsional eye-tracking using the WaveLight EX500 excimer laser.
J Emmetropia 2016; 2: 85-93
Femtosecond lasers have become a commonly used technology for the creation of corneal fl aps during refractive surgery.
Th e advantages of femtosecond lasers over
mechanical microkeratomes for fl ap creation include greater predictability of fl ap thickness and diameter, improved astigmatic neutrality, decreased incidence of fl ap injury, and stronger fl ap adhesion1-3.
Femtosecond lasers create corneal fl aps using photodisruption, in which each laser pulse creates a gas bubble within the corneal stroma. An opaque bubble layer (OBL), creating a diff use opacity, may form in the corneal stroma if the collection of gas bubbles becomes
trapped. Th e reported incidence of OBL ranges from
5% to 56.4%4-6. Gas situated in the pocket between
the hinge and limbus in the perilimbal area is often seen beneath the corneal fl aps created using IntraLase femtosecond laser (Abbott Medical Optics), and may interrupt the eye registration process.
Th e development of cyclotorsional eye-tracking
systems has led to major advances in excimer laser procedures. Eyes can move and cyclorotate from the upright to supine position and also during the
excimer laser ablation7. Cyclotorsion of the eye
during laser in situ keratomileusis (LASIK) can lead Submitted: 6/19/2016
Accepted: 7/23/2016
1 Universal Eye Center, Zhong-Li, Taiwan.
2 Department of Optometry, Central Taiwan University of Science
and Technology, Taichung, Taiwan.
3 Department of Ophthalmology, Fu-Jian Medical University,
Fuzhou, China.
4 Beijing Tongren Eye Center, Beijing Tongren Hospital of Capital
Medical University, Beijing, China.
5 Beijing Ophthalmology & Visual Sciences Key Lab, Beijing, China. 6 Universal Eye Center, Taipei, Taiwan.
7 Universal Eye Center, Banqiao, New Taipei, Taiwan.
Financial Disclosure: Th e authors have no proprietary or commercial interest in any of the materials discussed in this article.
Corresponding Author: Han-Chieh Yu, MD Universal Eye Center
1F., No.35, Zhongxiao Rd., Banqiao Dist., New Taipei 22063, Taiwan E-mail: hc.yu@eyecenter.com.tw
to decreased correction of astigmatism and worsen
visual and refractive outcomes8. Cyclotorsional
eye-tracking systems have been shown to improve refractive predictability and effi cacy9.
However, dense OBL that masks pupil or iris characteristics could cause failure of iris registration and subsequent cyclotorsional tracking. Furthermore, gas accumulation in the perilimbal area through the pocket may obscure the architectural landmarks of the iris and prevent the automatic iris detection from working, thereby interrupting the excimer laser surgery.
Th e effi cacy of LASIK for the correction of visual
acuity and refractive cylinders may be decreased when the cyclotorsional eye trackers are inactive during the procedure8.
In the present study, we describe novel techniques for overcoming intraoperative failure of cyclotorsional tracking while using an IntraLase 150-kHz femtosecond and EX500 excimer laser, and their utility in improving postoperative visual acuity and refraction.
PATIENTS AND METHODS
In this retrospective study, consecutive patients undergoing LASIK with femtosecond laser fl ap creation from March 2014 to May 2014 at Universal Eye Center, Zhongli, Taoyuan, Taiwan were evaluated. All patients received a thorough explanation of the risks and benefi ts of LASIK, including a discussion
of nonsurgical alternatives. Th e present study was
approved by the Institutional Review Board of Antai Tian-Sheng Memorial Hospital (15-026-B1).
Inclusion–Exclusion Criteria
All patients enrolled in the present study had no history of previous ocular surgery and had discontinued contact lens use (if present) for at least 1 week. Prior to intervention, a complete preoperative ophthalmologic evaluation ensured the absence of current or previous ocular pathology other than refractive error. Additional inclusion criteria were as follows: minimum age of 18 years and planned residual stromal bed thickness of at least 275 μm.
Exclusion criteria for LASIK were as follows: systemic or ocular diseases, history of corneal dystrophy or herpetic eye disease, topographic evidence of ectatic corneal disorder/keratoconus, corneal warpage from contact lens use, glaucoma, severe dry eye, and collagen vascular diseases.
