ARTICLE
Medication Errors Related to Computerized Order
Entry for Children
Kathleen E. Walsh, MD, MSca, William G. Adams, MDb, Howard Bauchner, MDb, Robert J. Vinci, MDb, John B. Chessare, MDb,c,
Maureen R. Cooper, RNb, Pamela M. Hebert, RNb, Elisabeth G. Schainker, MDd, Christopher P. Landrigan, MDe,f
aDepartment of Pediatrics, University of Massachusetts Medical School/University of Massachusetts Memorial Medical Center, Worcester, Massachusetts;bDepartment of Pediatrics, Boston University School of Medicine/Boston Medical Center, Boston, Massachusetts;cNorwood Caritas Hospital, Norwood, Massachusetts;dDepartment of Pediatrics, Tufts University School of Medicine/New England Medical Center, Boston, Massachusetts;eDepartment of Medicine, Brigham and Women’s Hospital, Boston, Massachusetts;fDepartment of Medicine, Children’s Hospital Boston, Boston, Massachusetts
The authors have indicated they have no financial relationships relevant to this article to disclose.
ABSTRACT
OBJECTIVE.The objective of this study was to determine the frequency and types of
pediatric medication errors attributable to design features of a computerized order entry system.
METHODS.A total of 352 randomly selected, inpatient, pediatric admissions were
reviewed retrospectively for identification of medication errors, 3 to 12 months after implementation of computerized order entry. Errors were identified and classified by using an established, comprehensive, active surveillance method. Errors attributable to the computer system were classified according to type.
RESULTS.Among 6916 medication orders in 1930 patient-days, there were 104
pediatric medication errors, of which 71 were serious (37 serious medication errors per 1000 patient-days). Of all pediatric medication errors detected, 19% (7 serious and 13 with little potential for harm) were computer related. The rate of comput-er-related pediatric errors was 10 errors per 1000 patient-days, and the rate of serious computer-related pediatric errors was 3.6 errors per 1000 patient-days. The following 4 types of computer-related errors were identified: duplicate medication orders (same medication ordered twice in different concentrations of syrup, to work around computer constraints; 2 errors), drop-down menu selection errors (wrong selection from a drop-down box; 9 errors), keypad entry error (5 typed instead of 50; 1 error), and order set errors (orders selected from a pediatric order set that were not appropriate for the patient; 8 errors). In addition, 4 preventable adverse drug events in drug ordering occurred that were not considered computer-related but were not prevented by the computerized physician order entry system.
CONCLUSIONS.Serious pediatric computer-related errors are uncommon (3.6 errors
per 1000 patient-days), but computer systems can introduce some new pediatric medication errors that are not typically seen in a paper ordering system.
www.pediatrics.org/cgi/doi/10.1542/ peds.2006-0810
doi:10.1542/peds.2006-0810
Key Words
computerized physician order entry, medication errors, hospital performance, patient safety, computer order entry
Abbreviations
CPOE— computerized physician order entry
CRE— computer-related error CI— confidence interval
Accepted for publication Jun 27, 2006 Address correspondence to Kathleen E. Walsh, MD, MSc, Department of Pediatrics, Benedict Second Floor, University of Massachusetts Memorial Medical Center, 55 North Lake St, Worcester, MA 01655. E-mail: walshk02@ ummhc.org
M
EDICATION ERRORS ARE a leading cause of pre-ventable injuries, resulting in the deaths of thou-sands of patients each year.1–4 Potentially dangerousmedication errors occur in up to 1 of 10 pediatric admis-sions.5,6One important strategy to address this problem,
computerized physician order entry (CPOE), has been demonstrated to reduce serious medication errors by 55% to 83%.7–12 More than one half of the nation’s
hospitals are planning to implement CPOE in the next several years.13
Recent reports suggest that design features of CPOE systems may increase the likelihood of some medication errors, termed “computer-related errors” (CREs). Volun-tary reports of CREs have increased steadily in recent years, and CREs have become the fourth leading cause of medication errors reported by hospitals to the US Phar-macopeia MedMARx system.14A recent study of
admin-istrative data described increased mortality rates for pe-diatric critical care transfers after implementation of CPOE.15A recent qualitative study of health care
provid-ers using CPOE described 22 types of possible CREs.16
CREs among pediatric patients have not been described. Voluntary reports cannot be used to quantify the inci-dence of CREs, and neither can qualitative methods.17,18
We conducted a study with established, comprehensive, active surveillance methods,5,19 to determine the
fre-quency, severity, and types of pediatric CREs and to determine the proportion of all medication errors repre-sented by CREs after implementation of a CPOE system. The focus of this study was not on evaluating the overall effectiveness of CPOE in preventing pediatric errors but rather on describing rates and types of pediatric CREs.
