ANNUAL REPORT I. ASSESSMENT ACTIVITIES:
A. Program Goals
The goals of the St. Mary‘s/Marshall University Cooperative Bachelor of Science in Respiratory Care are congruent with the mission of Marshall University.
Our goals must also be congruent with St. Mary's Medical Center. Our goals were therefore revised and approved by the Faculty Organization in its May 2006 meeting. The revised goals also included objectives which are sealed in measurable terms.
(See Appendix A for the evaluation of the BSRT program goals for the 2005-2006 academic goals.)
A formal Systematic Evaluation Plan is in place for the St. Mary's/ Marshall University Cooperative BSRT Program. The components being evaluated include:
Mission and Governance Faculty
Student
Curriculum and Instruction Resources
Integrity
Educational Effectiveness
The assessment plan is implemented by ad hoc committees out of the St. Mary's Center for Education Faculty Organization. The program is scheduled to be evaluated by site visitors from the Committee on Accreditation for Respiratory Care (CoARC) during the fall of 2009.
A ―letter of intent‖ to start a BSRT program was submitted to CoARC and approved in September of 2004.
A thorough self-study was submitted to CoARC in May of 2005. CoARC reviewed the self study issued and approved the program to begin following a few revisions.
The school will have an on site visit by CoARC within six months following the graduation of the first class. There were three standards that CoARC sought revision of and those have been addressed.
(See Appendix B for letter from CoARC)
The faculty reviews the evaluation data to be used for program development, maintenance and revision.
Therefore, the faculty members of St. Mary's/Marshall University Cooperative BSRT Program have reviewed the revision of the standards and criteria and are in the process of updating the program's systematic plan.
The faculty approved a calendar for reviewing each component at the May 2006 meeting of the Faculty Organization. A revised template was also approved at this same meeting.
B./C. LEARNING OUTCOMES/DATA COLLECTION/RESULTS
The Committee for Accreditation for Respiratory Care (CoARC) is the recognized accrediting body for
Respiratory Care and has specific guidelines in the standards that a Respiratory Care program must demonstrate to be in compliance with the program outcome criteria.
These specific standards and goals of the Bachelor of Science Degree in Respiratory Care are incorporated into the courses. The course and clinical objectives reflect these competencies.
See Appendix D for course and clinical syllabi.
The program outcomes used to evaluate the Cooperative BSRT Program are performance on licensure
examination, job placement rates, program satisfaction, and graduation rates. Our outcomes and definitions were changed to reflect the CoARC outcomes.
Criteria for each of the required and selected outcomes are measured at the end of the program during the students' final semester.
In addition course evaluations are administered at the end of each semester. The results of these course
evaluations are reviewed by the faculty and any deficiencies are corrected and implemented int o the appropriate course instruction.
Definition of Outcomes:
1. Clinical Assessment:
Assessment is evaluated each semester for application of procedures that have or are presently being instructed.
If a negative review has been noted by a faculty member then the student is re-instructed in the procedure and re- evaluated by another faculty member. If the student is again found to be deficient the student is re-instructed by the faculty member. A final review is done with the student by the director of the respiratory care program. If it is determined the student is in fact deficient in the competency a failing grade will be recorded.
2. Licensure Pass Rate:
Performance on licensing examination (NBRC) is the percentage of graduates passing the NBRC entry level examination on the first attempt.
Defined Level of Achievement:
The BSRT program has not graduated any students at this point. At this time there is no information to submit. The currently enrolled class will not be eligible to sit for their examination until January 2010.
Our goal is for each class that sits for the NBRC entry level licensure examination that we will meet or exceed the national pass rate on their first attempt.
This data is collected from reports submitted to each school by the Committee on Accreditation for Respiratory Care.
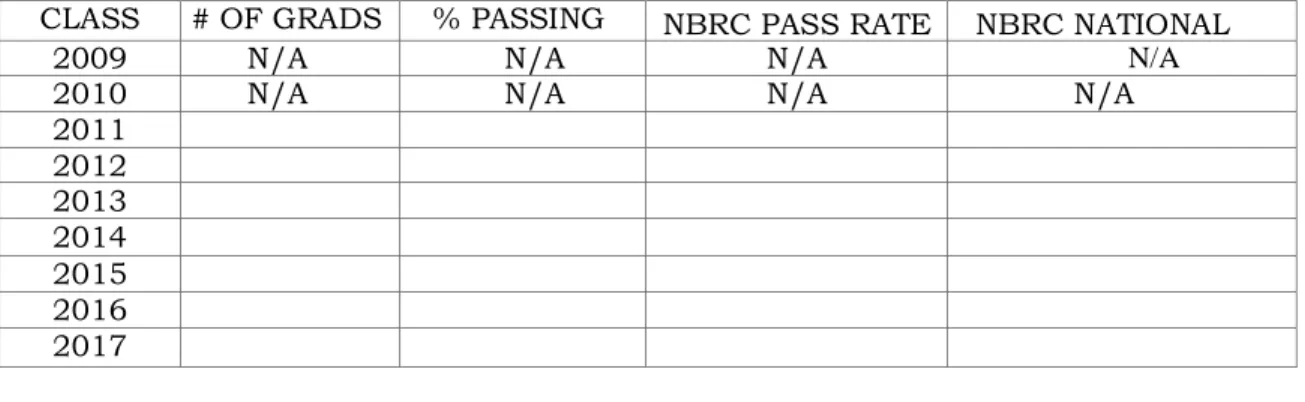
Table 1: Licensure Pass Rate
CLASS # OF GRADS % PASSING NBRC PASS RATE NBRC NATIONAL RATE
2009 N/A N/A N/A N/A
2010 N/A N/A N/A N/A
2011 2012 2013 2014 2015 2016 2017
Job Placement Rates: The first class will not graduate until December of 2008.
There is no information to report at this time.
Defined Level of Achievement:
90% or greater of graduates seeking employment as a CRT or RRT will be employed within 6 months of graduation.
This data is collected by the faculty.
The employment data does indicate that the graduates who are seeking employment do work as graduate CRT or RRT‘s.
Table 2, Job Placement Rates reflects this data.
Table 2: Job Placement Rates
CLASS # GRADUATES # EMPLOYED & % NO INFORMATION AVAILABLE
# NOT SEEKING EMPLOYMENT
2009 N/A N/A N/A N/A
2010 N/A N/A N/A N/A
2011 2012 2013 2014 2015 2016 2017 1. Program Satisfaction:
Program satisfaction is the degree to which the current students rate the effectiveness and quality of the Respiratory Care program. The students evaluate each course of instruction at the completion of the
semester and assigned a rating of 1-5 on a Likert scale.
Program satisfaction is the degree to which the graduates rate the effectiveness and quality of The Respiratory Care program.
Defined Level of Achievement:
Current students enrolled in the program evaluate each course of instruction at the completion of the semester and assigned a rating of 1-5 on a Likert scale.
Current students will indicate satisfaction with the program with 2.5 or higher on a Likert scale of 1-5.
To assess satisfaction with the class progression and the program, the St. Mary's School of Respiratory Care course evaluations is considered one of the primary sources of data.
Graduates will indicate satisfaction with the program with 2.5 or higher on a Likert scale of 1 -5. To assess graduate satisfaction with the program, the St. Mary's School of Respiratory Care Graduate Survey Questionnaire is one of the primary sources of data.