All patients underwent a baseline ophthalmic examination that included measurements of uncorrected distance visual acuity (UDVA) and corrected distance visual acuity (CDVA), manifest and cycloplegic refraction, keratometry (K), corneal topography (OPD-Scan III, Nidek) and tomography (Allegro Topolyzer Vario, WaveLight, Alcon Laboratories), corneal pachymetry (Allegro Topolyzer Vario, WaveLight, Alcon Laboratories), pupil size (OPD-Scan III, Nidek),
intraocular pressure (Nidek), slit lamp biomicroscopy, and dilated fundus examination. UDVA, manifest refraction and slit lamp biomicroscopy were repeated at 1-week, 1-month, and 3-month postoperative visits.
Surgical technique
All eyes underwent myopic LASIK surgery performed by the same surgeon (HYL). Corneal fl aps were created with a 150-kHz IntraLase femtosecond
laser (Abbott Medical Optics). Th e attempted fl ap
thickness was 100 μm. Th e elliptical fl ap diameter was
9.00 × 8.65 mm. Other laser parameters were temporal hinge, angle of 60 degrees, mean bed energy of 0.95 μJ, spot separation of 7 μm, line separation of 7 μm, side-cut energy of 1 μJ, side-cut angle of 110 degrees, pocket width of 0.25 mm, initial pocket depth of 230 μm, and pocket tangent and radian spot separation of 7/7 μm.
Excimer laser ablation was performed using a WaveLight EX500 excimer laser (WaveLight, Alcon Laboratories) at a pulse repetition rate of 500 Hz. Th e eye tracker scanning rate of the EX500 was 1050 Hz, synchronized to the 500-Hz repetition rate of the scanning spot, with a latency time of 2 milliseconds. Ablation was centered on 70% of the distance from the pupil center to the apex (which was a misnomer
in the EX500 that in fact meant corneal vertex). Th e
Custom-Q profi le with a plano refraction target was used in all patients, and treatment was based on manifest refraction. Cyclotorsional eye registration was attempted in all patients.
Novel methodology for improving cyclotorsional eye-tracking success rate
Preoperative
Th e Allegro Topolyzer Vario captured two-dimensional images of the anterior segment that
included the cornea, pupil, and iris. Th e pupil center
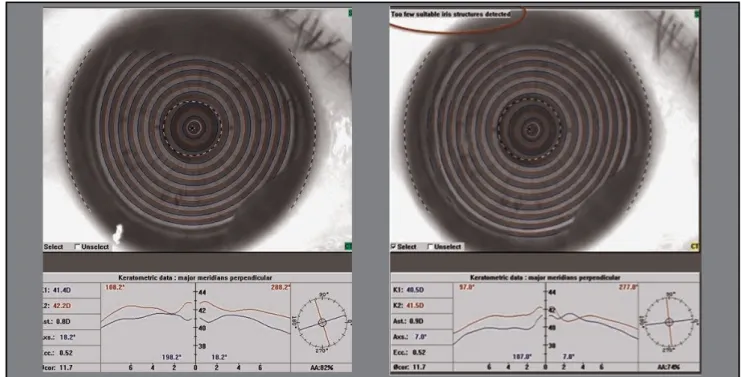
and limbus locations were also determined. Some patients demonstrated “Too few suitable iris structures detected” that could lead to a decreased tracking success rate (Figure 1).
Operators selected the best reference image for registration and paid close attention to keratometry values and axis, iris images, pupil diameter, and pupil center coordinates relative to the apex (expressed as “Pupil Dec. X/Y” in the EX500) (Figure 2).
Intraoperative
After fl ap creation and lifting, the following three steps were required for successful cyclotorsional eye-tracking.
Step 1. Automatic limbus fi t: Measurement of iris size
OBL in the perilimbal area might cause the EX500 excimer laser to erroneously detect the iris as smaller and return the “Diff erence of iris size between diagnostic
Figure 1. Normal photo capture in the right eye. Th e “Too few suitable iris structures detected” error was shown during examination of the left eye with the Topolyzer Vario.
