Assessment of Malnutrition Status in Hemodialysis
Patients
Doaa S. D. Zaki1,*, Ragaa R. Mohamed1, Nagwa A. G. Mohammed2, Rania B. Abdel-Zaher3 1
Internal Medicine Department, Faculty of Medicine, Al-Azhar University, Cairo, Egypt 2
Clinical and Chemical Pathology Department, National Research Center 3
Nephrology Unit, Helwan General Hospital, Cairo, Egypt
Abstract
Background: Malnutrition in hemodialysis (HD) patients is prevalent worldwide. However, data regarding the nutritional status of those patients among Arab countries is insufficient. Objectives: The purpose of this study was to estimate the prevalence of malnutrition among adult HD patients in Cairo, Egypt and to investigate the possible factors correlating with malnutrition in those patients. Patients and methods: This was a prospective cross-sectional observational study that conducted at 2 dialysis units in Cairo, Egypt. Patients were evaluated for the nutritional status by using modified subjective global assessment (mSGA). Biochemical and hematological parameters were collected pre-dialysis. Results: A total of 100 patients with ESRD on regular HD for more than 6 months (64% males and 36% females) were included in the study. Their mean age was 50.2 ± 12.5 years and the primary cause of ESRD was hypertension in 45% and diabetes in 34%. The prevalence of malnutrition was 67% according to the reference standard mSGA; either mildly-moderately malnourished (50%) or severely malnourished (17%). The mSGA score was positively correlated to age, duration of HD, and CRP and negatively correlated with albumin in HD patients. Conclusion: Malnutrition was highly prevalent among HD patients in Cairo, Egypt. Therefore, there is a need for adequate nutritional assessment early in starting of hemodialysis and tailored nutritional plan to minimize the consequences of malnutrition on the patients and health care system.Keywords
Hemodialysis, Prevalence, Malnutrition1. Introduction
Malnutrition refers to a state of over-nutrition or undernutrition of macronutrients elements or specific micronutrient needs, which are critical to tissues [1]. Malnutrition is a common problem in patients with end stage renal disease (ESRD) undergoing hemodialysis (HD) that is associated with increased morbidity and mortality [2]. The pathogenesis of malnutrition in patient with HD is multifactorial. Inadequate food intake due to anorexia and altered taste sensation combined with intercurrent illness, hyper-catabolism and reduced anabolism, dialysis procedure, chronic inflammatory state, and endocrine disorders of uraemia were reported as major causes of malnutrition in MHD [3, 4]. The prevalence of malnutrition in HD patients varies widely, ranging from 16% to 62% depending on the study subjects and assessment methods [5, 6, 7, 8]. It is advocated that early detection of malnutrition will facilitate early and comprehensive nutritional support, effective
* Corresponding author:
dsalah241@azhar.edu.eg (Doaa S. D. Zaki) Published online at http://journal.sapub.org/cmd
Copyright©2019The Author(s).PublishedbyScientific&AcademicPublishing This work is licensed under the Creative Commons Attribution International License (CC BY). http://creativecommons.org/licenses/by/4.0/
management and prevention of the associated negative clinical outcomes for malnutrition [9].
Various methods have been used to evaluate the nutritional state of HD patients. Among these methods, subjective global assessment (SGA) is widely used representative tool for nutritional screening. It is also recommended by national kidney foundation in CKD patients [10, 11]. The SGA is a specific, inexpensive, simple and clinically confident screening tool of malnutrition in hemodialysis patients [12]. Using components of conventional SGA, a fully quantitative scoring system consisting of 7 components with total score ranging between 7 (normal) and 35 (severely malnourished), has been developed and named as modified subjective global assessment score (mSGA) [13]. The aim of the current study was to estimate the prevalence of malnutrition among HD adult patients by using mSGA to gain an insight into this problem in Egypt.
2. Patients and Methods
2.1. Study Participants
dialysis unit at Military Production hospital. The study was carried out over a period of about one year; from January 2014 to February 2015. The study includes 100 patients with ESRD aged ≥ 18 years old on regular HD three-times a week for at least six months. The sample size was calculated by using equation in the Raosoft software package according to annual flow on dialysis units with accepted margin of error 5% and the confidence level 95%.