At this time there are no graduates from the school of respiratory care. The first survey is to be conducted in the summer of 2009.
The data collected will be trended and will indicate overall graduate satisfaction.
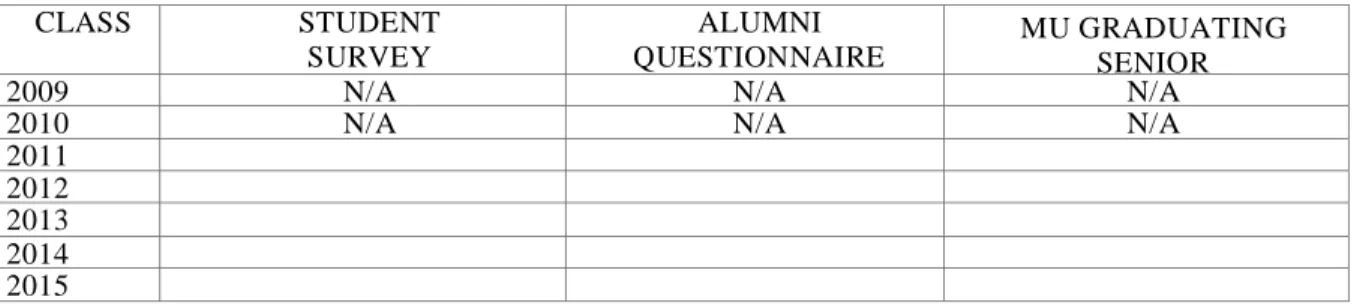
Table 3, Program Satisfaction illustrates the data.
Table 3: Program Satisfaction
CLASS STUDENT SURVEY ALUMNI QUESTIONNAIRE MU GRADUATING SENIOR QUESTIONNAIRE
2009 N/A N/A N/A
2010 N/A N/A N/A
2011 2012 2013 2014 2015
Likert Scale: 1 = Highest; 5 = Lowest
*Likert Scale: 5 = Highest; 1 = Lowest
**Percent of those responding to agree/valuable or higher ***Alumni Questionnaire results compiled for Classes of (N/A)
1. Graduation Rates:
Graduation rates are defined as the percentage of students successfully completing the program within four years.
75% or greater of students who enter the program will graduate within four years of the start of the program.
No graduation rates have been calculated since the first graduating class will not be complete all course requirements until December 2008 but will be based on criteria that the students must graduate in the specified time of four years.
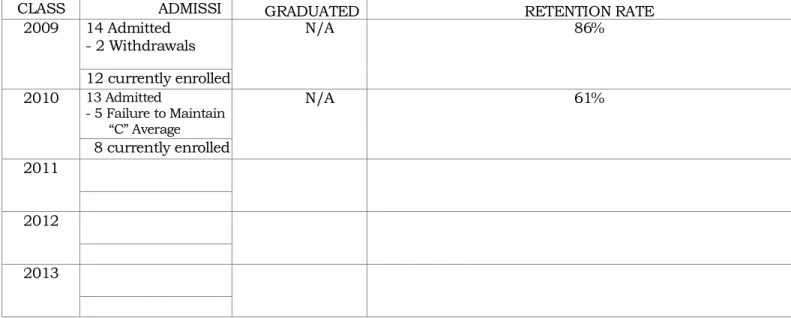
Table 4 demonstrates the admission/retention/graduation rates. This data is collected on a continual basis by the Director. This attrition report is filed annually with CoARC.
See Appendix E for annual report filed with CoARC.
The faculty of St. Mary‘s School of Respiratory Care is committed to be available to all students. Each student is assigned an advisor at the beginning of each year of the program. The faculty member meets during the year with each advisee.
The faculty also makes every effort to contact their respective advisees who are experiencing difficulty in the program to assess the problems and problem solve for solutions.
It is a requirement that any student scoring below a 75% on any unit exam meet with the assigned advisor to review the exam.
Table 4: Admission/Retention/Graduation Rates
CLASS ADMISSI
ONS GRADUATED RETENTION RATE
2009 14 Admitted - 2 Withdrawals N/A 86% 12 currently enrolled 2010 13 Admitted - 5 Failure to Maintain ―C‖ Average N/A 61% 8 currently enrolled 2011 2012 2013
2014
Academic difficulty is not the only reason a student may withdraw from the program. It is important to look at the number of students who withdraw for other reasons.
Table 5 demonstrates reasons for withdrawal over the past 3 years.
Table 5: Reason for Withdrawal
St. Mary‘s/Marshall University will make graduation comparison rates with the ACT news release (www.act.org) once the first class has graduated
Table 6
Retention Rates for NCAA
At the end of each semester, the St. Mary's Bachelor of Science Academic Planning and Standards Committee reviews course and clinical syllabi for activities and evaluation criteria related to the learning outcomes.
Copies of course syllabi are submitted with this report.
See Appendix F
In order to successfully complete the required courses, students must demonstrate the satisfactory achievement of the following learning outcomes from the RRT NBRC Job Matrix:
CLASS ACADEMIC HEALTH PERSONAL OTHER
2009 0 0 2 0
2010 4 N/A 1 N/A
2011 N/A N/A N/A N/A
2012 N/A N/A N/A N/A
2013 N/A N/A N/A N/A
2014 N/A N/A N/A N/A
2015 N/A N/A N/A N/A
2016 N/A N/A N/A N/A
2017 N/A N/A N/A N/A
Class Public Institutions Private Institutions All Institutions
2012 N/A N/A N/A
2011 N/A N/A N/A
2010 N/A N/A N/A
See Appendix G
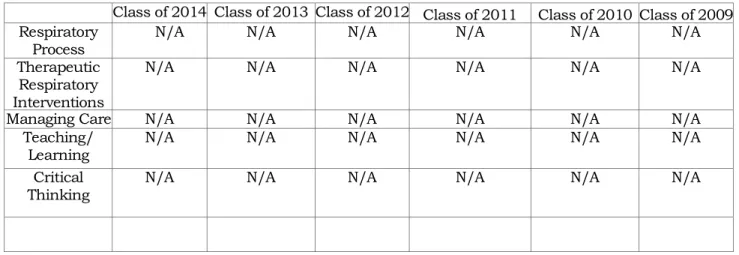
Table 7 illustrates the data that will be obtained from St. Mary's/Marshall University Graduate Questionnaire.
Table 7: Learning Outcomes
Class of 2014 Class of 2013 Class of 2012 Class of 2011 Class of 2010 Class of 2009 Respiratory
Process N/A N/A N/A N/A N/A N/A
Therapeutic Respiratory Interventions
N/A N/A N/A N/A N/A N/A
Managing Care N/A N/A N/A N/A N/A N/A
Teaching/
Learning N/A N/A N/A N/A N/A N/A
Critical
Thinking N/A N/A N/A N/A N/A N/A
Likert Scale: 1 = Excellent; 5 = Poor
At the end of each course, students complete evaluations of the course. The required learning outcomes are a part of these evaluations.
See Appendix - Course Evaluations
Prior to graduation, students complete a written evaluation of the BSRT program. This evaluation also includes the learning outcomes.
