Volume 16
Number 6
Reports 541
nerve axons. In the acute phase such an injury may impair axoplasmic flow by mechanical or ischemic factors or both. In later, more chronic phases inflammation might also impair axoplasmic flow in the retrobulbar region. In this experi-mental model it is important to note that the effects of retrobulbar ligature of the optic nerve are most evident in the lamina retinalis where both the axonal cross-section diameter and the number of mitochondria per axonal cross-section are increased by approximately two times on the treated side. Although it is known that the mito-chondria have complex anterograde and retro-grade movements, with a net movement away from the globe,7 the findings can best be ex-plained by a general stasis of axoplasmic flow rather than any specific mitochondrial obstruc-tion as has been noted in the regions of the nodes of Ranvier and axonal terminals.8
Our experiment will provide a unique method for (1) study of the flow of 3H-leucine-labeled axonal protein, (2) assessment of possible dam-age to the blood-retinal barrier during the de-velopment of papilledema with the use of the horseradish peroxidase technique, and (3) de-termination of nerve conduction velocity in dis-tended axons. For such experiments, it will be convenient to have a normal half of the optic nerve from the same eye for comparison.
We thank Daniel L. Weiss, M.D., for photo-micrographs and the staff of the Animal Re-search Facility of the Veterans Administration Hospital, Lexington, Ky.
From the Surgery (Neurosurg
and the Department of Engineering Mechanics, College of Engineering, University of Kentucky, and the Veterans Administration Hospital, Lexing-ton, Ky. Supported in part by Fight for Sight, Inc., New York, N. Y., and the Veterans Admin-istration Hospital, Lexington. Submitted for pub-lication June 22, 1976. Reprint requests: J. D. Wirtschafter, M.D., Department of Ophthalmol-ogy, University of Kentucky Medical Center, Lex-ington, Ky. 40506. After July 1, 1977, Dr. Wirt-schafter may be addressed at University of Minnesota, Minneapolis, Minn. 55455.
REFERENCES
1. Wirtschafter, J. D., Rizzo, F. J., and Smiley, B. C : Optic nerve axoplasm and papilledema, Surv. Ophthalmol. 20:157, 1975.
2. Minckler, D. S., and Tso, M. O. M.: Experi-mental papilledema produced by cyclocryo-therapy, Am. J. Ophthalmol. 82:577, 1976. 3. Hogan, M. J., and Zimmerman, L. E.:
Oph-thalmic Pathology: an Atlas and Textbook, ed. 2, Philadelphia, 1962, W. B. Saunders Co., p. 587.
4. Tso, M. O. M., and Fine, B. S.: Electron Departments of Ophthalmology and eurosurgery), College of Medicine,
microscopic study of human papilledema, Am. J. Ophthalmol. 82:424, 1976.
5. Minckler, D. S., Tso, M. O. M., and Zimmer-man, L. E.: A light microscopic, autoradio-graphic study of axoplasmic transport in the optic nerve head during ocular hypotony, in-creased intraocular pressure, and papilledema, Am. J. Ophthalmol. 82:741, 1976.
6. Minckler, D. S., McLean, I. W., and Tso, M. O. M.: Distribution of axonal and glial elements in the rhesus optic nerve head studied by electron microscopy, Am. J. Oph-thalmol. 82:179, 1976.
7. Weiss, P. A., and Mayr, R.: Neuronal or-ganelles in neuroplasmic ("axonal") flow. I. Mitochondria, Acta Neuropathol. [Suppl.] 5: 198, 1971.
8. Webster, H. D.: Transient, local accumula-tion of axonal mitochondria during the early stages of Wallarian degeneration, J. Cell Biol. 12:361, 1962.
Sensory recording from the isolated cornea.
DAVID MARK AND DAVID MAURICE. A technique of recording from single units of the
isolated rat cornea is described. The corneal sur-face is stimulated by a jet of fluid, which allows continuously graded, pressure and thermal or chemical stimuli to be applied at the same point. Some units respond to stimulation anywhere in a field of about one-third the corneal area, and others only to point stimulation.