Informed consent was obtained from all study participants in advance. All procedures were performed in accordance with the guidelines in the Declaration of Helsinki and approved by Research Ethics Committee of Faculty of Medicine for Girls, Al-Azhar University. Patients with Acute kidney injury, Active malignancy, Active infection, primary parathyroid disease and primary bone disease were excluded from the study. All patients were subjected to a standardized questionnaire including: age, gender, medical history, primary cause of CKD, duration of dialysis and comorbidities. Physical examination was done with special emphasis to height/m, weight/kg and resting blood pressure. Body mass index (BMI) was calculated using the following equation: BMI = weight (kg) divided by the square of the height (m).
2.2. Nutritional Assessment
As a reliable and valid tool for the nutritional assessment of patients on HD; mSGA was used to assess nutritional status of the HD patient via a questionnaire which includes data on weight change, dietary intake, gastrointestinal symptoms, functional capacity, comorbidity, subcutaneous fat and signs of muscle wasting. Each component has 5 levels of severity to calculate a score between 7 (normal) and 35 (severely malnourished) [13]. Patients with mSGA score from 7-10 are considered well nourished, from 11 to 20 are considered mild to moderate malnourished and from 21 to 35 are considered severely malnourished.
2.3. Laboratory Study
Biochemical and hematological parameters were collected pre-dialysis. Hemoglobin concentration was performed by Coulter Counter T890 (Coulter Counter, Harpenden, UK). Serum albumin, urea, creatinine, calcium, total cholesterol (TC) and triglyceride (TG) were carried out on Dimension RxL Max analyzer (Siemens Healthcare GmbH - Henkestr. 127, 91052 Erlangen, Germany) by colorimetric techniques. For detection of high-density lipoprotein (HDL), phosphortungestic acid and magnesium ions were used for precipitating lipoproteins except HDL fraction that was present in the supernatant and measured by auto analyzer. Low-density lipoprotein (LDL) was measured by Friedwald formula [14]. CRP was measured by turbidimetry [15] with a Cobas 6000 analyzer (Roche Diagnostics, USA). Serum magnesium was determined by using flame atomic absorption spectrophotometer (AA-630-12) (Schimadzu Europe, GmbH, Albert-Hahn-Strasse 6-10, Germany).
2.4. Statistical Methods
Data collected was reviewed, coded and statistically analyzed using Statistical Package for the Social Science (SPSS) program version 20 (Inc, Chicago, Illinois, USA). Data was described in terms of mean ± standard deviation (±SD) for continuous variables and percentage for categorical variables. Chi square-test (χ2) was used for the comparison of qualitative data, however, Student’s T test and one-way analysis of variance (ANOVA) were used for the comparison between groups as regard to quantitative data. Pearson‘s correlation coefficient (r) test was used to assess possible association between variables. The confidence interval was set to 95% and the margin of error accepted was set to 5%. So, the probability of error 0.05 was considered significant and 0.001 was considered as highly significant.
3. Results
Table 1. Demographic characteristics and laboratory data of the studied
HD patients
Variables HD patients n= 100 Age/years 50.2 ± 12.5 Male gender 64% Duration of hemodialysis/months 40.1 ± 31.5
Causes of ESRD Hypertension
Diabetes Primary renal disease
Idiopathic Autoimmune disease
45% 34% 18% 14% 4% BMI (kg/m²) 27.2 ± 4.3
mSGA 13.6 ± 5.0 Hb (g/dl) 9.93 ± 1.53 CRP (mg/l) 19.0 ± 5.3 Urea (g/dl) 123.84 ± 37.33 Creatinine (g/dl) 7.88 ± 2.42
Albumin (g/dl) 3.64 ± 0.70 Calcium (mg/dl) 9.04 ± 1.15 Phosphorus (mg/dl) 5.21 ± 1.72 Magnesium (mg/dl) 1.36 ± 0.20 Cholesterol (mg/dl) 153.19 ± 40.50 Triglyceride (mg/dl) 131.35 ± 46.17 HDL (mg/dl) 38.81 ± 13.16 LDL (mg/dl) 109.41 ± 21.04
BMI: body mass index; CRP: C-reactive protein; Hb: hemoglobin: HDL: high density lipoprotein; LDL: low density lipoprotein: mSGA: modified subjective global assessment.
characteristics and the laboratory data of all patients were represented by table (1). The data were expressed by mean± SD or percent as needed.