Graduating students also complete the Marshall University Graduating Student Outcomes Questionnaire. This survey was not available at the time this report was completed.
Performance on NBRC Entry Level Examination is described in Section II, Senate Bill 653 Compliance, and also in Table 1 in Section I.
II. SENATE BILL 653 COMPLIANCE:
St. Mary's/Marshall University Cooperative BSRT Program meets the requirements of Senate Bill 653. The program implements a Systematic Evaluation and evaluates achievement of goals annually. Both the Systematic evaluation and the goals are attached to this report in the appendices.
licensing examination (NBRC Entry Level).
The benchmark established by the faculty of the St. Mary's/Marshall University Cooperative BSRT Program is:
To meet or exceed the cut score established by the NBRC on their first attempt. This cut score changes from examination to examination based on national pass rates for all candidates.
See Table 1 in Section I.
III. PLANS FOR THE CURRENT YEAR:
The plans for the 2007 — 2008 academic year include the implementation of the Systematic Program Evaluation Plan in the areas of Mission and Governance, Curriculum, and Evaluation. This will be done during the Fall of 2008 semester.
A comprehensive standardized testing package will begin with the Class of 2009.
The tests are produced by the National Board for Respiratory Care (NBRC).
Beginning in the Fall of 2008, prior to the first day of class, every respiratory student will be required to take three tests:
1. Test of Essential Academic Skills (TEAS)
2. Critical thinking
3. Self Assessment Inventory.
Students who do not achieve pre-determined scores on these tests will be required to attend Strive for Success classes weekly for 10 weeks.
Strive for Success classes were developed by two nursing faculty members from the St. Mary‘s Center for Education. The classes will focus on study skills, learning styles, etc.
Also, each student who does not pass a unit exam with a 76% or above will be required to meet with the instructors who developed the test and complete a remediation assignment.
The Goals for 2007 – 2008 academic years are included in Appendix F.
IV. ASSISTANCE NEEDED:
The continued timely return of course and graduate evaluation data is greatly appreciated.
V. IMPORTANT THING LEARNED:
As with any assessment, the faculty members always find that program strengths and weaknesses are identified. Therefore, the faculty can try to correct weaknesses and continue to build upon strengths.
The faculty members continue to work diligently to assist students who are having academic difficulty. We did revise our criteria for admission to the school for the next pool of applicants. It will be interesting to see if that assists in increasing our retention rate.
The chart titled "Assessment of Student Outcomes: Component/Course/Program Level" is completed and may be reviewed below.
Marshall University
Assessment of Student Outcomes: Component/Course/Program Level
Component Area/Program/Discipline: St Mary's/Marshall University School of Respiratory Care
Student Outcomes as
Required by CoARC Person or Office Responsible Assessment Tool or Approach Standards/ Benchmark Results Analysis Action Taken
Job Placement Rates Chuck Zuhars, Director, And Brent Blevins, Clinical Director & Faculty & Faculty Graduate/Employer Survey Roster with names
and places of employment ent. 80% or greater of respiratory graduates seeking employment as a CRT or RRT will be employed within 6 months of graduation N/A N/A Performance on Licensure Examinations Chuck Zuhars, Director, And Brent Blevins, Clinical Director
Data from National Board of
Respiratory Care (NBRC) Mary’s/Marshall St. University School
of Respiratory graduates will meet or exceed the cut score as set by the NBRC student pass the
on the first attempt.
Graduation Rates Chuck Zuhars, Director, And Brent Blevins, Clinical Director
Roster of names with
data. 75% or greater of students who
enter the program will graduate within
four years.
N/A N/A
Program Satisfaction Chuck Zuhars, Director And Brent Blevins, Clinical Director St Mary's Graduate
Questionnaire. Graduates will indicate satisfaction with the program with an average of 2.5 or greater on scale of 1-5. (Liked Scale: 1 = highest;5 = lowest) N/A N/A
Appendix
A
St. Mary's/Marshall University Cooperative School of Respiratory
BSRT Program Goals and Objectives:
Service
1. Maintain a satisfactory graduation rate. a. Achieve a graduation rate of 80% or greater.
The first class does not graduate until December 2008. There are no statistics to report.
2. Provide academic support to students at risk of academic failure. a. Continue enhancing the existing services and resources for the
students.
Goal Met:
enhance their learning experience.
The Center for Education has purchased various manikins to enhance the students experience and training level prior to practice in the clinical area.
The Center for Education has purchased periodicals to enhance and support their learning experience. This information is located in the student library.
b. Identify at risk students and assist them with a remediation plan that will assist them in achieving success in the respiratory program .
Goal Met:
The faculty of the School of Respiratory Care has a mandatory conference with the students at mid term.
Weaknesses are identified at this point and discussed with the student. A remediation plan is designed and available for the student and assistance is rendered by the faculty to enhance the students learning experience.
Quality
1. Faculty will maintain membership in professional organizations. a. All faculty will be a member of a professional organization.
Goal Met:
All faculty members are members of the American Association of Respiratory Care and the National Board for Respiratory Care.
b. Fifty percent (50%) of faculty will serve in a leadership role (officer, board member, committee member) in a professional organization.
Goal Not Met:
2 faculty members have had the opportunity to be nominated for a leadership role in the West Virginia Society for
Respiratory Care. The formal election has not been held as of this report.
standardized tests.
a. Meet or exceed the national mean on standardized tests.
There has not been a graduating class from the School of Respiratory Care. The first class will graduate in December 2008.
3. Graduates will be prepared for entry level CRT/RRT positions as indicated by the National Board of Respiratory Care (NBRC).
a. The graduates will meet or exceed the national pass rate as determined by the National Board of Respiratory Care (NBRC).
There has not been a graduating class from the School of Respiratory Care. The first class will graduate in December 2008.
4. Maintain graduate satisfaction with the program.
a. The graduates will rate "program satisfaction" as a 2 or below on the St. Mary's Graduate Questionnaire.
There has not been a graduating class from the School of Respiratory Care. The first class will graduate in December 2008.
5. Enhance critical thinking skills.
a. The graduates will have a group mean score on the ATI Critical Thinking EXIT EXAM that meets or exceeds the ATI Critical Thinking ENTRANCE EXAM group mean.
This testing phase will begin with the class that enters in the Fall of 2007.
6. Implement the PDA bulk-buying program for all incoming Year I students.
Goal Met:
Financial
1. Enhance financial resources.
a. In collaboration with the SMMC Foundation, submit a grant through the Center for Education Grant Committee for student or faculty use.
Goal Met:
The faculty members of the School of Respiratory Care have participated in several grant applications to benefit the Center for Education.
2. Faculty will support the capital campaign for the Center for Education.
Goal Met:
The faculty members have participated in activities that directly support the capital campaign.
3. Faculty will seek support of area clinical affiliates to secure donations of supplies and equipment.
Goal Met:
The faculty and staff have solicited and obtained donations to assist the School of Respiratory Care.
People
1. Caring will be a concept of the curriculum.
a. Students will rate the courses as enhancing the "ability to be a caring professional" as evidenced by a mean of 2.5 or less on the St. Mary's Course Evaluation.
Goal Met:
The students complete course evaluations at the completion of each semester. The course evaluations have a rating for understanding of students needs. The faculty rating in this area is continues to rate above the cut score.