Figure 2. Selection of a good reference image for registration with consideration of keratometry values and axis, iris images, pupil diameter, and pupil center coordinates relative to the apex (expressed as “Pupil Dec. X/Y” in the EX500).
image and current image is too large” error message. Gentle scraping of the stromal surface with a fl ap lifter could decrease OBL density and gas accumulation in the perilimbal area (Figure 3).
Th e initial use of a fl ap lifter might increase the
automatic iris size (white-to-white) detection rate.
If the previous method failed, and the same error message occurred, the fl ap lifter was used to cover the gas accumulation in the perilimbal area, simulating an enlarged circle delineating the corneal periphery, to allow successful comparison with the reference iris image (Figure 4).
Figure 4. Th e fl ap lifter can be used to cover the gas accumulation in the perilimbal area (red arrow in right-upper panel) to simulate an enlarged circle delineating the corneal periphery (green arrows in right-upper panel) to allow successful comparison with the reference iris image if the “Diff erence of the iris size between diagnostic image and current image is too large” error occurs.
Figure 3. Left-upper panel shows an example of the “Diff erence of the iris size between diagnostic image and current image is too large” error. After gentle scraping of the surface with the fl ap lifter (right-upper panel) to decrease the density of the gas in the perilimbal area (red arrow in left-lower panel), the iris size (white-to-white) can be successfully detected.
Automatic Iris Detection
Iris Diameter
Diagnostic 11.98 mm
Treatment 10.18 mm
Automatic Iris Detection
Iris Diameter
Diagnostic mm
Treatment mm
Adapt Pupil Size
Pupil Diameter
Diagnostic 3.13 mm
Treatment 4.10 mm
Adapt Pupil Size
Pupil Diameter
Diagnostic 3.98 mm
Treatment 9.08 mm Automatic Iris Detection
Iris Diameter
Diagnostic 11.95 mm
Treatment 11.36 mm
Step 2. Adapt pupil size: Pupil diameter matching
Th e diameter of the pupil was continuously
measured under the laser and controlled by adjusting the illumination level to match the reference pupil image as closely as possible.
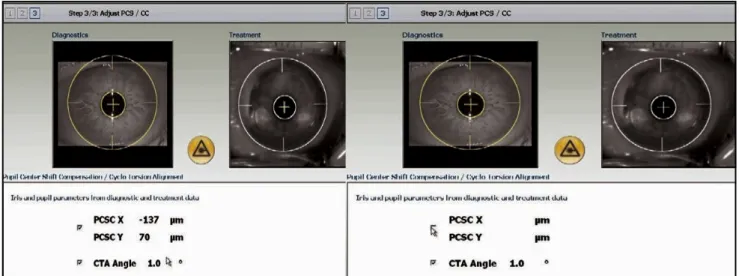
Step 3. Adjust PCS/CC: Pupil center shift compensation and cyclotorsion alignment
On beginning step 3, the most common issue was the inability to detect the “CTA angle” with the
bottom column showing “Confi rm with OK.” Th is
issue might result for several reasons. First, dense OBL would obscure the iris from being imaged. Second,
a diff erent pupil size from the reference image could
change the iris characteristic markers. Th ird, too few
suitable iris structures detected with the Topolyzer Vario (Figure 1) would cause CTA angle detection failure. Adjusting the infrared light level could enhance the contrast of the iris image and overcome the interference of OBL (Figure 5). A proper illumination level helped to obtain the intraoperative pupil size similar to the reference one, and retain the iris characteristic markers. However, failure to detect suitable iris structures with the Topolyzer Vario would make the determined pupil margin on the monitor become yellow and CTA angle detection invalid (Figure 6). Th is situation represents registration failure.
Figure 5. Low infrared light level would fail to reveal suff cient iris characteristics markers and the CTA angle would be unable to be detected (left panel). Adequate infrared light level could enhance the contrast of the iris image and overcome the interference of OBL (right panel).
Figure 6. Th e change of color of the determined pupil margin from green to yellow may indicate too few suitable iris structures detected with the Topolyzer Vario, which would cause the “CTA status: invalid” error message to be displayed. Th e operator could go to step 3, although the CTA angle would not be displayed and cyclotorsion registration would fail.