METHODS
Study Site and CPOE System
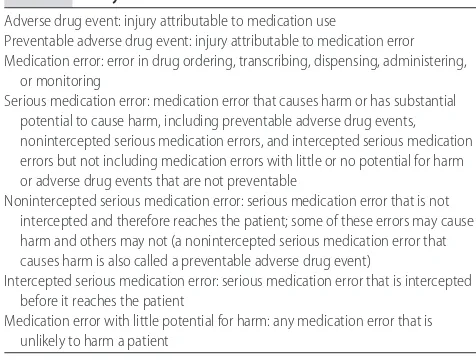
This study was designed during implementation of pe-diatric CPOE at the study hospital, to measure retrospec-tively rates and types of pediatric CREs by using com-prehensive error-detection methods. A medication error was defined as an error in drug ordering, transcribing, administering, or monitoring (Table 1).
The study, approved by the institutional review board of Boston University Medical School, was conducted in an urban teaching hospital with 40 general and surgical pediatric inpatient beds, 4 PICU beds, and 15 NICU beds. Patients in these units are cared for by pediatric and surgical residents and attending physicians. From April to June 2002, the pediatric units implemented Sunrise Clinical Manager 3.04, a CPOE system commercially available from Eclipsys (Boca Raton, FL).12 No changes
were made to the pediatric system during the time of the study. Only residents write orders, which are entered directly into the CPOE system. Attending physicians do not write orders. Medical students do write orders but are required to have a resident physician cosign orders to
activate them. Only medical student orders cosigned by resident physicians were reviewed in this study. Clini-cians were required to complete a 2- to 3-hour training class before being granted access to the CPOE system.
The patient’s weight and drug allergies are entered manually by the admitting resident before admission orders are written. To order a medication for a patient, the resident must select the patient’s name from the active patient list or a floor list of patients or enter the patient’s name or medical record number. The resident must then click on a button to enter orders and type in the name of the medication. A list of possible medica-tions and different formulary and route opmedica-tions appears in a drop-down menu; the resident must click on the medication formulary and route of interest. A dosing window then appears, in which the resident may type a numerical dose or use the optional calculator to calculate a medication dose for the patient. The resident then selects the units of the dose from a drop-down menu. Ordering is completed, and the order is entered into the system. If there are no alerts, then the resident enters another window to sign the order electronically. If there is an alert, then the physician may acknowledge the alert and sign the order or rewrite the order.
Incorporated decision support systems include pre-configured order sets for selected conditions, drug al-lergy alerts, drug-drug interaction alerts, alerts for du-plicate orders, and wrong-dose alerts. For all pediatric medications, the CPOE system checks the dosage auto-matically, on the basis of the patient’s weight as entered into the computer, and generates alerts for overdosing and underdosing. The ordering physician can override all alerts. Computer terminals are available on patient care units in well-lit areas outside patient rooms.
Medication orders are sent electronically to the phar-macy and verified by a pharmacist. During the period included in this study, nurses reviewed orders online but used a paper medication-administration record for
doc-TABLE 1 Study Definitions
Adverse drug event: injury attributable to medication use
Preventable adverse drug event: injury attributable to medication error Medication error: error in drug ordering, transcribing, dispensing, administering,
or monitoring
Serious medication error: medication error that causes harm or has substantial potential to cause harm, including preventable adverse drug events, nonintercepted serious medication errors, and intercepted serious medication errors but not including medication errors with little or no potential for harm or adverse drug events that are not preventable
Nonintercepted serious medication error: serious medication error that is not intercepted and therefore reaches the patient; some of these errors may cause harm and others may not (a nonintercepted serious medication error that causes harm is also called a preventable adverse drug event)
Intercepted serious medication error: serious medication error that is intercepted before it reaches the patient
umentation of medications given. Paper orders were written only during scheduled downtime for computer maintenance (usually 4 hours per month). Verbal orders during emergency situations were accepted by nursing staff members, who placed the orders into the CPOE system themselves.
Inclusion Criteria
Data were collected from 3 months after the implemen-tation of CPOE in September 2002 to May 2003. In each month, 40 admissions were selected randomly for inclu-sion. Patients with multiple admissions during the study period might have been included more than once.
