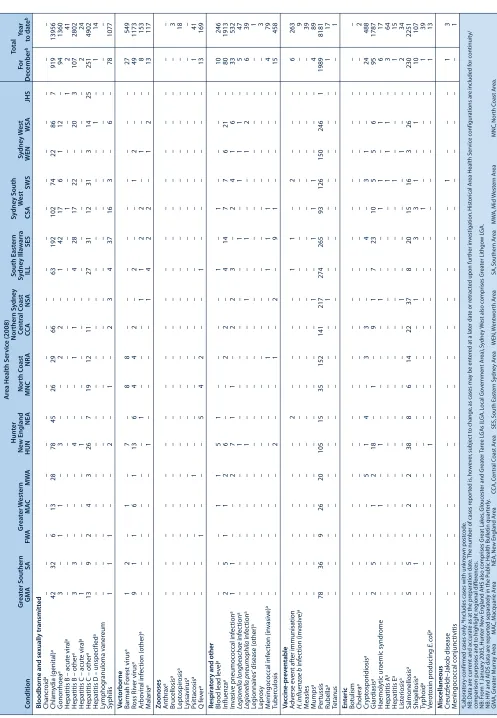
Figure 1 and Tables 1 and 2 show reports of communica-ble diseases received through to the end of December 2008 in New South Wales (NSW).
Pertussis (whooping cough)
An outbreak of pertussis that commenced in northern NSW in late 2007 has continued to spread across NSW. In November and December, there were 1740 cases and 1989 cases respectively reported. A total of 8181 cases were reported in 2008, equivalent to 119 cases per 100 000 people. This represents a significant increase since 2007 where 2097 cases were reported (30/100 000 people). Cases under 1 year of age had the highest age-specific incidence (346 cases notified, which is equivalent to 386 cases per 100 000). Many of these children were not yet immunised as the vaccine is routinely given at 2, 4 and 6 months of age. No deaths were reported in children or infants who are normally at greatest risk of severe mor-bidity and mortality from pertussis.
A second peak was seen in children aged around 14 years, where there were 293 cases reported (equivalent to an age-specific rate of 318 cases per 100 000). A school-based pertussis booster immunisation program is due to com-mence in 2009, targeting children in year 10 who will be aged around 15 years.
In recent months, the proportion of cases diagnosed using polymerase chain reaction (PCR) has increased substan-tially and the majority of cases are now diagnosed using PCR rather than by serology. This is likely to reflect the
Communicable Diseases Report, NSW,
November and December 2008
For updated information, including data and facts on specific diseases, visit www.health.nsw.gov.au and click on Infectious Diseases or access the site directly at: http://www.health.nsw.gov.au/public health/infectious/index.asp.
Communicable Diseases Branch
NSW Department of Health
increased proportion of cases in younger age groups where PCR-based diagnosis is typical and clinicians have increased awareness of the availability and advantages of PCR tests over traditional serological testing methods. Key public health messages for pertussis have included recommendations:
• to ensure that pertussis vaccines are given on time to babies at 2, 4 and 6 months and the booster is given to children at 4 years
• to inform the community about the adult booster vaccine for parents and carers of babies and young children, child-care workers and health-care workers • to be alert for the clinical features of pertussis and
seek medical assessment promptly; early diagnosis and treatment reduces the period of infectiousness • to administer chemoprophylaxis to contacts where the
case is likely to have significant contact with at-risk infants who are at greatest risk of severe disease.
Enteric diseases
In November and December 2008, NSW public health units investigated 61 outbreaks of gastroenteritis, including 47 where person-to-person transmission was likely and 14 sus-pected to be the result of foodborne transmission.
gens in curry meals.
The remaining outbreaks were small, affecting three and four people after restaurant meals. No pathogens were detected in any of these cases. The sites of the outbreaks were inspected and no known sources were identified.
Shiga toxin-producing Escherichia coli
and haemolytic uraemic syndrome
Shiga toxin-producing Escherichia coli (STEC) are bacte-ria that can cause serious gastrointestinal disease charac-terised by diarrhoea, which in some cases can be bloody. In a small proportion of cases, STEC can progress to haemolytic uraemic syndrome (HUS), which results in kidney failure, bleeding and anaemia. Infections tend to increase in the warmer months.1
In November and December 2008, NSW public health units were notified of eight STEC (two serotype O157 and seven of unknown serotype) and six HUS cases (three were also STEC positive). Of the eight cases, ages ranged from 2 to 75 years. Six were female and two male. The HUS cases were in both children and adults over 40. This number of STEC and HUS cases is consistent with the sea-sonal increase seen at this time each year.