The most common primary causes of ESRD were hypertension (45%) and diabetes (34%). Regarding laboratory investigations that related to the nutritional status of the patients; mean Hb level was low (9.93 ± 1.53 g/dl) but mean albumin and total cholesterol were within normal range. As regard to lipid profile that reflect the cardiovascular risk; mean HDL was low (38.81 ± 13.16 g/dl)
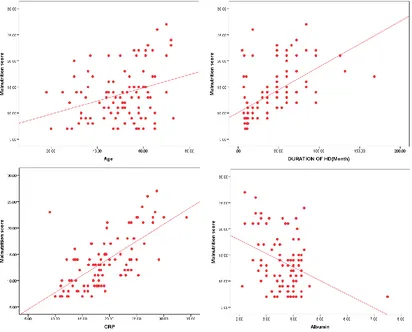
and mean LDL was high (109.41 ± 21.04 g/dl). The inflammatory state assessed by CRP was also high (19.0 ± 5.3). The mSGA score was positively correlated to age (r=0.276), duration of HD (r=0.610), and CRP (0.684) and negatively correlated to albumin in HD patients P < 0.001 (figure 1).
The prevalence of malnutrition in HD patients was 67% according to the reference standard mSGA; either mildly-moderately malnourished (50%) or severely malnourished (17%) (Figure 2).
Figure 1. Correlation between mSGA and age, duration of hemodialysis, CRP and albumin in HD patients
Figure 2. Nutritional status of the HD patients according to mSGA
33.0%
50.0% 17.0%
Well-nourished patients
Mild to moderate malnutrition
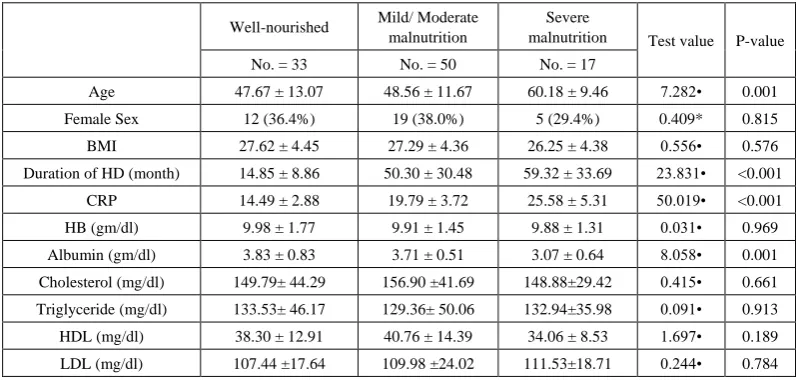
Table 2. Clinical characteristics and laboratory data of the studied HD patients according to nutritional status by mSGA
Well-nourished Mild/ Moderate malnutrition
Severe
malnutrition Test value P-value No. = 33 No. = 50 No. = 17
Age 47.67 ± 13.07 48.56 ± 11.67 60.18 ± 9.46 7.282• 0.001 Female Sex 12 (36.4%) 19 (38.0%) 5 (29.4%) 0.409* 0.815 BMI 27.62 ± 4.45 27.29 ± 4.36 26.25 ± 4.38 0.556• 0.576 Duration of HD (month) 14.85 ± 8.86 50.30 ± 30.48 59.32 ± 33.69 23.831• <0.001
CRP 14.49 ± 2.88 19.79 ± 3.72 25.58 ± 5.31 50.019• <0.001 HB (gm/dl) 9.98 ± 1.77 9.91 ± 1.45 9.88 ± 1.31 0.031• 0.969 Albumin (gm/dl) 3.83 ± 0.83 3.71 ± 0.51 3.07 ± 0.64 8.058• 0.001 Cholesterol (mg/dl) 149.79± 44.29 156.90 ±41.69 148.88±29.42 0.415• 0.661 Triglyceride (mg/dl) 133.53± 46.17 129.36± 50.06 132.94±35.98 0.091• 0.913 HDL (mg/dl) 38.30 ± 12.91 40.76 ± 14.39 34.06 ± 8.53 1.697• 0.189 LDL (mg/dl) 107.44 ±17.64 109.98 ±24.02 111.53±18.71 0.244• 0.784
BMI: body mass index; CRP: C-reactive protein; Hb: hemoglobin: HDL: high density lipoprotein; LDL: low density lipoprotein: mSGA: modified subjective global assessment; *: Chi-square test; •: One Way ANOVA test.