2. Student communication skills will be developed.
a. Students will rate the courses as facilitating "the development of my
communication skills" as evidenced by a mean score of 2.5 or less on the St. Mary's Course Evaluation.
Goal Met:
The students complete course evaluations at the completion of each semester. The course evaluations have a rating for understanding of students needs. The faculty rating in this area is continues to rate above the cut score.
Growth
1. Demonstrate a continued need for the BSRT Program.
a. Recruit a pool of qualified applicants for each space in the program. Total space allocation for the program is 15 students.
Goal Met:
The School of Respiratory Care has met the number of qualified applicant for the currently enrolled class and for the class beginning in January 2007.
The sophomore class had 14 students enrolled. The current enrollment is 12.
1 student dropped because she married and moved out of the state. 1 student dropped and changed her major to elementary education. The freshman class had a total enrollment of 13 students
1 student dropped due to personal reasons
4 were dropped due to failure to maintain a “C” average
b. Ninety percent (90%) of the graduates seeking a position in respiratory care will have a job offer within 6 months of graduation.
Care. The first class will graduate in December 2008
2. Demonstrate a plan to enhance the physical facilities of the School of Respiratory Care.
a. Faculty will continue to participate in the planning for the Center for Education.
Goal Met:
The Respiratory Care program has been moved to another section of the school and has doubled the space previously held. There is ample space provided for the classes and labs to be conducted.
The faculty of the School of Respiratory Care has been actively involved with the planning committee for the new Center for Education.
The faculty have provided input and assisted with the allocated space for classroom and labs for their program.
3. Implement a plan to address the respiratory shortage.
a. Achieve and implement a plan to attract the CRT‘s employed within a 50 mile radius of the school and recruit them for enrollment into the RRT program.
Goal Met:
Dr. Shelia Kyle, Vice President, School of Nursing and Health Professions, and St. Mary’s Center for Education and the faculty of the School of Respiratory Care have worked diligently this academic year and have seen qualified applicants for admission increase. Community
a. All faculty will participate in a community health related activities.
Goal Met:
The faculty members have participated in health fairs throughout the tri-state area to promote health and wellness for the population of our service area.
2. Enhance the students' ability to provide service to the community. a. All students will participate in a community health project.
Goal Met:
Students will be assisting with the community health fair conducted in December of 2007. The respiratory care students will be working in unison with the nursing and radiology students.
b. Students will rate the courses as enhancing the "ability to provide service to the community" as evidenced by an average score of 2.5 or greater on a Likert scale of 1-5 on the St. Mary's Course Evaluation.
Goal Not Met:
B
Sp o ns or ed By:
The American Association of Respiratory Care • The American College of Chest Physicians The American Society of Anesthesiologists • The American Thoracic Society
Executive Office
MEMORANDUM
TO: St. Mary's Medical Center FROM: Richard T. Walker, MBA, RRT
CoARC, Executive Director SUBJECT: "APPROVAL OF INTENT"
Date: September 16, 2004
This "Memorandum" serves as formal approval to begin the process of establishing an educational program in Respiratory Care. Please be advised that a qualified Program Director should be appointed and will be responsible for of the initial review process. The initial review process will consist of the following:
1. Self-Study #1 — For Programs seeking a "Letter of Review" 2. Self-Study #2 — For programs seeking "Initial Accreditation" 3. The On-Site Visit, to occur after the program's first class graduates 4. Response to the Site Visit Report following the On-Site Visit
The following items can be found on the CoARC Web Site: www.coarc.com
1. The CoARC Standards and Guidelines for the Profession of Respiratory Care
2. CoARC Accreditation Handbook — see "New or Re-Accreditation" section
NOTE: The Program Director should feel free to call me for any assistance needed during the remainder of the accreditation process (817-283-2835, Ext. 101).
1248 Harwood Road • Bedford, Texas 76021-4244 (817) 283-2835 • Fax (817) 252-0773 • (800) 874-5615
June 9, 2005
Chuck Zuhars, RRT, MS Program Director Respiratory Care Program
St. Mary's School of Respiratory Care/ Marshall University 2900 is! Avenue
Huntington, West Virginia 25755
Dear Mr. Zuhars: RE: 200506
preparation for your next self study and your annual program evaluation, please re-address the following Standards. Standard V. A. 2. Fair Practices
Program accreditation status must be stated in the college catalog. Note the following statement which should be in the college catalog. Any information that you send prospective students must also include program accreditation status. Program Statement:
The Respiratory Care program is accredited by the Commission on Accreditation of the Allied Health Education Programs (CAAHEP), in collaboration with the Committee on Accreditation for Respiratory Care (CoARC), 1248 Harwood Road Bedford, TX 76021, 1-817-283-2835, http://www.coarc.com/.
Standard III. A. Resources, Type & Amount and B. 1Key Administrative Personnel
I am concerned with the limited administrative hours for the program director and director of clinical education as well as the very high (10:1) lab and clinical teaching ratios. Please consult with your administrative officers regarding adjustments in both these areas.
Standard III, D Resource Assessment
I wish to advise you to include the advisory committee members in your surveying. Please refer to the CoARC evaluation instruments Web page which states that the Personnel-Program Resource Survey, edition 3-2003, is to be administered annually at the program advisory Board meeting. This survey instrument is to be completed by program faculty, the Medical Director, and advisory board members. I also recommend revising your purposes statements for the library to include computer resources and electronic reference materials and financial resources to include fiscal support for the retention of personnel and the acquisition and maintenance of equipment and supplies.
Please call me at (727) 341-3627 or reply via email should you require further assistance. Send your documents electronically or in hard copy form to the CoARC Executive Office and to me.
Sincerely,
Stephen Mikles, EdS, RRT Referee
Appendix
C
Standardized Progress Report Questions - Program Attrition
% Success
Directions to the Program: The following questions have been developed by CoARC to guide your analysis and action plan, directed toward improving your outcomes on Program Attrition. Your Threshold Level of Success results on this outcome have triggered an accreditation dialogue consisting of assigning a referee and requiring this progress report. The referee is available to assist
you with your preparation of this report and the identification of possible changes to improve your attrition results. REMINDER: Upon completion of these questions, please forward a copy
electronically to the Executive Office and Referee. Each program is encouraged to utilize the NBRC electronic filing system.
Program Name: St. Mary's/Marshall University School of Respiratory Care CoARC Program Number: 200506
Your referee is: Stephen Mikles
The progress report is due by: September 2009
For those Students leaving for non-academic reasons:
1. Could the attrition have been predicted at the time of the student's admission? For example, did the student expect to work part-time or full time during the program? Did the student have inadequate language skills to complete the program? If the answer is yes to any of the above, was the student adequately counseled about the rigors and time requirements of the program?
The attrition of students could not be predicted at the time of admission. 1 student in the class of 2008 entered the program with aspirations of being in respiratory therapy.
After attending the introductory classes she made the decision that respiratory care was not what she wanted to do as a career.
The student in the class of 2009 dropped because of personal reasons that she stated was not due to anything or anyone in the program. She stated it was purely for personal reasons she did not feel free to discuss.
The 2nd student was engaged to be married when accepted in the respiratory class. During the summer 2006 session her fiancé accepted employment in another state and she withdrew to move out of state with him.