STEC infection can be transmitted through:
• eating contaminated food (undercooked hamburgers, unwashed salad, fruit, vegetables and unpasteurised milk or milk products)
• drinking or swimming in contaminated water
infection
• contact with infected animals.2,3
The most important ways to prevent infection with STEC and other foodborne diseases are to:
• cook hamburgers and sausages thoroughly to at least 71°C. Although colour alone is not necessarily a good indicator, do not eat hamburgers or sausages if there is any pink meat inside
• wash hands well after handling raw meat
• use different knives and cutting boards for raw meat preparation and other food preparation
• wash raw vegetables and fruits thoroughly
• refrigerate perishable food until ready to eat – so that bacteria do not incubate out of the fridge
• wash hands well after touching animals or their faeces.
For more information see: http://www.health.nsw.gov.au/ publichealth/Infectious/a-z.asp
References
1. Tarr PI, Gordon CA, Chandler WL. Shiga-toxin-producing Esceherichia coli and haemolytic uraemic syndrome. Lancet 2005; 365: 1073–86.
2. Heymann D, ed. Control of Communicable Diseases Manual, 18th ed. Washington: American Public Health Association; 2004, 160–4.
Communicable Diseases Report
Salmonella infections
0 100 200 300 400 500
600 S. OtherS. Typhimurium Legionnaires’ disease
0 4 8 12 16 20 24
L. pneumophila L. longbeachae
Oct. 08–Dec. 08
Male 57%
<5 y 0%
5–24 y 0%
25–64 y 71%
65+ y 29%
Rural 24%
Cryptosporidiosis 0 25 50 75 100 125 150 175 Oct. 08–Dec. 08 Male 59%
<5 y 45%
5–24 y 31%
25–64 y 22%
65+ y 2%
Rural 59%
Meningococcal disease 0 10 20 30 Men Gp B Men Gp C Men other/unk Oct. 08–Dec. 08 Male 64%
<5 y 29%
5–24 y 36%
25–64 y 21%
65+ y 14%
Rural 43%
Gonorrhoea 0 40 80 120 160 200 Oct. 08–Dec. 08 Male 82%
<5 y 0%
5–24 y 31%
25–64 y 67%
65+ y 2%
Rural 16%
Oct. 08–Dec. 08 Male 50%
<5 y 26%
5–24 y 28%
25–64 y 38%
65+ y 8%
Rural 43%
Oct. 08–Dec. 08 Male 43%
<5 y 0%
5–24 y 57%
25–64 y 29%
65+ y 14%
Rural 21%
Hepatitis A 0 20 40 60 80 Arbovirus infections 0 80 160 240 320 400 480 BFV RRV Oct. 08–Dec. 08 Male 51%
<5 y 0.4% 5–24 y 12%
25–64 y 69%
65+ y 19%
Rural 88%
Pertussis 0 200 400 600 800 1000 1200 1400 1600 1800 2000 Oct. 08–Dec. 08 Male 45%
<5 y 15%
5–24 y 45%
25–64 y 34%
65+ y 6%
Rural 44%
Measles 0 4 8 12 16 20 24 28 32 Measles lab conf Measles other Oct. 08–Dec. 08 Male 0%
<5 y 0%
5–24 y 0%
25–64 y 0%
65+ y 0%
Rural 0%
Month of onset NSW Population Male 50%
<5 y 7%
5–24 y 27%
25–64 y 53% 65+ y 13%
Rural 46%
Month of onset Gastroenteritis outbreaks in institutions 0 500 1000 1500 2000 2500 3000 3500 0 20 40 60 80 100 120 140 Outbreaks Cases Cases Outbreaks Oct. 08–Dec. 08 All outbreaks 92
Nursing homes 45 Hospitals 22
Child care 17
Schools 2
Other 6 Jan. 04
Jan. 05
Jan. 06
Jan. 07
Jan. 08
Jan. 04
Jan. 05
Jan. 06
Jan. 07
Jan. 08
Jan. 04
Jan. 05
Jan. 06
Jan. 07
Jan. 08
Jan. 04
Jan. 05
Jan. 06
Jan. 07
Jan. 08
Jan. 04
Jan. 05
Jan. 06
Jan. 07
Jan. 08
Jan. 04
Jan. 05
Jan. 06
Jan. 07
Jan. 08
Jan. 04
Jan. 05
Jan. 06
Jan. 07
Jan. 08
Jan. 04
Jan. 05
Jan. 06
Jan. 07
Jan. 08 Jan.