To compare differences within HD patients according to their nutritional status (as revealed by mSGA scores); table 2 shows that there was significantly increased age in severely malnourished patients as compared to mild/moderate and well-nourished patients. Among other clinical characteristics, only duration of hemodialysis showed a significant gradual increase with severity of malnutrition (p < 0 .001).
As regard to inflammatory markers; CRP was significantly higher, and albumin was significantly lower in patients with severe malnutrition as compared to mild to moderate and well-nourished patients (P < 0.05 and P < 0.001 respectively). As regard to lipid profile; no significant differences were founded between patients according to malnutrition.
4. Discussion
Malnutrition is common and associated with increased morbidity and mortality in HD patients [16]. Only a few studies have been published about the prevalence of malnutrition among HD patients in Egypt. Nutritional status is frequently ignored in many dialysis centers while simple methods of nutritional assessment could have a favorable impact on patient management. In the present study; the prevalence of malnutrition among HD patients (n=100) was 67% (50% were mild to moderate malnourished and 17% were severe malnourished). These results were lower than the prevalence reported by similar study among HD patients in Egypt (Assuite city) which revealed about 85% malnourished patients (81.6% mild to moderate malnutrition and 3.6% severe malnutrition) [17]. This difference can be explained by lower educational level, socioeconomic state and health care facilities in south Egypt area compared to the capital city. However, our results were comparable with findings of other study in Jordan, that reported 61.8% malnutrition rate among 178 patients undergoing HD [18].
Another study was done in Saudi Arabia 2018 that revealed 57% of HD patients were malnourished according to SGA (49% were undernourished and 18% were severely malnourished) [19]. These differences in prevalence may be due to environmental diversity and different diet regiments in various regions of the middle east area.
In the current study, hypertension and DM showed up as being most common causes of ESRD (45% and 34% respectively). Presence of chronic disease with polypharmacy can be another cause of increased prevalence of malnutrition in HD patients [20].
In the present study, mSGA was positively correlated to age of HD patients as well as the duration of hemodialysis. The role of age in malnutrition was emphasized in some studies; where younger patients had better nutritional state than elderly patients [21]. The nutritional status of the elderly affected by increased catabolism of muscle protein, loss of body fat, eating difficulties, and low activity of daily living [22]. Furthermore, the long duration of hemodialysis is another factor that affect nutritional status of the HD patient [23].
status, dialysis losses, and acidemia [27].
In the present study, albumin level was gradually decreased as malnutrition increases being lowest in severely malnourished patients. Moreover, serum albumin shows significant negative correlation with mSGA score. However, serum albumin has low sensitivity and specificity for evaluating malnutrition status in HD patients [28]. As regard HB concentration, no significant correlation with malnutrition by mSGA has been founded. Many factors can affect Hb level in HD patients such as reduced erythropoietin production, hyperparathyroidism, acute and chronic inflammatory conditions, aluminum toxicity and reduced lifespan of red blood cells. High-amplitude fluctuation in Hb level predicts high mortality in HD patients [29]. Among electrolytes studied in the present study, serum magnesium was decreased, which was related with malnutrition and inflammatory marker (CRP). Lower serum magnesium is known as a risk factor of CV mortality [30] and serum magnesium levels > 2.10 mEq/L were associated with better survival in HD patients [31].
Regarding lipid profile, there were no significant difference between all groups of HD patients in TC, TG, HDL or LDL. Cholesterol level as an indicator of energy-protein status is insensitive, unspecific, and affected by other factors such as inflammation [32]. Bioimpedance vector analysis (BIVA) is a non-invasive, low cost and a commonly used approach for body composition measurements and assessment of clinical condition [33]. BIVA assess the state of nutrition and hydration in patients with dialysis and when combined with nutritional assessment and malnutrition inflammatory score can diagnose protein energy wasting syndrome in patients with dialysis [34]. Two centre study in a capital city has been considered as a limitation in this research. Multicentre studies with large sample size from different cities in Egypt was recommended.
5. Conclusions
Malnutrition was highly prevalent among HD patients in Cairo, Egypt. Therefore, development of nutritional assessment protocols for HD is an important issue and needs to be followed up by health-care teams in HD centres. The administration of the SGA as a well-validated, feasible, inexpensive and non-invasive nutritional screening tool can ensure an accurate evaluation of the nutritional status routinely in HD patients.
