Received for publication Jul 25, 1990; accepted Dec 5, 1990. PEDIATRICS (ISSN 0031 4005). Copyright © 1991 by the American Academy of Pediatrics.
Early
Formula
Supplementation
of
Breast-Feeding
Natalie
Kunnij,
PhD,*
and Patricia
H. Shiono,
PhDf
From the *Collaborative Clinical Research Branch, National Eye Institute, National
Institutes of Health, Bethesda, Maryland, and tCenter for the Future of Children, David
and Lucille Packard Foundation, Los Altos, California
ABSTRACT. Factors influencing early formula
supple-mentation in breast-fed neonates were examined among
726 women who were delivered of their first child in one
ofthree metropolitan Washington, DC, hospitals. Thirty-seven percent of breast-fed neonates were given supple-mentary formula in the hospital. Mothers who gave birth at a university hospital were more likely to breast-feed
exclusively (adjusted odds ratio 3.5; 95% confidence limit 2.1 to 5.9), after adjustment for maternal demographics, hospital factors (such as time of first breast-feed, demand feeding, delivery type, and rooming-in), and the maternal breast-feeding commitment. Aside from delivery hospital,
a strong predictor of formula use was the time between birth and initiation of the first breast-feed. The longer a mother waited to initiate breast-feeding the more likely
she was to use formula; the adjusted odds ratios for
women who initiated breast-feeding 2 to 6 hours, 7 to 11 hours, and 12 or more hours postpartum were 1.1, 0.5,
and 0.2, respectively. Feeding the baby on demand, hay-ing a vaginal delivery, deciding to breast-feed before
pregnancy, having a college education, and being married also were moderately, though significantly, predictive of
exclusive breast-feeding. The findings suggest that hos-pital influences can promote formula use and indirectly
shorten breast-feeding duration, particularly those
hos-pital practices that delay early initiation of
breast-feed-ing. Pediatrics 1991;88:745-750; breast-feeding, infant for-mula, supplementation.
Formula supplementation of breast-feeding has been consistently associated with a shortened
breast-feeding duration.’5 Although a causal
rela-tionship between formula use and discontinuation
of breast-feeding is difficult to establish, women who use formula supplements tend to breast-feed for a shorter time period than women who do not.’4 Moreover, women who introduce formula in
the early postpartum weeks have a higher rate of
breast-feeding discontinuation than women who
introduce formula in the later postpartum months.6 What remains unclear are the factors responsible for formula-supplemented breast-feeding, particu-larly formula use occurring in the early postpartum period. Formula supplementation may result from a maternal intention to stop breast-feeding, may be due to hospital influences (both staff and routines), or may reflect a lack of maternal confidence in
breast-feeding. The underlying cause of maternal
confidence in and commitment to breast-feeding are not easily understood; however, a hospital staff supportive of breast-feeding can bolster maternal confidence in the method.7 In contrast, hospital routines that restrict early initiation of breast-feed-ing by separating the mother from hen newborn after delivery can promote formula use. This sepa-ration thereby indirectly promotes a shortened du-ration of breast-feeding, if supplements replace breast milk.
We previously reported from a prospective survey of 755 breast-feeding women that 38% of neonates received formula supplements during the hospital
stay-a factor strongly predictive of a shortened
breast-feeding duration.’ In this paper we examine
maternal and hospital factors that might explain
why so many neonates of breast-feeding women are given supplementary formula. In particular, we
evaluate the influence of maternal
sociodemo-graphic characteristics, commitment to breast-feed, and the effect of specific hospital procedures on early formula use.
METHODS
were consecutively selected from the delivery logs at each of three metropolitan Washington, DC,
hospitals. Study procedures and the study design
have been described.1 To summarize, a total of 1409
women were asked to participate in the study and
84% (n = 1179) agreed. Women were interviewed
in the hospital between February 1984 and March
1985, after informed consent was obtained.