The other 4 students in the class of 2009 were forced to leave the program for academic reasons. All 4 students stated they did not realize the complexity of the program and due to other commitments this greatly decreased their performance.
All the students had the appropriate language skills to be successful in this program. All the students were counseled prior to admission to the respiratory care program as to the time commitment required to be successful in this program.
2. Did the student know what he/she was getting into? For example, does the program require prospective students to `shadow' a Respiratory Th erapist at one of its clinical sites before acceptance into program? Were potential or alleged health hazards explained to the student prior to acceptance? Does the program require a prospective student to speak with current students to get a feel for the physical and academic rigors of the program and profession? If some of the mandatory clinical sites are extremely distant, was this made clear to the student prior to admission?
It is the opinion of both the Program Director and the Director of Clinical Education that all the students were explained the processes and commitment required to be successful in the respiratory program. It is a requirement of our program that prior to entry they must attend a shadowing experience at a local hospital.
The potential hazards of the respiratory care field were explained in depth prior to acceptance into the program as well as information presented in the class room.
At this time it is not required for the prospective student to speak with previous classes . We did strongly recommend that they contact respiratory therapists at local hospitals to further explore the field.
Due to our program being located in rural Appalachia, we did address the issue of travel distance required to attend some of our distant clinical sit es.
3. Was adequate and timely financial aid and personal counseling available to students? Did students have a clear understanding of all financial requirements of the Program prior to admission? Do students in the program have access to all services avai lable to students in other programs?
The students did have available to them a financial aid counselor. Our financial aid counselor does assist the students through the whole process to insure their process is done correctly and is not an unpleasant experience
The financial requirements are explained in depth by our financial aid counselor prior to admission to the program. This process is a very important commitment for our students and is necessary for the student to understand.
The students in the respiratory program have the same privileges and availability of services as any other student in any of our other allied health programs.
4. Were students apprised of professional behavioral expectations prior to admission? Were students adequately counseled as to the significance and importance of these behaviors as problems occurred?
program. This was reinforced in the introductory academic classes as well. The students did not exhibit any behavioral problems
For students who leave for Academic reasons:
1. Could this have been predicted prior to admission based upon the student's prior academic performance? If so, was the student counseled that such an outcome was likely?
The admissions director does a very thorough job screening applicants that may have difficulty in progressing in this program.
Once the admissions director screens the applicants for all admissions criteria, the Vice President for the Center for Education, the Program Director and the Director of Clinical Education also review the applicants for admission.
2. If the program has data demonstrating that a certain level of academic competence (e.g., GPA, aptitude tests) is required to succeed in the program, is this information used to set entrance requirements? In institutions with an "open admissions" policy, do all programs have the same academic entrance requirements?
The Nursing program and the Respiratory Program do have the same admissions requirements.
3. Does the program use non-respiratory prerequisite courses as a predictor of success?
Yes
4. Are students regularly informed and counseled about their academic progress? Is academic counseling and systematic remediation (e.g., tutoring) available for students who are having difficulties?
Yes, all students not successfully passing an examination are remediated and retested to ensure academic success.
5. Can academic difficulties be traced to a particular instructor (didactic, laborato ry, or clinical rotations)? Does the program regularly evaluate all of its instructors (e.g., Resource Assessment, course evaluations) and address any problems identified?
No. All students are given a course evaluation to complete at the end of the semester. The instructors are rated on a Likert scale of 1-5. No deficiencies have been noted as of this date.
6. Can the students' academic difficulties be traced to a particular instructor or course (regardless of instructor)?
No
S T A N D A R D P R O G R E S S R E P O R T F O R M A T T R I T I O N
Program Name: Marshall University/St. Mary's Medical
Center - School of Respiratory Care CoARC Program # 200506
Was attrition due to: x General Education Courses x RT Core Courses
X Non-Academic
Analysis:
The Program Director and the Director of Clinical Education feel that adequate pre admission qualifications are in place. There is no way to predict family situations (marriage)that occur in an individuals life and the subsequent timing of this.
The student that left for a change of major, we did see some indicators after class began that maybe this was not the appropriate career for this student. The student who left for personal reasons would not reveal the circumstances that forced her to leave. The students that were unable to advance for academic reasons did not realize the time commitment required for this course of study.
Action Plan:
The faculty are going to reevaluate the form used for shadowing and see if it adequately covers what is required for a therapist to perform their functions.
Date Expected to Re-evaluate: Fall 2008
Revised November, 2002
2007 PROGRAM RESOURCE ASSESSMENT
RESOURCE: ADVISORY COMMITTEE
PURPOSE(S):
To actively develop, promote, support and evaluate the goals of the respiratory therapy program.
MEASUREMENT SYSTEM(S):
1. Program Personnel Program Resource Survey 2. Advisory Committee Minutes and Actions.
1. May of each year. 2. May of each year.
RESULTS: 2007
The advisory Committee felt like the goals and objectives were met for the academic school year.
ACTION PLAN(S):
No actions were noted to be taken
2007 PROGRAM RESOURCE ASSESSMENT
RESOURCE:
MEDICAL DIRECTORPURPOSE(S):
1. To provide input into curriculum including review of appropriateness of medical content.
2. To provide review of selected respiratory care topics in a format that encourages student interaction with a physician.
the evaluation of student attainment of these skills.
MEASUREMENT SYSTEM(s):
Program Course and Resource Survey(s) completed by the students.
Program Resource Survey completed by the faculty and advisory committee. Medical Director written evaluation(s) of student communication skills.
DATE(S) OF MEASUREMENT:
Program Resource Surveys are completed annually at the end of the spring semester.
Course Surveys are completed at the end of each semester.
Medical Director evaluation of student "communication skills"-Minimum of once per semester.
RESULTS: 200
1. No deficiencies were noted in the medical direction of the program.
ACTION PLAN(S):
It was the consensus of the Program full-time personnel that no specific changes in medical director activities were indicated based on the 2007 assessments.
2007 PROGRAM RESOURCE ASSESSMENT
RESOURCE: FACULTY
Program Director: To provide classroom, lab, and clinical instruction and to coordinate the overall program activities.
Director of Clinical Education: To provide classroom, lab, and clinical instruction and to coordinate the clinical education of the students.
Additional Full-time Faculty: To teach selected classroom and labs and to supervise the clinical rotation at various clinical sites.
Adjunct Clinical Faculty: to provide focused review on specific procedures and provide "formative evaluations" in the clinical setting.
Medical Director: See Medical Director Resource Assessment.
MEASUREMENT SYSTEM(S):
Program Resource Survey(s) completed by the students.
Program Personnel Resource Surveys completed by the faculty,
Note: Starting in 2006, also by: advisory committee, and Medical Director.
DATE(S) OF MEASUREMENT:
Student Exit/Resource Survey: End of each academic year (May)
Advisory Committee and Medical Director Survey: Spring Advisory meeting.
RESULTS: 2007
No deficiencies were noted.
ACTION PLAN(S):
1. Will monitor feedback on faculty performance by students.
2. Implement newest CoARC Program resource surveys this academic year, that include feedback from advisory committee and Medical director.
RESOURCE:
Support PersonnelPURPOSE(S):
To provide adequate secretarial support for primary program faculty.