Th e locations of the photopic pupil center and apex were determined preoperatively with the Topolyzer Vario. During PCSC, the diff erence between the live location of the pupil center to the limbus and the one recorded with the Topolyzer Vario was measured and expressed
in Cartesian coordinates. Th e angle of cyclotorsion was
calculated and shown in degrees. If the PCSC (X, Y) distances were less than 100 microns, their values were then added to the distance between the pupil center and apex (pupil shift compensation) measured with the Topolyzer Vario. If the distances were greater than 100 microns, the values were not added to the distance between the pupil and apex (Figure 7). We then set the center of ablation at 70% of the distance from the pupil center to apex. Finally, the excimer laser was applied as usual.
Statistical analyses
Descriptive statistics for each variable were calculated.
Th e preoperative and postoperative visual acuity and
astigmatism profi les are presented as means ± SD. All data were analyzed using PSPP 0.8.4 (Free Software Foundation) and Microsoft Excel 2013 (Microsoft).
RESULTS
Baseline patient demographics
Table 1 shows the demographic data of all treated
eyes. Th e study consisted of 25 female and 22 male
patients. Th ere were 42 right eyes and 42 left eyes.
Mean patient age was 32.4 ± 7.6 years (range, 18 to 46 years). Mean preoperative spherical error was −4.95 ± 2.24 D (range, −0.75 to −9.50 D). Mean preoperative cylindrical error was −0.95 ± 0.82 D (range, 0 to −4.25 D). Mean preoperative spherical equivalence (SE) was −5.43 ± 2.28 D (range, −1.00 to −10.25 D).
Intraoperative eye registration
Intraoperative cyclotorsional eye registration was successful in 84 eyes (100%). All eyes were matched to preoperative diagnostic images. Ablation center shift to 70% of the distance from the pupil center to the apex and cyclotorsion alignment was successfully accomplished
in all patients. Th e mean absolute value of the CTA angle
in the present study was 2.40 ± 1.89 degrees (range, 0 to 9 degrees). No patient in the present study encountered failure of cyclotorsional eye-tracking due to too few suitable iris structures being detected during the preoperative period.
Effi cacy and safety
Figure 8, A shows the effi cacy expressed as Snellen
visual acuity. A preoperative CDVA of 20/20 was observed in 74 of the 79 eyes (94%). A postoperative UDVA of 20/20 or better at 3 months was observed in 70 eyes (85%). A preoperative CDVA of 20/40 was observed in 100% of the eyes. A postoperative UDVA of 20/40 or better was observed in all eyes at 1 month and 3 months.
Figure 8, B shows no eyes (0%) lost CDVA, 4 eyes (5%) gained 1 line, and 1 eye (1%) gained 2 lines at 3 months.
Table 1. Preoperative demographics.
Parameter Mean ± SD Minimum Maximum
Age 32.49 ± 7.6 18 46
SE (D) −5.43 ± 2.28 −1.00 −10.25
Sphere (D) −4.95 ± 2.24 −0.75 −9.5
Cylinder (D) −0.95 ± 0.82 0 −4.25 D = diopters; SE = spherical equivalent.
Figure 7. In patients with PCSC X and PCSC Y distances greater than 100 microns, their values were not added to the distance between the pupil and apex.
Refractive predictability and stability
Th e attempted versus achieved SE refraction
for all eyes is shown in Figure 8, C. At 3 months, 63 eyes (75%) were within 0.5 D of the attempted refractive change and 78 eyes (93%) were within 1.0 D (Figure 8, D).
Seventy-six eyes (90%) had residual astigmatism within 0.5 D and 82 eyes (98%) within 1.0 D (Figure 8, E). Th e mean postoperative SE was −0.12 ± 0.59 D (range, +1.50 to −2.00 D) at 1 month and −0.20 ± 0.53 D (range, +1.25 to −1.75 D) at 3 months (Figure 8, F).
Figure 8. Th ree-month postoperative cumulative UDVA (effi cacy) (A) and change in CDVA (safety) (B). Attempted versus achieved SE (predictability) (C), refractive accuracy in SE (D) and astigmatism (E), and refractive stability (F).
DISCUSSION
Cyclotorsional movement is defi ned as the
rotational movement of the eye around the visual axis.