Sixty-four percent of the sample women initiated any
breast-feeding in the hospital.
Of the 755 women who breast-fed in the hospital,
29 women had not fed their newborn at the time of
the interview and were excluded from the present
analysis. Of the remaining 726 women, 456 (63%)
exclusively breast-fed. These 456 women defined
themselves as exclusively breast-feeding and
mdi-cated that the baby had not received formula
sup-plements in the hospital. Mixed feeders (n = 270)
were categorized based on their actual infant
feed-ing behavior in the hospital. Mixed feeders defined
themselves as simultaneously breast-feeding and
formula feeding (n = 100) on as exclusively
breast-feeding but indicated that the baby had received
formula in the hospital (n = 170). Categorization
of exclusive breast-feeders and mixed feeders was
based solely on maternal reports of the infant’s
being given supplementary formula. This formula
supplementation could have resulted from maternal choice on from hospital procedures. Definition of
feeding type did not take into consideration the
amount of formula offered to the neonate.
The following information was obtained during the hospital interview: maternal sociodernographic characteristics (age, education, marital status, net
family income, prenatal cane, and attendance in
childbirth classes); breast-feeding and
formula-feeding behavior; hospital procedures (delivery
type, timing of the first breast-feed, rooming-in,
and feeding pattern-demand, modified demand, or
schedule); and maternal commitment to breast-feed
(timing of decision to breast-feed and planned
du-nation of breast-feeding). The first maternal
re-sponse to an open-ended question regarding why
formula supplements were used was also examined. Eligible women were recruited consecutively for
4#{189}months at the public hospital, 13 months at the
community hospital, and 1 1 months at the
univer-sity hospital. Ninety percent of women were
inter-viewed during their hospital stay or in their baby’s
first 4 days of life. Because of an early discharge policy, 10% of women were not seen in the hospital
but were subsequently interviewed at home. No baby was older than 17 days at time of the first
interview.
The sociodemographic characteristics of
exclu-sive breast-feeders and mixed feeders were
evalu-ated by
x2
analysis.8 Logistic regression was usedto estimate the odds ratio for exclusive
breast-feeding vs mixed feeding while controlling for de-mographic factors, hospital procedures, and mater-nal commitment to breast-feed.9
RESULTS
Sixty-three percent of women (n = 726)
breast-fed without the use of formula supplements in the
hospital. Demographic predictors of exclusive
breast-feeding are presented in Table 1. The rate ofexclusive breast-feeding exceeded the overall rate
of 63% among women giving birth at the university hospital (86%), those with a college (65%) or
grad-uate school (75%) education, white women (74%),
married women (69%), those older than age 30
(71%), those receiving prenatal care from a private
physician (64%) on a health maintenance
organi-zation (85%), and those attending childbirth classes (65%). In the multivaniate model (Table 1) adjust-ing for education, ethnicity, marital status, age, type of prenatal care, and attendance in childbirth
classes, the strongest predictor of exclusive
breast-feeding vs mixed feeding was delivery at the
uni-vensity hospital (adjusted odds 3.5, 95% confidence
interval [CI] 2.1 to 6.0). The adjusted odds of
exclu-sive breast-feeding vs mixed feeding also were
sig-nificantly increased, approximately twofold, for
women having at least some college vs a high school
education, for white vs black women, and for those who were married (Table 1).