04 Jan.
05 Jan.
06 Jan.
07 Jan.
08
Jan. 04
Jan. 05
Jan. 06
Jan. 07
Jan. 08
Figure 1. Reports of selected communicable diseases, NSW, January 2004 to December 2008, by month of onset.
Preliminary data: case counts in recent months may increase because of reporting delays. Laboratory-confirmed cases only, except for measles, meningococcal disease and pertussis. BFV, Barmah Forest virus infection; RRV, Ross River virus infection; lab conf, laboratory confirmed; Men Gp C and Gp B, meningococcal disease due to serogroup C and serogroup B infection; other/unk, other or unknown serogroups.
NB: Multiple series in graphs are stacked, except gastroenteritis outbreaks.
T
a
ble 1.
Repor
ts of notifiable c
o
nditions r
e
ceiv
ed in No
v
ember 2008 b
y
ar
ea health ser
v
ic
es
Ar
ea Health S
e rv ic e (2008) Hunt er Nor thern S y dne y South East ern S y dne y South To tal Gr ea te r Southern Gr ea te r W e st ern N ew England Nor th C o ast C entr al C o ast S y dne y I lla w a rr a W est S y dne y W e st F o r C o ndition GMA S A F W A MA C M W A HUN N EA MNC N R A C C A NSA ILL SES C SA SWS WEN WSA JHS No v ember b to
Bloodborne and se
xually tr ansmitt e d Chancr o id a – – – – – – – –– – – – – – –––– – Chlam y d ia (genital) a 36 12 14 8 2 3 135 37 39 50 41 60 69 211 112 87 47 96 9 1088 13086 G o norrhoea a 2 – – – 1 5 – 2 – 1 6 3 40 22 9 1 11 – 107
Hepatitis B – acut
e viral a – – – – 1 – – – – – 1 – 1 – –––– 3
Hepatitis B – other
a 1 2 3 – – 6 4 – – 1 1 4 5 24 23 36 2 2 8 4 160
Hepatitis C – acut
e viral a 1– – 1 – – – – –– –– 1– – – – 1 4
Hepatitis C – other
a 11 9 6 8 9 26 12 14 17 18 10 27 39 37 31 12 25 56 372
Hepatitis D – unspecified
a –– ––– – – – – – – – – – – – 1 – 1 Ly m p h o g ra n u lo m a v a n e re u m – – – – – – – –– – – – – – –––– – S y philis – 2 4 – – 5 – 1 3 5 6 4 2 1 1 5 9 2 1 0 – 88 V e c torborne Barmah F o rest virus a – 1 1–– 6 3 7 1 4– – 1 –– – 1 – – 3 4 Ross R iv e r virus a 8 1 6 5 5 16 6 5 7 2 1 – – 1 1 – – – 64 Arbo viral inf ec tion (other) a –– ––– – 1 – 2 – 2 – 6 3 – 3 3 – 2 0 M alaria a 1– ––– – – 1 – – 1 – 1 – – 1 2 – 7 Z o onoses Anthrax a – – – – – – – –– – – – – – –––– – Bruc ellosis a – – – – – – – –– – – – – – –––– – Le pt ospir o sis a – – – 1 – – – – – – – – – – –––– 1 Ly ssa virus a – – – – – – – –– – – – – – –––– – P sittac o sis a –– ––– – – – – – – – – – 2 – – – 2 Q f e v e r a 1 1 2 1 1 – 4 2 2 1 – – – – –––– 1 5 Respir a to ry and other
Blood lead lev
e l a –– 4 6 – 1 1 – 1– –– 1– 1 3 – – 1 8 Influenza a 8 7 – 4 4 1 2 2 2 6 4 1 6 6 18 14 24 26 34 – 188 In v a siv e pneumoc o ccal inf ec tion a –– ––– 4 2 2 – 3 1 1 2 3 5 2 4 – 2 9 Legionella longbeachae inf ec tion a –– ––– 1 – – – – – – – – – 1 – – 2 Legionella pneumophila inf ec tion a –– ––– – – – – – – – – – 1 – 1 – 2 Le gionnair es
’ disease (other)