Only a few investigators have concerned them-selves with recording action potentials from the ciliary nerve in response to mechanical or thermal stimulus of the cornea.1"4 All have used intact eyes, which can lead to doubt whether an applied temperature stimulus is spreading to adjacent tissues, and their mechanical and thermal stimuli have been imprecise in their intensity or area of application. We will describe a method for re-cording sensory impulses in an isolated corneal preparation. This has the advantages that (1) it avoids any uncertainty whether a given nerve impulse arises from a sensory ending in the cornea or some other adjacent tissue and (2) it allows access to both sides of the preparation, permitting complete control of the temperature and chemical composition of the fluid bathing its surfaces.
An adult white rat was heavily anesthetized with sodium pentobarbital. The skin around the lids of an eye was incised, the cuts deepened and carried back into the orbit, and the eyeball was enucleated complete with the conjunctiva and lid margins. A thread was knotted around the margins so that the conjunctiva protected the corneal surface. The eye was pulled into a 5 mm. diameter hole punched into a circular disk of
Fig. 1. Method of mounting and stimulating cornea. A, Cornea protected by conjunctiva; eyeball pulled into hole in disc and glued. B, Contents of globe eviscerated. Sclera excised except for part carrying nerve. Surface of cornea stimulated with jet of fluid.
Fig. 2. Schematic diagram of cornea mounted in chamber. System of switching from a control jet to one carrying thermal or chemical stimulus is indicated.
Celluloid (Fig. 1, A). It was fixed in position by means of a very small amount of cyanoacrylate glue applied . around the sclera and limbus on either side of the disk (Fig. 1, B). The conjunc-tiva was then excised, and the disk sealed into a circular aperture between two chambers by means of silicone grease. A long ciliary nerve was iden-tified and brought to the top of the preparation
by rotating the Celluloid disk. The posterior globe was cut so as to create a tongue of sclera 2 mm. wide, which supported the external part of the ciliary nerve at its tip and carried the intraocular portion within it. The rest of the sclera was ex-cised, and the contents of the globe were carefully removed, with care taken not to evert or wrinkle the cornea.
Volume 16
Number 6
Reports 543
A) P = 200 mm Hg
B) P = 300 mm Hg
C) P = 900 mm Hg
Fig. 3A. Spike activity in a single preparation in response to jet exerting pressure. A) Below threshold; B) threshold; C) above threshold. Pressure labels correspond to driving pressure from gas cylinder.
A) T = 3 1 . 0 ° C
B) T = 3 5 . 5 ° C
C) T = 4 0 . 4 ° C
Fig. 3B. Spike activity in a single preparation in response to jet of constant velocity and delivered at temperature shown. Bath temperature 35° C.
The front chamber was filled with Ringer's solution, which covered the epithelial surface of the cornea (Fig. 2). This chamber was sealed and held at a suction about 15 cm. water below atmospheric so that the correct pressure relation-ship across the cornea was maintained. The fluid could be circulated through the chamber, entering
at the bottom and being sucked out at the top so that any air that leaked in was removed. Under normal conditions solution flowed through the chamber at about 5 ml./min. The rear chamber was open to the air and was also filled with Ringer's solution to a level above that of the cornea. Both front and rear chambers were
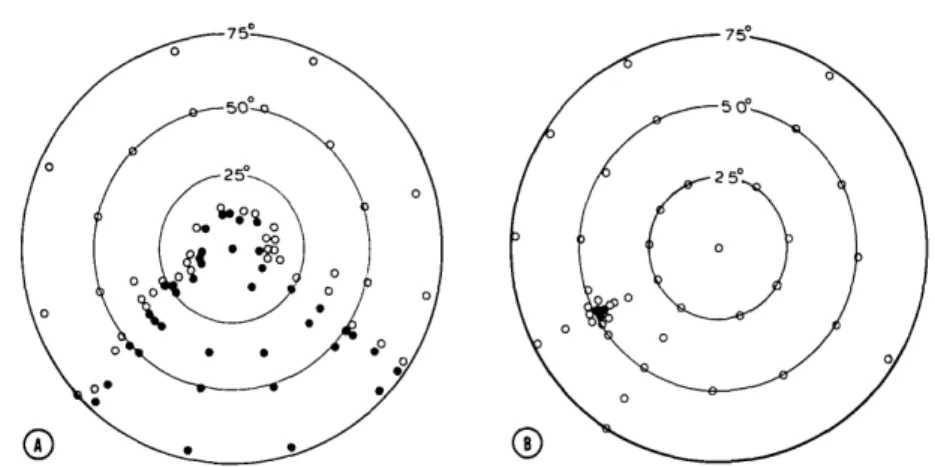
pro-Fig. 4. Two examples of areas of the corneal surface served by a single unit responding to jet pressure. A, Normal distribution. B, Point field. Filled circles, Points responsive to stimulus;
open circles, not responsive.
vided with heating jackets, and their tempera-tures were monitored with thermistors. Warm oil was circulated through the jackets in order to maintain the temperature of the tissue.