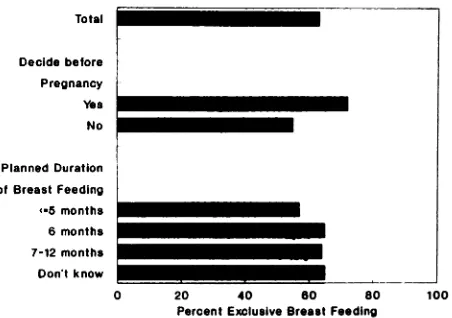
The associations between hospital factors, the
maternal commitment to breast-feed, and the
ex-clusive breast-feeding rate are presented in Figs 1 and 2. The rate of exclusive breast-feeding was higher than the overall proportion of 63% if the
women initiated breast-feeding in the first 6 hours
postpartum, if she delivered vaginally, or if she fed on demand (Fig 1). Rooming-in did not have an effect on exclusive breast-feeding (not shown). Women who decided to breast-feed before rather than during or after pregnancy were significantly
more likely to breast-feed exclusively, whereas
planned duration of breast-feeding
did
not affect the exclusive breast-feeding rate (Fig 2).We also evaluated the first maternal response to an open-ended question regarding why formula sup-plements were used (Table 2). The primary reasons given (n = 267) were “to give mother some nest”
(20%) or “mother ill” (18%). Other reasons given
were “not enough breast milk” (8%), “return to work” (6%), on “to make sure baby gets enough”
(6%). The most cited reason for use of formula at
Total
Hospital University Community Public
Delivery type Vaginal
Cesarean
First Breast Feed -2 hours 3-6 hours 7-12 hours 13. hours
Feeding Pattern
Demand
Modified demand
Schedule
0 20 40 60 80 100
Percent Exclusive Breast Feeding
Fig 1. Hospital factors and exclusive breast-feeding.
“to give mother some rest.” In contrast, the most
frequent reasons for use of formula supplements at
the community hospital was “mother ill” (40 of 177 respondents). The need for rest and recovery after delivery may be due to the type of delivery a women experienced because 71% ofthe 49 women who gave “mother ill” as a reason for formula use had been delivered of their neonate by cesarean section.
A logistic regression analysis was conducted to determine the effect of hospital procedures,
mater-0 20 40 60 80 100
Percent Exclusive Breast Feeding
Fig 2. Maternal commitment and exclusive breast-feed-ing.
nal commitment to breast-feed, and maternal
so-ciodemographic characteristics on exclusive
breast-feeding vs mixed feeding (Table 3). Delivery at the
university hospital remained a strong predictor of
exclusive vs mixed feeding (adjusted odds ratio 3.5,
95% CI 2.1 to 5.9) even after adjustment for all
other factors listed in Table 3 (the timing of the
first breast-feed, feeding pattern, delivery type,
rooming-in, timing of the decision to breast-feed,
TABLE 1. Demographic Predictors of Exclusive Breast-feeding
Factor No. %
Exclusive Breast-feeding*
Adjusted Odds Ratiof
95% Confidence
Interval
Hospital
Community 385 54 1.0 ...
Public 120 50 0.7 0.5-1.2
University 221 86 3.5 2.1-6.0
Education
12y 173 44 1.0 ...
13-16y 342 65 1.8 1.2-2.9
>16y 211 75 1.7 0.9-3.1
Ethnic group
Black 305 47 1.0 ...
White 421 74 2.2 1.4-3.2
Married
No 171 42 1.0 ...
Yes 554 69 1.7 1.1-2.6
Age
18-25 y 258 55 1.0 ...
26-30 y 246 63 0.7 0.5-1.1
>30y 222 71 0.7 0.4-1.2
Prenatal care
Private 535 64 1.0 ...
Clinic 120 47 0.9 0.6-1.5
HMO 65 85 1.2 0.5-2.8
Childbirth classes
No 148 53 1.0 ...
Yes 578 65 0.8 0.5-1.3
* x2statistics for each variable were statistically significant at P < .01.
t Because of missing data, adjusted odds ratios were calculated with data from 719 women. P<.05.
§Health maintenance organization.