a – – – – – – – –– – – – – – –––– – Le p ro sy – – – – – – – –– – – – – – –––– – M e ningoc occal inf ec tion (in v a siv e ) a –– ––– – 1 – – – 1 1 2 – – – 1 – 6 Tu b e rc u lo si s 3– ––– 1 – 3 – – 8 1 5 4 – 2 9 – 3 6 V a ccine-pr e v e ntable A d v e rse ev ent af te r immunisation – – – – – 1 – – – 2 1 1 – – 2 – 2 – 9 H . influenzae b inf ec tion (in v a siv e ) a – – – – – – – –– – – – – – –––– – M e a sl e s – – – – – – – –– – – – – – –––– – Mumps a –– ––– – – – – – 1 – – – 2 – – – 3 P e rtussis 7 3 5 7 2 2 4 0 2 8 103 15 30 123 105 248 142 183 6 2 8 5 147 277 – 1740 Rubella a – – – – – – – –– – – – – 1 –––– 1 Te ta n u s – – – – – – – –– – – – – – –––– – En te ric B o tu li sm – – – – – – – –– – – – – – –––– – Cholera a –– ––– – – – – – – – – 1 – 1 – – 2 Cr ypt o sporidiosis a 4 – – 1 1– 3– 1 1 1 1 2 – 1 1 2 – 1 9 Giar diasis a 3 2 – 4 1 1 3 – 3 – 6 1 7 6 16 9 1 0 4 15 – 109 H a e m o ly ti c u ra e m ic s y n d ro m e – – – – – 1 – –– – – – – – –––– 1 Hepatitis A a –– ––– – – – – – 1 2 – 1 1 – – – 5 Hepatitis E a –– ––– – – – – – – 1 – – 1 – 1 – 3 List e riosis a –– ––– – – – – – – – 1 – 1 – – – 2 Salmonellosis a 8 1 1 1 5 12 3 5 10 10 21 7 2 2 8 17 9 2 2 – 163 Shigellosis a – – – – – – – – 1 – 1 1 6 4 –––– 1 3 Ty phoid a –– ––– – – – – – – – 3 1 – – 2 – 6 V e ro to xin pr oducing E. coli a – – – – – 1 – –– – – – – – –––– 1 M isc ellaneous C re u tz fe ld t– Ja k o b d is e a se – – – – – – – –– – – – – – –––– – M e ningoc occal c o njunc tivitis – – – – – – – – – – – – – – –––– – aLaborat or y-c
onfirmed cases only
.
bIncludes cases with unk
n o w n post co de . NB: Data ar e curr
ent and accurat
e
as at the pr
eparation dat
e
. T
h
e number of cases r
e por ted is , ho w e v e r, subjec t t o change
, as c
ases ma
y be ent
e
red at a lat
e r dat e or r e trac
ted upon fur
ther in
v
estigation.
Hist
orical Ar
ea Health S
e rvic e c o nfigurations ar e included f o r c o ntinuit co
mparison purposes and t
o highlight r e gional diff er enc e s. NB: F
rom 1 Januar
y 2005,
Hunt
er New England AHS also c
o mprises Gr eat Lak es , Glouc est
er and Gr
eat e r Ta ree L G A s (L GA, L o cal G o v e rnment Ar ea), S y dney W
est also c
o mprises Gr eat e r Lithgo w L G A. NB:
HIV and AIDS data ar
e r
e
por
ted separat
ely in the P
u
blic Health Bulletin quar
te rly . GMA, Gr eat e r Murra y Ar ea MA C, M a cquarie Ar ea NEA,
New England Ar
ea C C A, C e ntral C o ast Ar ea SES, South East ern S y dney Ar
ea WEN,
W e ntw o rt h Ar
ea SA,
Southern
Ar
ea MW
A, M id W est ern Ar ea MNC, Nor th C o ast Ar ea. NSA, Nor thern S y dney Ar
ea CSA,
C e ntral S y dney Ar ea WSA, W est ern S y dney Ar
ea FW
A, F ar W est Ar ea HUN, Hunt er Ar ea NRA, Nor thern R iv e rs Ar ea ILL, I lla warra Ar ea SWS, South W est ern S y dney Ar ea JHS, Justic
e Health S
e
rvic
e
Communicable Diseases Report
T
a
ble 2.