Action potentials from the dissected strands of the ciliary nerve were recorded through a platinum wire electrode; the indifferent platinum electrode was positioned in the solution bathing the nerve. The electrical responses were amplified and dis-played by conventional means.
A jet of fluid was used to stimulate the cornea. Two advantages were obtained with this arrange-ment. (1) A mechanical force could be applied which was reproducible, continuously variable, measurable in absolute terms, and probably less traumatic than contact with a solid object. (2) Precisely defined thermal, mechanical, and chem-ical stimuli could be applied simultaneously or successively to exactly the same spot on the sur-face of the cornea. This allowed receptor fields to be plotted and correlated for the different stimulus modalities.
The jet could be moved to any portion on the corneal surface, up to 75 degrees from the optic axis, by a mounting corresponding to that of an astronomical telescope, fitted on the front chamber and concentric with the assumed center of curva-ture of the cornea, 1 mm. behind the plane of the Celluloid disk. Scales on the movements of both elevation and azimuth allowed the position of the jet to be read to 0.5 degree, corresponding to about 30 n at the corneal surface. A hydraulic mechanism was provided to advance or retract the jet with respect to the corneal surface.
The pressure exerted by a jet of fluid of density
p impinging with a velocity v on a stationary
surface is given by pv2/2g. The threshold pres-sure required to mechanically stimulate the cornea is of the order of 1 gm./mm.2, corresponding to a water velocity of 450 cm./sec, and provision was made for velocities up to 10 times this. For
jet diameters below 200 |iim the Reynolds number does not exceed 6,000 for the largest velocities, and the flow at the jet tip should be laminar.5 The velocity profile across the tip should there-fore be parabolic. The jet was drawn down from PE 100 polyethylene tubing, and fluid was pro-pelled through it by means of a cylinder of com-pressed gas. The velocity was altered by adjusting the pressure with the normal control valve. The pressure distribution was calibrated by means of a sensor consisting of a small (100 /tm) hole drilled in a plastic contact lens and connected to a pres-sure transducer. A profile was obtained by mov-ing the jet across this surface with a micrometer. As far as mechanical stimulation is concerned, practical limitations on the upper diameter of the jet are placed by the large volume of fluid that would have to be delivered and drained off and on the lower diameter by the pressure head neces-sary to generate the required velocity. A diameter of 200 jtim was found to be a convenient compro-mise, but values one-tenth of this would probably be feasible. For thermal and chemical stimuli these requirements are considerably less stringent. The procedure for isolating and mounting the cornea has been completed in more than 50 preparations, and with experience, the time be-tween enucleation of the eye and first recording from the nerve has been reduced to 1 hr. About three fourths of the preparations gave rise to useful action potentials; in case of failure the other eye of the animal was available for use. Preparations survived for up to 7 hr. after mount-ing.
The spontaneous discharge from the nerve was formed of many low- and occasional large-ampli-tude spikes. On stimulation with a jet of fluid of sufficient velocity, several large spikes were gen-erally evoked, and more were elicited as the force was increased above threshold. With a jet of 1 sec. duration, the threshold velocity was
Volume 16
Number 6
Reports 545
equivalent to 1 gm./mm.2 on the average (Fig. 3A). This is similar to the threshold to stimula-tion with von Frey hairs in the rat.'1 The dis-charge was characteristic of fibers responding to the onset of the stimulus, and their duration, 0.4 to 0.5 msec, suggests they corresponded to A fibers. No attempt was made to study conduc-tion velocity in these experiments.