Th e mean cyclotorsional movements observed during
refractive surgery procedures have been reported to
be approximately 3 degrees10. Th e mean absolute
value of the CTA angle in the present study was 2.41 ± 1.90 degrees (range, 0 to 9 degrees). Iris registration has been successful as a potential method
to compensate cyclotorsional misalignments11, and
may be useful in ensuring that ablation is delivered to the intended location to improve postoperative visual
acuity and decrease astigmatism9,12,13.
Photodisruption generated by the femtosecond laser creates gas bubbles that dissipate throughout the
cornea resulting in a cleavage plane. Th e expanding gas
bubbles migrate through the path of least resistance within the cornea and may occasionally be retained as OBL. OBL tends to form under conditions such as a thickened cornea, hard-docking, or a steeper cornea, possibly attributable to increased corneal rigidity and
resistance in these situations4,6. Th e incidence of OBL
has been reported to be 56.4% and 52.5% using the IntraLase 15-kHz and 60-kHz femtosecond laser
systems, respectively5,6. Jung et al.4 reported a lower
incidence of OBL of 5% using the newer Visumax 500-kHz femtosecond laser.
Dense OBL and gas accumulation in the perilimbal area may interfere with the cyclotorsional
eye-tracking system during excimer laser ablation5. Th e
EX500 excimer laser attempts to match the iris size (white-to-white) with the preoperative eye images from the fi rst step of eye registration. Gas situated in the pocket between the hinge and limbus in the perilimbal area may interrupt the eye registration process and thereby inactivate the eye tracker in the following excimer laser ablation. As maintained activation of the cyclotorsional eye tracker can improve postoperative visual acuity and
astigmatism correction results8,14, there is a clinical need
to overcome interruption of the eye tracker by dense OBL or gas accumulation in the perilimbal area.
Th e present study highlights the importance of
selecting a good reference image preoperatively. Several measurements are taken and provide information on pupil diameter, keratometry values and axes, and
location with respect to the apex. Th e intraoperative key
points are as follows:
1. Gentle scraping of the stromal surface with a fl ap lifter can decrease OBL density and gas
accumulation in the perilimbal area. Th e initial use of a
fl ap lifter may increase the automatic iris size (white-to-white) detection rate.
2. Using a fl ap lifter to cover the gas accumulation
in the perilimbal area can be used to simulate an enlarged circle delineating the corneal periphery for comparison with the reference image.
3. Adjustment of the illumination to ensure pupil
diameters are as close as possible to the reference pupil image.
4. Adequate infrared light to enhance the contrast
of the captured iris characteristic markers for matching with the reference image.
Adjustment of illumination to ensure live pupil diameter values are as close as possible to the reference pupil image, and adequate infrared lighting to optimize intraoperative imaging of the iris characteristic markers and facilitate the registration process are important during the second and third steps of eye registration.
With the use of novel methodology to improve cyclotorsional eye-tracking success rates, we achieved a higher eye-tracking success rate of 100%. Previous studies have reported eye-tracking success rates ranging from 57% to 90.5% with the IntraLase 60-kHz femtosecond and Zyoptix 100-Hz excimer laser
systems7,15,16. In the present study, we demonstrated
refractive effi cacy, safety, and predictability in correcting visual acuity and myopic astigmatism comparable to the results achieved using diff erent excimer laser platforms reported by previous studies13,17-19.
In conclusion, in patients in whom OBL or gas accumulation in the perilimbal area interferes with the eye tracker, initial gentle scraping of the surface with the fl ap lifter decreases OBL density and gas accumulation in the perilimbal area and increases the automatic iris size (white-to-white) detection rate. Using a fl ap lifter to cover the gas accumulation in the perilimbal area can simulate an enlarged circle delineating the corneal periphery, improving the success rate of eye registration and subsequent tracking. Adjustment of illumination and infrared light can be used to control pupil diameter and enhance captured iris characteristic markers for matching with the reference image. Good postoperative visual acuity and astigmatism results were obtained in the present study that were comparable to previous studies.