The normal newborn nursery was excluded from the study because few medications are dispensed there. Er-rors made in the emergency department, the operating room, and the postanesthesia care unit were excluded because those units did not use CPOE at the time of the study. At least 3 attempts were made to obtain hospital records selected for inclusion in the study. Any patient with persistently missing records was replaced by an-other patient, matched with respect to date of admission, hospital unit, and length of stay.
Detection of Medication Errors
Pediatric nurses (M.R.C. and P.M.H.) reviewed all ad-missions by using a previously validated strategy.5,19,20
Briefly, nurses reviewed charts for several signs of an error, such as the use of naloxone or a very low glucose measurement after an insulin injection. All orders that were discontinued abruptly and rewritten were re-viewed closely for errors. Nurses also used their clinical acumen to scan for signs of an error. Any sign of an error was investigated more thoroughly. If, with additional investigation, nurses thought that an error might have occurred, then a description of the possible error was recorded.
Nurses were trained to review admissions for errors in 2 sessions. In the first session, nurses were taught defi-nitions of terms, types of medication errors, and preven-tion strategies, with a review of the literature. In the second session, nurses were oriented to instruments for data collection, and 3 sample charts were reviewed by using comprehensive, error-detection methods. Nurses were not told the study objectives but were told simply to review all aspects of the chart for medication errors and preventable adverse drug events (injury attributable to medication error) (definitions in Table 1). One of the study physicians (K.E.W.) met with nurses weekly to biweekly throughout the study, to answer questions. Each nurse reviewed one half of the sample of charts. Although inter-rater reliability between the 2 nurse re-viewers was not calculated, there was no difference in the odds of an error being found by either nurse re-viewer (odds ratio: 0.97; 95% confidence interval [CI]: 0.89 –1.04).
The discharge summary, progress notes, nursing notes, nursing flowsheets, physician notes, and medica-tion-administration records of the paper record were reviewed. All medication orders were also reviewed. Descriptions of each possible error and any clinic out-comes (eg, additional testing or monitoring, transfer to the ICU, or permanent disability) were recorded in de-tail. Additional data collected included length of hospital stay, total number of medication orders per patient, and whether orders were computerized, handwritten, or both. Hospital incident reports describing medication er-rors and adverse drug events were obtained for all ad-missions included in the study, to supplement possible errors detected through review of the notes and orders. Two study pediatricians reviewed all possible errors identified by study nurses and through incident reports. Pediatrician reviewers classified errors as (1) adverse drug events, (2) serious medication errors without in-jury, (3) medication errors with little potential for harm, or (4) neither an adverse drug event nor a medication error (exclusion). Physician reviewers excluded 30% of all possible errors reported by nurses. The severity of serious medication errors and adverse drug events was rated as (1) significant, (2) serious, (3) life-threatening, or (4) fatal.
The preventability of medication errors that were not intercepted by hospital staff members was rated as (1) definitely not preventable, (2) probably not preventable, (3) probably preventable, or (4) definitely preventable. Preventable was defined as able to be avoided by a reasonable pediatrician. An allergic reaction to an anti-biotic the patient was known to be allergic to would be considered definitely preventable. An allergic reaction to an antibiotic the patient was not previously known to be allergic to would be considered definitely not prevent-able.
Pediatrician raters also classified errors as computer related or not computer related. Raters were instructed to rate errors as computer related only if the errors were highly unlikely to occur in a paper-based system and had a clear computer-based mechanism. Inter-rater reliabil-ity scores for these judgments were 0.7 (95% CI: 0.68 – 0.84) for error classification, 0.4 (95% CI: 0.26 – 0.57) for severity, 0.8 (95% CI: 0.67– 0.82) for prevent-ability, and 0.8 (95% CI: 0.61– 0.92) for computer relat-edness. Differences in judgments were resolved by physician raters through discussion, to reach consensus.
Grouping of CREs
and to describe each type. Independently, each staff member created 4 categories. The group then met and came to consensus regarding the names and descriptions of the categories.
Computer Log
The CPOE system logs automatically all error warnings generated by CPOE, such as a dose warning for an order for ceftriaxone at 900 g rather than 900 mg. Each record in the log contains the physician’s name, the medical record number, the date and time, the type of warning, and the response of the physician. One author (K.E.W.) reviewed this log to determine whether the computer generated an error alert regarding any of the CREs iden-tified and, if so, what the ordering physician’s response was. Information from the log was not used to deter-mine the incidence of CREs.