Repor
ts of notifiable c
o
nditions r
e
ceiv
ed in Dec
ember 2008 b
y
ar
ea health ser
v
ic
es
Ar
ea Health S
e rv ic e (2008) Hunt er Nor thern S y dne y South East ern S y dne y South To tal Gr ea te r Southern Gr ea te r W e st ern N ew England Nor th C o ast C entr al C o ast S y dne y I lla w a rr a W est S y dne y W e st F o r Y ear C o ndition GMA S A F W A MA C M W A HUN N EA MNC N R A C C A NSA ILL SES C SA SWS WEN WSA JHS Dec ember b to d a te b
Bloodborne and se
xually tr ansmitt e d Chancr o id a –– ––– – – – – – – – – – – – – – – – Chlam y d ia (genital) a 42 32 6 1 3 2 8 7 8 4 5 2 6 2 9 6 6 – 63 192 102 74 22 86 7 919 13956 G o norrhoea a 3 – 1 1 – 3 – – 2 2 – 1 42 17 6 1 12 – 9 4 1360
Hepatitis B – acut
e viral a –– ––– – – – – – – – – 1 – – – 1 2 4 1
Hepatitis B – other
a 3 3 – – – 4 – – 1 1 – 4 2 8 1 7 2 2 – 20 3 107 2802
Hepatitis C – acut
e viral a 1– ––– 1 – – – – – – – – – – – – 2 2 4
Hepatitis C – other
a 13 9 2 4 3 26 7 1 9 1 2 1 1 – 27 31 12 31 3 1 4 2 5 251 4902
Hepatitis D – unspecified
a –– ––– – – – – – – – – – – – 1 – 1 1 4 Ly mphogranuloma v aner e um – – – – – – – – – – – – – – – – – – – – S y philis 1 1 1 – – 2 – 1 – 2 3 4 3 7 1 6 3 – 6 – 7 8 1077 V e c torborne Barmah F o rest virus a 1 2 – 1 – 7 – 8 8– –– –– – – – – 2 7 5 4 9 Ross R iv e r virus a 9 1 1 6 1 13 6 4 4 2 – 2 – – 1 2 – – 49 1173 Arbo viral inf ec tion (other) a –– ––– – 1 – – – 1 1 2 2 – 1 – – 8 1 5 3 M alaria a –– ––– 1 – – – – 1 4 2 2 – 1 2 – 1 3 1 1 7 Z o onoses Anthrax a –– ––– – – – – – – – – – – – – – – – Bruc ellosis a –– ––– – – – – – – – – – – – – – – 3 Le pt ospir o sis a –– ––– – – – – – – – – – – – – – – 1 8 Ly ssa virus a –– ––– – – – – – – – – – – – – – – – P sittac o sis a –– –– 1 – – – –– –– –– – – – – 1 4 1 Q f e v e r a –– 1–– – 5 4 2 – – 1 – – – – – – 1 3 1 6 9 Respir a to ry and other
Blood lead lev
e l a – – –11 5 1 – – – –1 –1 – – – – 1 0 2 4 6 Influenza a 2 5 1 1 2 6 – – 2 2 – 4 1 4 7 7 6 21 – 8 0 1913 In v a siv e pneumoc o ccal inf ec tion a 1 1 – – 2 7 1 1 – 2 2 3 – 2 4 1 6 – 33 532 Legionella longbeachae inf ec tion a –– ––– 1 – – – – – – 1 – 1 1 1 – 5 4 7 Legionella pneumophila inf ec tion a –– ––– 1 – – – – 1 – 1 – – 1 2 – 6 3 9 Le gionnair es
’ disease (other)