REFERENCES
1. Binder PS. Flap dimensions created with the IntraLase FS laser. J Cataract Refract Surg 2004; 30:26-32.
2. Kezirian GM, Stonecipher KG. Comparison of the IntraLase femtosecond laser and mechanical keratomes for laser in situ keratomileusis. J Cataract Refract Surg 2004; 30:804-11. 3. Kim JY, Kim MJ, Kim TI, Choi HJ, Pak JH, Tchah H. A
femtosecond laser creates a stronger fl ap than a mechanical microkeratome. Invest Ophthalmol Vis Sci 2006; 47:599-604. 4. Jung HG, Kim J, Lim TH. Possible risk factors and clinical
eff ects of an opaque bubble layer created with femtosecond laser-assisted laser in situ keratomileusis. J Cataract Refract Surg 2015; 41:1393-9.
5. Kaiserman I, Maresky HS, Bahar I, Rootman DS. Incidence, possible risk factors, and potential eff ects of an opaque bubble layer created by a femtosecond laser. J Cataract Refract Surg 2008; 34:417-23.
6. Liu CH, Sun CC, Hui-Kang Ma D, Chien-Chieh Huang J, Liu CF, Chen HF, Hsiao CH. Opaque bubble layer: incidence, risk factors, and clinical relevance. J Cataract Refract Surg 2014; 40:435-40.
7. Chang J. Cyclotorsion during laser in situ keratomileusis. J Cataract Refract Surg 2008; 34:1720-6.
8. Ghosh S, Couper TA, Lamoureux E, Jhanji V, Taylor HR, Vajpayee RB. Evaluation of iris recognition system for wavefront-guided laser in situ keratomileusis for myopic astigmatism. J Cataract Refract Surg 2008; 34:215-21. 9. Neuhann IM, Lege BA, Bauer M, Hassel JM, Hilger A,
Neuhann TF. Static and dynamic rotational eye tracking during LASIK treatment of myopic astigmatism with the Zyoptix laser platform and Advanced Control Eye Tracker. J Refract Surg 2010; 26:17-27.
10. Arba Mosquera S, Verma S. Eff ects of torsional movements in refractive procedures. J Cataract Refract Surg 2015; 41:1752-66.
11. Chernyak DA. From wavefront device to laser: an alignment method for complete registration of the ablation to the cornea. J Refract Surg 2005; 21:463-8.
12. Bharti S, Bains HS. Active cyclotorsion error correction during LASIK for myopia and myopic astigmatism with the NIDEK EC-5000 CX III laser. J Refract Surg 2007; 23:S1041-45. 13. Khalifa M, El-Kateb M, Shaheen MS. Iris registration in
wavefront-guided LASIK to correct mixed astigmatism. J Cataract Refract Surg 2009; 35:433-7.
14. Mrochen M, Eldine MS, Kaemmerer M, Seiler T, Hutz W. Improvement in photorefractive corneal laser surgery results using an active eye-tracking system. J Cataract Refract Surg 2001; 27:1000-6.
15. Luengo Gimeno F, Chan CM, Li L, Tan DT, Mehta JS. Comparison of eye-tracking success in laser in situ keratomileusis after fl ap creation with 2 femtosecond laser models. J Cataract Refract Surg 2011; 37:538-43.
16. Prakash G, Ashok Kumar D, Agarwal A, Jacob S, Sarvanan Y, Agarwal A. Predictive factor analysis for successful performance of iris recognition-assisted dynamic rotational eye tracking during laser in situ keratomileusis. Am J Ophthalmol 2010; 149:229-37e222.
17. Shen EP, Chen WL, Hu FR. Manual limbal markings versus iris-registration software for correction of myopic astigmatism by laser in situ keratomileusis. J Cataract Refract Surg 2010; 36:431-6.
18. Tantayakom T, Lim JN, Purcell TL, Nalgirkar A, Cheng L, Schanzlin DJ. Visual outcomes after wavefront-guided laser in situ keratomileusis with and without iris registration. J Cataract Refract Surg 2008; 34:1532-7.
19. Yu CQ, Manche EE. Comparison of 2 wavefront-guided excimer lasers for myopic laser in situ keratomileusis: one-year results. J Cataract Refract Surg 2014; 40:412-22.
First author:
Hung-Yuan Lin, MD
Universal Eye Center, Zhong-Li, Taiwan. Central Taiwan University of Science and Technology, Taichung, Taiwan.