MEASUREMENT SYSTEM:
Faculty Resource surveyDATE(S) OF MEASUREMENT:
Program Resource Surveys are completed annually at the end of the spring semester.
RESULTS: 2007
Faculty felt there was not enough secretarial support for the program.
ACTION PLAN(S):
2007 PROGRAM RESOURCE ASSESSMENT
RESOURCE:
PHYSICAL RESOURCES / LABORATORYPURPOSE(S):
1. To provide adequate physical resources (classroom and lab) for effective delivery of the program curriculum.
2. To provide each student an opportunity to practice with equipment and procedures prior to being responsible for the equipment or skill in the clinical environment.
MEASUREMENT SYSTEM(s):
Program Resource Survey(s) completed by the students. Program Resource Survey completed by the faculty.
DATE(S) OF MEASUREMENT:
Program Resource Surveys are completed annually at the end of the spring semester.
RESULTS: 2007
The students there was not adequate space for classrooms and lab.
ACTION PLAN(S):
The respiratory care department was moved to a larger area on the 3rd floor of the center for education.
2007 PROGRAM RESOURCE ASSESSMENT
RESOURCE:
LABORATORY – EQUIPMENT & SUPPLIESPURPOSE(S):
1. To provide adequate laboratory resources (equipment and supplies) for effective delivery of laboratory exercises.
2. To provide each student an opportunity to practice with equipment and procedures prior to being responsible for the equipment or skill in the clinical environment.
MEASUREMENT SYSTEM(s):
Program Resource Survey(s) completed by the students. Program Resource Survey completed by the faculty.
DATE(S) OF MEASUREMENT:
Program Resource Surveys are completed annually at the end of the spring semester.
RESULTS: 2007
The respiratory students felt there was not adequate space allocated for the laboratory exercises.
ACTION PLAN(S):
The respiratory class room and lab was moved to a larger area on the 3rd floor for the center of education.
2007 PROGRAM RESOURCE ASSESSMENT
RESOURCE: LEARNING RESOURCES
PURPOSE(S):
1. To provide a quiet place to study (Library).
2. To provide reference material when required to complete class assignments. 3. To provide sufficient computer support for students to complete assignments
(computer lab).
MEASUREMENT SYSTEM(S):
Program Resource Survey(s) completed by the students. Program Resource Survey completed by the faculty.
DATE(S) OF MEASUREMENT:
Program Resource Surveys are completed annually at the end of the spring semester.
RESULTS: 2005
ACTION PLAN(S):
No action necessary
2007 PROGRAM RESOURCE ASSESSMENT
RESOURCE: FINANCIAL RESOURCES
PURPOSE(S):
To provide adequate financial support to support program needs as identified during the various outcome (product) assessments.
MEASUREMENT SYSTEM:
Faculty Resource surveyProgram Resource Surveys are completed annually at the end of the spring semester.
RESULTS: 2005
The faculty felt more money should be allocated to capital purchases for the laboratory.
ACTION PLAN(S):
A proposed increase in the budget for fiscal year 2009 will be submitted.
2007 PROGRAM RESOURCE ASSESSMENT
RESOURCE: CLINICAL RESOURCESPURPOSE(S):
St. Mary’s Medical Center:
To provide sufficient clinical experience at a large teaching medical university in order to: (1) develop the student's ability to perform respiratory critical care procedures as identified in the
program's clinical activities summary log.
(2) facilitate the student's development of patient assessment skills. (3) develop students "physician interaction" skills
(4) provide clinical instruction with periodic "formative evaluations" to assist the student and the program in identifying progress in clinical skills development.
All other clinical affiliates (except Neonatal Intensive Care Units):
To provide sufficient clinical experience at teaching and community hospitals in order to:
(1) develop the student's ability to perform respiratory care procedures as identified in the program's clinical activities summary log.
(2) facilitate the student's development of patient assessment skills. (3) develop students "physician interaction" skills
Neonatal Intensive Care Units:
To provide sufficient clinical experience in Neonatal Intensive Care in order to: (1) familarize the student with neonatal respiratory care.
(2) develop students "physician interaction" skills MEASUREMENT SYSTEM(s):
Program Resource Survey(s) completed by the students. Program Resource Survey completed by the faculty. Faculty Review of student Clinical Summary Logs. DATE(S) OF MEASUREMENT:
Program Resource Surveys are completed annually at the end of the spring semester.
Clinical Summary logs are reviewed on an on-going basis as well as being formally reviewed twice each semester
RESULTS:
The students did not feel their pediatric/neonatal rotation was adequate for their educational goals
ACTION PLAN:
CAMC has been added for the pediatric/neonatal rotation.
2007 PROGRAM RESOURCE ASSESSMENT
RESOURCE:
PHYSICAIN INPUT - INSTRUCTIONALPURPOSE(S):
1. The primary purpose of physician interaction in the clinical setting is to assist the students in developing their "professional communication" skills to facilitate their
effective interaction in the clinical setting.
2. Physician input by the Medical Director is to assist in the development and evaluation of practitioner/physician "communication skills".
MEASUREMENT SYSTEM(s):
1. Program Resource Survey(s) completed by the students. 2. Program Resource Survey completed by the faculty. 3. Physician Interaction documentation forms.
4. Daily clinical log documentation of physician interaction.
5. Medical Director written evaluation(s) of student communication skills.
6. Pulmonologist written assessment of student assessment and communication skills.
DATE(S) OF MEASUREMENT:
1. Exit survey conducted at end of academic year (May). 2. May each year.
3. 6 per semester required / reviewed and approved by program faculty. 4. Clinical Activity logs are reviewed weekly by program faculty.
5. Medical Director evaluation of student "communication skills" performed a minimum of once each semester based on bedside clinical rounds.
6. Written evaluations are performed by Dr. Pete Ottavanio twice during Fall and Spring semesters based on clinical interaction during "patient assessment" and "Ventilator rounds" activities at St. Mary’s Medical Center.
RESULTS: 2007
The students felt physician interaction was good and beneficial in both their classroom and clinical experience.
ACTION PLAN(S):
No action necessaryAppendix
D
RESPIRATORY CARE PROGRAM Statement of Philosophy
The Respiratory Care faculty believe:
that all people have dignity and worth.
that these programs should serve people regardless of race, creed, sex, disadvantage, or handicap.
that the cognitive base, psychomotor skills, and effective domain are of equal importance in the
training of respiratory care practitioners.
that the graduates of these programs should possess competence in the technical phases of
respiratory care and a sound understanding of the scientific principles of respiratory care. that graduates should have developed the ability to make independent clinical judgments within
the limits of the respiratory therapy technician‘s responsibilities. that graduates should exhibit strong ethical behavior and attitudes.
that competent respiratory care technicians are significant participants on the health care team.
RESPIRATORY CARE PROGRAM
Goals:
1. Provide instruction necessary to enable individuals to function as competent entry level respiratory care practitioners.
2. To help satisfy the need in local and regional communities for competent respiratory care practitioners.
The Respiratory Care Program prepare graduates to:
1. Recognize the role of the respiratory care practitioner as a member of the health care team.
2. Develop a caring ethical behavior.
3. Develop a respect for the dignity and worth of the patient. 4. Develop effective communication skills.
5. Utilize a knowledge base in the sciences and technologies for the practice of respiratory care at the technician level.