Analysis
Error frequencies were expressed per 1000 patient-days, per 100 admissions, and per 1000 medication orders. The total number of patient-days was the sum of the length of stay for all included patients. The total number of medication orders was the sum of the number of medications per patient (from nurse review) for all cluded patients. Orders for pharmaceutical products, in-travenous fluids, total parenteral nutrition, and blood products were all considered medication orders and were included in this count. Orders for oral or gastric tube formulas were not considered medication orders and were not included in this count.
RESULTS
Overall Medication Error Rates
Three hundred fifty-two of 975 PICU (n⫽51), NICU (n
⫽ 47), and inpatient ward admissions (n ⫽254) were reviewed. Twenty-six patients had ⬎1 admission in-cluded in the study (19 patients had 2 admissions, 6 had 3 admissions, and 1 patient had 4 admissions). Thirty-three patient admissions (9%) were excluded because of missing charts that were not found despite multiple
at-tempts; these admissions were replaced with other matched admissions, as described above. There was no significant difference in length of stay or hospital unit (NICU, PICU, or wards) between included records and missing records. Of the admissions included in the study, 27 records (5.7%) were incomplete and some were miss-ing more than 1 part of the record; 20 (5%) were missmiss-ing some or all of the medication-administration records, 6 (2%) were missing some or all of the vital sign flow-sheets, 7 (2%) were missing some or all of the nursing notes, 7 (2%) were missing some of the progress notes, and 12 medication orders were missing from 4 records (1%). We excluded an additional 8 admissions from the study because many parts of the charts were missing, making comprehensive chart review impossible.
There were 6916 medication orders written for the 352 included admissions, over the course of 1930 pa-tient-days. There were 24 handwritten medication or-ders (0.3% of all medication oror-ders) in total; 3 admis-sions had handwritten medication orders only and 4 admissions had some handwritten and some computer-ized medication orders. None of the handwritten medi-cation orders contained errors.
A total of 26 adverse drug events were identified, of which 12 were caused by medication errors (Table 2). There were 71 serious medication errors, of which 46 reached the patient (including the 12 adverse drug events caused by error), and 33 medication errors with little potential for harm (total errors: 104). The rates of adverse drug events, serious medication errors, and total errors were 13 events per 1000 patient-days, 37 errors per 1000 days, and 54 errors per 1000 patient-days, respectively. Of all serious medication errors, 71% were in drug ordering, 2.6% in transcribing (from the computer to the paper medication-administration record), 0% in dispensing, 15.8% in administering, 7.9% in monitoring, and 2.7% other (a child sprayed another child with an aerosolized medication).
Four ordering errors that resulted in patient injury were not CREs but also were not prevented by CPOE. Of those, 2 resulted from failure to increase a medication
TABLE 2 Overall Rates of Adverse Drug Events, Serious Medication Errors, and Medication Errors With Little Potential for Harm
Incidents Rate, Cases per 1000
Patient-Days (n)
Rate, Cases per 100 Admissions
Rate, Cases per 1000 Medication Orders
Adverse drug events
Not attributable to error 7.3 (14) 4.0 2.0
Attributable to error 6.2 (12) 3.4 1.7
Serious errors
Reached patienta 23.8 (46) 13.1 6.7
Intercepted 13.0 (25) 7.1 3.6
Errors with little potential for harm 17.1 (33) 9.4 4.8
Total errors 53.9 (104) 29.5 15.0
dose despite repeated low serum levels and clinical signs of subtherapeutic treatment. Another was an order for an electrolyte for a patient with a normal electrolyte level. After administration of the electrolyte, the patient developed high electrolyte levels. The last was an order for a medication that was contraindicated.