REFERENCES
[1] Cantürk, N.Z. and Şimşek, T. Basic aspects of nutrition: Effects of malnutrition, nutritional assessment, macro and micronutrients, determination of nutritional support. T Klin J Anest Reanim, 2010, 3, 1-17.
[2] Bossola, M., Muscaritoli, M., Tazza, L., Giungi, S., Tortorelli, A., Rossi Fanelli, F. and Luciani, G. Malnutrition in hemodialysis patients: what therapy? Am J Kidney Dis, 2005, 46, 371-86.
[3] Sharma, R.K. and Sahu, K.M. Nutrition in dialysis patients. J Indian Med Assoc., 2001, 99 (4), 206-8, 210-1, 213. [4] Moncef, E., Kadiri, M.B., Nechba, R.B. and Oualim, Z.
Factors predicting malnutrition in hemodialysis patients. Saudi J Kidney Dis Transpl, 2011, 22 (4), 695-704.
[5] Rezeq, H.A., Khdair, L.N., Hamdan, Z.I. and Sweileh, W.M. Prevalence of malnutrition in hemodialysis patients: A single-center study in Palestine. Saudi J Kidney Dis Transpl., 2018, 29(2), 332-340.
[6] Espahbodi, F., Khoddad, T. and Esmaeili, L. Evaluation of malnutrition and its association with biochemical parameters in patients with end stage renal disease undergoing hemodialysis using subjective global assessment. Nephrourol Mon., 2014, 6 (3), e16385.
[7] Barker, L.A., Gout, B.S. and Crowe, T.C. Hospital malnutrition: prevalence, identification and impact on patients and the healthcare system. Int J Environ Res Public Health, 2011, 8(2), 514-27.
[8] Kopple, J.D. and McCollum, A. Protein-energy malnutrition in maintenance dialysis patients. Am J Clin Nutr, 1997, 65, 1544–1557.
[9] Weekes, C.E., Spir, A., Baldwin, C., Whelan, K., Thomas, J.E., Parkin, D. and Emery, P.W. A review of the evidence for the impact of improving nutritional care on nutritional and clinical outcomes and cost. J Hum Nutr Diet, 2009, 22, 324-335.
[10] Fouque, D., Kalantar-Zadeh, K., Kopple, J., Cano, N., Chauveau, P., Cuppari, L., Franch, H., Guarnieri, G., Ikizler, T.A., Kaysen, G., Lindholm, B., Massy, Z., Mitch, W., Pineda, E., Stenvinkel, P., Treviño-Becerra, A. and Wanner, C.A. proposed nomenclature and diagnostic criteria for protein-energy wasting in acute and chronic kidney disease. Kidney Int., 2008, 73, 391–398.
[11] Enia, G., Sicuso, C., Alati, G. and Zoccali, C. Subjective global assessment of nutrition in dialysis patients. Nephrol Dial Transplant, 1993, 8(10), 1094-8.
[12] Sum, S.S., Marcus, A.F., Blair, D., Olejnik, L.A., Cao, J., Parrott, J.S., Peters, E.N., Hand, R.K. and Byham-Gray, L.D. Comparison of Subjective Global Assessment and Protein Energy Wasting Score to Nutrition Evaluations Conducted by Registered Dietitian Nutritionists in Identifying Protein Energy Wasting Risk in Maintenance Hemodialysis Patients. J Ren Nutr., 2017, 27(5), 325-332.
[13] Kalantar-Zadeh, K., Kleiner, M., Dunne, E., Lee, G.H. and Luft, F.C. A modified quantitative subjective global assessment of nutrition for dialysis patients. Nephrol Dial Transplant, 1999, 14 (7), 1732-8.
[14] Friedwald, W.T., Levy, R.I. and Fredrickson, D.S. Estimation of the concentration of low-density lipoprotein cholesterol in plasma without use of the preparative ultracentrifuge. Clin Chem, 1972, 18, 499-502.
protein based on phosphocholine interaction, Clin Chem Lab Med, 2009, 47(11), 1417-22.
[16] Kalantar-Zadeh, K., Ikizler, T.A., Block, G., Avram, M.M., Kopple, J.D. "Malnutrition-inflammation complex syndrome in dialysis patients: causes and consequences." American Journal of Kidney Diseases, 2003, 42(5), 864-881.
[17] Abozead, S.E.S., Ahmed, A.M., Mahmoud, M.A. Nutritional Status and Malnutrition Prevalence among Maintenance Hemodialysis Patients. IOSR-JNHS, 2015, 4(4), 51-54. [18] Tayyem, R.F. and Mrayyan, M.T. Assessing the prevalence
of malnutrition in chronic kidney disease patients in jordan. J Ren Nutr, 2008, 18(2), 202-9.
[19] Ali-Bokhari, S.R., Faizan-Ali, M.A., Khalid, S.A., Iftikhar, B., Ahmad, H.I., Hussain, A.S., Yaqoob, U. The development of malnutrition is not dependent on its traditional contributing factors in patients on maintenance hemodialysis in developing countries. Saudi J Kidney Dis Transpl, 2018, 29(2), 351-360.
[20] Parmar, M.S. Chronic renal disease. BMJ, 2002, 325, 85-90. [21] Segall, L., Mardare, N.G., Ungureanu, S., Busuioc, M., Nistor,
I., Enache, R., Marian, S. and Covic, A. Nutritional status evaluation and survival in haemodialysis patients in one centre from Romania. Nephrol Dial Transplant, 2009, 24, 2536-40.
[22] Rodrigues, J., Cuppari, L., Campbell, K.L. and Avesani, C.M. Nutritional assessment of elderly patients on dialysis: pitfalls and potentials for practice. Nephrol Dial Transplant, 2017, 32(11), 1780-1789.
[23] Alvarenga, L.A., Andrade, B.D., Moreira, M.A., Nascimento, R.P., Macedo, I.D. and Aguiar, A.S. Nutritional profile of hemodialysis patients concerning treatment time. J Bras Nefrol, 2017, 39(3), 283-286.
[24] Iorember, F.M. Malnutrition in Chronic Kidney Disease. Front Pediatr, 2018, 6, 161.
[25] Ruperto, M., Sánchez-Muniz, F.J. and Barril, G. Predictors of protein-energy wasting in haemodialysis patients: a cross-sectional study. J Hum Nutr Diet, 2014, 29(1), 38-47. [26] Kizil, M., Tengilimoglu-Metin, M.M., Gumus, D., Sevim, S.,
Turkoglu, İ. and Mandiroglu, F. Dietary inflammatory index is associated with serum C-reactive protein and protein energy wasting in hemodialysis patients: A cross-sectional study. Nutr Res Pract, 2016, 10(4), 404-10.
[27] Kopple, J.D. National kidney foundation K/DOQI clinical practice guidelines for nutrition in chronic renal failure. Am J Kidney Dis., 2001, 37 (2), S66-70.
[28] Stosovic, M.D., Naumovic, R.T., Stanojevic, M.L.j., Simic-Ogrizovic, S.P., Jovanovic, D.B., Djukanovic, L.D. Could the level of serum albumin be a method for assessing malnutrition in hemodialysis patients? Nutr Clin Pract., 2011, 26(5), 607-13.
[29] Bal, Z., Demirci, B.G., Karakose, S., Tutal, E., Erkmen-Uyar M., Acar, N.O. and Sezer, S. Factors Influencing Hemoglobin Variability and Its Association with Mortality in Hemodialysis Patients. Scientific World Journal, 2018, Article ID 8065691, 7 pages.
[30] Yu, L., Li, H. and Wang, S.X. Serum Magnesium and Mortality in Maintenance Hemodialysis Patients. Blood Purif, 2017, 43 (1-3), 31-36.
[31] Lacson, E. Jr., Wang, W., Ma, L., Passlick-Deetjen, J. Serum Magnesium and Mortality in Hemodialysis Patients in the United States: A Cohort Study. Am J Kidney Dis., 66 (6), 2015, 1056-66.
[32] Chmielewski, M., Verduijn, M., Drechsler, C., Lindholm, B., Stenvinkel, P., Rutkowski, B., Boeschoten, E.W., Krediet, R.T., Dekker, F.W. Low cholesterol in dialysis patients--causal factor for mortality or an effect of confounding? Nephrol Dial Transplant. 2011, 26 (10), 3325–31.
[33] Khalil S.F., Mohktar M.S., Ibrahim F. The theory and fundamentals of bioimpedance analysis in clinical status monitoring and diagnosis of diseases. Sensors (Basel). 2014, 19, 14(6), 10895-928.