Total
Decide before
Pregnancy
Yea No
Planned Duration of Breast Feeding (.5 months
TABLE 2. First Maternal Reason Given for Formula
Supplementation
Reason for Formula Use No. %
To give mother some rest 53 20
Mother ill 49 18
Not enough breast milk 22 8
Return to work 16 6
Make sure baby gets enough 15 6
To give mother more time 13 5
To fill baby up until milk comes 13 5 in
As a supplement 13 5
Baby rejects breast 13 5
Convenience 1 1 4
To increase blood sugar 1 1 4
Baby ill 10 4
Accustom baby to bottle 9 3
Hospital procedures 7 3
Freedom 5 2
Sore nipples 4 1
Let others feed baby 3 1
Total 267
education, marital status, and ethnicity). A first
breast-feed that occurred 7 to 12 hours postpartum on more than 12 hours postpartum decreased the odds of exclusive breast-feeding (adjusted odds 0.5, 95% CI 0.3 to 0.8 and adjusted odds 0.2, 95% CI 0.1 to 0.4, respectively). The odds of exclusive breast-feeding were increased approximately twofold for women delivering vaginally rather than by cesarean section, for those deciding to breast-feed before rather than during or after pregnancy, for those with some college vs a high school education, and for those who were married vs single. Women who breast-fed on a schedule rather than by demand decreased their odds of exclusive breast-feeding (adjusted odds 0.5, 95% CI 0.3 to 0.9). Ethnicity was not associated with exclusive breast-feeding.
DISCUSSION
Early formula supplementation in breast-fed
neonates is generally not recommended by medical
professionals.2 Yet, we found that 37% of breast-fed neonates (n = 726) were given supplementary
formula. This percentage varied by hospital of de-livery. Approximately half of the newborns of breast-feeding women delivered at the public or community hospital were given supplementary for-mula, whereas only 15% of newborns delivered at the university hospital were given formula.
Delivery at the university hospital was a strong
predictor of exclusive breast-feeding (adjusted odds
ratio 3.5, 95% CI 2.1 to 5.9) even after analyses
were controlled for maternal sociodemographic
characteristics, maternal commitment to
breast-TABLE 3. Hospital an clusive Breast-feeding
d Demogr aphi c Predictors of
Ex-Factor No.5 Odds
Ratio
95% Confidence Interval
Hospital
Community 333 1.0 ...
Public 114 1.0 0.6-1.7
University 208 3.5 2.1-5.9t
First breast-feed
2h 267 1.0 ...
2-6 h 137 1.1 0.7-1.9
7-12 h 133 0.5 O.3-0.8t
>12 h 118 0.2 0.1-0.4t
Feeding pattern
Demand 257 1.0 ...
Modified demand 223 0.8 0.5-1.3
Schedule 175 0.5 0.3-0.9t
Delivery
Vaginal 457 1.8 1.1-2.8t
Cesarean 198 1.0 ...
Rooming-in
Yes 436 1.4 0.9-2.2
No 219 1.0 ...
Decided to breast-feed
Before pregnancy 373 1.9 1.3-2.8t
During pregnancy 282 1.0 ...
Education
12y 156 1.0 ...
13-16y 305 1.6 1.0-2.6t
>16 y 194 1.3 0.7-2.3
Married
Yes 500 2.0 1.2-3.3t
No 154 1.0 ...
Ethnic group
White 388 1.1 0.7-1.7
Black 267 1.0 ...
* Total sample in this
analysis was 654 women after
exclusions for missing data and responses of “don’t know” to items regarding rooming-in, feeding pattern, and tim-ing of the first breast-feed.
t P < .05.
feed, and hospital procedures. The university hos-pital differed from the other two hospitals in the following ways: (1) a greater proportion of women initiated breast-feeding in the first 6 hours post-partum (74% vs approximately 50% at the other two hospitals); (2) a lower rate of cesarean
deliver-ies (25% compared with 34% at the community and
41% at the public county hospital); (3) a larger
proportion of married women (90% vs approxi-mately 70% at the other two hospitals); and (4) a larger proportion of white women (81% vs 63% at the public county and 43% at the community hos-pital). Even after analyses were controlled for these factors, women giving birth at the university hos-pital were more than 3#{189}times as likely to exclu-sively breast-feed as the women giving birth at the other two hospitals.