6. Demonstrate an ability to practice independent clinical judgment under the direction of a physician.
RESPIRATORY CARE PROGRAM TASK LIST
A. Administering Medical Gas Therapy
1. Identify, transport, and store medical gas cylinders 2. Select, attach, and use regulating devices
3. Operate, and perform general maintenance of air compressors and oxygen concentrators
4. Select, obtain, and assemble oxygen delivery devices appropriate to the respiratory care plan
5. Administer oxygen via low flow systems 6. Administer oxygen via high flow systems
7. Administer oxygen utilizing precision metering devices] 8. Perform oxygen analysis
9. Evaluate patient response to oxygen therapy, and recommend modification as indicated
B. Administering Humidity and Aerosol Therapy
1. Select, obtain, and assemble humidifying devices appropriate to the respiratory care plan
3. Select, obtain, and assemble nebulizing devices appropriate to the respiratory care plan
4. Administer aerosol therapy via pneumatic nebulizers 5. Administer aerosol therapy via ultrasonic nebulizers 6. Administer aerosol therapy via tents
7. Evaluate patient response to humidity or aerosol therapy and recommend modifications as indicated
C. Administering Therapeutic Procedures
1. Select, obtain, and assemble therapeutic equipment appropriate to the respiratory care plan
2. Administer incentive spirometry
3. Administer intermittent positive pressure breathing (IPPB) therapy 4. Administer mask CPAP (continuous positive airway pressure) therapy 5. Administer chest physiotherapy
6. Evaluate patient response to therapeutic procedures and recommend modification as indicated
D. Administering Pulmonary Medications
1. Obtain and prepare prescribed dosage of medication
2. Administer prescribed agents via aerosol, inhalation, or metered dose inhaler 3. Monitor and evaluate patient response to the medications administered, and
recommend modification as indicated
E. Providing Airway Management
1. Select, obtain, and assemble airway management equipment 2. Position the patient to assure a patent airway
3. Insert appropriate oral and nasal pharyngeal airways 4. Perform oral endotracheal intubation
5. Change tracheostomy tubes
6. Maintain proper cuff inflation and position of endotracheal and tracheostomy tubes
7. Extubate patients
8. Remove esophageal obturator airways 9. Suction artificial airways
10. Perform naso-tracheal suctioning
11. Perform tracheal suctioning for specimen collection
and recommend modification as indicated
F. Select, Reviewing, Obtaining, and Interpreting Patient Data
1. Review existing data in the patient record, and recommend diagnostic procedures 2. Assess patient‘s respiratory status by inspection
3. Assess patient‘s respiratory status by palpation 4. Assess patient‘s respiratory status by auscultation 5. Inspect the chest x-ray for gross abnormalities 6. Interview the patient
7. Measure and assess the patient‘s vital signs
8. Recommend procedures for obtaining additional data
G. Cardiopulmonary Testing and Evaluation
1. Measure and interpret tidal volume, respiratory rate, and minute volume 2. Calculate I:E (inspiratory to expiratory) ratio
3. Measure and evaluate the negative inspiratory force 4. Measure and evaluate peak flow
I. Providing Respiratory Care in Special Settings
1. Provides respiratory care to pediatric and neonatal patients 2. Provide respiratory care in the home environment
3. Provide respiratory care in emergency situations
4. Provide respiratory care to pulmonary rehabilitation patients
J. Maintaining Infection Control
1. Utilize aseptic techniques while providing respiratory care 2. Practice isolation techniques
3. Disinfect respiratory care equipment 4. Sterilize respiratory care equipment 5. Measure and evaluate the vital capacity
6. Measure and evaluate timed forced expiratory volumes
7. Perform and evaluate spirometry pre- and post- bronchodilator 8. Measure and evaluate lung volumes
9. Evaluate the results of closing volume determination 10. Evaluate the results of diffusion studies
11. Evaluate the results of volume of isoflow measurement 12. Evaluate flow volume curves
13. Obtain samples for arterial blood gas measurement 14. Measure arterial blood gases
15. Interpret arterial blood gases 16. Perform and interpret oximetry
17. Perform and interpret capnography 18. Calculate and evaluate A-aDO2 19. Calculate and evaluate shunt 20. Calculate and evaluate VD/VT 21. Perform electrocardiography
22. Recognize basic cardiac arrhythmias 23. Measure and evaluate blood pressure 24. Interpret arterial pressure tracings
25. Interpret central venous pressure measurements
26. Evaluate (basic) hemodynamic patterns from pulmonary artery catheters 27. Inspect the chest x-ray to find gross abnormalities
H. Providing ventilatory Support
1. Assess the patient‘s need for ventilatory support 2. Select, assemble and prepare appropriate ventilators 3. Select appropriate ventilatory parameters
4. Adjust the mechanical ventilator to comply with physician orders or established protocol
5. Recommend modification of ventilatory parameters based on patient data 6. Initiate, adjust, and monitor effects of CPAP and PEEP
7. Replace ventilator circuits as needed
8. Institutes modifications of ventilator circuitry following established protocol 9. Institute and modify weaning procedures
10. Monitor, record, and react to changing conditions related to mechanical ventilation
This 3 credit hour will introduce the student to the basic principles of pharmacology. This will include regulatory agencies, dosage calculations, and the physiology of the autonomic nervous system as it is related to respiratory care pharmacology. Major topics of discussion include; sympathomimetics, parasympolytics, xanthines, prostaglandins, Mucokinetics, cortiocosteriods, cromlyn sodium, other broncho-active agents, and neuromuscular blockers. Additionally, central nervous system agents, cardiovascular and diuretic agents, and antimicrobials are included.
RSP 101 – Introduction to Respiratory Care
This 2 credit hour course will introduce the student to the History of Respiratory Care and Professional
Organization. Emphasis is on exploring the role of the respiratory therapist or technician as a member of the health care team. Ethical and medicolegal dimensions of health care are presented. Basic techniques of patient evaluation are covered. Included are: Chest physical examination, measurement of the vital signs, patient interview and history, evaluation of the chest x-ray, and spirometry.
Pre- requisites Admission into the Respiratory Care Program
RSP 102 – Introduction to Respiratory Care Procedures
This introduction course is 3 credit hours in length. The administration of medical gases, humidity and aerosol therapy is covered. Emphasis is placed on the safe handling of medical gases and safety in administration. Principles and techniques of therapeutic procedures used in basic respiratory care are covered. Also included are: Techniques of chest inflation therapy, chest physical therapy, breathing exercises, bronchial hygiene. The physiologic effects, indications, and contraindications of each therapy are stressed. Detailed study of isolation, equipment and supplies used in these therapies is included.
Pre-requisites – Admission into the Respiratory Care Program.
RSP 102L - Respiratory Care Procedures Lab
This 1 hour laboratory class will give the student the opportunity to practice techniques and use of technology covered in Respiratory Care Procedures and Introduction to Respiratory Care. Lab exercises will be given for the student to complete.
Pre-requisites – Successful completion of program sequence.
RSP 201 – Pulmonary Pathophysiology
This 3 credit hour course is designed to supplement the information presented in Introduction to Respiratory Care. The most frequently encountered diseases and syndromes are presented in detail. Emphasis is placed on the etiology, signs and symptoms, pathology, clinical manifestations, sequellae, and treatment. The respiratory therapists role in the recognition and treatment of pulmonary diseases is given special emphasis.