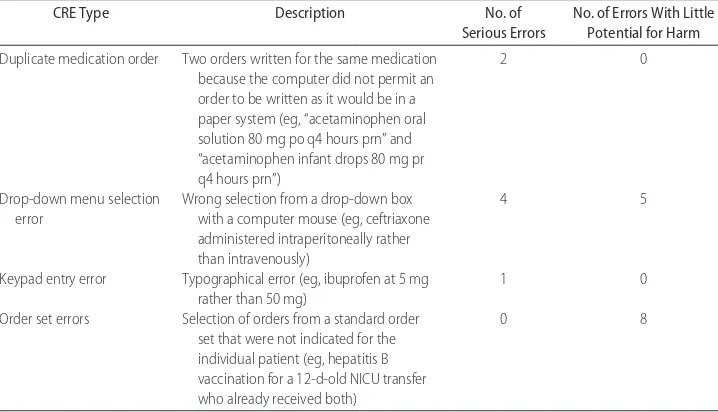
CREs
Of the 104 total medication errors, 20 were CREs, in-cluding 7 serious medication errors and 13 medication errors with little potential for harm (Table 3). The rate of CREs was 10 errors per 1000 patient-days, and the rate of serious CREs was 3.6 errors per 1000 patient-days. One of the errors that was judged to have little potential for harm reached the patient and caused no harm. Four hospital staff members grouped these CREs into 4 cate-gories; there were 2 sets of duplicate medication orders (both serious errors), 9 drop-down menu selection er-rors (including 4 serious erer-rors), 1 serious keypad entry error, and 8 order set errors (none serious).
The first category was duplicate medication orders, which occurred when the computer did not permit an order to be written in the computer as it would be written in a paper system and so 2 orders were written by the user for the same medication. Both errors were sets of duplicate acetaminophen orders; because of the potential for acetaminophen overdose, they were both classified as serious medication errors. In a review of the computer log, neither of those errors generated com-puter error warnings.
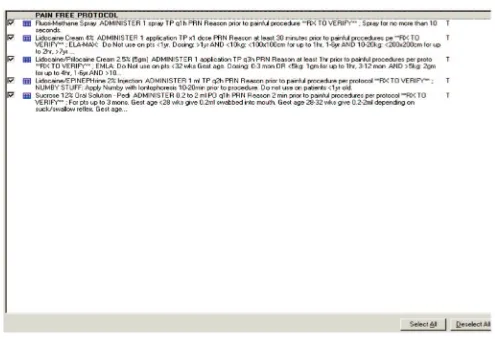
The second category created, drop-down menu selec-tion errors made with the computer mouse, led to 4 serious medication errors (eg, 900 g rather than 900 mg
of ceftriaxone) and 5 errors with little or no potential for harm (eg, ceftriaxone ordered “IP” rather than “IV”) (Fig 1). Three of the serious errors were orders for ceftriax-one overdoses that did generate computer error warn-ings. However, the physicians overrode the alerts and did not change or cancel the orders. In the fourth serious error, a medication was ordered erroneously for the wrong patient, whose name followed that of the in-tended patient alphabetically in the computer drop-down box. A nurse intercepted that error when the medication arrived from the pharmacy. None of these errors reached the patients.
There was only 1 keypad entry error, the third cate-gory created. The error was an order for ibuprofen at 5 mg rather than 50 mg. The error was considered serious because this patient was in septic shock in the PICU, and possible chronic underdosing of a fever medication for such a sick patient was not considered a trivial error. This error did generate a computer warning when the phy-sician wrote the order; the phyphy-sician overrode the alert and did not change or cancel the order. The nurse ad-ministered the appropriate dose, however.
The final category was order set errors, of which there were 8, all with little potential for harm. The newborn care order set contains standardized orders for hepatitis B vaccination, erythromycin eye ointment, vitamin K injection, diet, and bath. Housestaff members may click on a “select all” box to order all medications in this order set or may click on a “deselect all” box and then order medications individually. Seven order set errors were hepatitis B vaccinations ordered for premature infants of ⬍2 kg in the NICU. Consistent with the American Acad-emy of Pediatrics clinical report on immunization of
TABLE 3 Types of Medication Errors Caused by Design Features of the CPOE System Among 352 Pediatric Inpatients
CRE Type Description No. of
Serious Errors
No. of Errors With Little Potential for Harm
Duplicate medication order Two orders written for the same medication because the computer did not permit an order to be written as it would be in a paper system (eg, “acetaminophen oral solution 80 mg po q4 hours prn” and “acetaminophen infant drops 80 mg pr q4 hours prn”)
2 0
Drop-down menu selection error
Wrong selection from a drop-down box with a computer mouse (eg, ceftriaxone administered intraperitoneally rather than intravenously)
4 5
Keypad entry error Typographical error (eg, ibuprofen at 5 mg rather than 50 mg)
1 0
Order set errors Selection of orders from a standard order set that were not indicated for the individual patient (eg, hepatitis B vaccination for a 12-d-old NICU transfer who already received both)
0 8
preterm infants, hepatitis B vaccines were not adminis-tered in the NICU until the premature infants weighed 2 kg.21 One child was administered a hepatitis B vaccine
prematurely as a result of an order set error. The eighth order set error was an order for hepatitis B vaccination for a newborn who was transferred to the NICU from another hospital at 12 days of age and who had already received the vaccine at the other hospital.