a –– ––– – – – – – – – – – – – – – – 1 Le p ro sy – –– – – – – – – –– – – –– – – – – 3 M e ningoc occal inf ec tion (in v a siv e ) a –– ––– – – – 1 – – 1 1 1 – – – – 4 7 9 Tu ber culosis – – – – – 2 – – 1 – 2 – 9 1 – – – – 15 458 V a ccine-pr e v e ntable A d v e rse ev ent af te r immunisation – – – – – – 2 – – – – 1 1 – 2 – – – 6 263 H . influenzae b inf ec tion (in v a siv e ) a –– ––– – – – – – – – – – – – – – – 9 M e a sl e s – –– – – – – – – –– – – –– – – – – 3 9 Mumps a –– ––– – – – – – 1 – 1 1 1 – – – 4 8 9 P e rtussis 7 8 3 6 9 26 20 105 15 35 152 141 217 274 265 93 126 150 246 1 1989 8181 Rubella a –– ––– – – – – – 1 – – – – – – – 1 1 7 Te ta n u s – –– – – – – – – –– – – –– – – – – 1 En te ric B o tu li sm – –– – – – – – – –– – – –– – – – – – Cholera a –– ––– – – – – – – – – – – – – – – 2 Cr ypt o sporidiosis a –– –– 5 1 4 – 3 3 –– 4– 3 1 – – 2 4 4 8 8 Giar diasis a 2 5 – 1 2 1 8 – 1 – 9 1 7 2 3 1 0 5 5 6 – 9 5 1787
Haemolytic uraemic syndr
o me – – – 1 – 1 – – – – 1 – – 1 1 – 1 – 6 1 7 Hepatitis A a –– ––– – – – – – – – – – 1 1 1 – 3 6 4 Hepatitis E a –– ––– – – – – – – – – – 1 – – – 1 1 5 List e riosis a –– ––– – – – – – 1 – – – – 1 – – 2 3 4 Salmonellosis a 5 5 – 2 2 3 8 8 6 1 4 2 2 3 7 8 20 15 16 3 2 6 – 230 2251 Shigellosis a – 1 ––– – – – – – 1 – 3 3 1 – 1 – 1 0 1 0 7 Ty phoid a –– ––– – – – – – – – – 1 – – – – 1 3 9 V e ro to xin pr oducing E. coli a –– ––– 1 – – – – – – – – – – – – 1 1 3 M isc ellaneous Cr eutzf e ldt–Jakob disease – – – – – – – – – – – – – – 1 – – – 1 3 M e ningoc occal c o njunc tivitis – – – – – – – – – – – – – – – – – – – 1 aLaborat or y-c
onfirmed cases only
.
bIncludes cases with unk
n o w n post co de . NB: Data ar e curr
ent and accurat
e
as at the pr
eparation dat
e
. T
h
e number of cases r
e por ted is , ho w e v e r, subjec t t o change
, as c
ases ma
y be ent
e
red at a lat
e r dat e or r e trac
ted upon fur
ther in
v
estigation.
Hist
orical Ar
ea Health S
e rvic e c o nfigurations ar e included f o r c o ntinuit y/ co
mparison purposes and t
o highlight r e gional diff er enc e s. NB: F
rom 1 Januar
y 2005,
Hunt
er New England AHS also c
o mprises Gr eat Lak es , Glouc est
er and Gr
eat e r Ta ree L G A s (L GA, L o cal G o v e rnment Ar ea), S y dney W
est also c
o mprises Gr eat e r Lithgo w L G A. NB:
HIV and AIDS data ar
e r
e
por
ted separat
ely in the P
u
blic Health Bulletin quar
te rly . GMA, Gr eat e r Murra y Ar ea MA C, M a cquarie Ar ea NEA,
New England Ar
ea C C A, C e ntral C o ast Ar ea SES, South East ern S y dney Ar
ea WEN,
W e ntw o rt h Ar
ea SA,
Southern
Ar
ea MW
A, M id W est ern Ar
ea MNC,
Nor th C o ast Ar ea. NSA, Nor thern S y dney Ar
ea CSA,
C e ntral S y dney Ar
ea WSA,
W est ern S y dney Ar
ea FW
A, F ar W est Ar ea HUN, Hunt er Ar ea NRA, Nor thern R iv e rs Ar ea ILL, I lla warra Ar ea SWS, South W est ern S y dney Ar ea JHS, Justic
e Health S
e
rvic
e