A spike that was elicited by stimuli just above threshold and which could be identified by its amplitude was used to map the receptor field. Such fields usually encompassed one fourth to one third of the corneal surface as described by Tower1 in the cat (Fig. A, A). Occasional recep-tors with very restricted field, less than 1 mm.2, were also found (Fig. 4, B). Since these are inherently less likely to be chosen for study, they may be more frequent than immediately apparent. Only preliminary investigations using thermal stimuli were carried out, but it was evident that raising or lowering the temperature of the jet a few degrees Celsius in comparison to that in the bath would elicit action potentials (Fig. 3, B). Responses to both mechanical and thermal stimuli were abolished shortly after the application of 0.5% proparacaine HC1 through the jet.
In addition to the A fiber responses noted above, a larger number of smaller spikes were observed both discharging spontaneously and responding to nociceptive stimuli. Although a definite identifica-tion has not been made, their duraidentifica-tion, 1 to 3 msec, suggests that these are C fibers. Recordings from such fibers in the cornea have already been noted.1
Mr. Gunther Kuhn fabricated the equipment used in these experiments.
From the Division of Ophthalmology, Stanford University School of Medicine, Stanford, Calif. This work was supported by NIH Grant EY 00431. Submitted for publication Dec 29, 1976. Reprint requests: Dr. David Maurice, Division of Ophthalmology, Stanford University School of Medicine, Stanford, Calif. 94305.
Key words: cornea, sensory nerves, sensation, re-ceptor fields.
REFERENCES
1. Dawson, W. W.: The thermal excitation of afferent neurones in the mammalian cornea and iris. In Hardy, J. D^ editor: Temperature —Its Measurement and Control in Science and Industry, New York, 1963, Reinhold Pub-lishing Co., pp: 199-210.
2. Lele, P. P., and Weddell, G.: Sensory nerves of the cornea and cutaneous sensibility, Exp. Neurol. 1:334, 1959.
3. Tower, S. S.: Unit for sensory reception in cornea, J. Neurophysiol. 3:486, 1940.
4. Trimarchi, F.: La sensibilita corneale alle variazioni termiche, Ann. Ottal. 93:592, 1967,
5. Schweitzer, P. H.: Mechanism of disintegra-tion of liquid jets, J. Appl. Physics 8:513, 1937.
6. Strughold, H.: The mechanical threshold of the cornea-reflex of the usual laboratory animals, Am. Physiol. 94:235, 1930.
Effect of vidarabine and related
com-pounds on corneal endothelium.
DAVID S. HULL, KAREN BOWMAN, AND KEITH GREEN.The endothelial surface of rabbit corneas was perfused with vidarabine monophosphate (with and without adenosine deaminase inhibitor), vidarabine (with and without adenosine deaminase inhibitor), and ara-Hx. In concentrations 10 times to 1,500 times higher than those that have been obtained in the aqueous humor following topical, subconjunctival, or systemic administration, none of the compounds had any effect on corneal endothelial cell function or ultrastructure for the duration of the experimental model.
Recent work has suggested that systemic ad-ministration of vidarabine (adenine arabinoside, 9-/?-D-arabinofuranosyl adenine, ara-A; Vira-A [Parke, Davis & Co., Detroit, Mich.]) is of benefit in treating some patients with herpes simplex kera-touveitis.1 Measurable aqueous humor levels of vidarabine and its metabolite ara-Hx (hypo-xanthine arabinoside, 9-/8-D-arabinofuranosyl hy-pcxanthine) have been demonstrated in these patients. However, the effect of vidarabine and related compounds on the corneal endothelium is not currently known. Since these drugs enter the eye, it is imperative to establish what dose levels are cytotoxic to the endothelium. This in-vestigation was conducted to determine the ef-fects of vidarabine and related compounds on corneal endothelial physiology and ultrastructure during in vitro perfusion.
Methods. Adult albino rabbits weighing about
3 kg. were killed with an overdose of intra-venous sodium pentobarbital. The eyes were enucleated together with conjunctival sac and eyelids, after which the corneas were mounted in a specular microscope.2"4 Using the specular microscope allowed constant perfusion of the corneal endothelium with Ringer's solution at a temperature of 37° C. and a pressure of 15 mm. Hg. Sequential observations of the corneal endo-thelium and measurements of corneal thickness were made every half hour. Silicone oil (Dow Chemical Co., Midland, Mich.) was placed on the epithelial surface. Corneal swelling rates were determined by linear regression analysis, and a comparison of experimental and control regres-sion lines was made by an analysis of