hos-pitals may exist in the breast-feeding attitude or infant-feeding counseling practices of the hospital
staff. Reiff and Essock-Vitale7 suggested that “hos-pital staff and routines exerted a stronger influence
on mothers’ infant-feeding practices by nonverbal
teaching (the hospital ‘modeling’ of infant formula
products) than by verbal teaching (counseling
sup-porting breast feeding).” This implies that hospital
staff and routines, centered around a
formula-feed-ing mode, can by suggestion influence maternal infant-feeding behavior. These nonverbal hospital
routines may be responsible for the observed differ-ences in exclusive breast-feeding rates between hos-pitals.
The longer a mother waited to initiate breast-feeding the more likely she was to use formula. Moreover, initiation of breast-feeding and delivery type were significantly correlated (r = .38; P < .05);
so that women who had a cesarean delivery tended
to initiate breast-feeding in the later postpartum hours. The cesanean delivery rates varied by hos-pital (lowest at the university hospital), as did the
proportion of women initiating breast-feeding
dun-ing the first 6 postpartum hours (highest at the university hospital). This finding indicates that the
rising cesarean delivery rate in the United States’#{176}
may indirectly promote formula use by delaying
initiation of breast-feeding.
Ideally, the hospital environment is conducive to the successful establishment of lactation. Often, however, the hospital routine is organized around a bottle-feeding mode, which can adversely affect breast-feeding.”2 Hospital practices that increase mother-neonate contact and increase the frequency of breast-feeds should have a positive effect on establishment of lactation, minimizing breast prob-lems such as engorgement, and ultimately increase the duration of breast-feeding. The findings of 5ev-eral studies support these hypotheses. Interviews with 100 mothers after delivery revealed that the sooner the neonate was put to the breast, the earlier lactation was established.’3 In addition, the earlier a first feed and the more frequent the number of feeds, the longer the duration of breast-feeding.’4
The maternal breast-feeding commitment was evaluated by examining when the mother made the decision to breast-feed and her planned duration of breast-feeding. The maternal anticipated duration of breast-feeding had no effect on formula use. Interestingly, 39% of these first-time mothers were unsure of how long they would breast-feed, which
indicates that breast-feeding continuation for many
women is guided by their experience with the method. In contrast, women who made the decision to breast-feed before rather than during or after
pregnancy were significantly more likely to
breast-feed exclusively.
Ethnicity was not associated with exclusive
breast-feeding in the final multivariate model. The
apparent ethnic differences were largely accounted for by hospital factors and timing of the decision to breast-feed. For example, 41% ofblack compared with 72% of white women initiated breast-feeding in the first 6 postpartum hours; 37% of black vs 19% of white women breast-fed on a schedule; and
35% black vs 51% of white women decided to
breast-feed before pregnancy.
In summary, delivery at the university hospital and early initiation of breast-feeding were strong indicators of exclusive breast-feeding, which im-plies that hospital factors can affect the early in-fant-feeding pattern and may influence long-term successful breast-feeding. Hospital staff should be aware that their breast-feeding attitude, infant-feeding counseling practices, and specific hospital
routines may play a large role in promoting on
inhibiting exclusive breast-feeding.
ACKNOWLEDGMENTS
This research was supported by a contract from the National Institute of Child Health and Human
Devel-opment of the National Institutes of Health, Bethesda,
Maryland.
We recognize and appreciate Survey Research Associ-ates, mc, for conducting the field work in completion of the study and particularly Sandi Eznine and Anna Martin
for their work in coordinating the project. We also appre-ciate the George Washington University Medical Center,
Prince George’s General Hospital and Medical Center, and the Washington Hospital Center. We particularly
thank Maureen Edwards, MD, William F. Peterson, MD,
and Elaine LoGuidice, RN.
REFERENCES
1. Kurinij N, Shiono PH, Rhoads GG. Breast-feeding incidence and duration in black and white women. Pediatrics. 1988;81:365-371
2. Lawrence RA. Breast-feeding: A Guide for the Medical Profession. 3rd ed. St Louis, MO: CV Mosby Co; 1989 3. Samuels SE, Margen 5, Schoen EJ. Incidence and duration
of breast-feeding in a health maintenance organization pop-ulation. Am J Clin Nutr. 1985;42:504-510
4. Wright HJ, Walker PC. Prediction of duration of breast feeding in primiparas. J Epidemiol Commun Health. 1983;37:89-94
5. Loughlin HH, Clapp-Channing NE, Gehlbach SH, Pollard JC, McCutchen TM. Early termination of breast-feeding-identifying those at risk. Pediatrics. 1985;75:508-513
6. Samuels SE. Socio-cultural obstacles to breastfeeding in an American community: the role of formula supplementation. Paper presented at the American Public Health Association Annual Meeting; November 1981; Los Angeles, CA 7. Reiff ML, Essock-Vitale SM. Hospital influences on early
infant-feeding practices. Pediatrics. 1985;76:872-879
9. Dixon WJ. BMDP Statistical Software. Berkeley, CA: Uni- lating ‘breast is best’ from theory to practice. Am J Obstet
versity of California Press; 1983:330-344 GynecoL 1980;138:105-117
10. Shiono PH, Fielden JG, McNellis D, Rhoads GG, Pearse 13. Mercer J, Russ R. Variables affecting time between child-WH. Recent trends in cesarian birth and trial of labor rates birth and the establishment of lactation. J Gen Psychol.
in the US. JAMA. 1987;257:494-497 1980102155-156
1 1. Johnson CA. Breast-feeding skills for health professi?nals. 14. Salariya EM Easton PM Cater JI. Duration of breast
A workshop at the American Public Health Association . . . . .
Annual Meeting; November 1981; Los Angeles, CA feeding after early initiation and frequent feeding. Lancet. 12. Winikoff B, Baer EC. The obstetrician’s opportunity: trans- 1978;2:11411143
NOTICE
REGARDING
THE
AMERICAN
ACADEMY
OF PEDIATRICS
NUTRITION
AWARD
1992
Nominations for the 1992 AAP Nutrition Award are now being solicited.
Separate letters should be written for each individual nominated. The letter
should contain a description of the nominee’s achievements and state clearly
the basis for the recommendation (including references to the literature which
describes his/her work). It is requested that the nominee’s bibliography be
submitted with the nominating letter, together with copies of available reprints.
Letters supporting the nomination (no more than five) are to be solicited and screened by the nominator and forwarded to the attention of:
Edgar 0. Ledbetter, MD, Director
Department of Maternal, Child and Adolescent Health
American Academy of Pediatrics
141 Northwest Point Boulevard
P0 Box 927
Elk Grove Village, IL 60009-0927
Please note that the deadline for award nominations is December 14, 1991. The Academy appreciates your effort to assist in the appropriate selection of a deserving person for this award.
NUTRITION
AWARD
STIPULATIONS
The Nutrition Award of the American Academy of Pediatrics was established in 1944. The award is made possible by a grant from the Infant Formula Council.
The Nutrition Award provides an honorarium of $3000 to be awarded under
the following stipulations:
1. The award will be made for outstanding achievement in research relating to
the nutrition of infants and children.
2. That the award be made for research, which has been completed and publicly
reported.
3. That the award be made for research, conducted by residents of the United
States and Canada.
4. That the award be made to one individual or for one project.
5. The award is open to all regardless of age. In fact, it is hoped that younger
persons will be considered for the award. No current member of the
Com-mittee on Nutrition shall be eligible for the award.
The Nutrition Award also includes round trip tourist class airfare as well as two days lodging at $150 per diem for the recipient and another person of his/ hen choice to attend the Annual Meeting of the Academy.