The student completing the course is expected to have a firm understanding of the diseases covered.
RSP 202 – Mechanical Ventilation Technology & Management
This 3 credit hour course provides an introduction to the fundamentals of mechanical ventilation techniques and terminology is presented. Various classes of mechanical ventilators are discussed and compared, emphasizing the differences required in their uses. The technology of adult continuous mechanical ventilation is covered. The design, function, and operation of representative mechanical ventilators of the various classifications are examined in detail.
Management of continuous adult mechanical ventilation is covered with emphasis on the physiologic effects of various techniques and selection of optimal methods. Monitoring, quality control, and the ability to solve clinical problems relating to mechanical ventilation are emphasized.
Pre-requisites – Successful completion of program sequence
RSP 202L -Mechanical Ventilation Technology & Management Lab
This 1 hour laboratory class will give the student the opportunity to practice techniques and use of technology covered in Mechanical Ventilation & Management. Lab exercises will be given for the student to complete.
Pre-requisites – Successful completion of program sequence
RSP 203 – Respiratory Internship 1
This 4 credit hour course is designed to introduce the student to the clinical facility and to clinical education. Opportunity is given for observation of the various aspects of respiratory care. Practice in gathering information from the patient record, patient evaluation, oxygen administration, and record keeping is provided. Techniques of cardiopulmonary resuscitation are covered with laboratory practice and evaluation.
Pre-requisites – Successful completion of program sequence.
RSP 204 – Cardiopulmonary Diagnostics
This 3 credit hour course will cover advanced techniques of pulmonary function testing. Topics include lung volume determination, tests of small airways, diffusion, and distribution of ventilation. Invasive and non-invasive methods of arterial blood gas sampling, analysis, and interpretation are also covered. The technology and
methodology of invasive and non-invasive cardiovascular testing including electrocardiography and hemodynamic monitoring are presented. Fundamental interpretation of these tests is covered.
Pre-requisites – Successful completion of program sequence.
RSP 205 – Neonatal/Pediatric Respiratory Care
This introductory course is 3 credit hours. It is designed to provide the student with detailed knowledge to the needs of neonatal and pediatric patients. Fetal cardiopulmonary development and changes at birth are covered.
Equipment, procedures and methods used in the care and evaluation of neonatal and pediatric patients are also covered (Neonatal Vents). Also included are cardiopulmonary conditions and diseases particular to neonate and pediatric patients.
Pre-requisites – Successful completion of program sequence.
RSP 206 – Introduction to Critical Care Management
This introductory course is 3 credit hours and is designed to provide the student with detailed knowledge to the principles and techniques of therapeutic procedures used in Respiratory Care as covered: Airway management, transtracheal oxygen therapy and aspiration, bronchoscopy, thoracentisis and pleural chest tubes, arterial lines, ABG interpretation and analysis, transports, and electrocardiogram interpretation.
Pre-requisites – Successful completion of program sequence.
RSP 207 – Pulmonary Rehabilitation/Home Care
This 1 credit hour course will cover care of the patient with long term pulmonary disability. Psychosocial and physical needs of the patient are addressed with emphasis on motivating and conditioning the patient with the goal of improving both quality of life and cardiopulmonary reserve. Special requirements for the patient in the home who requires respiratory care are covered.
Pre-requisites – Successful completion of program sequence.
RSP 208 – Seminar in Respiratory Care
This 1 credit hour course introduces the student to NBRC exam taking skills, mock examinations of the NBRC matrix, and self-evaluation studies. Study methods and application are also covered. A study of realistic clinical problems and situations, with emphasis on analyzing and evaluating these problems to formulate acceptable respiratory care modalities. Practice will be provided in the necessary techniques to take the NBRC clinical simulation examination. Computer simulations are an integral part of this course.
Pre-requisites – Successful completion of program sequence.
RSP 209 –Respiratory Internship 2
This course is 4 credit hour course is designed to introduce the student to aspects of Respiratory Care learned in RSP 102 and RSP 101. Emphasis is on the supervised practice of basic respiratory care techniques covered in
Introduction to Respiratory Care Procedures and in Introduction to Respiratory Care. Opportunity for respiratory care techniques such as oxygen therapy, humidity and aerosol therapy, aerosol drug therapy, lung inflation therapy is provided. Also, observation and supervised practice in the techniques used in electrocardiography.
Pre-requisites – Successful completion of program sequence.
RSP 210 – Respiratory Internship 3
This course is 4 credit hour course is designed to provide the student with additional experience in the practice of fundamental respiratory care techniques. Emphasis is given to the development of efficiency in the practice of these techniques. Opportunities for observation and strictly supervised practice in the techniques of arterial blood gas sampling and analysis, arterial line management and chest tube management. are also provided. Also, included is critical care observation, supervised practice of techniques used in electrocardiography and observation of hemodynamic measurement and monitoring. Additional experiences in the application of all previously covered respiratory care techniques are also provided.
Neonatal/Pediatric assessment and care will be provided in addition to mechanical ventilation, airway management, critical care respiratory therapy, pulmonary function testing and sleep studies. Emphasis will be placed in
pulmonary rehab/home care and neonatal/pediatric respiratory care. The student of this course will maintain daily records of all activities. The student will submit and present a detailed case study.
Pre-requisites – Successful completion of program sequence.
RSP 211 –ACLS/PALS
This 1 credit hour course is designed to provide the student, upon successful completion, the Advanced Cardiac Life Support and Pediatric Advanced Life Support certification. This course will cover topics required by the American Heart Association for certification.
Pre-requisites – Successful completion of program sequence.
RSP 212 – Cardiopulmonary/Renal Anatomy & Physiology
This 3 credit hour course will cover the anatomy and physiology of the respiratory systems in detail. Emphasis is placed on the interaction of systems in gas exchange renal and acid base balance. The structure and function of the chest cage, mechanics of breathing, and control of respiration are also included.
Pre-requisites – Successful completion of program sequence.
RSP 301 – Introduction to Management
Introduction to basic principles of management and their application in the current healthcare environment. Course content includes: management theory, scope of management, quality issues, budgeting, personnel issues, and evaluation and application of management concepts.
RSP 302 –Directed Reading/Seminar Critical Care
This course affords the senior respiratory care student with the opportunity to practice advanced evaluative and procedural skills in the intensive care setting. Emphasis is placed on cardiopulmonary assessment and treatment of trauma, post-surgical, cardiac and renal patients, quantitative assessment techniques, refinement of monitoring procedures, and interpretation of data.
RSP 303 - Respiratory Education
This 3 credit hour course is designed as an introduction to clinical teaching in a respiratory care program. The course includes self-directed study in instructional and evaluation strategies and development of performance objectives. The student performs functions required of a clinical instructor in a respiratory care program. The student will be required to set up
Prerequisite:
RSP 304 - Respiratory Cost Management & Solutions
This 3 credit hour course introduces the student to management decision making and providing costs solutions for a respiratory department. Topics covered will be annual budgets, purchasing decisions, effective staffing, inventory and supply controls as well as searching for other methods to contain costs in the healthcare environment.
Prerequisite: