C
URRENTO
PINIONTopography-guided laser refractive surgery
Simon Holland
a,b, David T.C. Lin
a, and Johnson C.H. Tan
b,cPurpose of review
Topography-guided laser refractive surgery regularizes the front corneal surface irregularities to achieve the desired refractive outcome. This is particularly applicable in highly aberrated corneas, where wavefront aberrometry is often not possible. This article aims to review the recently published results of topography-guided ablations in normal regular corneas, highly aberrated corneas, and its application in conjunction with collagen cross-linking (CXL) in cases of keratectasia.
Recent findings
Topography-guided laser ablation is increasingly used with good efficacy and safety outcomes in highly aberrated corneas with irregular astigmatism. These include eyes with refractive surgery complications including postlaser in-situ keratomileusis ectasia, decentered ablation, small optical zones, asymmetrical astigmatism, and postradial keratectomy astigmatism. Further indications are for postkeratoplasty astigmatism and keratoconus. Simultaneous topography-guided ablations with CXL in keratectasia have been promising, both in addressing the surface irregularities and progressive nature of the conditions. Summary
Topography-guided laser refractive surgery is proving to be effective and well tolerated in the visual rehabilitation of highly aberrated eyes, with increasing predictability based on the recent research. Keywords
laser in-situ keratomileusis, laser refractive surgery, photorefractive keratectomy, topography-guided
INTRODUCTION
After gaining Conformite´ Europe´enne mark appro-val in Europe more than a decade ago, topography-guided laser ablation is still undergoing various stages of United States (US) Food and Drug Admin-istration (FDA) trials in the USA. Since Mrochen [1] reported his initial three cases of wavefront-guided laser in-situ keratomileusis (LASIK) in 2000, wave-front-guided ablation has been widely adopted in laser refractive surgery. That same year, Knorz and Jendritza [2] reported successful outcomes with topography-guided LASIK to treat corneal irregular-ities. Despite more than 10 years of experience, topography-guided ablation has not been accepted to the extent that wavefront-guided ablation has been, primarily because of its unpredictability, as any corneal topographic change will lead to an accompanying change in refraction. In the recent years, there is a resurgence of topography-guided ablations in corneas with high irregular astigma-tism, including post-LASIK ectasia, decentered ablation, small optical zones, postradial keratec-tomy, postkeratoplasty astigmatism, and keratoco-nus. There are increasing reports of simultaneous topography-guided treatment of keratectasia with
collagen cross-linking (CXL), which is not yet FDA approved in the USA. We aim to review the recent advances in topography-guided ablations not only in this group of highly aberrated corneas, but also in corneas with regular astigmatism, specifically com-paring topography guided with wavefront ablations in regular corneas.
WAVEFRONT VS. TOPOGRAPHY
MEASUREMENT
Wavefront-guided treatments attempt to improve the refractive outcomes by addressing higher order aberrations of the optical system, which takes into
aPacific Laser Eye Centre,bCornea Unit, Department of Ophthalmology,
Eye Care Centre, University of British Columbia, Vancouver, British Columbia, Canada andcNational Healthcare Group Eye Institute, Tan Tock Seng Hospital, Singapore, Singapore
Correspondence to Johnson C.H. Tan, MBBS, FRCSEd(Ophth), FAMS, Cornea Unit, Eye Care Centre, 2550 Willow Street, Vancouver, BC, Canada V5Z 3N9. Tel: +1 604 875 5850; e-mail: johnsontch@gmail. com
Curr Opin Ophthalmol2013, 24:302–309 DOI:10.1097/ICU.0b013e3283622a59
account the aberrations from the cornea, the lens, and even the retina; topography-guided ablation aims to regularize the uneven corneal front surface to achieve the desired refractive outcome. Wave-front maps are derived from theoretical models, and are dependent on the pupil size and accommo-dation. In highly aberrated corneas with irregular astigmatism, such as LASIK ectasia and post-penetrating keratoplasty astigmatism, it is often not possible to obtain a wavefront map or at least of a good quality. In these situations, corneal topo-graphy or tomotopo-graphy is usually possible to map out the irregularities on the corneal surfaces.
A key difference is that in wavefront measure-ments, the Zernike expansion is calculated from the entrance pupil center [3]. Topographic measure-ments of the cornea are centered on the corneal vertex, which approximates best to the visual axis. In most cases with normal corneas, the line of sight and the visual axis are in close proximity. However, in cases with a large topographic decentration, or even in normal eyes with a large angle kappa, such as in hyperopes as illustrated by Reinstein [4]
and Kanellopoulos [5&
], the different reference axes may give very different ablation profiles and refractive outcomes between wavefront-guided and topography-guided treatments.
PLANNING SOFTWARE
A range of planning software and topography-guided ablation platforms are commercially avail-able in the market. Topography-guided customized ablation treatment (T-CAT) planning software with ALLEGRETTO WAVE Eye-Q Excimer laser platform (Alcon Laboratories Inc, Ft Worth, Texas, USA) is currently under evaluation by the U.S. FDA, and has been approved in Europe since 2003 and in Canada. ALLEGRETTO T-CAT treatments usually result in a net hyperopic ablation, requiring a second myopic treatment to neutralize the cornea. Our group, Lin
et al.[6] developed a custom topographic
neutraliz-ation technique (TNT) to compensate for such a
change in a single treatment (Fig. 1). Other plat-forms currently available outside the USA are the CRS-Master planning software (Carl Zeiss Meditec, Jena, Germany), Nidek Advanced Vision Excimer (NAVEX; Nidek, Gamagori, Japan), and the Corneal
Interactive Programmed Topographic Ablation
(CIPTAmax; iVis Technology, Taranto, Italy). Topography-guided platforms use a Placido disk, Scheimpflug rotating camera, or a combination of both to capture corneal topography images to be analyzed by the proprietary algorithms to determine the ablation profile. ALLEGRETTO WAVE platforms offer both types of topography. The Scheimpflug-based rotating camera scans the eye either 25 or 50 times, and is best for centrally located aberra-tions. The Placido disk-based Allegretto Topolyzer obtains 22 000 data points to map the surface, but produces a central scotoma that needs to be extra-polated. Allan and Hassan [8] reported a prospective case series of topography-guided transepithelial photorefractive keratectomy (TG-PRK) using a 213-nm solid-state laser. The Pulsar Z1 platform (CV Laser Pty Ltd., Perth, Australia) has a combi-nation of both Placido disk imaging and sequential spot aberrometry, which obtains readings even in the presence of significant corneal irregularities. This allows spherocylindrical corrections to be incorporated into topographic ablation design. This platform also has the potential to perform wet-field ablation, as at 213 nm far-ultraviolet irradiation is less strongly absorbed by water [9].
TOPOGRAPHY-GUIDED REFRACTIVE
TREATMENT IN REGULAR CORNEAS
The greatest benefit and application of topography-guided ablations is probably in the treatment of highly aberrated corneas. However, there are also reports of successful topography-guided ablations in
regular corneas. Kanellopoulos [5&
] in his study of 202 eyes with hyperopia and hyperopic astigmatism that had undergone topography-guided LASIK showed that 75.5% of eyes achieved within 0.5 diopters (D) and 94.4% within 1D of target spherical equivalent at 24 months, whereas 46.6% gained at least one line of acuity postoperatively. Hyperopes may have a significant angle kappa, and wavefront-guided ablation centered on the entrance pupil might potentially introduce astigmatism [4].
Tanet al.’s [10] large retrospective series of 2051
eyes with low-to-high myopia and myopic
astigma-tism (mean spherical equivalent 5.042.33D,
range 0.00 to12.45D) treated topographically with
T-CAT treatment planning on the ALLEGRETTO WAVE Eye-Q Excimer laser platform achieved 20/20 or better in 72.9% of the eyes, with good
KEY POINTS
Topography-guided ablation regularizes the front corneal surface irregularities based on the acquisition of topographic maps of the corneal surface.
Results of topography-guided ablations are comparable to wavefront ablations in normal regular corneas. Successful topography-guided ablations have been
achieved in highly aberrated corneas, which were otherwise not possible with wavefront-based treatments.
predictability of 86.1% of eyes with spherical equiv-alent within 0.5D of target spherical equivequiv-alent. A total of 13.2% of eyes gained one or more lines in postoperative uncorrected distance visual acuity (UDVA) compared to preoperative corrected dis-tance visual acuity (CDVA). These results were com-parable to a recent study by Cummings and Mascharka [11], in which they demonstrated 88% of eyes achieved 0.5D of target spherical equivalent with the topolyzer-guided ablation, while 95% of eyes achieved 0.5D of target spherical equivalent
with the oculyzer-guided ablation with the
ALLEGRETTO WAVE Eye-Q system. Neither study had a control group of ALLEGRETTO WAVE wave-front-guided nor wavefront-optimized ablations.
There appear to be limited data on the direct comparison of topography-guided with
wavefront-guided ablations in regular corneas. Falavarjaniet al.
[12] studied 20 patients with low-to-moderate myo-pia with or without astigmatism who had received TG-PRK ablation and wavefront-optimized ablation on the contralateral eye. Though there were no
statistical differences between the two eyes in terms of visual outcomes and photopic contrast sensi-tivity, UDVA and contrast sensitivity were better in the wavefront-optimized group. Farooqi [13] found that topography-guided LASIK treatments achieved better night vision than conventional LASIK, but this may be from the expanded treatment zone. There is no compelling evidence of wavefront ablations being superior to topography-guided ablations or vice versa. The difficulty with using topography-guided ablations for normal, regular corneas is that there is likely less predictability of refractive outcome.
TOPOGRAPHY-GUIDED REFRACTIVE
TREATMENT IN HIGHLY ABERRATED
CORNEAS
The greatest value of topography-guided treatment is in the treatment of highly aberrated corneas. Postlaser refractive surgery complications, such as post-LASIK ectasia, decentered ablation, small optical
FIGURE 1. Four steps in custom topographic neutralization technique (TNT) with topography-guided customized ablation treatment (T-CAT) planning software, ALLEGRETTO WAVE Eye-Q Excimer laser. Reproduced with permission [7&
zones, postradial keratectomy astigmatism, and other highly irregular corneas seen in postkerato-plasty astigmatism and keratoconus, have been suc-cessfully treated with this modality.
Postrefractive surgery complications
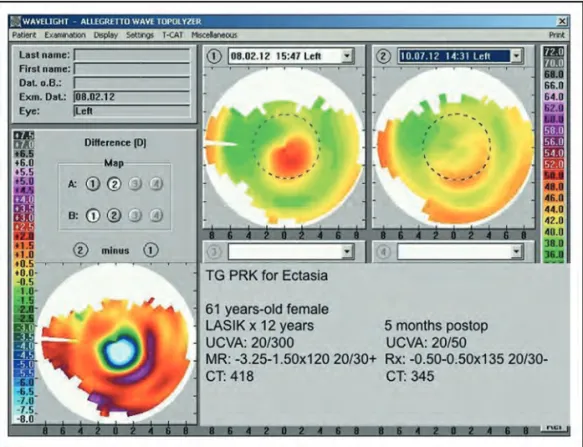
In our series of 17 eyes treated for post-LASIK ectasia, 71% of eyes achieved UDVA of 20/40, compared to 12% preoperatively, with 53% of eyes gaining 2 lines
or more of CDVA [7&
] (Fig. 2). Kanellopoulos and
Binder [14] targeted a maximum ablation of 50mm
to limit possible exacerbation of ectasia. Thus, treat-ment was more therapeutic by reducing the corneal irregularities than refractive, although managed to decrease the mean refractive error by more than 2.5D in 27 of 32 eyes, and mean final spherical
equivalent of1.75D.
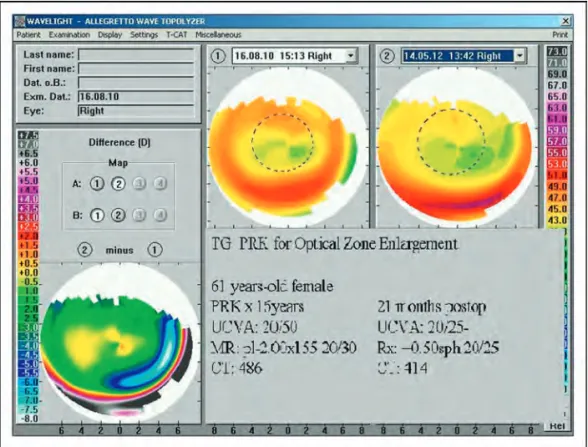
Other postrefractive surgery complications were
studied by our group and Chen et al. [15]. We
showed an improvement in decentration and enlargement in optical zones after treatment with TG-PRK, with 94 and 92% of eyes within 1D of target
refraction, respectively [7&
] (Fig. 3). Also reported was the improvement in cylinders from 1.31D (range 0.00–5.75D) preoperatively to 0.52D (range 0.00–1.50D), and from 2.00D (range 0.00–4.50D) to 0.89D (range 0.00–1.50D) after treatment with TG-PRK with custom TNT for asymmetrical astig-matism and radial keratotomy.
Chen et al.’s [15] mixed group of 17 eyes
with post-LASIK complications (free cap, micro-folds, buttonhole, decentered flap, small flap,
epithelial ingrowth, diffuse lamellar keratitis
scarring, lacerated flap interface, and double-flap interface) had an improvement in the irregularity
index from 25.8212.82mm preoperatively to
20.3610.64mm, whereas asymmetry changed from
3.742.22D to 2.161.19D. A total of 47% of eyes
were within 0.5D of intended refraction and 88% were within 1D of intended refraction.
Postkeratoplasty astigmatism
High astigmatism is common after penetrating keratoplasty, such as 38% of eyes having more than 5D of astigmatism [16]. Often these corneas are highly irregular, with astigmatism that cannot be corrected with glasses or contact lenses. Spadea [17] performed TG-PRK with prophylactic CXL for residual refractive error on 14 eyes that had pre-viously undergone lamellar keratoplasty for
kerato-conus. Mean preoperative manifest refractive
spherical equivalent improved from6.112.48D
(range 2.50 to 9.50D) to 0.792.09D (range
þ1.0 to 3.0D). However, the improvement in
topographic keratometric astigmatism was not
significant (5.57D3.52D to 5.022.93D). In our
larger series of 27 eyes, mean cylinder improved from 4.46D (range 1.75–7.50D) preoperatively to
FIGURE 2. Topography-guided photorefractive keratectomy for postlaser in-situ keratomileusis ectasia. Reproduced with permission [7&
].
1.64D (range 0.00–5.50D) [7&
] (Fig. 4). The improve-ment was similarly seen in Ohno’s small study of five eyes [18], in which the mean cylinder improved
from 7.00D (range 4.75 to 9.00D) to 1.25D
(range 0.50D to 2.50D). Gao et al. [19] also
reported statistical improvement in asphericity and index of surface variance in his series of 10 eyes after topography-guided laser-assisted subepithelial keratectomy (LASEK) treatment for irregular astig-matism after epikeratophakia.
FIGURE 3.Enlargement of optical zone with topography-guided photorefractive keratectomy. Reproduced with permission [7& ].
FIGURE 4. Improvement in uncorrected distance visual acuity and astigmatism after topography-guided photorefractive keratectomy for postoperative keratoplasty astigmatism. Reproduced with permission [7&
Improvement in CDVA was higher for irregular astigmatism from refractive surgery than for
post-keratoplasty astigmatism [7&
,8]. This could be explained by the higher amount of astigmatism and irregularities in the latter group.
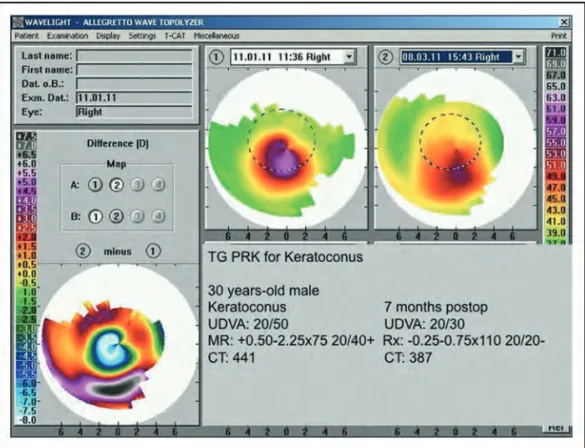
Keratoconus and cross-linking
There are increasing reports of topography-guided laser treatment combined with CXL for keratoconus to achieve improved topography and reduction of refractive error. It has been shown that CXL is effective in halting or slowing the progression of keratoconus [20]. Neither procedure is yet approved by the U.S. FDA. Kanellopoulos and Binder [21] in 2007 reported CXL with sequential TG-PRK with significant clinical improvement and stability. How-ever, sequential PRK will remove some of the pre-viously cross-linked cornea. Corneal ablation may also be less predictable in cross-linked corneas. Kanellopoulos [22] also showed that same-day simultaneous TG-PRK with CXL was superior to sequential treatment in visual rehabilitation of patients with keratoconus. In the treatment plan-ning of such cases, target was to undercorrect by 30% in anticipation of further flattening effect of CXL. We reported that 8 of 75 eyes in our study had a hyperopic spherical equivalent of greater than
þ1.50D at 1 year despite targeting an outcome of
1.25D, but this may have been related to the
treat-ment nomogram and the CXL flattening effect [7&
] (Fig. 5).
Kymionis [23] and Tuwairqi [24] showed a safety index of 1.21 and 1.6, respectively, in keratoconus patients treated with simultaneous TG-PRK and CXL. A total of 48–60% of eyes gained 1 line or
more and 10–12.5% lost 1 line of acuity [7&
,23]. Our group reported 58% of eyes achieving UDVA of 20/40 or better, and 92% having CDVA of 20/40 or better. Keratometry readings decreased by 1.18D and 2.35D at the flat and steep meridians, respect-ively, in the study by Kymionis [23], which reported lower numbers than Kannellopoulos’s large series of
198 eyes with a reduction of 3.501.3D [22].
The role of prophylactic CXL is controversial. Spadea [17] performed CXL after TG-PRK in eyes that had undergone lamellar keratoplasty for kera-toconus. Although it is rare to get ectasia after PRK, prophylactic CXL may offer benefits to patients with a personal history of keratoconus. Although there are reports of recurrence of ectasia after keratoplasty in eyes with previous history of keratoconus, and usually at the host rim rather than true ectasia of the graft, it is extremely uncommon. Spadea performed CXL after epithelial ablation up to 9 mm. It is not known whether this larger diameter of irradiation is enough to strengthen the peripheral host cornea rim.
FIGURE 5. Topography-guided photorefractive keratectomy with collagen cross-linking for keratoconus. Reproduced with permission [7&
].
Kanellopoulos introduced the concept of high irradiance, short exposure CXL in myopic LASIK (LASIK Xtra). In his recent study of topography-guided hyperopic LASIK with CXL to modulate the intrinsic corneal flattening effect of hyperopic ablation [25], he showed greater kera-tometric stability over 2 years in the 34 eyes in the study. There are no long-term results beyond 2 years and no similar published data to reach a consensus on the use of prophylactic CXL in such cases.
NEW CONCEPTS
The corneal epithelium had been shown to be able to compensate for irregular stromal surfaces by altering its thickness profile to achieve a smooth
optical surface. Reinsteinet al. [26&
] reported that current planning treatment does not take into account the epithelial–stromal interface, and sig-nificant regressions after refractive surgeries may be because of epithelial remodeling. They reported a case in which three-dimensional Artemis very high-frequency (VHF) digital ultrasound scan (Arcscan Inc, Morrison, Colorado) was used to provide pachymetric maps of the individual corneal layers, and found a 3.2D difference of inferior-superior asymmetrical index at 2 mm radius between the epithelial and stromal surface of an eye that had previously undergone radial keratotomy. The first step of the treatment was to perform an Artemis-assisted transepithelial phototherapeutic keratec-tomy targeting at the component of the stromal irregularity compensated by the epithelium, and subsequent steps of topography-guided excimer ablation to correct the irregularities not masked by the epithelium. This case suggests that epithelial remodeling may result in unpredictable outcome after laser refractive surgery, presumably more in eyes with previous ocular surface injuries or surgeries.
CONCLUSION
Topography-guided ablation has the potential to be a valuable addition to laser vision correction, especi-ally in highly aberrated eyes in which wavefront aberrometry cannot be reliably obtained. There are increasing studies on improving the predictability and safety profiles. Presently, the use of topography-guided ablation in regular corneas is undecided pending further studies.
Acknowledgements
None.
Conflicts of interest
S.H. received research support from Alcon Laboratories Inc., and travel support from Allergan and Bausch & Lomb. The other authors have no financial interests in the materials mentioned.
REFERENCES AND RECOMMENDED
READING
Papers of particular interest, published within the annual period of review, have been highlighted as:
& of special interest && of outstanding interest
Additional references related to this topic can also be found in the Current World Literature section in this issue (pp. 363–364).
1. Mrochen M, Kaemmerer M, Seiler T. Wavefront-guided laser in situ kerato-mileusis: early results in three eyes. J Refract Surg 2000; 16:116–121.
2. Knorz MC, Jendritza B. Topographically-guided laser in situ keratomileusis to treat corneal irregularities. Ophthalmology 2000; 107:1138–1143.
3. Applegate RA, Thibos LN, Bradley A,et al.Reference axis selection: sub-committee report of the OSA Working Group to establish standards for measurement and reporting of optical aberrations of the eye. J Refract Surg 2000; 16:S656–S658.
4. Reinstein DZ, Archer TJ, Gobbe M. Is topography-guided ablation profile centered on the corneal vertex better than wavefront-guided ablation profile centered on the entrance pupil? J Refract Surg 2012; 28:139– 143.
5.
&
Kanellopoulos AJ. Topography-guided hyperopic and hyperopic astigmatism femtosecond laser-assisted LASIK: long-term experience with the 400 Hz eye-Q excimer platform. Clin Ophthalmol 2012; 6:895–901.
A total of 75.5% of 202 eyes with hyperopia, with or without astigmatism, achieved within 0.5D and 94.4% within 1D of target spherical equivalent at 24 months, whereas 46.6% gained at least one line of acuity postoperatively. Hyperopes with significant angle kappa perform well with topography-guided LASIK centered on the corneal vertex.
6. Lin DT, Holland SR, Rocha KM, Krueger RR. Method for optimizing topo-graphy-guided ablation of highly aberrated eyes with the ALLEGRETTO WAVE excimer laser. J Refract Surg 2008; 24:S439–S445.
7.
&
Lin DT, Holland S, Tan JC, Moloney G. Clinical results of topography-based customized ablations in highly aberrated eyes and keratoconus/ectasia with cross-linking. J Refract Surg 2012; 28:S841–S848.
In eyes undergoing topography-guided photorefractive keratectomy for post-keratoplasty astigmatism (27 eyes), and combined with simultaneous collagen cross-linking for keratoconus (72 eyes) and post-LASIK ectasia (17 eyes), mean cylinder improved from 4.46D to 1.64D, 2.87D to 1.40D and reduction of 2.56D of cylinder, respectively.
8. Allan BD, Hassan H. Topography-guided transepithelial photorefractive ker-atectomy for irregular astigmatism using a 213 nm solid-state laser. J Cataract Refract Surg 2013; 39:97–104.
9. Shah S, Sheppard AL, Castle J,et al.Refractive outcomes of laser-assisted subepithelial keratectomy for myopia, hyperopia, and astigmatism using a 213 nm wavelength solid-state laser. J Cataract Refract Surg 2012; 38:746– 751.
10. Tan J, Simon D, Mrochen M, Por YM. Clinical results of topography-based customized ablations for myopia and myopic astigmatism. J Refract Surg 2012; 28:S829–S836.
11. Cummings AB, Mascharka N. Outcomes after topography-based LASIK and LASEK with the wavelight oculyzer and topolyzer platforms. J Refract Surg 2010; 26:478–485.
12. Falavarjani KG, Hashemi M, Modarres M, et al. Topography-guided vs wavefront-optimized surface ablation for myopia using the waveLight platform: a contralateral eye study. J Refract Surg 2011; 27:13–17.
13. Farooqui MA, Al-Muammar AR. Topography-guided CATz versus conven-tional LASIK for myopia with the NIDEK EC-5000: a bilateral eye study. J Refract Surg 2006; 22:741–745.
14. Kanellopoulos AJ, Binder PS. Management of corneal ectasia after LASIK with combined, same-day, topography-guided partial transepithelial PRK and collagen cross-linking: the Athens protocol. J Refract Surg 2011; 27: 323–331.
15. Chen X, Stojanovic A, Zhou W,et al.Transepithelial, topography-guided ablation in the treatment of visual disturbances in LASIK flap or interface complications. J Refract Surg 2012; 28:120–126.
16. Williams KA, Ash JK, Pararajasegaram P,et al.Long-term outcome after corneal transplantation. Visual result and patient perception of success. Ophthalmology 1991; 98:651–657.
17. Spadea L, Paroli M. Simultaneous topography-guided PRK followed by corneal collagen cross-linking after lamellar keratoplasty for keratoconus. Clin Ophthalmol 2012; 6:1793–1800.
18. Ohno K. Customized photorefractive keratectomy for the correction of regular and irregular astigmatism after penetrating keratoplasty. Cornea 2011; 30 (Suppl. 1):S41–S44.
19. Gao H, Shi W, Liu M,et al.Advanced topography-guided (OcuLink) treatment of irregular astigmatism after epikeratophakia in keratoconus with the wave-light excimer laser. Cornea 2012; 31:140–144.
20. Vinciguerra P, Albe` E, Trazza S,et al.Intraoperative and postoperative effects of corneal collagen cross-linking on progressive keratoconus. Arch Ophthal-mol 2009; 127:1258–1265.
21. Kanellopoulos AJ, Binder PS. Collagen cross-linking (CCL) with sequential topography-guided PRK: a temporizing alternative for keratoconus to pene-trating keratoplasty. Cornea 2007; 26:891–895.
22. Kanellopoulos AJ. Comparison of sequential vs same-day simultaneous collagen cross-linking and topography-guided PRK for treatment of kerato-conus. J Refract Surg 2009; 25:S812–S818.
23. Kymionis GD, Portaliou DM, Kounis GA,et al.Simultaneous topography-guided photorefractive keratectomy followed by corneal collagen cross-linking for keratoconus. Am J Ophthalmol 2011; 152:748 – 755.
24. Tuwairqi WS, Sinjab MM. Safety and efficacy of simultaneous corneal collagen cross-linking with topography-guided PRK in managing low-grade keratoconus: 1-year follow-up. J Refract Surg 2012; 28:341–345.
25. Kanellopoulos AJ, Kahn J. Topography-guided hyperopic LASIK with and without high irradiance collagen cross-linking: initial comparative clinical findings in a contralateral eye study of 34 consecutive patients. J Refract Surg 2012; 28:S837–S840.
26.
&
Reinstein DZ, Archer TJ, Gobbe M. Refractive and topographic errors in topography-guided ablation produced by epithelial compensation predicted by 3D Artemis VHF digital ultrasound stromal and epithelial thickness mapping. J Refract Surg 2012; 28:657–663.
Epithelial remodeling over anterior stromal surface masked the underlying stromal irregularities. By first performing an Artemis-assisted transepithelial photothera-peutic keratectomy procedure targeting the component of the stromal irregularity compensated for by the epithelium, and subsequent ablations to correct for residual refractive error, uncorrected distance visual acuity of 20/20þ2 with plano refraction was achieved in a case with prior radial keratotomy. This case demon-strated the significant optical shift contributed by the epithelium that if not taken into account, may result in suboptimal refractive outcome.