Hazardous Orders From an Order Set
Hazardous orders (orders that introduced excess poten-tial for error but were not frankly erroneous themselves) facilitated by the CPOE system were also identified; these were specific to the nonnarcotic pain control order set (Fig 2). In total, there were 119 nonnarcotic order set
orders of 4% lidocaine and lidocaine/epinephrine for infants. Pediatrician reviewers considered these medica-tions hazardous in this age group but, because the order set contains text indicating that these 2 formulations should not be used for infants, these were not counted as errors. However, the text must be read carefully, in full, by nurses or a medication error could result.
In addition, there were multiple order set orders (both related and not related to the nonnarcotic pain control order set) that were not considered hazardous but did result in extra work. There were 189 orders for sucrose for pain relief for teenage patients, fluorometh-ane spray for pain relief for infants, and sunscreen for PICU patients in the winter, leading to extra work such as delivery of unnecessary sunscreen to the PICU. FIGURE 1
Screenshot demonstrating 2 drop-down menu selection errors. In the first error, the user selected grams of ceftriaxone, rather than milligrams, from a drop-down menu. In the second error, the user selected intraperitoneal rather than intravenous as the route. The 900-g dose generated a computer warning, which the physician overrode. These errors were later intercepted; the corrected order is written beneath the original order.
FIGURE 2
DISCUSSION
Among 6916 pediatric inpatient medication orders re-viewed, 20 pediatric inpatient medication CREs were detected. These errors constituted 19% of all pediatric medication errors in the hospital during the time period of study. Of these, 7 were serious medication errors, none of which was administered to the patient, and 13 were trivial medication errors, including a vaccine that was administered prematurely. Four of the 7 serious errors generated computer alerts that were overridden. In addition, there were 4 injuries attributable to ordering errors that were not CREs but also were not prevented by the CPOE system decision support.
Rates of serious pediatric medication errors in this study were slightly higher than in previous research using similar methods.5Our study included more NICU
patients than the previous study, and many of the pa-tients in inpatient wards in our study received narcotic medications because of trauma or sickle cell disease. The number of errors with little potential for harm in this study was lower than that in the previous study. The computer system might have prevented some errors with little potential for harm by preventing incomplete order writing.22
In contrast to a recent qualitative study by Koppel et al16
that identified 22 types of errors related to CPOE, we found only 4 types of CREs. Many of the system design problems described by Koppel et al16 were not found. Our study
hospital used a more-recent version of the same CPOE system described by Koppel et al.16Some of the problems
they described might be infrequent or specific to the older version of this system. Although we identified only a frac-tion of the error types described by Koppel et al,16 our
findings do support the assertion that problems with the human-machine interface can pose a risk to patients.
A limitation of this study is that it was conducted in a single hospital and, like the study by Koppel et al,16 it
focused on only 1 type of CPOE system; generalizability to other hospitals and systems is a concern. Although Eclipsys is the leading vendor of CPOE systems,23other
computer systems might not have some of the design limitations described. Some of the design features we describe, however, are common across CPOE systems, yielding drop-down menu selection errors and keypad entry errors. Order set errors may occur with any CPOE system that allows selection of the entire order set with a single mouse click on a “select all” button. Duplicate medication orders attributable to inflexible ordering screens result from computer constraints. Hospitals im-plementing CPOE should consider the possibility that constraints designed to prevent ordering errors can cause user “workarounds” that create new errors.
This study used rigorous methods of comprehensive chart review, medication order review, and incident re-port review. However, a second limitation is that, al-though our study was designed to capture all
medica-tion-ordering errors, some errors might have been missed, particularly given the retrospective design. Com-prehensive review for errors with current methods is not ideally suited for detection of drug administration er-rors18 or dispensing errors that are not noted in the
medical record. Ordering errors that were caught by the CPOE system and corrected before the resident signed the order would not have been recorded in the final orders and therefore were not reviewed. Reviewers, who were unaware of the study objectives, might have missed some CREs, but blinding avoided bias in estima-tion of the rate of CREs. Although undoubtedly this study missed some errors that occurred, our multi-pronged, active surveillance method provides informa-tion that adds substantially to previous qualitative re-search on CREs and to previous studies of pediatric CPOE that used incident reports or order review alone.8,10,16
Some of the CREs we detected were fundamentally different from previously described errors occurring at the point of care in paper ordering systems, in that they were not attributable to errors in human cognition or task execution. For example, in the case of some dupli-cate medication orders identified, it was impossible for users to write an order to give oral or rectal forms of acetaminophen as deemed appropriate by the nurses. Therefore, separate oral and rectal orders were written, which introduced the unintended potential for both to be given, yielding a twofold overdose. Many of the hu-man-machine interface errors resulted from a computer design that facilitated incorrect order writing. Correct order writing might have been difficult, more time-con-suming, or impossible.
The findings in this study must be placed in a larger context of continuous quality improvement. Although it is impossible to eliminate all errors, resilient interfaces of computers and health care workers should be created to ensure safe care. We found 4 preventable adverse drug events in ordering that were not prevented by the CPOE system. More-sophisticated decision support may pre-vent these ordering errors in the future.
Four CREs generated computer alerts that ordering physicians overrode. The computer log at the study site contained 17 alerts per admission overall. Overriding of alerts is a common problem; in one study, 80% of drug allergy alerts were overridden.24In some high-risk
situ-ations, more-specific alerts (such as, “You have written a dose that is 10 times the recommended dosage for this patient. Is this the dose you want to order?”) may pre-vent some CREs. To prepre-vent some serious errors, the newest version of the CPOE system in the study hospital will use hard stops that cannot be overridden, keeping in mind that users sometimes work around hard stops by using free-text orders. The best use of alerts in CPOE is a subject of research and continues to be refined.
To date, there is no established taxonomy of CREs. In attempting to describe CREs and some possible solutions, this and previous research16began to build a taxonomy
of CREs. Such taxonomy may allow hospitals imple-menting CPOE to monitor their own patients for these CREs or to anticipate and to prevent them.
Some of the CREs described may be unique to pedi-atrics. The order set errors, for example, occurred when a medication was ordered that was inappropriate for the child’s age. The duplicate-medication order errors oc-curred when a physician ordered 2 different concentra-tions of acetaminophen syrup. Pediatricians implement-ing CPOE at their own institutions should be mindful of the unique opportunities for error when computer sys-tems are applied to pediatric populations.
After implementation of CPOE, 19% of pediatric medication errors were CREs, although none resulted in patient injury. Hospitals implementing CPOE for pediat-ric use should be aware of this risk and should take steps to prevent the CREs described here. Many of these 4 types of CREs may be prevented by refining CPOE sys-tem design features, so that future CPOE syssys-tems used at other hospitals have fewer associated CREs.
ACKNOWLEDGMENTS
This work was supported by the National Library of Medicine (grant R03 LM008289-01) and the Boston Medical Center Risk Management Department. Dr Land-rigan is the recipient of a career development award from the Agency for Healthcare Research and Quality (grant K08 HS13333) and Dr Bauchner is the recipient of a career development award from the National Insti-tute of Child Health and Human Development (grant K24HD042489).
REFERENCES
1. Brennan TA, Leape LL, Laird NM, et al. Incidence of adverse events and negligence in hospitalized patients: results of the Har-vard Medical Practice Study I.N Engl J Med.1991;324:370 –376 2. Leape LL, Brennan TA, Laird N, et al. The nature of adverse
events in hospitalized patients: results of the Harvard Medical Practice Study II.N Engl J Med.1991;324:377–384
3. Miller MR, Zhan C. Pediatric patient safety in hospitals: a national picture in 2000.Pediatrics.2004;113:1741–1746 4. Institute of Medicine.To Err Is Human: Building a Safer Health
System. Washington, DC: National Academy Press; 2000 5. Kaushal R, Bates DW, Landrigan C, et al. Medication errors and
adverse drug events in pediatric inpatients. JAMA. 2001;285: 2114 –2120
6. Holdsworth MT, Fichtl RE, Behta M, et al. Incidence and im-pact of adverse drug events in pediatric inpatients.Arch Pediatr Adolesc Med.2003;157:60 – 65
7. Bates DW, Leape LL, Cullen DJ, et al. Effect of a computerized physician order entry and a team intervention on prevention of serious medication errors.JAMA.1998;280:1311–1316 8. Potts AL, Barr FE, Gregory DF, Wright L, Patel NR.
Comput-erized physician order entry and medication errors in a pedi-atric critical care unit.Pediatrics.2004;113:59 – 63
9. Lehman CU, Conner KG, Cox JM. Preventing provider errors: online total parenteral nutrition calculator.Pediatrics.2004;113: 748 –753
10. King WJ, Paice N, Rangrej J, Forestell GJ, Swartz R. The effect of computerized physician order entry on medication errors and adverse drug events in pediatric inpatients.Pediatrics.2003;112: 506 –509
11. Mullett CJ, Evans RS, Christenson JC, Dean JM. Development and impact of a computerized pediatric antiinfective decision support program. Pediatrics. 2001;108(4). Available at: www.pediatrics.org/cgi/content/full/108/4/e75
12. Upperman JS, Staley P, Friend K, et al. The impact of hospi-talwide computerized physician order entry on medical errors in a pediatric hospital.J Pediatr Surg.2005;40:57–59
13. Kilbridge P. Computer crash: lessons from a system failure.
N Engl J Med.2003;348:881– 882
14. Borden S.Computer Entry a Leading Cause of Medication Errors in US Health Systems. Rockville, MD: US Pharmacopeia; 2004 15. Han YY, Carcillo JA, Venkataraman ST, et al. Unexpected
in-creased mortality after implementation of a commercially sold computerized physician order entry system.Pediatrics.2005;116: 1506 –1512
16. Koppel R, Metlay JP, Cohen A, et al. Role of computerized physician order entry systems in facilitating medication errors.
JAMA.2005;293:1197–1203
17. Jha AK, Kuperman GJ, Teich JM, et al. Identifying adverse drug events: development of a computer-based monitor and compar-ison with chart review and stimulated voluntary report.J Am Med Inform Assoc.1998;5:305–314
18. Kaushal R. Using chart review to screen for medication errors and adverse drug events.Am J Health Syst Pharm.2002;59:2323–2325 19. Bates DW, Cullen DJ, Laird N, et al. Incidence of adverse drug events and potential adverse drug events: implications for pre-vention.JAMA.1995;274:29 –34
20. Landrigan CP, Rothschild JM, Cronin JW, et al. Effect of re-ducing interns’ work hours on serious medical errors in inten-sive care units.N Engl J Med.2004;351:1838 –1848
21. Saari TN. Immunization of preterm and low birth weight infants: American Academy of Pediatrics, Committee on Infec-tious Diseases.Pediatrics.2003;112:193–198
22. Bates DW, Teich JM, Lee J, et al. The impact of computerized physician order entry on medication error prevention.J Am Med Inform Assoc.1999;6:313–321
23. Eclipsys. Industry recognitions for Eclipsys solutions and cus-tomers. Available at: www.eclipsys.com/PDFs/Datasheets/ DTS%20208-Awards.pdf
DOI: 10.1542/peds.2006-0810
2006;118;1872
Pediatrics
Christopher P. Landrigan
Chessare, Maureen R. Cooper, Pamela M. Hebert, Elisabeth G. Schainker and
Kathleen E. Walsh, William G. Adams, Howard Bauchner, Robert J. Vinci, John B.
Medication Errors Related to Computerized Order Entry for Children
Services
Updated Information &
http://pediatrics.aappublications.org/content/118/5/1872
including high resolution figures, can be found at:
References
http://pediatrics.aappublications.org/content/118/5/1872#BIBL
This article cites 20 articles, 7 of which you can access for free at:
Subspecialty Collections
_sub
http://www.aappublications.org/cgi/collection/system-based_practice System-Based Practice
http://www.aappublications.org/cgi/collection/safety_sub Safety
following collection(s):
This article, along with others on similar topics, appears in the
Permissions & Licensing
http://www.aappublications.org/site/misc/Permissions.xhtml
in its entirety can be found online at:
Information about reproducing this article in parts (figures, tables) or
Reprints
http://www.aappublications.org/site/misc/reprints.xhtml
DOI: 10.1542/peds.2006-0810
2006;118;1872
Pediatrics
Christopher P. Landrigan
Chessare, Maureen R. Cooper, Pamela M. Hebert, Elisabeth G. Schainker and
Kathleen E. Walsh, William G. Adams, Howard Bauchner, Robert J. Vinci, John B.
Medication Errors Related to Computerized Order Entry for Children
http://pediatrics.aappublications.org/content/118/5/1872
located on the World Wide Web at:
The online version of this article, along with updated information and services, is
by the American Academy of Pediatrics. All rights reserved. Print ISSN: 1073-0397.